Abstract
Previously the National Health and Examination Survey measured physical activity with an accelerometer worn on the hip for seven days, but recently changed the location of the monitor to the wrist.
PURPOSE
This study compared estimates of physical activity intensity and type with an accelerometer on the hip versus the wrist.
METHODS
Healthy adults (n=37) wore triaxial accelerometers (Wockets) on the hip and dominant wrist along with a portable metabolic unit to measure energy expenditure during 20 activities. Motion summary counts were created, then receiver operating characteristic (ROC) curves were used to determine sedentary and activity intensity thresholds. Ambulatory activities were separated from other activities using the coefficient of variation (CV) of the counts. Mixed model predictions were used to estimate activity intensity.
RESULTS
The ROC for determining sedentary behavior had greater sensitivity and specificity (71% and 96%) at the hip than the wrist (53% and 76%), as did the ROC for moderate to vigorous physical activity on the hip (70% and 83%) versus the wrist (30% and 69%). The ROC for the CV associated with ambulation had a larger AUC at the hip compared to the wrist (0.83 and 0.74). The prediction model for activity energy expenditure (AEE) resulted in an average difference of 0.55 (+/− 0.55) METs on the hip and 0.82 (+/− 0.93) METs on the wrist.
CONCLUSIONS
Methods frequently used for estimating AEE and identifying activity intensity thresholds from an accelerometer on the hip generally do better than similar data from an accelerometer on the wrist. Accurately identifying sedentary behavior from a lack of wrist motion presents significant challenges.
Keywords: Activity monitor, accelerometer, mobile phones, thresholds, coefficient of variation, sedentary behavior, exercise
Introduction
Accelerometer-based measurements of physical activity and sedentary behavior play an increasingly important role in observational and experimental studies evaluating habitual physical activity. Most of these data have been collected with an accelerometer worn at the hip and typically for a period of seven days. The National Health and Nutrition Examination Survey (NHANES) previously relied on an accelerometer worn on the hip to measure physical activity and sedentary behavior (43). The NHANES investigators recently made a decision to measure physical activity with an accelerometer on the wrist instead of the original hip location. Early results indicated data collection on the wrist has greater user acceptability, assuming this leads to greater compliance to the protocol (44). The measurement from the accelerometer output typically has been a summary of motion (counts), and calibration studies have shown the relationship between counts and intensity of activity (sedentary, light, moderate and vigorous intensities) or activity energy expenditure (AEE) (7, 15, 29). Calibration of the Actigraph (Actigraph, Pensacola, FL) - the accelerometer used in NHANES - has been conducted using the hip location as the measurement standard. Several studies have evaluated accelerometers at other locations such as the wrist (5, 34, 37, 41) or ankle (14), but until recently (45), no studies used contemporary calibration methods for estimating activity intensity thresholds and AEE from measurements made at the hip compared to the wrist. Zhang and colleagues examined the use of multiple features extracted from a raw signal from accelerometers on the hip and wrist to classify activities into one of four categories, but they did not compare the ability of the accelerometers placed at the hip or the wrist to predict AEE (45).
Epidemiological studies increasingly rely on data from accelerometers for physical activity and sedentary behavior measurement. Until recently, the two most studied variables determined from accelerometer-based data were time spent in moderate to vigorous intensity physical activity (MVPA) and AEE. Time spent in sedentary behavior, measured through accelerometry, is now considered as a separate health risk (16, 17, 35). More minutes spent in MVPA as measured by an accelerometer on the hip are related to lower risk of a variety of cardiovascular and metabolic disease biomarkers and clinical events (1, 11, 39). Similarly, sedentary time is associated with increased risk of mortality from all causes and cardiovascular disease (25), waist circumference and metabolic risk (21). When both sedentary time and MVPA are measured and controlled for, sedentary time and MVPA are separately related to an increase in biomarkers for breast cancer (28) and metabolic syndrome (23). Since there are no current calibrations for accelerometers worn on the wrist for either MVPA or sedentary behavior, this study evaluated the current methods used for hip accelerometer calibration and applied them to the wrist.
Linear regression has been the most common method to create an AEE prediction model from accelerometry data, but a more accurate method for estimating AEE on data from the hip uses the accelerometer signal to classify activity into an “activity type.” Crouter and colleagues used a coefficient of variation from the accelerometer counts to separate activities into different types or categories before using regression methods to predict energy expenditure (6). Ambulation produces less variation in the signal than activities of daily life such as self-care, household chores or other free-form activities. This allows an intensity prediction model to be built on ambulatory activities separate from other activities, improving AEE estimates. There are no studies to our knowledge that have attempted to perform similar calibration methods using accelerometer data collected from the wrist, as well as the hip. One study did compare wrist and hip sites for predicting AEE, but it used different methods and activities (34). A sedentary behavior threshold of < 50 Actigraph counts was used in the Crouter method, but this threshold was not determined analytically. Since the CV method was introduced, a sedentary threshold was established using Actigraph data from the hip, and that method was replicated in this study (35).
This report compares the hip and wrist accelerometer placement locations using common calibration methods for establishing activity intensity thresholds and estimating AEE. A second comparison is made to determine the ability of the accelerometer worn at the hip or wrist to identify sedentary behaviors.
Methods
Participants
Thirty-seven adults ages 18 – 74 years were recruited from the Stanford, CA community. Stanford University’s Human Use Committee approved the protocol, and written informed consent was obtained from all subjects before participation. Participants were asked to visit the clinic once to perform a variety of laboratory-based and simulated daily activities. All participants were generally healthy with no medical conditions that would prevent moderate intensity exercise.
Measurements
Participants first completed the Physical Activity Readiness Questionnaire (38) and the Stanford Brief Activity Survey (42). Resting heart rate and blood pressure, waist and hip circumference, body height, and weight were measured using standard methods prior to fitting the participant with the testing equipment. Oxygen uptake and related variables were measured with a portable metabolic system (Oxycon Mobile, Cardinal Health, Dublin, OH) attached to the torso and custom accelerometers (Wockets)(24) were used to measure motion, worn on both the hip and the wrist. A detailed description of the Wockets and the activities performed is included below.
