Abstract
While a number of genome-wide association studies have identified microtubule-associated protein tau as a strong risk factor for Parkinson’s disease (PD), little is known about the mechanism through which human tau can predispose an individual to this disease. Here, we demonstrate that expression of human wild-type tau is sufficient to disrupt the survival of dopaminergic neurons in a Drosophila model. Tau triggers a synaptic pathology visualized by vesicular monoamine transporter-pHGFP that precedes both the age-dependent formation of tau-containing neurofibrillary tangle-like pathology and the progressive loss of DA neurons, thereby recapitulating the pathological hallmarks of PD. Flies overexpressing tau also exhibit progressive impairments of both motor and learning behaviors. Surprisingly, contrary to common belief that hyperphosphorylated tau could aggravate toxicity, DA neuron degeneration is alleviated by expressing the modified, hyperphosphorylated tauE14. Together, these results show that impairment of VMAT-containing synaptic vesicle, released to synapses before overt tauopathy may be the underlying mechanism of tau-associated PD and suggest that correction or prevention of this deficit may be appropriate targets for early therapeutic intervention.
Electronic supplementary material
The online version of this article (doi:10.1007/s00401-013-1105-x) contains supplementary material, which is available to authorized users.
Keywords: Parkinson’s disease, Dopamine, Tau, MAPT, Neuron degeneration, Tauopathy
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder, affecting 1–2 % of people over the age 60, and is characterized by clinical manifestations of bradykinesia, rigidity, resting tremor, and postural instability. These motor defects are thought to result from degeneration of pigmented dopaminergic (DA) neurons in the basal ganglia, particularly those projecting from substantia nigra pars compacta to the striatum [13, 21, 45]. Deposition of Lewy bodies or formation of Lewy neurites, composed of fibrillar aggregates of α-synuclein, are the classical pathological hallmark of PD [48]. However, tau-containing neurofibrillary tangles (NFTs) are also found in the brains of PD patients [60]. Although the inherited forms of PD are rare, genetic variation in PD susceptibility genes may play a significant role, through gene–environment interactions, in the development of sporadic PD [45].
Microtubule-associated protein tau (MAPT), leucine-rich repeat kinase 2 (LRRK2), and α-synuclein (SNCA) have been identified as the top three PD susceptibility genes [46]. Both SNCA and LRRK2 have been extensively studied in vitro and in vivo; however, the molecular and pathological role of MAPT in PD remains poorly understood [57]. The link between MAPT and disease, originally identified for inherited autosomal dominant frontotemporal dementia and Parkinsonism, is linked to chromosome 17 (FTDP-17). A similar association was later found in several rare atypical Parkinsonism syndromes, including progressive supranuclear palsy (PSP) and corticobasal degeneration (CB) [20, 22, 28]. More recently, a number of studies have suggested that genetic variants in MAPT can also predispose an individual to the development of sporadic and familiar forms of PD [45]. Interestingly, most mutations of MAPT associated with FTDP-17 are located in protein coding sequences for microtubule-binding repeats and splicing sites [22], whereas the mutations identified in allelic variants of MAPT associated with PD are located in upstream regulatory elements [17].
The relationship between human tau and PD is illustrated by a number of genome-wide association studies (GWAS) [16, 32, 38, 46]. The MAPT H1 haplotype is associated with an increased risk of PD [17]. In addition, individuals homozygous for MAPT H1/H1 have an increased susceptibility to develop PD compared to those bearing the heterozygous H1/H2 genotype [59]. Furthermore, some of the MAPT variants appear to increase overall Tau expression [25]. Together, these studies suggest that elevated expression of tau may increase the risk of PD via a genetically gain-of-function mechanism, similar to the duplication of the amyloid precursor proteins gene (APP gene) [43] or duplication or triplication of SNCA (encodes α-synuclein) [47]. However, unlike aberrant copy numbers of APP and SNCA, which have been clearly identified in hereditary AD and PD pedigrees, respectively, evidence for a relationship between MAPT gene dosage and either PD or tauopathies remains primarily circumstantial.
In the present study, we explored whether expression of wild-type MAPT affects DA neurons, the most vulnerable cells in PD, by using a Drosophila animal model. We found that expression of wild-type human tau (htauWT) produces the progressive degeneration of DA neurons. In addition, we observed age-dependent formation of tau-positive, tangle-like pathology in the soma of the DA neurons that was similar to NFTs seen in transgenic mice and AD brains. Flies expressing tau also exhibited motor and learning deficits that coincided with progressive neurodegeneration. Surprisingly, we observed that expression of htauWT caused molecular pathogenesis in synapses, visualized by VMAT-pHluorin localization to nerve terminals that preceded identified pathological events such as tangle formation and overt cell loss. Our results suggest a potential molecular pathological mechanism through which tau may increase the risk of PD.
Materials and methods
Fly strains and genetics
Flies were cultured in standard corn meal–yeast–agar media at 25 °C, and 75 % relative humidity with a light/dark = 12/12 h cycle. Ddc-Gal4 and 996TPH-GAL4 were kindly provided from Jay Hirsh (University of Virginia). UAS-G-CaMP was obtained from Richard Axel (Department of Biochemistry and Molecular Biophysics, Columbia University). UAS-mCD8-GFP and GMR-GAL4 were obtained from Larry Zipursky (University of California, Los Angeles). Fly strains TH-GAL4, DVGLUT-GAL4, GAD-GAL4, NPF-GAL4, RH1-GAL4, UAS-actinGFP and tubGAL80ts were used in this study. UAS-htau.1 (II), UAS-htau.2 (III) and UAS-VMAT- pHluorin (III) were characterized in this study. UAS-tau AP , UAS-tau E14 and UAS-tau WT were described previously [49, 50].
Molecular cloning and transgenic flies
For generating human tau transgenes, the longest isoform of human tau cDNA, encoding amino acids 1–441, (Origene Technologies, Rockville, MD), was cloned into pUAST vector using EcoRI and NotI restriction sites. Site-directed mutagenesis was used to generate htau G272V and htau R406W with forward and reverse primer pairs of 5′-GAAGCACCAGCCGGGAGTC-3′ and 5′-CTTCCCGACTCCTG-3′ for G272V, and 5′-GACACGTCTCCATGGCATCTC-3′ and 5′-GAGATGCCATGGAGACGTGTC-3′ for R406W, respectively. The mutations of htau G272V and htau R406W were confirmed by DNA sequencing and subcloned into pUAST expression vector. Germ line transformation and standard fly-balancer crosses were performed. We obtained multiple UAS-htau WT, UAS-htau G272V and UAS-htau R406W transgenic lines. Those with comparable expression level were selected for this study. PHluorin was inserted into the first luminal loop of VMAT and cloned into pUAST vector.
Behavioral analysis
The startle-induced negative geotactic climbing assays were performed as previously described [2, 44]. For locomotion assay, 4-week-old flies (4 weeks after eclosion) were placed in chambers marked with grids and individual were recorded (videotaped) for periods of 10 min. Locomotion (locomotion index) was manually scored by counting the number of grids individuals crossed per minute. Olfactory associative learning was measured by training 3-week-old adult flies in a T-maze with the Pavlovian conditioning procedure as previously described [52]. Briefly, a group of 100 flies were first exposed to an odor (a conditioned stimulus, CS+) paired with 12 1.5 s pluses of 75 V DC electric shock (an unconditioned stimulus, US). For conditioning order stimulus, we used 3-octanol and 4-methyl-cyclohexanol. This was sequentially followed by presentation of a second odor (CS−) without reinforcement. Performance of conditioned avoidance responses was immediately measured with a choice between CS+ and CS− odors in a T-maze for 2 min after training. A performance index (PI) of aversive learning was calculated as (the number of flies in CS− arm) − (the number of flies in CS+ arm)/(the total number of flies) × 100.
Confocal and electron microscopy
Fly brains and eyes were fixed, stained and mounted in Vectashield (Vector Laboratories, Burlingame, CA) as previously described [9]. Congo-philic stain was performed as previously describe [3]. Confocal microscopic observations of fly brains were performed using a Zeiss LSM 510 laser scanning confocal microscope (Carl-Zeiss, Germany). For characterization of different clusters of DA neurons, Z-stack confocal images that span 50 μm depth were collected from posterior to anterior direction to ensure all posterior clusters are covered. 3D images for each brain are used for examining neuron structure. For presenting purpose, Z-stack images are projected into a single 2D image.
For live brain imaging, fly brains were dissected in 1× PBS and G-CaMP was visualized immediately following brain dissection by confocal microscopy [54]. For VMAT-pHluorin experiments, released sites of VMAT-pHluorin of DA neurons were visualized as previous described [40]. Primary antibodies included mouse tau monoclonal antibodies AT8, AT100, and AT180 (Thermo Fisher Scientific, Waltham, MA), rabbit tau polyclonal antibody (Dako, Denmark), and mouse anti-TH (Immunostar, Hudson, WI). Secondary antibodies FITC and Cy3 conjugated anti-mouse or anti-rabbit (Jackson ImmunoResearch Laboratories, West Grove, PA) were used. NIH imageJ64 was used for quantification of G-CaMP and GFP using monochrome images, by measuring pixel intensity, as relative fluorescence with fluorescence-background calibration. For presenting G-CaMP activity, signal intensity was transformed to the pseudocolored thermal scale. Scanning electron microscopy was used to analyze fly eye morphology as previously described [10]. For pair-helical filament examination, transmission electron microscopy (TEM) was used as previously described [23], with the following modifications. Briefly, a resuspended sarkosyl insolubility pellet was placed on a carbon-coated copper grid (75 mesh) and stained with 1 % uranyl acetate. Samples were examined using HT7700 TEM (Hitachi).
Western blots and sarkosyl insolubility assay
To detect the protein expression level, aged fly brains were homogenized in sample buffer using a glass micro-tissue grinder. To enrich tangles, sarkosyl-insoluble fractions of tau were purified from 40 homogenized fly heads as previously described [14] and used for western blot analysis and TEM observation. Standard western blotting procedures were used as previously described [8]. Primary antibodies included mouse cytochrome c (Gene Tex, Irvine, CA), and rabbit cleaved caspase 3 (Cell signaling technology, Danvers, MA). ECL reagents were used for antibody detection (Millipore, Billerica, MA) and imaging was performed using ImageQuant 350 (GE Healthcare).
Results
MAPT overexpression results in the progressive loss of DA neurons
Numerous mutations in MAPT have been linked to FTDP-17, including an increased ratio of the longest 4R Tau isoform [8]. In addition, several GWAS suggest tau variants as a risk factor for PD, and an increased incidence of PD is associated with elevated MAPT levels [16, 25, 32, 36, 38, 46, 55]. These observations suggest that misregulation of tau expression might contribute to the death of dopaminergic neurons. To investigate the effects of human tau overexpression in DA cells, we chose to test the effects of the largest htauWT isoform (2N4R), because an increase of this largest isoform may predispose the susceptibility to PD or some FTDP-17.
