Abstract
Purpose
Balloon reduction and cement fixation of displaced articular fractures of the calcaneus have been described elsewhere but support for it lacks clinical evidence. We have been performing the technique since October 2006 and describe here our clinical experience including three to five-year follow up of our first ten cases with no patient lost to follow up.
Methods
From September 2006 to September 2009, ten patients were admitted with a calcaneus fracture, six were female and four male, one case was bilateral (11 fractures). Patients were operated upon in the prone position according to the technique we have described. Reduction was obtained in all cases. Patients were discharged after an average of four days postoperatively and were allowed weight bearing after two to three months. All patients were followed up regularly and were examined by an independent observer at the latest follow up. The clinical results were assessed using the AOFAS ankle score, the Babin score and the RAND-36 physical components score. A CT scan was obtained in all patients before, after the operation and at the latest follow up.
Results
After a minimal follow up of 36 months (three to five years), no patient was lost to follow up and none required further surgery. The AOFAS clinical results were rated good or excellent in 81.8 % of cases (nine fractures, eight patients), and the physical component of the RAND-36 was 74.6. One patient only (one fracture) had a bad clinical result and evidence of subtalar arthritis on the CT scan and was offered a subtalar fusion; she refused. All patients had returned to their former professional activities at the same level as before the fracture except one who had retired but had resumed leisure walking.
Conclusion
Balloon reduction and cement fixation of fresh calcaneal fractures (“balloon calcaneoplasty”) appears a safe and effective procedure in a variety of calcaneal fractures with lasting and excellent clinical results. More studies are needed to further refine the indications and the limits of the procedure.
Introduction
Balloon reduction of a calcaneal fracture was first reported in the literature by Bano et al. [1] in one case in 2009. The technique has been described in several papers recently with technical details [2–8]. However, it lacks follow up and clinical evidence of efficacy. We have been initiating the technique since 2006 and hereby describe our first consecutive 11 cases in ten patients with a three- to five-year follow up with no patient lost to follow up.
Material and methods
From 2006 to 2009, ten patients were operated upon for fractures of the calcaneus with thalamic articular involvement. This cohort represents the first ten patients managed by this technique. Patients were treated as consecutive cases by the same operator. Only one additional patient with psychiatric problems and IV drug use was excluded and had indeed functional treatment with this cohort.
Patients
The mean age was 37.8 years (range 26–58). The demographic data are shown in Table 1. Four were male and six female. Three suffered a work-related accident. The initial accident was a fall on stairs in two, in a swimming pool in one, from a ladder in five, from a window on the first floor in one (bilateral case) and the result of a street fight in one.
Table 1.
Demographic data
| Case number | Gender | Work related | Side | Age (years) | Day op | Accident | Occupation | Follow up (months) | Work |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | No | Right | 29 | 3,00 | Fall/stairs | Bartender | 70 | Yes |
| 2 | F | Yes | Right | 53 | 9,00 | Fall/ladder | Designer | 68 | Yes |
| 3 | F | No | Left | 26 | 5,00 | Fall/swimming pool | Administrator | 56 | Yes |
| 4 | F | No | Left | 54 | 5,00 | Fall/ladder | Retired | 56 | Retired |
| 5 | F | No | Left | 32 | 18,00 | Fall/ladder | Floor sweeper | 40 | Yes |
| 6 | M | No | Right (Bilat.) | 26 | 3,00 | Fall/1st floor | Teacher | 39 | Yes |
| 7 | M | No | Left (Bilat.) | 26 | 3,00 | Fall/1st floor | Teacher | 39 | Yes |
| 8 | M | Yes | Left | 58 | 5,00 | Fall/ladder | Painter | 39 | Yes |
| 9 | F | Yes | Left | 56 | 3,00 | Fall/stairs | Concierge | 39 | Yes |
| 10 | M | No | Right | 33 | 11,00 | Street fight | Hotel cook | 36 | Yes |
| 11 | M | No | Right | 27 | 13,00 | Fall/ladder | Construction worker | 36 | Yes |
F female, M male
Fractures
Five fractures were located on the right side and six on the left side. One fracture was bilateral. Fractures occurred after a low energy fall from a height of one to three metres in all cases. Fractures types according to Sanders are shown in Table 2. The mean Boehler angle at the time of presentation was 2.45° (−20 to 25°). There were no open fractures. Patients were operated on after three to 18 days (mean seven days) after the trauma.