Equipment
Subjects wore the Oxycon Mobile portable metabolic device to measure the energy cost of activities through indirect calorimetry. The device has a specially designed harness to hold the two processing units tightly to the torso with the sampling and volume measurements made through lines attached to a mask worn over the subject’s nose and mouth. The Oxycon Mobile unit was warmed up for 30 minutes prior to each test session and calibrated according to the manufacturer’s instructions. Data were measured, stored and reported on a breath by breath setting, and energy expenditure was determined from the V̇O2 V̇CO2, and volume of expired air measurements according to the manufacturer’s equations. Data were monitored via telemetery during the test on a laptop computer and also downloaded from the removable storage disk attached to the device after the activities were completed.
The Wockets system consists of a custom-built accelerometer-based device communicating wirelessly to a mobile phone. Raw motion data was collected from the accelerometers at 90 Hertz and summarized as described below. The Wockets are small (43 mm × 30 mm × 7 mm), light weight (13 g) and include a triaxial accelerometer, small circuit board, Bluetooth radio, and rechargeable battery. Custom Velcro bands were used to hold a Wocket to the dorsal aspect of the dominant wrist midway between the radial and ulnar process. The Wocket worn on the dominant hip was held in a small pocket attached to a belt worn around the waist, then for security, the whole band and pocket were wrapped under a wide Velcro waist strap. The mobile phone used in this version of the system was an HTC Diamond Touch running a windows mobile operating system. A more detailed technical description of the Wockets can be found on the website (http://wockets.wikispaces.com)(24). The Wockets system is open source technology, and information on downloading and using Wocket software technology is also available on the previously mentioned website.
Activities
Participants completed a combination of laboratory-based sedentary and physical activities followed by selected simulated daily activities. Activities were classified into four categories: sedentary behaviors (lying, sitting, reading a book, working at a computer, sorting paper), cycling (indoor and outdoor), ambulation (treadmill, carrying a box, and natural walking), and lifestyle (painting a wall, sweeping the floor, folding laundry). Each subject performed approximately 20 activities. Only activities with sufficient time to reach a metabolic steady state were included in this analysis. A time to reach metabolic steady state was defined by the intensity and the sequence of the activity within the protocol.
Data Processing
After completing the testing session, data were downloaded from the individual devices, processed, combined and then imported into a database for analysis. Wocket data were transmitted wirelessly from the accelerometers to the mobile phone during the data collection period. After the data collection period, the mobile phone was connected to a laptop computer and the files were transferred. A custom time synchronization program was run on both laptops and the mobile phone to ensure that the data could be temporally aligned from all of the devices for each second of data collection.
Data were condensed to averages of the steady-state period for each activity, and individual data for each activity were listed together to create the final dataset. At the same time, the coefficient of variation of the accelerometer signal was calculated from the change in counts over time according to the method defined by Crouter and colleagues (6, 7). Because the accelerometer data were provided in three axes, the axes were summed for both counts and coefficient of variation.
Data Analysis
All data processing was completed using custom software developed by engineers at the Massachusetts Institute of Technology and Northeastern University, and can be found at http://wockets.wikispaces.com/. The first piece of custom software was a time sync that allowed all of the devices to start at the same clock time, down to the millisecond. The second piece of custom software allowed voice recordings that annotated the activities to be converted into a text file that aligned the instant the annotation button was compressed with the label for each specific activity. A third program then pulled all of the data files downloaded from individual devices into a data file that created a second-by-second visualization and merging of the data with annotations. A thorough checklist was used to identify and correct any errors in timing, downloading or data collection before the data were condensed. A fourth software package then summarized the data by activity for the steady-state period. At this point, data were combined into one dataset for all subjects and all activities.
Because raw data from the accelerometers were collected, included below is a description of how raw data were converted to activity summary counts similar to the output produced by the Actigraph. Each Wocket output synchronized raw, triaxial ±2g accelerometer data, sampled at 90 Hz. These raw data were converted to a similar motion summary count using an area under the accelerometer curve calculation, as follows. To correct for the effects of static acceleration from gravity on the raw signal, a lowpass filter was applied to each axis of the raw signal using a moving average computation (i.e., at each time point subtracting the mean value of the signal from the prior 5 seconds). The filter calculation is:
| [1] |
where xt is the accelerometer data at time t, yt is the filtered output at time t, and h is the number of samples in the last 5 seconds including the current sample. Each second, the signal was then integrated to obtain the area under of the curve of each axis for each sensor. The calculation for the area under the curve (AUC) is:
| [2] |
where t is a particular second, xi is the accelerometer reading for sample i, yi is the filtered reading for sample i (removing the effects of gravity), and the integration is done on all samples that belong to t. The values from individual axes for each sensor are then summed to generate a motion summary count for each Wocket.
Statistical analyses were conducted using a combination of methods to evaluate the ability of accelerometer-based data to first classify activity intensity and then identify activity type (sedentary, ambulation, and other) to assist AEE prediction models. Both models of activity intensity and activity identification include sedentary behavior. The definition of sedentary behavior used in this report is derived from a generally accepted sedentary definition by Owen et al. (31) that includes both sitting and low levels of energy expenditure (<1.5 METs). Unfortunately, using an accelerometer on the hip or wrist cannot accurately determine posture, so for the purpose of conducting statistical analyses, sedentary behavior is based on low levels of energy expenditure (<1.5 METs). For activity intensity analysis determining thresholds, moderate to vigorous physical activity is also defined in terms of METs, (≥ 3.0 METs). Accuracy in identifying activity intensity is therefore defined as the ability of the accelerometer to classify activity into sedentary, light-intensity (1.5–2.9 METs) or MVPA.
Other analyses conducted in this paper are directed at identifying three specific groups of activities to improve AEE estimates. These analyses included identifying sedentary behavior (activities < 1.5 METs), ambulation, and other (non-ambulatory) activities. Using these three activity types has been shown to produce a 2-regression model that is more accurate at predicting AEE than a single regression, at least at the hip (7). For sedentary behavior identified from a low number of counts, 1 MET was the assigned predicted value. After using logistic regression to separate the remaining activities into ambulation and non-ambulation, mixed model analyses were conducted on the two groups of activities to produce the 2-regression model. Mixed model analyses was used to account for both fixed and random effects, in this case to account for the effects produced using multiple activities per subject.