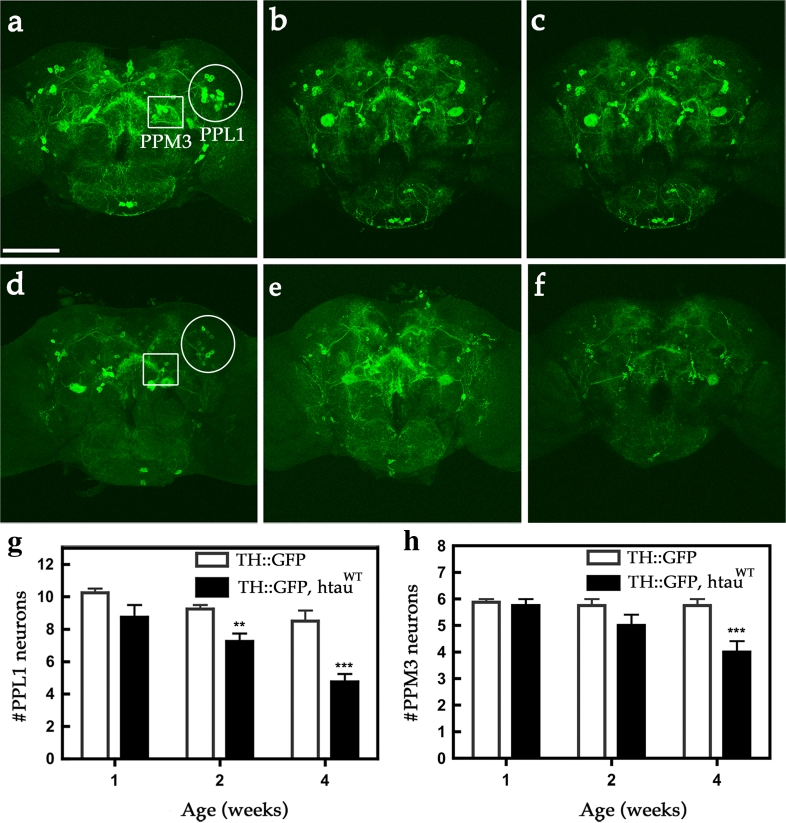
Since the most affected neurons in PD are the DA neurons, we used the TH-GAL4 driver to overexpress UAS-htau WT and co-express UAS-mCD8-GFP, to fluorescently label the plasma membrane of the cell body and neurite processes (TH::htauWT, mCD8-GFP). We then tested whether htauWT expression resulted in degeneration of these DA neurons. In young adults (1-week-old), the number of GFP-marked DA neurons in htauWT transgenic brains was comparable to control brains (TH::mCD8-GFP). At 2 weeks after eclosion, limited degeneration was observed in a small subset of PPL1 neurons expressing htauWT compared to age-matched controls. Remarkably, at 4 weeks after eclosion, we observed a significant loss of DA neurons in transgenic flies relative to controls (Fig. 1). This loss occurred in two clusters of DA neurons: PPL1 and PPM3 (Fig. 1). Other FTDP-17 associated two tau variants of G272V and R406W, also showed similar effects (Fig. S1). To validate these htauWT-expressing cells may have undergone progressive degeneration, we characterized two components of the cell death signaling: cytochrome c and activated caspase 3-like caspase [53] for these htauWT-expressing cells and their GFP expressing controls in Drosophila. As expected, the expression of htauWT produced an abnormal increase in the expression of cytochrome c, before a surge of caspase 3-like caspase activation in 3-week-old flies expressing htauWT, relative to controls, suggesting the activation of cell death signaling in htauWT-expressing brains in Drosophila (Fig. S2). These results indicate a progressive degeneration of DA neurons in the brains of Drosophila expressing htauWT. To further confirm the effect of htauWT, we employed a second GAL4 driver, DDC-GAL4, which targets htauWT in both DA and serotonergic neurons. We confirmed that htauWT does induce the age-dependent DA neuron degeneration (Fig. S3). Together, these results show that expression of htauWT can induce progressive loss of DA neurons, manifesting the pathological DA degeneration in PD.
Fig. 1.
Expression of htauWT induces age-dependent DA neuron demise. Representative confocal images show mCD8-GFP-marked DA neurons in age-matched control fly brains (a–c TH::mCD8-GFP) and htauWT-expressing brains (d–f TH::htauWT, mCD8-GFP) of one- (a, d), two- (b, e), and four- (c, f) week-old individuals. Two clusters of DA neurons, PPL1 (protocerebral posterior lateral 1, circles) and PPM3 (protocerebral posterior medial 3, squares), are indicated. Scale bar 100 μm. Cell counts of PPL1 (g) and PPM3 (h) DA neurons from age-matched control and htauWT brains. Values shown represent Mean ± SEM (unpaired t test, **P < 0.001 at week 2 for g; ***P < 0.0001 at week 4 for g and h; n = 12)
MAPT overexpression produces age-dependent motor and learning deficits
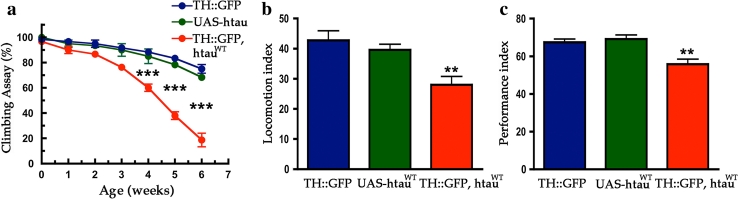
Similar to its role in mammals, the Drosophila nervous system utilizes many neurotransmitters to operate motor and cognitive behaviors. In the dopaminergic system, fruit fly use the same neurotransmitter as mammals to modulate a number of intricate neuronal circuits, ranging from those that control voluntary movement, mating, rewards, learning, and memory [41]. We tested whether expression of htauWT would alter motor behaviors. Using a negative geotaxis assay, we observed that TH::htauWT flies have a dramatically age-dependent climbing deficit; they showed significant loss of climbing ability compared to control flies at 4–6 weeks post-eclosion (Fig. 2a). In addition, we observed that flies expressing htauWT showed reduced spontaneous locomotion; they appeared “sluggish” and exhibited an increase in the number of “pauses” between bouts of spontaneous locomotion and travelled shorter distances during each bout (Fig. 2b).
Fig. 2.
Expression of htauWT in DA neurons causes motor and learning deficits. Behavioral analyses of driver control (TH::mCD8-GFP, blue), transgene control (UAS-htau WT, green), and htauWT expression (TH::htauWT, mCD8-GFP, red) flies. a Negative geotaxis assay was utilized for testing climbing activities of newly enclosed to 6 weeks age-matched adults. Accelerated decline of climbing activity was observed in flies expressing htauWT in DA neurons (one-way ANOVA with Bonferroni’s multiple comparison test, ***P < 0.0001 compares each genotypes, n = 4). b Quantitative locomotion behaviors of 4-week-old flies show reduced activity in htauWT expression group as compared to that in control groups (one-way ANOVA with Bonferroni’s multiple comparison test, **P < 0.001, n = 16). c Olfactory associative learning assay of 3-week-old flies revealed that flies in which DA neurons expressed htauWT exhibited defects of olfactory aversive associative learning as compared to the control groups (one-way ANOVA with Bonferroni’s multiple comparison test, **P < 0.001, n = 4)
Next, we performed short-term olfactory association assays to test whether expression of htau in DA neurons affects learning. To avoid the potential confound caused by motor deficits, we tested 3-week-old cohorts, an age at which the motor behavior of htauWT-expressing flies is comparable to that of controls. As expected, we observed modest but significant learning deficit in htauWT-expressing flies, which scored 10 % lower than the age-matched control groups (Fig. 2c). This result is consistent with recent empirical findings indicating that dopaminergic neurons projecting to the mushroom body are essential mediators of olfactory associative learning and memory [1, 4, 7, 39, 42]. Together, these results show that flies expressing htauWT in DA neurons manifest deficits in both motor and learning behaviors, which corroborate the observed age-dependent loss of DA neurons.
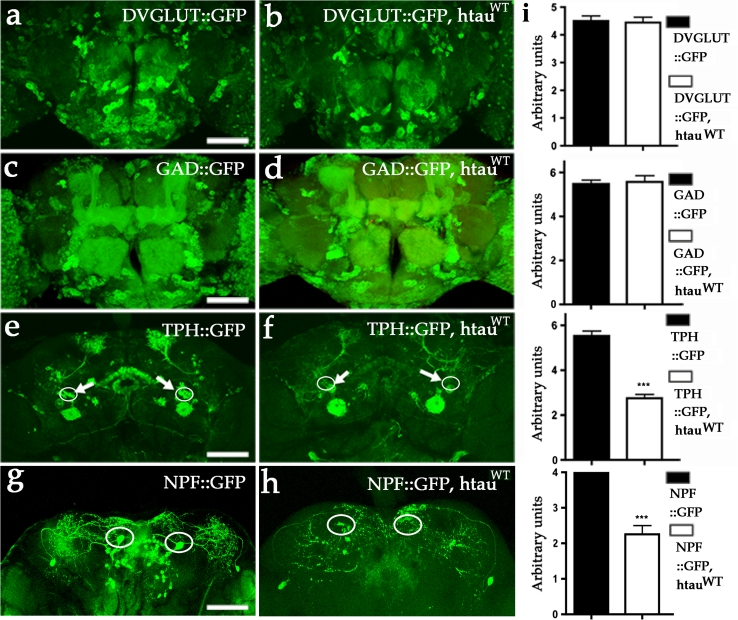
Aminergic and NPF neurons are relatively more vulnerable to MAPT expression
To determine how expression of htauWT would affect neurons using other types of neurotransmitters, we used additional GAL4 drivers including DVGLUT-GAL4 for glutamatergic neurons, GAD-GAL4 for GABAergic neurons, TPH-GAL4 for a subset of serotonergic neurons and NPF-GAL4 for a subset of peptidergic F neurons. We did not observe loss of either GFP-marked glutamatergic or GABAergic cells (Fig. 3a–d, i); however, we observed that a subset of putative serotonergic neurons that project to the central complex and a subset of putative NPF neurons were lost (Fig. 3e–i). These results are consistent with previous studies that have shown human tau expression can cause degeneration of several neuronal populations in Drosophila [23, 33, 56]. Together, these results demonstrate that htauWT can induce degeneration of DA neurons, serotonergic neurons, and NPF neurons, whereas most glutamatergic and GABAergic neurons are unaffected by htauWT expression based on the fluorescent optical observation.