Table 2.
Radiographic data
| Case number | Boehler angle (°) | Sanders |
|---|---|---|
| 1 | −8 | IIC |
| 2 | −6 | IIIBC |
| 3 | −4 | IIB |
| 4 | 3 | IIIAB |
| 5 | −4 | IIIAB |
| 6 | 25 | IIB |
| 7 | 5 | IIB |
| 8 | −6 | IIIAB |
| 9 | −4 | IIIAB |
| 10 | −6 | IIIAB |
| 11 | −10 | IIB |
Technique
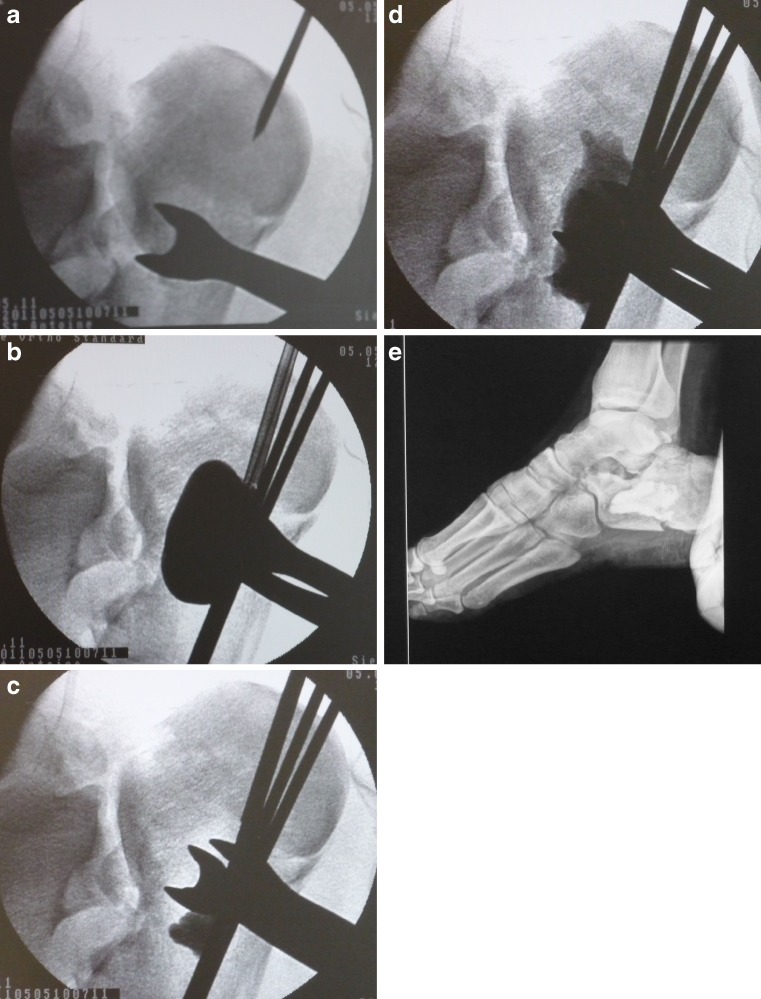
All cases were operated on in the prone position with a double image intensifier control in the lateral and AP/ thalamic view as already described [5–7]. Additional reduction techniques were used, such as lateral compression using two plastic slabs and a large reduction clamp, as well as “framing” of the fracture using temporary plantar K-wire stabilisation to direct the pressure of the balloon towards the thalamic fragment. Reduction was obtained through progressive balloon inflation and, once obtained, was stabilised using PMMA cement only (Fig. 1). Metallic hardware was removed once stability was obtained, and percutaneous entry ports were closed using absorbable sutures and cyanocrylate glue (Dermabond™). No further dressing was required. Full weight bearing was allowed only after healing of the fracture was obtained (three months) in a very conservative fashion in this series. Partial weight bearing was allowed after two months in four cases with very reliable patients (cases 3, 6, 7, 11) (Fig. 2).
Fig. 1.