All statistical analyses were conducted using SAS (SAS Institute Inc, Cary, NC, version 9.2). The analyses were organized into four analytical techniques to answer a variety of questions based on the accelerometer and indirect calorimetry output:
Simple regression comparing energy expenditure to counts for both wrist and hip data.
-
Receiver operating characteristic (ROC) curves (logistic regression)
Threshold in counts between sedentary behavior and physical activity
Threshold in counts between MVPA and other activity
Threshold in CV for the accelerometer signal between ambulatory and non- ambulatory activities.
Statistical comparison of the hip and the wrist for the above classifications to test for significance using the method of DeLong et al. (8)
Mixed model analysis was then used to create the 2-regression models.
Leave-one-out cross validation to test the AEE model on each subject.
The analyses were planned according to the best methods known to evaluate summary data.
Results
Each of the 37 subjects provided accelerometer and steady-state AEE data for 20 activities. The men (n=13) had an average age of 39 years, height of 179 cm, and weight of 82 kg. The women (n=24) had an average age of 38 years, height of 164 cm, and weight of 64 kg. The average body mass index (BMI), in kg/m2 for men was 25 and for women it was 24.
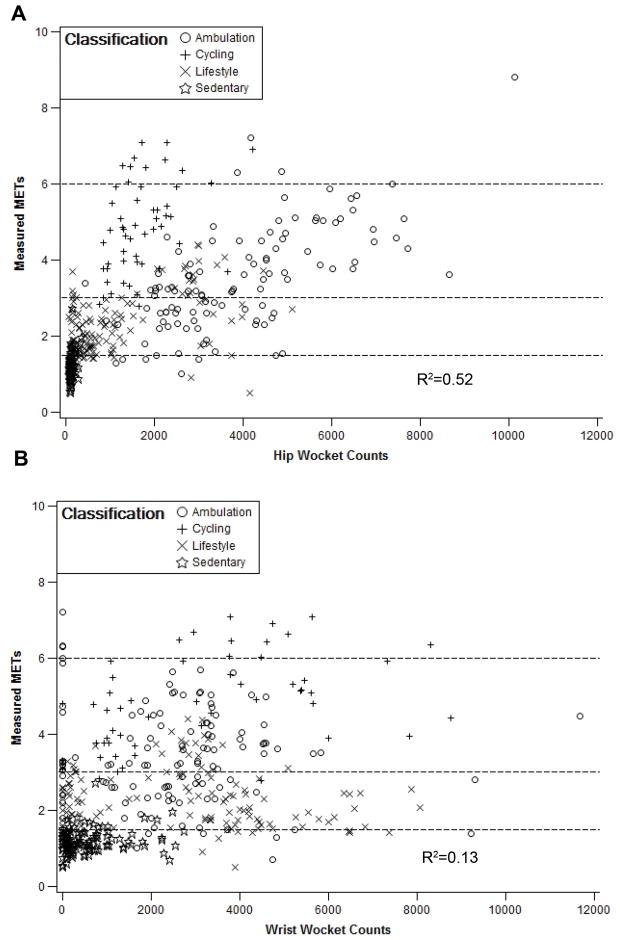
Activities were classified as sedentary, ambulation, lifestyle and cycling based on observation by staff conducting the testing. Figure 1 provides individual data and illustrates the relationship between accelerometer counts and measured AEE for the hip (A) and wrist (B), with the R2 value for the relationship being 0.52 for the hip and 0.13 for the wrist. This value for data from the hip is similar to what other investigators have reported (41) and the results for predicting AEE for accelerometer data collected on the wrist are quite variable when using very different calibration protocols (5, 41). Studies using ambulation only results in higher R2 values on the hip, but Figure 1 includes sedentary and lifestyle activities as well as cycling which are known to reduce the prediction of AEE from accelerometer counts on the hip.
Figure 1.
Wrist (A) and Hip (B) counts and measured METs for all activities (shown in four classifications). Linear regression of counts with activity energy expenditure resulted in an R2 of 0.52 for the hip and 0.13 for the wrist.
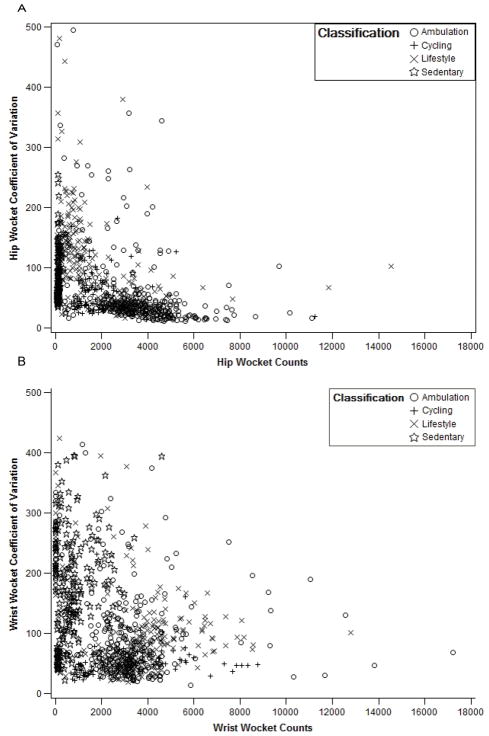
In addition to counts, this analysis explored using the coefficient of variation (CV) to separate activity type and improve estimates of energy expenditure. Following the method of Crouter and colleagues (6), the activities were separated into sedentary behaviors, ambulation and other activities (non-ambulation). Figure 2A presents the CV for data from the hip plotted vs. counts on the hip. Figure 2B is a similar plot for the wrist data. The data are more scattered from the wrist, but more importantly, note for the hip, the grouping of ambulation activities (open circles) for a range of counts at a low CV, where there is no such grouping on the wrist. Since more accurate AEE predictions can be made when ambulation is separated from other activities, it is apparent that there will be a greater number of misclassifications in activity type on the wrist when using the CV to do activity typing. A comparison of the AEE predictions with and without activity typing is presented below.