Fig. 3.
Expression of htauWT fails to manifest neuronal loss in most glutamatergic and GABAergic neurons. a, b Representative confocal images show glutamatergic neurons of 4-week-old fly brains marked with mCD8-GFP. Several thousands of glutamatergic neurons with comparable GFP signals in both control (a, DVGLUT::mCD8-GFP) and htauWT brains (b, DVGLUT::htauWT, mCD8-GFP). c, d Representative confocal images show mCD8-GFP-marked GABAergic neurons in 6-week-old fly brain. Comparable GFP signals can be detected in both control (c GAD::mCD8-GFP) and htauWT brains (d GAD::htauWT, mCD8-GFP). e Representative confocal image shows a group of putative serotonergic neurons (TPH996::mCD8-GFP) projecting to central complex (arrows) at 4 weeks of age. f Representative confocal image shows the absence of GFP signals in neurons projecting to central complex in age-matched brain expressing htauWT (TPH996::htauWT, mCD8-GFP). g Representative confocal image shows two pairs of putative NPF neurons (NPF::mCD8-GFP) projecting to parietal central brains in control (f). In contrast, the GFP signals in a pair of NPF neurons that are located in the anterior region are absent in htauWT-expressing brains (NPF::htauWT, mCD8-GFP) at 4 weeks of age. Scale bar 100 μm. i Quantitative analyses show no significant differences between control (black bars) and htauWT (white bars) brains in DVGLUT, and GAD groups (unpaired t test, P = 0.54 for a and b; P = 0.60 for c and d, n = 4). In TPH and NPF groups, both the cell measurements (circles) between controls and htauWT are different (unpaired t test, ***P < 0.0001 for both e and f, and for g and h, n = 4)
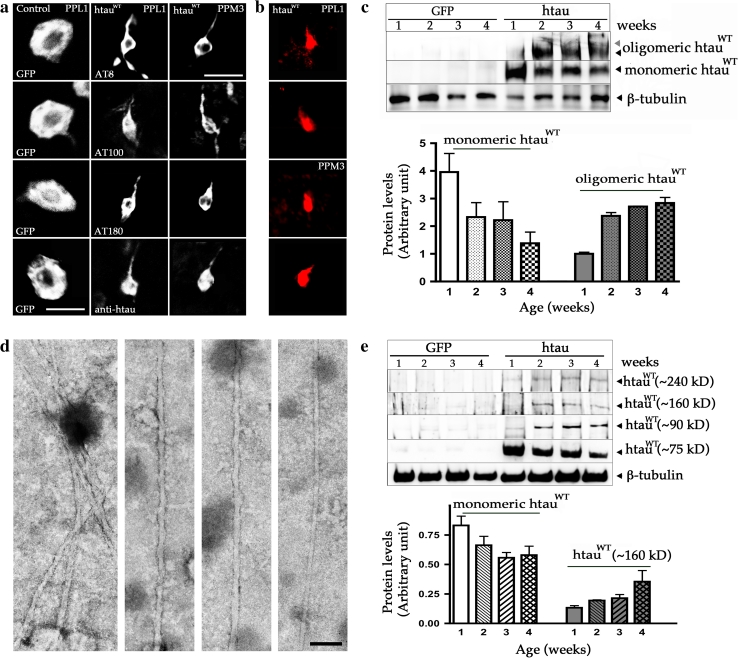
Formation of abnormal oligomeric tau and tangle-like pathology in DA neurons
Hyperphosphorylated tau has been suggested to accumulate as homogeneous or heterogeneous oligomers and subsequently form NFT [5]. To determine whether similar pathogenesis occurs in DA neurons that express htauWT, we used three common phosphoepitope antibodies (AT8, AT100, and AT180) and a polyclonal anti-tau antibody that have been widely utilized to characterize AD-like abnormal phosphorylation of tau in the postmortem brains of AD patients and animal models of tauopathies. Immunohistochemical analysis of TH::htauWT brains at different ages revealed that the morphology of DA neurons appeared normal in the first week, with no detectable morphological changes in the soma and neurites, suggesting that the neuronal architecture was normal in young adults (Fig. S4). At approximately 2 weeks post-eclosion, the staining pattern of the soma in some DA neurons has changed relative to the wild-type morphology, indicating that the cytoskeletal networks had been perturbed or disintegrated by this time (Fig. S4). Strikingly, after 3 weeks, the phosphoepitope antibodies and a polyclonal anti-tau antibody began to reveal abnormal tangle-like morphology, resembling NFTs at the microscopic level in most DA neurons including those in PPL1 and PPM3. This result suggests that the appearance of abnormal NFTs in DA neurons is an age-dependent process (Fig. S4). To explore whether htau expression might also induce tangle pathology in general, we investigated other types of neurons expressing htauWT. Similar morphological change was also detected in a small subset of 5HT neurons, but no obvious alteration was detected in glutamatergic, GABAergic and NPF neurons in 6-week-old flies (Fig. S4). DA neurons that express htauWT exhibited largely pruned neurite branches at the distal end in 4-week-old individuals (Fig. S4). The few cells that survived until 6 weeks experienced soma shrinkage, which was dramatically different from age-matched, GFP-labeled DA neurons from control brains (Fig. 4a, S4). Moreover, we confirmed that at 6 weeks, these abnormal DA neurons expressing htauWT were stained by Congo red, a synthetic dye which recognized the abnormal β-sheet conformation of htau aggregations (Fig. 4b).
Fig. 4.
Expression of htauWT produces AD-like abnormal tau phosphorylation and NFT-like pathology. a Single cell of PPL1 and PPM3 DA neurons from fly brains at 6 weeks of age. Compared to the age-matched control DA neurons from PPL1 cluster labeled with GFP (left column), immunostaining of three antibodies that recognize AD-like hyperphosphorylated tau (AT8 top row, AT100 top second row, AT180 bottom second row), and a polyclonal tau antibody (bottom row) reveal tangle-like pathology in the degenerating DA neurons from PPL1 (second column) and PPM3 (third column) clusters. b The degenerating DA neurons from both PPL1 and PPM3 clusters are stained with Congo red. The time course of pathological tangle-like structure formation in htauWT brains during the aging process is presented in Fig. S3. c Representative immunoblot of polyclonal anti-htau shows that a substantial amount of htauWT proteins are converted from monomer tau (75 kDa) to the oligomeric Tau species (>400 kDa). Anti-β-tubulin serves as a loading control. Protein expression levels from four independent immunoblots with monomeric and oligomeric htau protein levels calibrated against the loading control are shown as relative expression. Values shown represent mean ± SEM. d Electron micrographs of abnormal filaments extracted from tangle-rich preparation (sarkosyl-insoluble pellets) of fly brains expressing htauWT. Images show several PHF-like filaments are bundled (left panel), a single PHF (middle panels), and a straight filament (right panel). Scale bar 100 nm. d Representative immunoblot from sarkosyl-insoluble pellets reveals monomer tau ***(75 kD) and the htau-containing species with molecular weights range between 75 and 400 kD (~90, ~160 and ~240 kD). Anti-β-tubulin also serves as a loading control. e Monomeric and polymeric htau protein levels are quantified by analyzing three independent immunoblots and shown as relative expression. Values represent mean ± SEM
To determine whether these morphological changes were associated with structural changes in htauWT, we performed additional biochemical analyses on whole brain extracts from aged flies expressing TH::htauWT. We observed a gradual reduction of monomeric tau, and an increase in high-molecular-weight species, of human tau protein with increasing age (Fig. 4c). The appearance of the putative tau oligomers (>400 kDa) seemed to coincide with the onset of morphological change in DA neurons, which is in agreement with the hypothesis that tau oligomers may be toxic.
In order to more rigorously evaluate htau aggregates in DA neurons, we performed ultrastructure examination on sarkosyl-insoluble fraction extracted from htau transgenic brains. TEM revealed abundant filamentous aggregates formed in the extracts from fly brains of 4-week-old Drosophila expressing htauWT (Fig. 4d), but not in identically prepared sarkosyl-insoluble fraction from age-matched nontransgenic control brains. These negatively stained filaments were either helical (paired helical filaments, PHF) or straight (paired straight filaments, SF), with diameters of approximately 15–40 nm and the axial distance between consecutive wider portions of approximately 80–100 nm (Fig. 4d), resembling those PHFs found in AD [12]. Therefore, we suggest that the observed htau aggregates with an NFT-like pathology may be composed by PHF or SF.
To determine whether htauWT insolubility coincided with the appearance of the tangle-like morphology in DA neurons, we performed sarkosyl insolubility assays from brains at different ages. Western blotting of anti-htau revealed a modest reduction of insoluble tau monomer, and an increase with age, of several insoluble high-molecular-weight species between 75 and 400 kDa, including ~90, ~160, and ~240 kDa tau-positive bands (Fig. 4e). The formation of these insoluble high-molecular-weight aggregations apparently preceded the formation of tangles, which is consistent with the hypothesis that insoluble tau-containing aggregations may be responsible for the NFT-like pathology.
Effects of tau phosphorylation on neuron degeneration
Previous studies have suggested that tau phosphorylation is associated with AD and other tauopathies, although the role of phosphorylated state in disease pathogenesis remains controversial. To test whether the htauWT-induced DA neuron degeneration in Drosophila is related to its phosphorylation state, we expressed htauWT and phosphorylation site variants in DA neurons and compared their potential toxicity in aged fly brains. We focused on SP/TP sites, for which several proline-directed kinases such as glycogen synthase kinase 3 beta (GSK-3β) have been shown to modulate tau-mediated toxicity [23], and compared the effects of htauWT, htauAP, and htauE14. The AP mutation blocked proline-directed tau phosphorylation and the E14 mutation mimics phosphorylation of the endogenous 14 serine/threonine amino acids in htau. To confirm that htauWT can undergo phosphorylation in Drosophila DA cells, we performed western blots and observed a shift in the molecular weight of htauWT, from 75 to 60 kDa, in response to treatment with alkaline phosphatase (Fig. S5).