A patient undergoing ballon reduction of a calcaneal fracture. a Per operative image intensifier view inserting the first K-wire. b Balloon dilatation and fracture reduction. c Insertion of the polymethylmethacrylate (PMMA) bone cement under image intensifier. d Filling the void with PMMA bone cement. e Postoperative radiograph showing cement and reduction
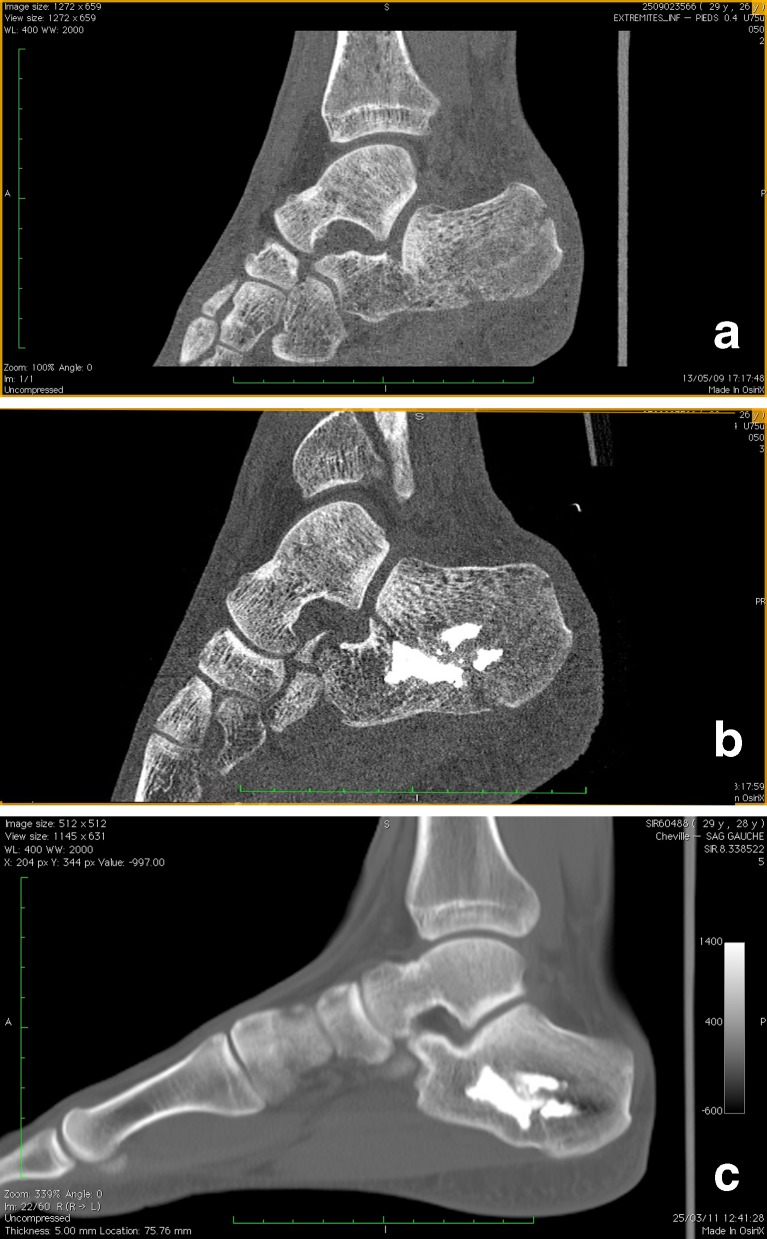
Fig. 2.
Patient 7, a Sanders IIB fracture in a bilateral case. a Preoperative view. b Postoperative view after balloon reduction and cement insertion. c A 22-month postoperative CT scan showing no arthritis
Assessment
Postoperative clinical evaluation was performed by the surgeon after three weeks, six weeks, three months, six months and each year after the fracture. Radiographs were made at each time point. All patients had a CT scan evaluation prior to the operation, immediately after the operation, at three months and each year postoperatively.
Clinical and radiological evaluation was performed by an independent orthopaedic surgeon at the latest follow up as noted in Table 1 in all patients. The American Orthopaedic Foot and Ankle Society (AOFAS) score [9] as well as the Babin score [10] were obtained at the latest follow up and as rated by the independent observer. Self evaluation was performed using the RAND-36 [11] quality of life questionnaire administered to the patients using a dedicated iPad application (RAND-SF36, Altavi, Luxembourg). Work status was also recorded independently.