Figure 2.
Wrist (A) and Hip (B) counts and coefficient of variation for all activities (shown in four classifications). Hip (A) shows separation between sedentary and lifestyle activities and ambulation, but this separation is not seen on the wrist (B).
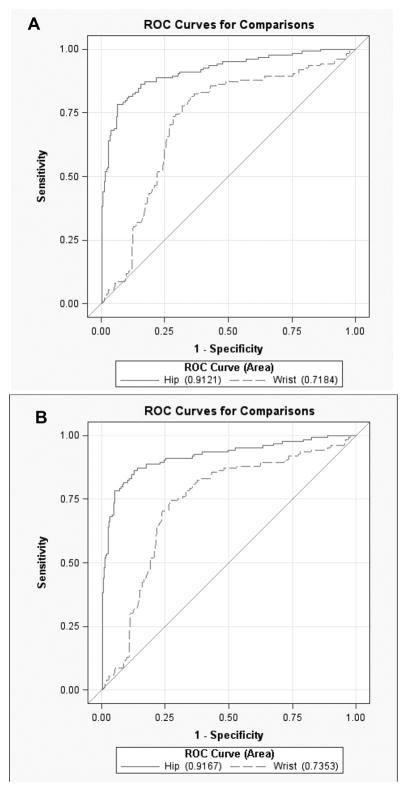
Since sedentary behavior has become an important health predictor separate from MVPA, the objective measurement of sedentary behavior was explored in this analysis. Sedentary activities were previously separated from other activities by observation (6), but logistic regression used to produce ROC curves will balance the ability of different thresholds in accelerometer counts at predicting sedentary behavior. This method was used previously, to create a sedentary threshold on data from the Actigraph worn on the hip (35). Figure 3 illustrates the ability to identify sedentary behavior from the A) hip and wrist for all activities and B) hip and wrist for all activities except cycling. A higher area under the curve (AUC) is preferable, and a higher AUC is seen for the hip (0.917) compared to the wrist (0.737), and the hip was a significantly better predictor of sedentary behavior than the wrist (p<0.001). The specificity and sensitivity for identifying sedentary behavior, including all activities, were 86% and 92%, for the hip and 32% and 89% for the waist.
Figure 3.
Receiver operating characteristic curves for identifying sedentary behavior from the A) hip and wrist including all activities. There is little change in the ability to identify sedentary behavior when cycling is removed from the B) hip and wrist activities. The differences between the two curves are significant (p<.0001) for both A) and B).
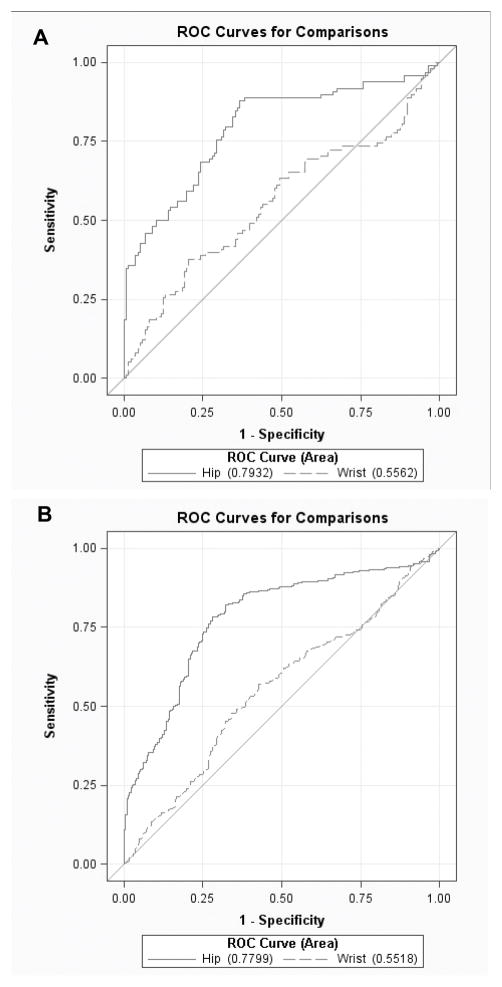
Similar to finding a threshold in the counts for identifying sedentary behavior, a threshold in the CV can be used to separate ambulatory from non-ambulatory activities. Figure 4 shows the results of producing a CV threshold for both the A) hip and wrist for all activities and the B) hip and wrist for all activities except cycling. Again, a significantly (p<0.001) higher AUC is obtained for the hip (0.747) than the wrist (0.603). This resulted in a sensitivity and specificity for the hip of 78% and 49% when no cut point was defined for the wrist. For the activity identification presented using these thresholds to separate activities into 1) sedentary, 2) ambulation and 3) non-ambulation, the hip had a total accuracy of 76%, while the wrist had an accuracy of 69%. This accuracy value on the wrist is somewhat inflated because all of the non-ambulatory activities were correctly classified while none of the ambulatory activities were correctly classified because there was no separation.
Figure 4.
Receiver operating characteristic curves for identifying ambulatory activities from the A) hip and wrist including all activities. There is little change in the ability to identify ambulatory activities when cycling is removed from the B) hip and wrist activities. The differences between the two curves are significant (p<.0001) for both A) and B).
One way to use accelerometer data is to determine the type of physical activity performed, but often studies have classified activities into intensity categories such as time spent in MVPA or time spent in sedentary behavior. Logistic regression was used to produce ROCs for separating (MVPA) from other activities (light-intensity activity and sedentary behavior). The sensitivity and specificity for identifying MVPA using data from the hip were 52% and 84%, while from the wrist they were 12% and 93%. The hip accelerometer had 62% total accuracy for identifying activity intensity thresholds, whereas the wrist resulted in 41% total accuracy. The hip was significantly better at identifying MVPA (p<0.001).