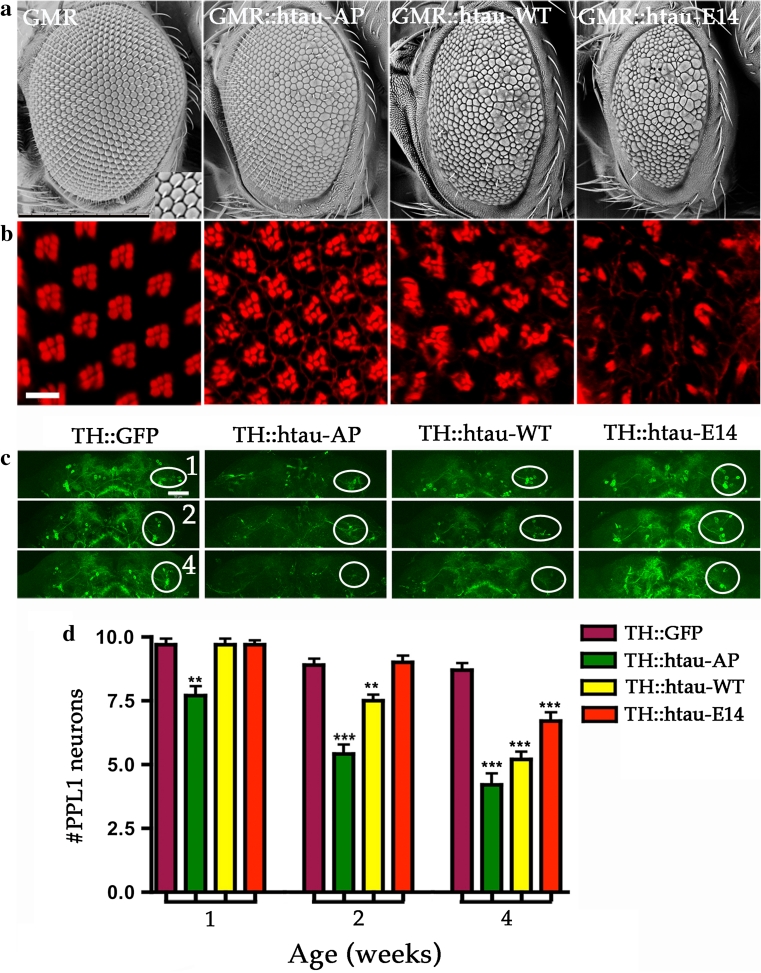
An earlier study showed that the htauAP mutation is less toxic than htauWT when expressed in Drosophila photoreceptors, but that the htauE14 mutation enhances neurotoxicity in the retina [49, 50]. Our results, using GMR-GAL4 driver to express these htau constructs in the retina, confirmed these observations (Fig. 5a, b). Surprisingly, the htau constructs appeared to have inverse effects when expressed in DA cells using TH-GAL4. TH::htauAP brains showed an increase in DA cell death, compared to flies expressing htauWT, and htauE14 resulted in less neurodegeneration than tauWT (Fig. 5c, d). Western blots validated that htauWT, htauAP, and htauE14 were expressed at similar levels, indicating that the phenotype is specific for the mutation in tau rather than expression of the transgenes (Fig. S5).
Fig. 5.
Different phosphorylation site mutations of tau exert contrary effects on DA and histaminergic neurons. Representative SEM (a) and confocal (b) images of fly compound eyes. Control (GMR-GAL4) fly eyes show crystalline array of ~800 hexagonal-shaped ommatidia form the smooth external surface. Phalloidin staining reveals the underlying organization of each ommatidium with actin-rich rhabdomeres from seven photoreceptors being arranged in a trapezoid format. Expression of three human tau transgenic alleles, htauAP14 (GMR::htau-AP), htauWT (GMR::htau-WT), and htauE14 (GMR::htau-E14), produce different degrees of eye phenotypes and the severity ranking of eye defect is htauE14 > htauWT > htauAP14 that is based on external eye size and roughness and the internal organization of photoreceptor cells (a, b). Scale bars 10 μm. c Representative confocal images of control DA neurons marked with mCD8-GFP (TH::GFP), or co-expressing with either of the three human tau alleles (htauAP14, TH::htau-AP; htauWT, TH::htau-WT; and htauE14, TH::htau-E14) from 1-, 2-, and 4-week-old brains. Circles indicate the PPL1 cluster. d Quantitative analysis presents DA neuron numbers in PPL1 cluster at different ages from control and three tau alleles. TH::GFP (purple), TH::htau-AP (green), TH::htau-WT (yellow) and TH::htau-E14 (red). Values shown represent mean ± SEM (unpaired t test compares individual tau allele to control in the age-indicated groups; **P < 0.001; ***P < 0.0001, n = 12)
It is possible that the severe neuronal phenotype induced by htauAP is a developmental, but not a degenerative event. To circumvent potential developmental effects of htauAP on DA neurons, we used a conditional expression system by incorporating temperature-sensitive GAL80ts [27] in our model to predominantly, if not exclusively, expressing htauAP in adult brains. By shifting temperature from 25 to 29 °C for newly enclosed adult flies. We induced transgene expressing, and observed that adult onset of htauAP expression (GAL80 ts/UAS-htau AP; TH-GAL4, UAS-CD8GFP/+) induced severe neurodegeneration, similar to that of the continuously expression of htauAP (TH::htauAP, GFP), while the control flies (TH::GFP) exhibited normal DA neurons (Fig. S6). Therefore, these data suggest the effect of htauAP on DA neuron was an age-dependent degeneration, but not a developmental defect.
Loss of vesicular dopamine release preceded tauopathy and neurodegeneration
Previously, we have shown that vesicular monoamine transporter (VMAT) reduced environmental toxins and mutant human parkin-induced toxicity [26, 44]. We reasoned that the loss of DA neurons resulting from the expression of human tau may be associated with a change in the DA storage and release machinery. To investigate this, we used the ecliptic VMAT-pHluorin, with a pH-sensitive GFP conjugated in the first luminal loop of the 12 trans-membrane domains of VMAT to visualize the release of VMAT-pHluorin containing synaptic vesicle released to nerve terminals [34].
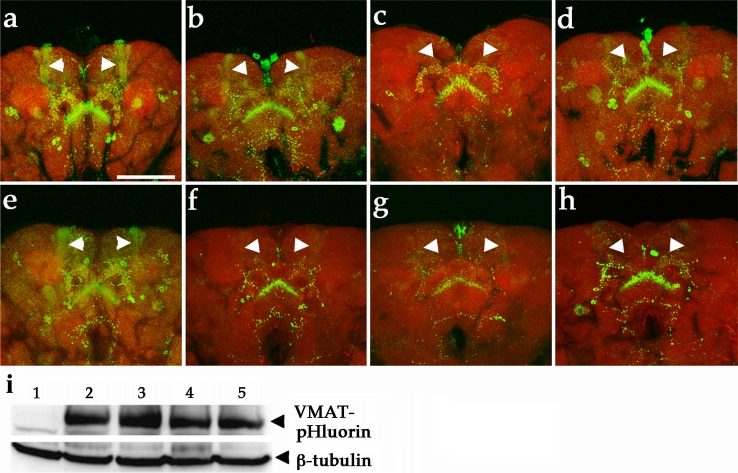
In wild-type fly brain, VMAT-pHluorin visualizes the synaptic vesicle-releasing regions of DA neurons in the fly brain. At one day after eclosion, VMAT was observed in many brain regions, including mushroom bodies, the fan-shaped body, and the protocerebral bridge, in wild-type flies (Fig. 6a) [31]. The single neuron of PPL1 and PPM3 data has been deposited in the database of Drosophila neurons (http://www.flycircuit.tw). In contrast, the localization of VMAT to the mushroom body and protocerebral bridge was reduced in age-matched flies expressing htauWT (Fig. 6b). This decrease was most pronounced in 3-week-old fly brains compared to the wild-type fly brain (Fig. 6e, f). Remarkably, the VMAT-pHluorin signals in the mushroom body and protocerebral bridge were selectively absent from the htauAP brains at one-day post-eclosion, but remained prominent in controls (Fig. 6a, c). Interestingly, some neurons that project to the fan-shaped body appeared to be unaffected, as the VMAT-pHluorin signal appeared normal in both control and three htau (htauWT, htauAP and htauE14) expressing brains. Given that some TH-GAL4-marked neurons are not dopaminergic, we suspect that the unaffected VMAT-pHluorin labeling of the fan-shaped body might be a result of expression in those cells. To further investigate whether declines in VMAT-pHluorin localization to nerve terminals were indeed related to human tau-induced toxicity, DA neurons expressing of htauWT, htauAP, or htauE14, were compared in different ages (Fig. 6a–h). Surprisingly, the age-matched flies expressing htauAP had earlier and more profound loss of VMAT-pHluorin signals (Fig. 6c) than flies expressing htauWT or htauE14 (Fig. 6b, d). Variation in the GFP signals in brains co-expressing VMAT-pHluorin and htauWT or htauAP were not a result of variation in levels of VMAT-pHluorin expression, since levels of VMAT-pHluorin were similar in both experimental and control groups (Fig. 6i).
Fig. 6.
DA neurons expressing htauWT cause early impairment of vesicular dopamine release to nerve terminals as visualized by VMAT-pHluorin. a–f Confocal images of DA neurons from brains of 1-day-old (a–d) and 3-week-old (e–h) flies show VMAT-pHluorin reporter (green). a DA neurons expressing VMAT-pHluorin (TH::VMAT-pHluorin) reveal localization of VMAT-pHluorin to presynaptic terminals in brain regions, and b age-matched DA neurons co-expressed VMAT-pHluorin and htauWT (TH::VMAT-pHluorin, UAS-htauWT) show decreased GFP signals in mushroom bodies (arrowheads). e A representative confocal image shows the VMAT-pHluorin signals to mushroom bodies and other brain structure remains prominent (green) in 3-week-old control brain, while the GFP signals localized to mushroom bodies is diminished in DA neurons expressing htauWT (f, arrowheads). c, g Expression of htauAP evokes severe loss of pHluorin signaling compared to age-matched tauWT (b, f) and TauE14 (d, h). Rhodamine-phalloidin (red) marks the brain structure. Scale bar 100 μm. i Representative western blot shows the expression levels of VMAT-pHlurion of 1-week-old fly brains in control and experiment groups. 1 TH-GAL4, 2 TH::VMAT-pHluorin, 3 TH::VMAT-pHluorin, htauWT, 4 TH::VMAT-pHluorin, htauAP, 5 TH::VMAT-pHluorin, htauE14. Anti-β-tubulin served as a loading control
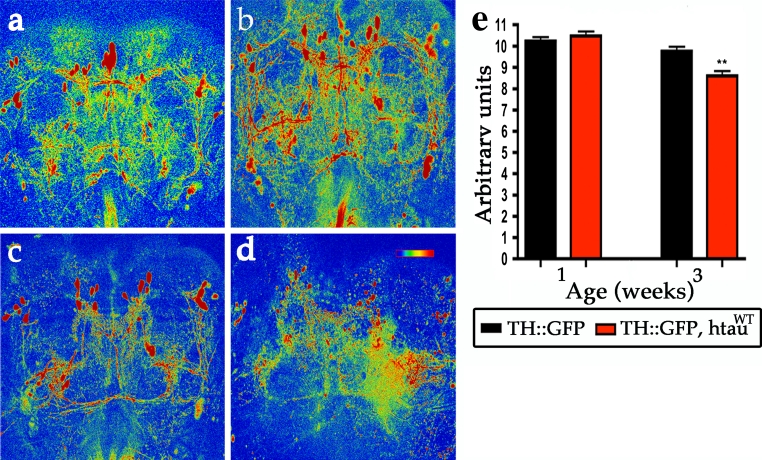
It is possible that htau could cause a general dysfunction of DA neurons resulting in multiple deficits in the DA release machinery. To determine whether expression of htauWT also disrupts calcium influx, we used a calcium-sensitive fluorescent protein, G-CaMP, to monitor changes in calcium. By visualizing 1-week-old live brains, we found that expression of htauWT did not alter the G-CaMP activity, compared to controls (Fig. 7a, b, e), suggesting that htauWT expression did not disrupt the general function of DA neurons during neuronal activation. However, at 3 weeks, we found that DA neurons expressing htauWT showed a minor but significant reduction of the G-CaMP signal compared to controls (Fig. 7c–e), consistent with overt DA neuronal degeneration around this age (Fig 7c–e). In conclusion, these results suggest htauWT inhibits the VMAT-containing synaptic vesicle release to neuronal processes, before overt neuronal degeneration.