Results
Eleven fractures (ten patients) were operated upon and had a three-year minimum follow up (36–70 months). No patient was lost to follow up and none was revised. All patients had resumed their previous professional activities after 15 days to four months. One patient had retired from public service but resumed her field walking activities after four months.
Clinical results
The mean AOFAS score was 84.5 (27–100). The AOFAS scores are shown in Table 3. The clinical results were rated good or excellent in 81.8 % of cases (nine fractures). According to the AOFAS and the Babin functional score, one result was rated poor and one fair. The mean physical component of the RAND-36 was 74.6 (28–97.5). Clinical data are shown in Table 3.
Table 3.
Radiological and clinical data at follow up
| Case number | AOFAS score | Functional assessment | RAND-36 physical | Boehler angle (°) | |||
|---|---|---|---|---|---|---|---|
| Babin | AOFAS | Preop | Postop | Latest follow up | |||
| 1 | 100 | Excellent | Excellent | 97.5 | −8 | 25 | 24 |
| 2 | 27 | Poor | Poor | 42.5 | −6 | 12 | 12 |
| 3 | 100 | Excellent | Excellent | 91.25 | −4 | 17 | 16 |
| 4 | 94 | Excellent | Excellent | 75.5 | 3 | 15 | 14 |
| 5 | 92 | Excellent | Excellent | 88 | −4 | 6 | 7 |
| 6 | 100 | Excellent | Excellent | 91.25 | 25 | 26 | 26 |
| 7 | 90 | Excellent | Excellent | 91.25 | 5 | 25 | 25 |
| 8 | 79 | Good | Good | 56.75 | −6 | 7 | 6 |
| 9 | 59 | Fair | Fair | 28 | −4 | 20 | 20 |
| 10 | 86 | Good | Good | 71.25 | −6 | 11 | 10 |
| 11 | 97 | Excellent | Excellent | 87.5 | −10 | 12 | 13 |
AOFAS American Orthopaedic Foot and Ankle Society
Radiological results
The mean preoperative Boehler angle was 2.45° as measured on conventional radiographs. The mean postoperative Boehler angle on radiographs was 15.27°; a mean improvement of 19.8° was obtained. At the latest follow up, upon examination by the independent observer, the mean Boehler angle was 15.9°; no joint subsidence was observed.
One patient with an excellent clinical result had no long-term CT scan examination at the final assessment because of ongoing pregnancy. Another patient refused to have the CT examination due to no pain and no complaint. Three patients showed signs of subtalar arthritis on the CT scan at the latest follow up. One patient only (one fracture) who had evidence of subtalar arthritis on the CT scan was offered a subtalar fusion by the surgeon, but refused to proceed. This patient is the one with the poor clinical result and was our second case. Postoperative CT scan showed an enlarged intra-articular fracture line as a reduction defect.
As a matter of fact, it was after operating on this patient we that developed the concept of lateral compression while inflating the balloon, to direct the pressure towards reduction rather than enlargement of the calcaneus bone. It can be said this patient had a reduction defect with an overall bad result. The postoperative CT scan evaluation prompted us to modify and improve the technique.
At the time of the latest follow up, all patients had resumed their work at the same level as before the fracture.
Discussion
Balloon reduction and fixation using various types of cement has been described elsewhere in articular displaced calcaneal fractures [1, 3, 4] and in other metaphyseal fracture locations [12–15]. As with any new technique in articular trauma, validation is provided only by sound clinical evaluation after a sufficient follow up.
We initiated the technique in September 2006 with one case and have consistently improved on the technique since that time [5–7].
The idea of using kyphoplasty balloons for a minimally-invasive reduction and fixation of calcaneal fractures arose from an apparent contradiction, inspired by Epstein [16]. First, the outcomes of these fractures depends often more on psychosocial factors (sex, work-related accident, tobacco smoking, in that order) than on anatomical factors, or the experience of the surgeon [16, 17]. Second, surgical treatment, when providing an unsatisfactory reduction, consistently leads to a poor clinical result, actually worse than functional, early weight-bearing treatment. Thus, we needed to find better ways to treat these fractures. Either by improving the quality of the reduction, or by decreasing soft tissue injury and local impingement between the implants and the fibular tendon sheath. Minimally invasive techniques might be able to improve on this [16, 18, 19]. Our technique accomplishes both.
Overall, the results in our small initial series are satisfactory with a long follow up.