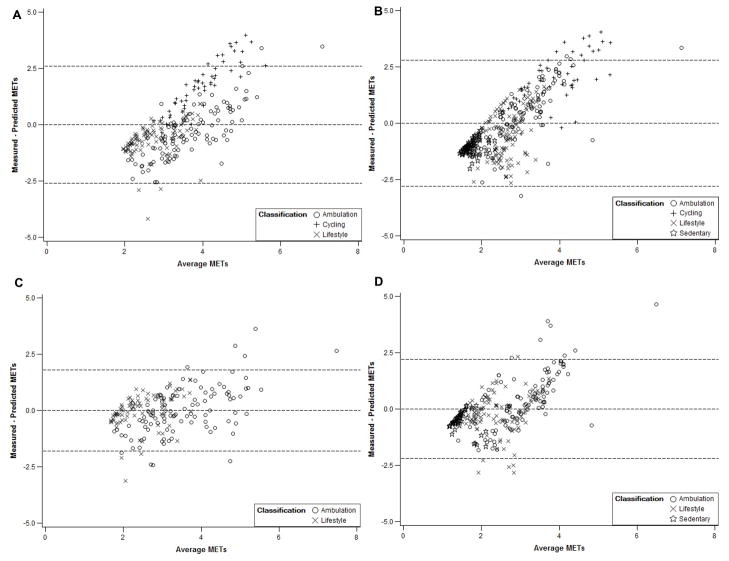
In Figure 5, Bland-Altman plots are presented to show the difference in error for predicting AEE between the hip and the wrist with and without cycling. Sedentary behaviors are excluded from this analysis because they were all assigned a 1.0 MET value. The mean error (± standard deviation) for the hip was 0.55 (± 0.55) METs whereas for the wrist it was 0.85 (± 0.93) METs for all activities except cycling. When cycling is included in this prediction model, the mean error for the hip increases to 0.79 (± 0.80) METs, as does the mean error for the wrist to 1.17 (± 0.95) METs. For reference, when these models are tested without activity typing, the error increases in the hip (0.86 ± 0.80 METs), but not at the wrist (1.17 ± 1.44 Mets).
Figure 5.
Bland-Altman plots showing the differences between measured and predicted METs for the A) hip and B) wrist prediction models including all non-sedentary activities. There are significant improvements in prediciton when cycling is removed for both the C) hip and D) wrist models.
Discussion
In this study we compared data from a triaxial accelerometer worn on the hip with data from a similar accelerometer worn on the dominant wrist in men and women performing 20 common and well-defined physical activities. A majority of the data published from major studies evaluating physical activity using accelerometry is based on summary data (counts) from the hip (9, 11, 18, 28). Thus, we decided that it would be informative to investigators and practitioners who measure physical activity to use summary data and frequently used analytical procedures in comparing data acquired from the wrist versus the hip. Our primary goals were to determine the ability of data from the wrist and hip to (1) estimate AEE and (2) classify physical activities into specific activity categories; sedentary versus non-sedentary; ambulatory versus non-ambulatory and MVPA versus other activities.
Estimation of AEE
Based on data from all activities expressed as counts, values from the hip were more highly correlated with measured AEE than values recorded from the wrist (R2 = 0.52 versus 0.13). Also, the two-regression prediction model for AEE resulted in an average difference of 0.55 (±0.55) METs for data from the hip and 0.82 (± 0.93) for data from the wrist (excluding cycling). These results were expected given the general consensus that an accelerometer located nearer the center of the body’s mass (on the trunk) provides better estimates of AEE during large-muscle dynamic activities than data from an accelerometer located on the wrist. Similar AEE predictions have been obtained by measuring motion on the hip and other trunk locations (15, 41). When walking, jogging or running on the horizontal and the arms are swinging free, an accelerometer on the wrist can provide reasonably accurate information about AEE (4, 5, 45). But, if the wrist is constrained from free movement during ambulation, such as when carrying a briefcase or cup of coffee, talking on a mobile phone, or pushing a grocery cart, the characteristics of the signal from the accelerometer will be very different from when the wrist is not constrained even though the AEE will be quite similar. Also, the motion at the wrist can represent movement of just a small mass (arm/forearm) such as arm movements when sitting or it can represent movement of a large body mass such as when walking or running. The future of AEE prediction from wrist motion likely lies in accurate activity type classification using multiple features of the raw data (4).
The Crouter method for estimating energy expenditure from accelerometers is one way of using a basic feature of the accelerometer signal to improve estimates while not requiring extensive computing power to extract additional features from the signal (2, 33, 37, 40, 45). This will be important in the future in mobile intervention technologies that must perform real-time signal processing to enable feedback to the user when lifestyle physical activity decisions are being made. Activity classification using several features of the accelerometer signal and mixed modeling for energy expenditure prediction seemed like a reasonable compromise, and it worked quite well on the hip.
Comparisons of AEE estimations based on accelerometer data from wrist versus hip in adults have been reported previously (5, 30, 41) with substantially varying results regarding data from the wrist. Melanson and Freedson evaluated the validity of estimating AEE during walking and jogging on a treadmill using CSA accelerometers on the hip, wrist and ankle in 28 young men and women. With increasing treadmill speed but not increasing grade estimations of AEE were similar using data from the hip, wrist or ankle with the highest single accelerometer R2 of 0.86 obtained using a multiple regression including wrist data and BMI. Swartz and colleagues using linear regression obtained an R2 of 0.03 for estimating AEE from the wrist and an R2 of 0.32 for the hip in 70 men and women performing from 7 to 12 common activities (41). Chen and colleagues had 60 women perform a variety of common activities while in a calorimetry chamber and wearing an accelerometer on the hip (Tritrac R3D) and wrist (Actiwatch). Using nonlinear regression models they obtain better estimates of AEE from the hip (R2 = 0.81) than the wrist (R2 = 0.53), but both substantially higher than the results by Swartz. The GENEA accelerometer worn on the wrist and multiple logistic regression were used to estimate AEE compared to values obtained from doubly labeled water over approximately 8 days in Swedish women who were non-pregnant or pregnant (44). In non-pregnant women (N = 48) the accelerometer data explained 19% of AEE in the leave-one-out cross validation, while in the pregnant women (N = 26) only 11% of the AEE was explained. In youth, AEE estimations from an Actiwatch accelerometer worn on the dominant wrist and multiple linear regression obtained an R2 of 0.72 for 8 commonly performed activities. No comparison was made with data collected at the hip (10).