Fig. 7.
Expression of htauWT causes age-dependent loss of G-CaMP activities. G-CaMP signal reveals Ca2+ activity in control DA neurons (TH::G-CaMP) from 1-week-old (a) and 3-week-old (c) flies. Expression of htauWT shows comparable G-CaMP signals compared to control group at 1 week (b), but the signals are reduced 10 % at 3 weeks (d). The G-CaMP activities are represented by thermal color from the higher (red) to lower intensity (blue). Scale bar 100 μm. e Quantitative analysis shows G-CaMP activities in control brains (TH::G-CaMP, black bars) and in htauWT brains (TH::G-CaMP, htauWT, red bars) at indicated ages. Values shown represent Mean ± SEM (unpaired t test; **P < 0.001)
Discussion
In the present study, we used Drosophila DA neurons as a model to examine the pathogenic mechanism of PD-linked tauopathies. Expression of htauWT in these neurons resulted in age-dependent, progressive neurodegeneration and the deposition of abnormal polymeric tau protein aggregates. Systematic characterizations of functional, pathological, and behavioral readouts from these htauWT flies at different ages demonstrate a plausible pathogenic link between tau and vesicular DA release, as demonstrated by a fluorescent VMAT-pHluorin marker in the synaptic vesicle-releasing sites of DA neurons. This defect represents the earliest pathological manifestation that precedes the robust pathophysiological phenotypes and suggests that a functional inhibition of DA neurotransmission is a prelude of the hallmark lesions in our PD model.
The molecular components of DA signaling and homeostasis in Drosophila are similar to those in humans; both human and fly DA neurons express two types of transporters: (1) a vesicular monoamine transporter for transport of DA from the cytosol to the lumen of secretory vesicles [29]; (2) a plasma membrane DA transporter (DAT) for reuptake of exocytosed DA [18]. Therefore, despite the anatomical differences, Drosophila models of PD, as well as other human neurological disorders, can help contribute to our understanding of the pathogenic mechanism underlying these diseases [6]. This tau-PD Drosophila model is the first animal model to demonstrate that tau expression can cause degeneration of DA neurons, a hallmark of Parkinson’s disease.
Most motor symptoms and mild cognitive impairment of PD result primarily from progressive degeneration of DA neurons in the substantia nigra, but the mechanism through which pathogenic factors target DA neurons is not completely understood. While several toxic compounds are known to produce PD symptoms in animal models, only MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) has been firmly established as a cause of selective DA neuron toxicity. The issue of neuronal vulnerability, in terms of transporter or transmission mechanisms among individuals with monogenic PD risk factors, has rarely been addressed directly. One exception is a study that showed that the expression of human α-synuclein in mice inhibited DA transmission by reducing the recycling of synaptic vesicles [37]. In addition, an association between DA metabolism and the death of DA neurons in PD has been postulated, and this association has been demonstrated in a α-synuclein PD model. Oxidative metabolites of DA may conjugate with α-synuclein to form an adduct of DA–α-synuclein, which may stabilize the toxic form of α-synuclein through covalent bound to DA quinone [11], while also promoting selective neurotoxicity [58]. Tau protein is ubiquitous in the brain, and has been shown to affect different types of neurons in various cell and animal models. A previous study showed that DA quinones, toxic metabolites that lead to PD, could promote the assembly of tau into fibrillar polymeric tau in vitro [15] which suggests a potential interplay between DA and tau in vivo and may provide a basis for the vulnerability of DA neurons.
One of the common themes of tau pathology is abnormal hyperphosphorylation of tau, originally identified in AD patients. However, the role of tau hyperphosphorylation in the pathophysiology of disease remains debated. In Drosophila photoreceptors, tau hyperphosphorylation is correlated with phenotypic severity [49], similar to the results observed in this study. However, we also determined that in DA neurons, the hypophosphorylated AP mutation increases toxicity while the hyperphosphorylated E14 mutation reduces toxicity. These data indicate that tau pathogenesis is likely influenced by multiple pathological mechanisms, because its phosphorylation mutations in DA and histaminergic neurons produce contrasting results. The hyperphosphorylation E14 mutation has a reduced binding affinity for microtubules, whereas the hypophosphorylation AP mutation has an increased affinity for microtubules. Thus, we suspect that hypophosphorylation AP tau mutation may profoundly block axonal transport and consequently inhibit synaptic vesicle transport. These notions raise the possibility that microtubule bound tau may partially contribute to tau pathogenesis in DA neurons due to its association with severity of phenotype in DA neurons; they are consistent with the concept that tau can compete with microtubule motor proteins and lead to the detachment of motor proteins (kinesin and dynein), which may lead to abnormal axonal trafficking [51]. However, since this tauAP is a tool to study the relationship of dephosphorylation state and disease severity in Drosophila, it may have little relevance to pathophysiology of tau in PD because tau is likely hyperphosphorylated in PD. Although the precise pathogenic mechanism of tau on DA neuron degeneration remains unclear, tau may interfere with the transport of synaptic vesicles and organelles such as mitochondria along microtubules [30]. Interestingly, when tau was overexpressed in photoreceptors at late pupal stage, we observed that transport of rhodopsin to the photosensitive membrane, rhabdomere, was inhibited (Fig. S7). Here, we show that the localization of VMAT to nerve terminals is also impeded. VMATs have been shown to exert neuroprotective effects in DA neurons in both flies [26] and mammals presumably via sequestration of cytosolic DA [19, 35]. We postulate that decreased localization of VMAT to the nerve terminal caused by tau could contribute to the pathogenesis of PD.
We show that the expression of human tau evokes aberrant polymeric tau formation, during which PHF-like aggregates accumulate and NFT-like tangles develop in DA neurons; this occurs in an age-dependent manner. This is the first longitudinal study to directly examine tau tangle formation and other pathogenesis in DA neurons. In contrast to previous studies which show that tauopathy can evoke neuronal degeneration but cannot form neurofibrillary tangles in other types of neurons in Drosophila and Caenorhabditis [24, 56]; our results suggest that human tau can produce tangle pathology in DA neurons, similar to the tau neurofibrillary tangles seen in PD patients. We suspect that the difference of tau manifestations is likely due to dopamine modifications and perhaps different amount of tau proteins in each neuron and believe that our tau-PD Drosophila model offers a robust animal model that can facilitate to investigate modification of tau pathogenesis.