However, the weaknesses of our series include the following: this is a small, relatively selected series of patients who have sought treatment in a relatively small department with no heavy traffic or industrial casualties and who have been able to express consent to being involved in the use of a new technique after careful explanation. The female-dominant, 20 %-only work-related, educated urban context is non typical in the usual calcaneal trauma setting. However, cases were not selected based on the fracture characteristics; four of them were Sanders III. Reduction and fixation of these difficult fractures may be problematic with the open technique. The balloon technique was able to address even difficult cases. We need more studies to extend indications to a regular male, smoking, with heavy work-related issues, calcaneum trauma population.
Definitive fixation of fractures in this series was obtained through the use of polymethylmetacrylate (PMMA) cement only as all metallic hardware used for reduction was removed after cement polymerisation at the time of skin closure. PMMA is a highly biocompatible and well-known material, which provided us with good initial reduction stability, and no loss of correction at the latest follow up. However, calcium phosphate bioadsorbable cement has been available for a while in the trauma field and its use has been described already in calcaneal fractures [20]. Although PMMA bone cement has provided us with good clinical results, a trend towards the use of more bioadsorbable materials has been observed and its use may be preferable in the current clinical setting for this application, especially since the review of the literature showed very positive results in metaphyseal fractures when compared to no graft or autogenous bone graft [21]. Long-term data are needed to asses this question.
Balloon reduction and cement fixation of calcaneal fractures is a work in progress as with any technique in its infancy. Following the indications given by the postoperative radiological assessment and the systematic CT scan review of anatomical results, modifications and improvements of the technique have been developed to obtain a better and easier reduction [5]. In this first series, one patient (patient #2) showed enlargement of the calcaneus on the postoperative CT scan. This patient had a poor AOFAS score at the latest follow up (68 months) but refused a further operation. As a matter of fact, after operating on this patient we developed the concept of lateral compression whilst inflating the balloon, to direct the pressure towards reduction rather than enlargement of the calcaneus bone. Additional techniques may be developed in the future to better address particular cases. The use of additional Steinman pins to obtain reduction and better “frame” the fracture site is one approach. Adding temporary external fixation may be an answer to better reduce the elevation of the greater tuberosity as found in some cases [22]. However, the balloon reduction tamp and cement fixation concept have provided us excellent tools to achieve reduction without performing an extensive approach damaging to the soft tissues, and we believe the tools and concept are here to stay in the arsenal available to the surgeon in regular clinical practice.
References
- 1.Bano A, Pasku D, Karantanas A, Alpantaki K, Souvatzis X, Katonis P. Intra-articular calcaneal fracture: closed reduction and balloon-assisted augmentation with calcium phosphate cement: a case report. Cases J. 2009;2:9290. doi: 10.1186/1757-1626-2-9290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Broome B, Mauffrey C, Statton J, Voor M, Seligson D. Inflation osteoplasty: In vitro evaluation of a new technique for reducing depressed intra-articular fractures of the tibial plateau and distal radius. J Orthop Traumatol. 2012;13(2):89–95. doi: 10.1007/s10195-012-0185-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta AK, Gluck GS, Parekh SG. Balloon reduction of displaced calcaneus fractures: surgical technique and case series. Foot Ankle Int. 2011;32(2):205–210. doi: 10.3113/FAI.2011.0205. [DOI] [PubMed] [Google Scholar]
- 4.Heiney JP, O’Connor JA. Balloon reduction and minimally invasive fixation (bramif) for extremity fractures with the application of fast-setting calcium phosphate. J Orthop. 2010;7(2):e8. [Google Scholar]