So far only a limited number of studies have compared predicted versus measured AEE using advanced feature extraction and machine algorithms such as artificial neural networks based on accelerometer data collected at the hip (36, 40). None of the reports using these advanced analytical procedures on data collected at the wrist have estimated AEE; they have predicted physical activity type and intensity categories (2, 3, 13, 32, 45).
Identification of activity intensity thresholds
A major objective for accelerometer data analyses in many studies has been to predict amount of time spent in activities of different intensities, and this study evaluated intensity thresholds for both hip and wrist data. Better classification of activities into sedentary, light-intensity and MVPA was achieved using data from the hip then from the wrist. The magnitude of the intensity category predictions for data collected from the hip in this study are quite comparable with prior studies using similar data collection protocols and analytical procedures (22, 41). More recently studies have been published evaluating accelerometers placed on multiple body locations including the wrist to classify activities into categories usually based on intensity using advanced data extraction and analytical procedures. For example, Bao and Intille recorded raw data from wireless biaxial accelerometers placed on 5 body locations and had 20 subjects perform 20 different activities. The major objective was to determine which combination of sensors provided the best discrimination of activities into specific categories. Performance of individual sensors was not reported, but when using just two sensors the combination of wrist and thigh worked best. Atallah and colleagues used 13 features extracted from the raw triaxial accelerometer signal to determine optimal features and sensor location for activity group discrimination (7 sensor locations, 11 subjects, 15 activities). For very low levels of activity (lying still) and moderate-intensity the wrist was a good location for precision of activity identification, but generally did less well than the sensor at the waist for identifying low- and high-intensity activities. Overall it appears that the precision for identifying activity categories was in the 60%–80% range for data collected at the wrist (exact values not provided). The authors indicated that their approach had high computational costs, especially when using all 13 features extracted from the signal. In a study by Ruch and colleagues (37) involving 41 boys and girls wearing a biaxial accelerometer (Actigraph GT1M) on the hip and wrist during free-living activities, they found extracting features from both accelerometers provided better activity classification than from either location alone. No comparison was made between the hip and wrist sensors to identify activity categories.
A relatively new triaxial accelerometer designed to be worn on the wrist (GENEA, Actinsights Ltd. Kimbolton, United Kingdom) has been tested for its ability to provide physical activity classification in adults (12, 45) and youth (32). In an evaluation of the GENEA worn on both wrists and at the hip in 60 middle-aged men and women who performed 10–12 semi-structured physical activities the accelerometers all performed exceptionally well in assigning activities into intensity categories (12). For both wrists and the hip accelerometer, the area under the ROC curve was >0.90 when separating activities into sedentary, light, moderate and vigorous intensity categories except for the right wrist where the values were 0.84 for separating moderate from light and 0.89 for separating vigorous from moderate intensity. These values are higher than the results from other studies for either hip or wrist. These high values may, in part, be explained by the selection of test activities (8 activities were ambulation), and the changing of the lower intensity threshold for moderate intensity activity from 3.0 to 4.0 METs and for the lower threshold for vigorous intensity from 6.0 to 7.0 METs. In a GENEA validation study in 44 children wearing accelerometers on both wrists and the hip while performing 8 activities similar results were obtained with areas under the ROC curves for separating activity categories in the range of 0.92 to 0.97 (32). Again, activity selection is likely one reason for the high level of prediction accuracy.
Zhang and colleagues evaluated the ability of raw data from the triaxial GENEA accelerometer worn on the wrist or hip to identify sedentary activities, walking, running and household activities in adults (N= 50, 10–12 activities, 11 features of the signal). Using Decision Tree algorithms to classify activities into the 4 categories, data from both the waist and wrist showed exceptionally high classification accuracy with overall accuracy for the right wrist being 95% and 99% for the waist with the area under the curve for the ROCs for each of the 4 categories all exceeded 0.95. These are extremely high values compared to the results of our study and of other studies that have used either summary data (counts) or raw data from the waist, hip or other location. (2, 15, 37, 40). These very high values for activity type classification are due, at least in part, to the activity selection for each category. It is very apparent that the accelerometer signal from the wrist will be quite different when lying, sitting or standing still (sedentary category) from all the other activities, and that walking and running with the arms swinging freely involving 5 or 6 activities per subject will be different from the 2 household (non ambulatory) activities (6). Although cross-validation was used in testing, the study did not use leave-one-subject-out cross validation (personal communication) and this would likely decrease this predictive power somewhat. Comparison across studies of the strength of prediction of activity type or intensity by accelerometry is difficult because these associations are strongly influenced by the specific activities included in the evaluation.
In the current study, both the hip and the wrist performed quite poorly for correctly identifying MVPA. While the accuracy of neither of these estimations is very good, there are known problems with establishing intensity thresholds, such as activities that fall near the thresholds are easily misclassified. Because time performing MVPA is often the measure of activity used in epidemiological studies, a <50% accuracy in classification on the wrist is probably unacceptable. These numbers are fairly low partly because activities near the 3.0 MET threshold were selected specifically to see if MVPA could be teased out of activities that are in the 2.5–3.5 MET range. Eslinger and colleagues (13) partly avoided this challenge by changing the threshold from 3.0 to 4.0 METs. Although epidemiological studies have obtained positive results using MVPA thresholds to classify participants into categories of physical activity and relating it to health outcomes (20), this same approach may perform less well when data are collected from the wrist.