Our neuropathological observations reveal at least two distinct molecular mechanisms of tau pathogenesis in DA neurons for PD. We show that failure of VMAT-containing synaptic vesicle release to nerve terminals is an early pathogenic manifestation, and the formation of neurofibrillary tangle-like pathology in the soma of DA neurons is a late-stage of tauopathy, providing pathological evidence for why MAPT may be a strong risk factor for idiopathic PD. The correction or prevention of the deficit in vesicular DA storage may be appropriate target for early therapeutic intervention.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 Expression of htauG272V and htauR406W cause DA neuron degeneration similar to htauWT. Related to Fig 1. (a) A depicted human tau isoform with 441 amino acids. The N domains are shown in white boxes and the C-terminal microtubule binding repeats are shown in black boxes with labeled as R1-R4. Two FTDP-17 associated mutations, G272V and R406W, are indicated. (b-e) Representative confocal images show mCD8-GFP-marked DA neurons in four-week-old control fly brain (b, TH::mCD8-GFP), and age-matched brains from flies expressing htauWT (c, TH:: htauWT, mCD8-GFP), htauG272V (d, TH:: htauG272V, mCD8-GFP), and htauR406W (e, TH:: htauR406W, mCD8-GFP). Two clusters of DA neurons, PPL1 (circles) and PPM3 (squares), are indicated. (f) Representative western blot shows protein levels of htauWT, htauG272V, and htauR406W that expressing in DA neurons. No human tau proteins can be detected in TH::mCD8-GFP and UAS-htauWT controls. β-Tubulin serves as a loading control. (g) Quantification of four independent western blots. Values shown represent Mean ± SEM; one-way ANOVA, P = 0.6185; ns, not significant. (TIFF 3756 kb)
Supplementary material 2 Expression of htauWT activates cell death signaling. (a) Representative immunoblot shows increased cytochrome c and activated caspase 3-like caspase in brains with DA neurons that expressing htauWT (TH::htauWT) compared to age-matched control (TH::GFP). The decrease of caspase 3-like signal at the fourth week is likely influenced by DA neuron loss by this age. Anti-ß-tubulin serves as a loading control. Quantification from four independent immunoblots shows expression levels of cytochrome c (b) and activated caspase 3 (c) represented as relative expression. Values shown represent Mean ± SEM. (TIFF 923 kb)
Supplementary material 3 Expression of htauWT in DA and 5HT neurons also induced DA neuron degeneration. Related to Fig 1. (a) Representative confocal images of control fly brains (left panels, DDC::mCD8-GFP) and brains expressing htauWT (right panels, DDC::htauWT, mCD8-GFP) at different ages (weeks numbered in the upper right corner of the left panels) stained with anti-tyrosine hydroxylase (anti-TH, red). PPM2 clusters of DA neurons (circles) are marked with both anti-TH and GFP (yellow). Scale bar, 50 µm. (b) Immunoblotting of a polyclonal Tau antibody (against the C-terminal amino acids 243-441) detects a 75 kDa band in DDC:: htauWT, but not in DDC-GAL4 or UAS-htauWT controls. Anti-tubulin served as a loading control. (c) Quantitative analysis shows the number of DA neurons in PPM2 clusters in htauWT (pink) and control (green) at indicated ages. Values shown represent Mean ± SEM (unpaired t-test, *P < 0.01; ** P < 0.001; ***P < 0.0001, n = 10). (TIFF 2561 kb)
Supplementary material 4 The time course of developing tangle-like pathology in the degenerating DA neurons and the effect of htauWT on other types of neurons. Related to Figure 4. (a) Confocal images focusing at a single DA neuron from control (TH::mCD8-GFP) and htauWT expressing (TH-GAL4:: UAS-htauWT, mCD8-GFP) brains at indicated ages (in week indicated at the lower left corner of row). GFP-marked DA neuron in control brains shows comparable soma size at different ages (a), while DA neuron expressing htauWT reveals progressive reduction of soma size as well as the formation of tangle-like pathology extended from the soma begin at approximate 3 weeks of age, featured by AD-like hyperphosphorylated tau antibodies AT8 and AT180 staining and a polyclonal Tau antibody (a). (b) Confocal images of a single DA neuron marked by actin-GFP reveal edges of the soma are associated with actin rich puncta in the control brain (TH::actin-GFP), but are absent of these actin rich puncta on the surface of the soma in the htauWT expressing brain. Confocal images of AT8 immunostaining show the fragmented axonal branches (arrows) at 4 weeks (c) and 6 weeks (d) htauWT expressing DA neurons. (e) Other types of neurons expressing htauWT show comparable soma size and shape (right panels) as compared to normal glutamatergic (top row), GABAergic (second row from top) and NPF (bottom row) neurons (left panels). In contrast, 5HT neurons expressing htauWT show reduction in soma size and morphological change, similar to that of DA neurons in 6-week-old flies. Scale bar, 10 µm. (TIFF 3941 kb)
Supplementary material 5 Analysis of phosphorylation states of htauWT proteins and protein levels of three human tau alleles: htauAP, htauWT, and htauE14 in DA neurons. (a) Representative western blot shows expression of htauWT protein in DA neurons were phosphorylated (-) and the migration in SDS-PAGE is slower than those htauWT proteins treated with alkaline phosphatase (+). No human tau proteins can be detected in control TH::GFP. β-Tubulin serves as a loading control. (b) Representative western blot shows protein levels of three htau alleles in DA neurons: htauWT (TH::mCD8-GFP, htauWT), htauAP (TH::mCD8-GFP, htauAP), and htauE14 (TH::mCD8-GFP, htauE14). β-Tubulin serves as a loading control. (c) Quantification of three independent western blots. Values shown represent Mean ± SEM; one-way ANOVA, P = 0.925; n = 3). (TIFF 474 kb)
Supplementary material 6 Adult onset of htauAP expression also produces severe age-dependent neurodegeneration. Related to Figure 5. (a) Representative western blot shows conditional expression of htauAP. At room temperature (25°C), tub-GAL80ts represses transgene expression, thus htauAP is silenced (TH::htauAP,mCD8-GFP/tubGAL80ts at 25°C); whereas at 29°C, tub-GAL80ts fails to repress transgene expression, thus the expression of htauAP transgene is detected (TH::htauAP, mCD8-GFP/tubGAL80ts at 29°C). No htauAP is detected in control (TH::mCD8-GFP). (b) Representative confocal images of PPL1 groups of DA neurons marked with mCD8-GFP (TH::GFP) in the control, conditional expression of htauAP in adult flies (TH::htauAP, mCD8-GFP/tubGAL80ts), or developmental expression of htauAP (TH::htauAP, mCD8-GFP) at indicated ages. Circles indicate the PPL1 clusters. (c) Quantitative analysis presents DA neuron numbers in PPL1 cluster at different ages (weeks) from control and htauAP with indicted expression regimes. TH:: mCD8-GFP (blue); TH::htauAP, mCD8-GFP/tubGAL80ts (yellow); TH::htauAP, mCD8-GFP (pink). Values shown represent Mean ± SEM (unpaired t test compares individual tau allele to the control in the age-matched groups; *P < 0.01; ***P < 0.0001, n = 12). (TIFF 1482 kb)
Supplementary material 7 Expression of htauWT causes the mislocalization of rhodopsin in photoreceptors. (a-c) Confocal images of control fly eyes (Rh1-GAL4) and eyes expressing htauWT (d-f, RH1::htauWT). Newly eclosed adult eyes are stained with anti-rhodopsin (4C5, green) and rhodamine-phalloidin (red). Aberrant accumulation of rhodopsin staining in htauWT eye (e) is evident as compared to control (b). Scale bar, 100 µm. (TIFF 8084 kb)
Acknowledgments
We thank J. Hirsh, R. Axel, M. Feany, J.-L. Juang, and Bloomington Drosophila Stock Center for fly strains. We are grateful to Tzu-Kang Sang and Don Ready for their critical comments and suggestions, and Horng-Dar Wang, Jui-Chou Hsu, Kathy Sang for their suggestions on this manuscript. We thank the support from Imaging Core of the Brain Research Center in National Tsing Hua University. This work is supported by National Science Council Grant 98-2311-B-007-014-MY3 and National Tsing Hua University Grant N2612E1 (H.-Y. C).
References
- 1.Aso Y, Herb A, Ogueta M, Siwanowicz I, Templier T, Friedrich AB, Ito K, Scholz H, Tanimoto H. Three dopamine pathways induce aversive odor memories with different stability. PLoS Genet. 2012;8:e1002768. doi: 10.1371/journal.pgen.1002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benzer S. Behavioral mutants of Drosophila isolated by countercurrent distribution. Proc Nat Acad Sci USA. 1967;58:1112–1119. doi: 10.1073/pnas.58.3.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berg I, Nilsson KP, Thor S, Hammarstrom P. Efficient imaging of amyloid deposits in Drosophila models of human amyloidoses. Nat Protoc. 2010;5:935–944. doi: 10.1038/nprot.2010.41. [DOI] [PubMed] [Google Scholar]
- 4.Berry JA, Cervantes-Sandoval I, Nicholas EP, Davis RL. Dopamine is required for learning and forgetting in Drosophila. Neuron. 2012;74:530–542. doi: 10.1016/j.neuron.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Binder LI, Guillozet-Bongaarts AL, Garcia-Sierra F, Berry RW. Tau, tangles, and Alzheimer’s disease. Biochim Biophys Acta. 2005;1739:216–223. doi: 10.1016/j.bbadis.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Bonini NM, Fortini ME. Human neurodegenerative disease modeling using Drosophila. Annu Rev Neurosci. 2003;26:627–656. doi: 10.1146/annurev.neuro.26.041002.131425. [DOI] [PubMed] [Google Scholar]
- 7.Burke CJ, Huetteroth W, Owald D, Perisse E, Krashes MJ, Das G, Gohl D, Sillies M, Certel S, Waddell S. Layered reward signalling through octopamine and dopamine in Drosophila. Nature. 2012;492:433–437. doi: 10.1038/nature11614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang HY, Grygoruk A, Brooks ES, Ackerson LC, Maidment NT, Bainton RL, Krantz DE. Overexpression of the Drosophila vesicular monoamine transporter increases motor activity and courtship but decreases the behavioral response to cocaine. Mol Psychiatr. 2006;11:99–113. doi: 10.1038/sj.mp.4001742. [DOI] [PubMed] [Google Scholar]
- 9.Chang HY, Ready DF. Rescue of photoreceptor degeneration in rhodopsin-null Drosophila mutants by activated Rac1. Science. 2000;290:1978–1980. doi: 10.1126/science.290.5498.1978. [DOI] [PubMed] [Google Scholar]
- 10.Chang YC, Hung WT, Chang YC, Chang HC, Wu CL, Chiang AS, Jackson GR, Sang TK. Pathogenic VCP/TER94 alleles are dominant actives and contribute to neurodegeneration by altering cellular ATP level in a Drosophila IBMPFD model. PLoS Genet. 2011;7:e1001288. doi: 10.1371/journal.pgen.1001288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conway KA, Rochet JC, Bieganski RM, Lansbury PT., Jr Kinetic stabilization of the alpha-synuclein protofibril by a dopamine-alpha-synuclein adduct. Science. 2001;294:1346–1349. doi: 10.1126/science.1063522. [DOI] [PubMed] [Google Scholar]