- 5.Jacquot F, Atchabahian A. Balloon reduction and cement fixation in intra-articular calcaneal fractures: a percutaneous approach to intra-articular calcaneal fractures. Int Orthop. 2011;35(7):1007–1014. doi: 10.1007/s00264-011-1249-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacquot F, Atchabahian A, Letellier T. Comment to the paper “balloon reduction and cement fixation in intra-articular calcaneal fractures: a percutaneous approach to intra-articular calcaneal fractures” by Jacquot et al. Int Orthop. 2011;35(11):1741–1742. doi: 10.1007/s00264-011-1319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacquot F, Mokhtar MA, Sautet A, Feron J-M. Balloon percutaneous reduction and cementoplasty of thalamic fractures of the calcaneum: four cases with two years follow-up. J Bone Joint Surg Br. 2011;93-B(Suppl IV):539. [Google Scholar]
- 8.Mauffrey C, Bailey JR, Hak DJ, Hammerberg ME (2012) Percutaneous reduction and fixation of an intra-articular calcaneal fracture using an inflatable bone tamp: description of a novel and safe technique. Patient Saf Surg 6(1):6. doi:10.1186/1754-9493-6-6 [DOI] [PMC free article] [PubMed]
- 9.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 10.Babin SR, Copin G, Simon P, Kempf JF, Vidal P. Statistical study of a series of 355 subtalar fractures of the calcaneus. Therapeutic conclusions. Int Orthop. 1985;9(3):171–179. doi: 10.1007/BF00268167. [DOI] [PubMed] [Google Scholar]
- 11.Loutzenhiser L, Lawrence SJ, Donegan RP. Treatment of select open calcaneus fractures with reduction and internal fixation: an intermediate-term review. Foot Ankle Int. 2008;29(8):825–830. doi: 10.3113/FAI.2008.0825. [DOI] [PubMed] [Google Scholar]
- 12.Hahnhaussen JHD, Weckbach S, Heiney JP, Stahel PF. Percutaneous inflation osteoplasty for indirect reduction of depressed tibial plateau fractures. Orthopedics. 2012;35(9):768–772. doi: 10.3928/01477447-20120822-04. [DOI] [PubMed] [Google Scholar]
- 13.Iida KSA, Ishiguro S. Clinical and radiological results of calcium phosphate cement-assisted balloon osteoplasty for Colles’ fractures in osteoporotic senile female patients. J Orthop Sci. 2010;15(2):204–209. doi: 10.1007/s00776-009-1449-1. [DOI] [PubMed] [Google Scholar]
- 14.Ishiguro SOY, Sudo A, Uchida A. Calcium phosphate cement-assisted balloon osteoplasty for a Colles’ fracture on arteriovenous fistula forearm of a maintenance hemodialysis patient. J Hand Surg Am. 2007;32(6):821–826. doi: 10.1016/j.jhsa.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Pizanis AGP, Pohlemann T, Burkhardt M. Balloon tibioplasty: a useful tool for reduction of tibial plateau depression fractures. J Orthop Trauma. 2012;26(7):e88–e93. doi: 10.1097/BOT.0b013e31823a8dc8. [DOI] [PubMed] [Google Scholar]
- 16.Epstein N, Chandran S, Chou L (2012) Current concepts review: intra-articular fractures of the calcaneus. Foot Ankle Int 33(1):79–86. doi:10.3113/FAI.2012.0079 [DOI] [PubMed]
- 17.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A(10):1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Rammelt S, Amlang M, Barthel S, Zwipp H. Minimally-invasive treatment of calcaneal fractures. Injury. 2004;35(Suppl 2):SB55–SB63. doi: 10.1016/j.injury.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 19.Rammelt S, Gavlik JM, Barthel S, Zwipp H. The value of subtalar arthroscopy in the management of intra-articular calcaneus fractures. Foot Ankle Int. 2002;23(10):906–916. doi: 10.1177/107110070202301004. [DOI] [PubMed] [Google Scholar]
- 20.Wee AT, Wong YS. Percutaneous reduction and injection of Norian bone cement for the treatment of displaced intra-articular calcaneal fractures. Foot Ankle Spec. 2009;2(2):98–106. doi: 10.1177/1938640009334153. [DOI] [PubMed] [Google Scholar]
- 21.Bajammal SSZM, Lelwica A, Tornetta P, 3rd, Einhorn TA, Buckley R, Leighton R, Russell TA, Larsson S, Bhandari M. The use of calcium phosphate bone cement in fracture treatment. A meta-analysis of randomized trials. J Bone Joint Surg Am. 2008;90(6):1186–1196. doi: 10.2106/JBJS.G.00241. [DOI] [PubMed] [Google Scholar]
- 22.Kissel CG, Husain ZS, Cottom JM, Scott RT, Vest J (2011) Early clinical and radiographic outcomes after treatment of displaced intra-articular calcaneal fractures using delta-frame external fixator construct. J Foot Ankle Surg 50(2):135–140. doi:10.1053/j.jfas.2010.12.026 [DOI] [PubMed]