Sedentary Behavior
Measurement of sedentary behavior with accelerometers is a relatively new field of research with few calibration studies reported (26, 35). Early definitions of sedentary behavior using accelerometry at the hip was set at <100 Actigraph counts/minute (19). Establishing sedentary behavior with an accelerometer would seem to be easy because a lack of movement should accompany sedentary behavior. At the hip, the calibration can be complicated by sitting or standing activities that use just the arms, or sitting activities that use just the legs with little or no movement of the waist (cycling). Also, if a person is sedentary but riding in a car some movement frequently is registered. Thus, a wide range of activities not frequently used to establish thresholds for MVPA are needed for establishing a threshold for sedentary behavior using accelerometers. At the wrist, motion can be quite high with little or no increase in AEE. Also, there is greater inter-person variability in wrist movements during sedentary behavior, resulting in more misclassification (e.g., some people talk with hands and wrists remaining still while others constantly are moving their hands and wrists). So far the ability to determine sitting from standing using accelerometers on the waist or wrist has not been demonstrated. Zhang and colleagues (45) have demonstrated the possibility that more advanced analytical techniques using raw data from an accelerometer on the wrist may provide good classification of activities into broad categories, but accurate identification of sedentary behavior in real-life settings is yet to be established.
Study limitations
The predictions of AEE from both hip and wrist data in this study are very likely higher than what would be obtained in free-living or naturalistic conditions. Both within and between person variations in the accelerometer signal for a specific activity were minimized as a result of standardized protocols and close researcher monitoring (37). Also, all AEE predictions used data obtained during “steady state” conditions, and when the duration of a task is short with rapid transitions in motion and posture, both within and between person variation in how tasks are performed day to day will increase. Generalizability of our results is limited by the lack of subjects who were obese and few activities in the vigorous intensity category (≥6 METs). Since this study was part of a project for the development and evaluation of new wireless sensors and mobile phones for data collection, we used Wockets instead of the Actigraph or other commonly used activity monitors.
Study Strengths
Study strengths included the evaluation of men and women over a wide age range and the use of a variety of activities that are typical of activities performed by many adults. The activities were carefully selected to represent both common activities and activities that are known to challenge this type of analysis, including cycling and lifestyle activities such as painting a wall and scrubbing a floor. Activities near the MET thresholds were chosen to evaluate the challenging task of accurately classifying activity intensity and identifying sedentary behavior, light-intensity activity and MVPA. Another strength of this study is the technology developed over the course of the evaluation of the Wockets. Custom software and equipment was built so that we could annotate, time-sync and visually review data from a variety of sensors second-by-second. These new technologies are available as open source tools for researchers.
Conclusions
Based on the results of this study, it appears that the use of accelerometer-based data collected from the wrist presents unique challenges in classifying activities into type and intensity categories and estimating AEE. More specifically, the hip outperforms the wrist in simple linear regression, two-regression AEE prediction models, and classifying activities into sedentary, ambulation, and MVPA categories. Future directions for this type of research should be to explore additional features of the wrist accelerometer signal and to conduct calibration studies using data collected in naturalistic settings. As suggested by Liu and colleagues (27) in their review of computational methods for estimating PAEE in humans, advanced approaches for feature extraction and analysis of the raw accelerometer signal will increase the accuracy and reliability of predicting activity type and intensity and estimating AEE. While the compliance to the protocol may improve with a wrist compared to a waist/hip accelerometer, it appears that there are challenges for using wrist accelerometer data for the traditional epidemiological variables such as time spent in MVPA or sedentary behavior, or estimating AEE, and this should be considered when selecting a data collection protocol for addressing a specific research question.
Acknowledgments
Funding for this study:
Financial support for this project was provided by NIH (UO1-HL091737) with Stephen Intille as PI and Mary Rosengerger was a NIH postdoctoral research fellow (NIHT2HL07034HL). Additional support was provided from the The National Institute of Environmental Health Sciences, with William L. Haskell as PI, subaward 5710002222 (3-U01-HL091737-01S1).
Footnotes
The authors have no conflicts of interest to disclose.
Conflict of Interest Statement: The authors have no conflicts of interest to disclose. The authors acknowledge the results of the current study do not constitute endorsement by the American College of Sports Medicine.
References
- 1.Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368(9532):299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- 2.Atallah L, Lo B, King R, Yang GZ. Sensor positioning for activity recognition using wearable accelerometers. Biomedical Circuits and Systems, IEEE Transactions on. 2011;5(4):320–9. doi: 10.1109/TBCAS.2011.2160540. [DOI] [PubMed] [Google Scholar]
- 3.Bao H, Cao J. Delay-distribution-dependent state estimation for discrete-time stochastic neural networks with random delay. Neural Netw. 2011;24(1):19–28. doi: 10.1016/j.neunet.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Bao L, Intille SS. Activity recognition from user-annotated acceleration data. Proc Pervasive. 2004:1–17. [Google Scholar]
- 5.Chen KY, Acra SA, Majchrzak K, Donahue CL, Baker L, Clemens L, Sun M, Buchowski MS. Predicting energy expenditure of physical activity using hip-and wrist-worn accelerometers. Diabetes technology & therapeutics. 2003;5(6):1023–33. doi: 10.1089/152091503322641088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crouter SE, Clowers KG, Bassett DR., Jr A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol. 2006;100(4):1324–31. doi: 10.1152/japplphysiol.00818.2005. [DOI] [PubMed] [Google Scholar]
- 7.Crouter SE, Kuffel E, Haas JD, Frongillo EA, Bassett DR., Jr Refined two-regression model for the ActiGraph accelerometer. Med Sci Sports Exerc. 2010;42(5):1029–37. doi: 10.1249/MSS.0b013e3181c37458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988:837–45. [PubMed] [Google Scholar]