- 12.Crowther RA. Straight and paired helical filaments in Alzheimer disease have a common structural unit. Proc Nat Acad Sci USA. 1991;88:2288–2292. doi: 10.1073/pnas.88.6.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dawson TM, Ko HS, Dawson VL. Genetic animal models of Parkinson’s disease. Neuron. 2010;66:646–661. doi: 10.1016/j.neuron.2010.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Calignon A, Polydoro M, Suarez-Calvet M, William C, Adamowicz DH, Kopeikina KJ, Pitstick R, Sahara N, Ashe KH, Carlson GA, Spires-Jones TL, Hyman BT. Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron. 2012;73:685–697. doi: 10.1016/j.neuron.2011.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dixit R, Ross JL, Goldman YE, Holzbaur EL. Differential regulation of dynein and kinesin motor proteins by tau. Science. 2008;319:1086–1089. doi: 10.1126/science.1152993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edwards TL, Scott WK, Almonte C, Burt A, Powell EH, Beecham GW, Wang L, Zuchner S, Konidari I, Wang G, Singer C, Nahab F, Scott B, Stajich JM, Pericak-Vance M, Haines J, Vance JM, Martin E. Genome-wide association study confirms SNPs in SNCA and the MAPT region as common risk factors for Parkinson disease. Ann Hum Genet. 2010;74:97–109. doi: 10.1111/j.1469-1809.2009.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farrer M, Skipper L, Berg M, Bisceglio G, Hanson M, Hardy J, Adam A, Gwinn-Hardy K, Aasly J. The tau H1 haplotype is associated with Parkinson’s disease in the Norwegian population. Neurosci Lett. 2002;322:83–86. doi: 10.1016/S0304-3940(02)00106-4. [DOI] [PubMed] [Google Scholar]
- 18.Giros B, Jaber M, Jones SR, Wightman RM, Caron MG. Hyperlocomotion and indifference to cocaine and amphetamine in mice lacking the dopamine transporter. Nature. 1996;379:606–612. doi: 10.1038/379606a0. [DOI] [PubMed] [Google Scholar]
- 19.Guillot TS, Miller GW. Protective actions of the vesicular monoamine transporter 2 (VMAT2) in monoaminergic neurons. Mol Neurobiol. 2009;39:149–170. doi: 10.1007/s12035-009-8059-y. [DOI] [PubMed] [Google Scholar]
- 20.Hoglinger GU, Melhem NM, Dickson DW, Sleiman PM, Wang LS, Klei L, Rademakers R, de Silva R, Litvan I, Riley DE, van Swieten JC, Wszolek ZK, Uitti RJ, Vandrovcova J, Hurtig HI, Gross RG, Maetzler W, Goldwurm S, Tolosa E, Borroni B, Pastor P, Cantwell LB, Han MR, Dillman A, van der Brug MP, Gibbs JR, Cookson MR, Hernandez DG, Singleton AB, Farrer MJ, Yu CE, Golbe LI, Revesz T, Hardy J, Lees AJ, Devlin B, Hakonarson H, Muller U, Schellenberg GD. Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat Genet. 2011;43:699–705. doi: 10.1038/ng.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiat. 1992;55:181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hutton M, Lendon CL, Rizzu P, Baker M, Froelich S, Houlden H, Pickering-Brown S, Chakraverty S, Isaacs A, Grover A, Hackett J, Adamson J, Lincoln S, Dickson D, Davies P, Petersen RC, Stevens M, de Graaff E, Wauters E, van Baren J, Hillebrand M, Joosse M, Kwon JM, Nowotny P, Che LK, Norton J, Morris JC, Reed LA, Trojanowski J, Basun H, Lannfelt L, Neystat M, Fahn S, Dark F, Tannenberg T, Dodd PR, Hayward N, Kwok JB, Schofield PR, Andreadis A, Snowden J, Craufurd D, Neary D, Owen F, Oostra BA, Hardy J, Goate A, van Swieten J, Mann D, Lynch T, Heutink P. Association of missense and 5′-splice-site mutations in tau with the inherited dementia FTDP-17. Nature. 1998;393:702–705. doi: 10.1038/31508. [DOI] [PubMed] [Google Scholar]
- 23.Jackson GR, Wiedau-Pazos M, Sang TK, Wagle N, Brown CA, Massachi S, Geschwind DH. Human wild-type tau interacts with wingless pathway components and produces neurofibrillary pathology in Drosophila. Neuron. 2002;34:509–519. doi: 10.1016/S0896-6273(02)00706-7. [DOI] [PubMed] [Google Scholar]
- 24.Kraemer BC, Zhang B, Leverenz JB, Thomas JH, Trojanowski JQ, Schellenberg GD. Neurodegeneration and defective neurotransmission in a Caenorhabditis elegans model of tauopathy. Proc Nat Acad Sci USA. 2003;100:9980–9985. doi: 10.1073/pnas.1533448100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwok JB, Teber ET, Loy C, Hallupp M, Nicholson G, Mellick GD, Buchanan DD, Silburn PA, Schofield PR. Tau haplotypes regulate transcription and are associated with Parkinson’s disease. Ann Neurol. 2004;55:329–334. doi: 10.1002/ana.10826. [DOI] [PubMed] [Google Scholar]
- 26.Lawal HO, Chang HY, Terrell AN, Brooks ES, Pulido D, Simon AF, Krantz DE. The Drosophila vesicular monoamine transporter reduces pesticide-induced loss of dopaminergic neurons. Neurobiol Dis. 2010;40:102–112. doi: 10.1016/j.nbd.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee T, Luo L. Mosaic analysis with a repressible cell marker (MARCM) for Drosophila neural development. Trends Neurosci. 2001;24:251–254. doi: 10.1016/S0166-2236(00)01791-4. [DOI] [PubMed] [Google Scholar]
- 28.Lee VM, Goedert M, Trojanowski JQ. Neurodegenerative tauopathies. Annu Rev Neurosci. 2001;24:1121–1159. doi: 10.1146/annurev.neuro.24.1.1121. [DOI] [PubMed] [Google Scholar]
- 29.Liu Y, Edwards RH. The role of vesicular transport proteins in synaptic transmission and neural degeneration. Annu Rev Neurosci. 1997;20:125–156. doi: 10.1146/annurev.neuro.20.1.125. [DOI] [PubMed] [Google Scholar]
- 30.Mandelkow EM, Stamer K, Vogel R, Thies E, Mandelkow E. Clogging of axons by tau, inhibition of axonal traffic and starvation of synapses. Neurobiol Aging. 2003;24:1079–1085. doi: 10.1016/j.neurobiolaging.2003.04.007. [DOI] [PubMed] [Google Scholar]
- 31.Mao Z, Davis RL. Eight different types of dopaminergic neurons innervate the Drosophila mushroom body neuropil: anatomical and physiological heterogeneity. Front Neural Circ. 2009;3:5. doi: 10.3389/neuro.04.005.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maraganore DM, de Andrade M, Lesnick TG, Strain KJ, Farrer MJ, Rocca WA, Pant PV, Frazer KA, Cox DR, Ballinger DG. High-resolution whole-genome association study of Parkinson disease. Am J Hum Genet. 2005;77:685–693. doi: 10.1086/496902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mershin A, Pavlopoulos E, Fitch O, Braden BC, Nanopoulos DV, Skoulakis EM. Learning and memory deficits upon TAU accumulation in Drosophila mushroom body neurons. Learn Mem. 2004;11:277–287. doi: 10.1101/lm.70804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miesenbock G, De Angelis DA, Rothman JE. Visualizing secretion and synaptic transmission with pH-sensitive green fluorescent proteins. Nature. 1998;394:192–195. doi: 10.1038/28190. [DOI] [PubMed] [Google Scholar]
- 35.Mosharov EV, Larsen KE, Kanter E, Phillips KA, Wilson K, Schmitz Y, Krantz DE, Kobayashi K, Edwards RH, Sulzer D. Interplay between cytosolic dopamine, calcium, and alpha-synuclein causes selective death of substantia nigra neurons. Neuron. 2009;62:218–229. doi: 10.1016/j.neuron.2009.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Myers AJ, Pittman AM, Zhao AS, Rohrer K, Kaleem M, Marlowe L, Lees A, Leung D, McKeith IG, Perry RH, Morris CM, Trojanowski JQ, Clark C, Karlawish J, Arnold S, Forman MS, Van Deerlin V, de Silva R, Hardy J. The MAPT H1c risk haplotype is associated with increased expression of tau and especially of 4 repeat containing transcripts. Neurobiol Dis. 2007;25:561–570. doi: 10.1016/j.nbd.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 37.Nemani VM, Lu W, Berge V, Nakamura K, Onoa B, Lee MK, Chaudhry FA, Nicoll RA, Edwards RH. Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron. 2010;65:66–79. doi: 10.1016/j.neuron.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pankratz N, Wilk JB, Latourelle JC, DeStefano AL, Halter C, Pugh EW, Doheny KF, Gusella JF, Nichols WC, Foroud T, Myers RH. Genomewide association study for susceptibility genes contributing to familial Parkinson disease. Hum Genet. 2009;124:593–605. doi: 10.1007/s00439-008-0582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qin H, Cressy M, Li W, Coravos JS, Izzi SA, Dubnau J. Gamma neurons mediate dopaminergic input during aversive olfactory memory formation in Drosophila. Curr Biol. 2012;22:608–614. doi: 10.1016/j.cub.2012.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reiff DF, Ihring A, Guerrero G, Isacoff EY, Joesch M, Nakai J, Borst A. In vivo performance of genetically encoded indicators of neural activity in flies. J Neurosci. 2005;25:4766–4778. doi: 10.1523/JNEUROSCI.4900-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Riemensperger T, Isabel G, Coulom H, Neuser K, Seugnet L, Kume K, Iche-Torres M, Cassar M, Strauss R, Preat T, Hirsh J, Birman S. Behavioral consequences of dopamine deficiency in the Drosophila central nervous system. Proc Nat Acad Sci USA. 2011;108:834–839. doi: 10.1073/pnas.1010930108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Riemensperger T, Voller T, Stock P, Buchner E, Fiala A. Punishment prediction by dopaminergic neurons in Drosophila. Curr Biol. 2005;15:1953–1960. doi: 10.1016/j.cub.2005.09.042. [DOI] [PubMed] [Google Scholar]
- 43.Rovelet-Lecrux A, Hannequin D, Raux G, Le Meur N, Laquerriere A, Vital A, Dumanchin C, Feuillette S, Brice A, Vercelletto M, Dubas F, Frebourg T, Campion D. APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet. 2006;38:24–26. doi: 10.1038/ng1718. [DOI] [PubMed] [Google Scholar]
- 44.Sang TK, Chang HY, Lawless GM, Ratnaparkhi A, Mee L, Ackerson LC, Maidment NT, Krantz DE, Jackson GR. A Drosophila model of mutant human parkin-induced toxicity demonstrates selective loss of dopaminergic neurons and dependence on cellular dopamine. J Neurosci. 2007;27:981–992. doi: 10.1523/JNEUROSCI.4810-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shulman JM, De Jager PL, Feany MB. Parkinson’s disease: genetics and pathogenesis. Annu Rev Pathol. 2011;6:193–222. doi: 10.1146/annurev-pathol-011110-130242. [DOI] [PubMed] [Google Scholar]
- 46.Simon-Sanchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, Berg D, Paisan-Ruiz C, Lichtner P, Scholz SW, Hernandez DG, Kruger R, Federoff M, Klein C, Goate A, Perlmutter J, Bonin M, Nalls MA, Illig T, Gieger C, Houlden H, Steffens M, Okun MS, Racette BA, Cookson MR, Foote KD, Fernandez HH, Schreiber S, Arepalli S, Zonozi R, Gwinn K, van der Brug M, Lopez G, Chanock SJ, Schatzkin A, Park Y, Hollenbeck A, Gao J, Huang X, Wood NW, Lorenz D, Deuschl G, Chen H, Riess O, Hardy JA, Singleton AB, Gasser T. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat Genet. 2009;41:1308–1312. doi: 10.1038/ng.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singleton AB, Farrer M, Johnson J, Singleton A, Hague S, Kachergus J, Hulihan M, Peuralinna T, Dutra A, Nussbaum R, Lincoln S, Crawley A, Hanson M, Maraganore D, Adler C, Cookson MR, Muenter M, Baptista M, Miller D, Blancato J, Hardy J, Gwinn-Hardy K. alpha-Synuclein locus triplication causes Parkinson’s disease. Science. 2003;302:841. doi: 10.1126/science.1090278. [DOI] [PubMed] [Google Scholar]