- 9.Dubbert PM, Carithers T, Ainsworth BE, Taylor HA, Jr, Wilson G, Wyatt SB. Physical activity assessment methods in the Jackson Heart Study. Ethn Dis. 2005;15(4 Suppl 6):S6–56–61. [PubMed] [Google Scholar]
- 10.Ekblom O, Nyberg G, Bak EE, Ekelund U, Marcus C. Validity and comparability of a wrist-worn accelerometer in children. Journal of physical activity & health. 2012;9(3):389–93. [PubMed] [Google Scholar]
- 11.Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–12. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Esliger DW, Rowlands AV, Hurst TL, Catt M, Murray P, Eston RG. Validation of the GENEA Accelerometer. Med Sci Sports Exerc. 2011;43(6):1085–93. doi: 10.1249/MSS.0b013e31820513be. [DOI] [PubMed] [Google Scholar]
- 13.Esliger DW, Tremblay MS. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc. 2006;38(12):2173–81. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- 14.Foster RC, Lanningham-Foster LM, Manohar C, McCrady SK, Nysse LJ, Kaufman KR, Padgett DJ, Levine JA. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Prev Med. 2005;41(3–4):778–83. doi: 10.1016/j.ypmed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–81. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Hart TL, Ainsworth BE, Tudor-Locke C. Objective and subjective measures of sedentary behavior and physical activity. Med Sci Sports Exerc. 2011;43(3):449–56. doi: 10.1249/MSS.0b013e3181ef5a93. [DOI] [PubMed] [Google Scholar]
- 17.Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011;8:62. doi: 10.1186/1479-5868-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawkins MS, Storti KL, Richardson CR, King WC, Strath SJ, Holleman RG, Kriska AM. Objectively measured physical activity of USA adults by sex, age, and racial/ethnic groups: a cross-sectional study. Int J Behav Nutr Phys Act. 2009;6:31. doi: 10.1186/1479-5868-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 20.Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, Owen N. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–71. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 22.Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Med Sci Sports Exerc. 2000;32(9 Suppl):S442–9. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- 23.Hsu YW, Belcher BR, Ventura EE, Byrd-Williams CE, Weigensberg MJ, Davis JN, McClain AD, Goran MI, Spruijt-Metz D. Physical activity, sedentary behavior, and the metabolic syndrome in minority youth. Med Sci Sports Exerc. 2011;43(12):2307–13. doi: 10.1249/MSS.0b013e318222020f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Intille S, Albinali F, Mota S, Kuris B, Botana P, Haskell W. Design of a wearable physical activity monitoring system using mobile phones and accelerometers. 2011. p. 3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 26.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43(8):1561–7. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 27.Liu S, Gao R, Freedson P. Computational Methods for Estimating Energy Expenditure in Human Physical Activities. Med Sci Sports Exerc. 2012 doi: 10.1249/MSS.0b013e31825e825a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lynch BM, Friedenreich CM, Winkler EA, Healy GN, Vallance JK, Eakin EG, Owen N. Associations of objectively assessed physical activity and sedentary time with biomarkers of breast cancer risk in postmenopausal women: findings from NHANES (2003–2006) Breast Cancer Res Treat. 2011;130(1):183–94. doi: 10.1007/s10549-011-1559-2. [DOI] [PubMed] [Google Scholar]
- 29.Matthew CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 Suppl):S512–22. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 30.Melanson EL, Jr, Freedson PS. Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Med Sci Sports Exerc. 1995;27(6):934–40. [PubMed] [Google Scholar]
- 31.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Phillips LR, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. J Sci Med Sport. 2012 doi: 10.1016/j.jsams.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 33.Pober D, Staudenmayer J, Raphael C, FREEDSON P. Development of novel techniques to classify physical activity mode using accelerometers. Med Sci Sports Exerc. 2006;38(9):1626. doi: 10.1249/01.mss.0000227542.43669.45. [DOI] [PubMed] [Google Scholar]
- 34.Rawson ES, Walsh TM. Estimation of resistance exercise energy expenditure using accelerometry. Med Sci Sports Exerc. 2010;42(3):622–8. doi: 10.1249/MSS.0b013e3181b64ef3. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberger M, Haskell W, Quatromoni P, Albini F, Intille S. Objective Measurement of Sedentary Behavior with Accelerometers. Proceedings of the NPAM/EPI Scietific Sessions; 2011; Atlanta, GA. p. 101. [Google Scholar]
- 36.Rothney MP, Neumann M, Beziat A, Chen KY. An artificial neural network model of energy expenditure using nonintegrated acceleration signals. J Appl Physiol. 2007;103(4):1419–27. doi: 10.1152/japplphysiol.00429.2007. [DOI] [PubMed] [Google Scholar]
- 37.Ruch N, Rumo M, Mader U. Recognition of activities in children by two uniaxial accelerometers in free-living conditions. Eur J Appl Physiol. 2011;111(8):1917–27. doi: 10.1007/s00421-011-1828-0. [DOI] [PubMed] [Google Scholar]
- 38.Shephard RJ. PAR-Q, canadian home fitness test and exercise screening alternatives. Sports Med. 1988;5(3):185–95. doi: 10.2165/00007256-198805030-00005. [DOI] [PubMed] [Google Scholar]
- 39.Sisson SB, Camhi SM, Church TS, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps/day and metabolic syndrome. Am J Prev Med. 2010;38(6):575–82. doi: 10.1016/j.amepre.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 40.Staudenmayer J, Pober D, Crouter S, Bassett D, Freedson P. An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. J Appl Physiol. 2009;107(4):1300. doi: 10.1152/japplphysiol.00465.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swartz AM, Strath SJ, Bassett DR, Jr, O’Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32(9 Suppl):S450–6. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- 42.Taylor-Piliae RE, Haskell WL, Iribarren C, Norton LC, Mahbouba MH, Fair JM, Hlatky MA, Go AS, Fortmann SP. Clinical utility of the Stanford brief activity survey in men and women with early-onset coronary artery disease. J Cardiopulm Rehabil Prev. 2007;27(4):227–32. doi: 10.1097/01.HCR.0000281768.97899.bb. [DOI] [PubMed] [Google Scholar]
- 43.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 44.van Hees VT, Renström F, Wright A, Gradmark A, Catt M, Chen KY, Löf M, Bluck L, Pomeroy J, Wareham NJ. Estimation of Daily Energy Expenditure in Pregnant and Non-Pregnant Women Using a Wrist-Worn Tri-Axial Accelerometer. PloS one. 2011;6(7):e22922. doi: 10.1371/journal.pone.0022922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang S, Rowlands AV, Murray P, Hurst TL. Physical Activity Classification Using the GENEA Wrist-Worn Accelerometer. Med Sci Sports Exerc. 2012;44(4):742–8. doi: 10.1249/MSS.0b013e31823bf95c. [DOI] [PubMed] [Google Scholar]