- 48.Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M. Alpha-synuclein in Lewy bodies. Nature. 1997;388:839–840. doi: 10.1038/42166. [DOI] [PubMed] [Google Scholar]
- 49.Steinhilb ML, Dias-Santagata D, Fulga TA, Felch DL, Feany MB. Tau phosphorylation sites work in concert to promote neurotoxicity in vivo. Mol Biol Cell. 2007;18:5060–5068. doi: 10.1091/mbc.E07-04-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steinhilb ML, Dias-Santagata D, Mulkearns EE, Shulman JM, Biernat J, Mandelkow EM, Feany MB. S/P and T/P phosphorylation is critical for tau neurotoxicity in Drosophila. J Neurosci Res. 2007;85:1271–1278. doi: 10.1002/jnr.21232. [DOI] [PubMed] [Google Scholar]
- 51.Talmat-Amar Y, Arribat Y, Redt-Clouet C, Feuillette S, Bouge AL, Lecourtois M, Parmentier ML. Important neuronal toxicity of microtubule-bound Tau in vivo in Drosophila. Hum Mol Genet. 2011;20:3738–3745. doi: 10.1093/hmg/ddr290. [DOI] [PubMed] [Google Scholar]
- 52.Tully T, Quinn WG. Classical conditioning and retention in normal and mutant Drosophila melanogaster. J Comp Physiol A Sens Neural Behav Physiol. 1985;157:263–277. doi: 10.1007/BF01350033. [DOI] [PubMed] [Google Scholar]
- 53.Varkey J, Chen P, Jemmerson R, Abrams JM. Altered cytochrome c display precedes apoptotic cell death in Drosophila. J Cell Biol. 1999;144:701–710. doi: 10.1083/jcb.144.4.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang JW, Wong AM, Flores J, Vosshall LB, Axel R. Two-photon calcium imaging reveals an odor-evoked map of activity in the fly brain. Cell. 2003;112:271–282. doi: 10.1016/S0092-8674(03)00004-7. [DOI] [PubMed] [Google Scholar]
- 55.Williams-Gray CH, Evans JR, Goris A, Foltynie T, Ban M, Robbins TW, Brayne C, Kolachana BS, Weinberger DR, Sawcer SJ, Barker RA. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the Campaign cohort. Brain. 2009;132:2958–2969. doi: 10.1093/brain/awp245. [DOI] [PubMed] [Google Scholar]
- 56.Wittmann CW, Wszolek MF, Shulman JM, Salvaterra PM, Lewis J, Hutton M, Feany MB. Tauopathy in Drosophila: neurodegeneration without neurofibrillary tangles. Science. 2001;293:711–714. doi: 10.1126/science.1062382. [DOI] [PubMed] [Google Scholar]
- 57.Wray S, Lewis PA. A tangled web—tau and sporadic Parkinson’s disease. Front Psychiat. 2010;1:150. doi: 10.3389/fpsyt.2010.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu J, Kao SY, Lee FJ, Song W, Jin LW, Yankner BA. Dopamine-dependent neurotoxicity of alpha-synuclein: a mechanism for selective neurodegeneration in Parkinson disease. Nat Med. 2002;8:600–606. doi: 10.1038/nm0602-600. [DOI] [PubMed] [Google Scholar]
- 59.Zabetian CP, Hutter CM, Factor SA, Nutt JG, Higgins DS, Griffith A, Roberts JW, Leis BC, Kay DM, Yearout D, Montimurro JS, Edwards KL, Samii A, Payami H. Association analysis of MAPT H1 haplotype and subhaplotypes in Parkinson’s disease. Ann Neurol. 2007;62:137–144. doi: 10.1002/ana.21157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zimprich A, Biskup S, Leitner P, Lichtner P, Farrer M, Lincoln S, Kachergus J, Hulihan M, Uitti RJ, Calne DB, Stoessl AJ, Pfeiffer RF, Patenge N, Carbajal IC, Vieregge P, Asmus F, Muller-Myhsok B, Dickson DW, Meitinger T, Strom TM, Wszolek ZK, Gasser T. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron. 2004;44:601–607. doi: 10.1016/j.neuron.2004.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1 Expression of htauG272V and htauR406W cause DA neuron degeneration similar to htauWT. Related to Fig 1. (a) A depicted human tau isoform with 441 amino acids. The N domains are shown in white boxes and the C-terminal microtubule binding repeats are shown in black boxes with labeled as R1-R4. Two FTDP-17 associated mutations, G272V and R406W, are indicated. (b-e) Representative confocal images show mCD8-GFP-marked DA neurons in four-week-old control fly brain (b, TH::mCD8-GFP), and age-matched brains from flies expressing htauWT (c, TH:: htauWT, mCD8-GFP), htauG272V (d, TH:: htauG272V, mCD8-GFP), and htauR406W (e, TH:: htauR406W, mCD8-GFP). Two clusters of DA neurons, PPL1 (circles) and PPM3 (squares), are indicated. (f) Representative western blot shows protein levels of htauWT, htauG272V, and htauR406W that expressing in DA neurons. No human tau proteins can be detected in TH::mCD8-GFP and UAS-htauWT controls. β-Tubulin serves as a loading control. (g) Quantification of four independent western blots. Values shown represent Mean ± SEM; one-way ANOVA, P = 0.6185; ns, not significant. (TIFF 3756 kb)
Supplementary material 2 Expression of htauWT activates cell death signaling. (a) Representative immunoblot shows increased cytochrome c and activated caspase 3-like caspase in brains with DA neurons that expressing htauWT (TH::htauWT) compared to age-matched control (TH::GFP). The decrease of caspase 3-like signal at the fourth week is likely influenced by DA neuron loss by this age. Anti-ß-tubulin serves as a loading control. Quantification from four independent immunoblots shows expression levels of cytochrome c (b) and activated caspase 3 (c) represented as relative expression. Values shown represent Mean ± SEM. (TIFF 923 kb)
Supplementary material 3 Expression of htauWT in DA and 5HT neurons also induced DA neuron degeneration. Related to Fig 1. (a) Representative confocal images of control fly brains (left panels, DDC::mCD8-GFP) and brains expressing htauWT (right panels, DDC::htauWT, mCD8-GFP) at different ages (weeks numbered in the upper right corner of the left panels) stained with anti-tyrosine hydroxylase (anti-TH, red). PPM2 clusters of DA neurons (circles) are marked with both anti-TH and GFP (yellow). Scale bar, 50 µm. (b) Immunoblotting of a polyclonal Tau antibody (against the C-terminal amino acids 243-441) detects a 75 kDa band in DDC:: htauWT, but not in DDC-GAL4 or UAS-htauWT controls. Anti-tubulin served as a loading control. (c) Quantitative analysis shows the number of DA neurons in PPM2 clusters in htauWT (pink) and control (green) at indicated ages. Values shown represent Mean ± SEM (unpaired t-test, *P < 0.01; ** P < 0.001; ***P < 0.0001, n = 10). (TIFF 2561 kb)
Supplementary material 4 The time course of developing tangle-like pathology in the degenerating DA neurons and the effect of htauWT on other types of neurons. Related to Figure 4. (a) Confocal images focusing at a single DA neuron from control (TH::mCD8-GFP) and htauWT expressing (TH-GAL4:: UAS-htauWT, mCD8-GFP) brains at indicated ages (in week indicated at the lower left corner of row). GFP-marked DA neuron in control brains shows comparable soma size at different ages (a), while DA neuron expressing htauWT reveals progressive reduction of soma size as well as the formation of tangle-like pathology extended from the soma begin at approximate 3 weeks of age, featured by AD-like hyperphosphorylated tau antibodies AT8 and AT180 staining and a polyclonal Tau antibody (a). (b) Confocal images of a single DA neuron marked by actin-GFP reveal edges of the soma are associated with actin rich puncta in the control brain (TH::actin-GFP), but are absent of these actin rich puncta on the surface of the soma in the htauWT expressing brain. Confocal images of AT8 immunostaining show the fragmented axonal branches (arrows) at 4 weeks (c) and 6 weeks (d) htauWT expressing DA neurons. (e) Other types of neurons expressing htauWT show comparable soma size and shape (right panels) as compared to normal glutamatergic (top row), GABAergic (second row from top) and NPF (bottom row) neurons (left panels). In contrast, 5HT neurons expressing htauWT show reduction in soma size and morphological change, similar to that of DA neurons in 6-week-old flies. Scale bar, 10 µm. (TIFF 3941 kb)
Supplementary material 5 Analysis of phosphorylation states of htauWT proteins and protein levels of three human tau alleles: htauAP, htauWT, and htauE14 in DA neurons. (a) Representative western blot shows expression of htauWT protein in DA neurons were phosphorylated (-) and the migration in SDS-PAGE is slower than those htauWT proteins treated with alkaline phosphatase (+). No human tau proteins can be detected in control TH::GFP. β-Tubulin serves as a loading control. (b) Representative western blot shows protein levels of three htau alleles in DA neurons: htauWT (TH::mCD8-GFP, htauWT), htauAP (TH::mCD8-GFP, htauAP), and htauE14 (TH::mCD8-GFP, htauE14). β-Tubulin serves as a loading control. (c) Quantification of three independent western blots. Values shown represent Mean ± SEM; one-way ANOVA, P = 0.925; n = 3). (TIFF 474 kb)
Supplementary material 6 Adult onset of htauAP expression also produces severe age-dependent neurodegeneration. Related to Figure 5. (a) Representative western blot shows conditional expression of htauAP. At room temperature (25°C), tub-GAL80ts represses transgene expression, thus htauAP is silenced (TH::htauAP,mCD8-GFP/tubGAL80ts at 25°C); whereas at 29°C, tub-GAL80ts fails to repress transgene expression, thus the expression of htauAP transgene is detected (TH::htauAP, mCD8-GFP/tubGAL80ts at 29°C). No htauAP is detected in control (TH::mCD8-GFP). (b) Representative confocal images of PPL1 groups of DA neurons marked with mCD8-GFP (TH::GFP) in the control, conditional expression of htauAP in adult flies (TH::htauAP, mCD8-GFP/tubGAL80ts), or developmental expression of htauAP (TH::htauAP, mCD8-GFP) at indicated ages. Circles indicate the PPL1 clusters. (c) Quantitative analysis presents DA neuron numbers in PPL1 cluster at different ages (weeks) from control and htauAP with indicted expression regimes. TH:: mCD8-GFP (blue); TH::htauAP, mCD8-GFP/tubGAL80ts (yellow); TH::htauAP, mCD8-GFP (pink). Values shown represent Mean ± SEM (unpaired t test compares individual tau allele to the control in the age-matched groups; *P < 0.01; ***P < 0.0001, n = 12). (TIFF 1482 kb)
Supplementary material 7 Expression of htauWT causes the mislocalization of rhodopsin in photoreceptors. (a-c) Confocal images of control fly eyes (Rh1-GAL4) and eyes expressing htauWT (d-f, RH1::htauWT). Newly eclosed adult eyes are stained with anti-rhodopsin (4C5, green) and rhodamine-phalloidin (red). Aberrant accumulation of rhodopsin staining in htauWT eye (e) is evident as compared to control (b). Scale bar, 100 µm. (TIFF 8084 kb)