Abstract
Purpose
The purpose of this study was to assess the value of SPECT/CT imaging in patients with chronic spinal pain.
Methods
This was a retrospective consecutive study. Patients with chronic neck or back pain from outpatient spinal clinics with clinical features raising the possibility of a facetogenic pain generator and non-conclusive MRI/CT findings were included. Imaging was performed on a dual-headed, hybrid SPECT/CT γ-camera with a low-dose CT transmission scan acquired after the SPECT study. SPECT/CT studies were viewed in the coronal, axial, and sagittal planes and in 3-dimensional mode. Descriptive statistical analysis was performed.
Results
Seventy-two patients were included (37 females, 35 males, mean age of 53.9 years). There were 25 cervical spine scans and 49 lumbar spine scans. In the cervical spine group, 13 (52 %) patients had scintigraphically active cervical facet joint arthropathy and ten (36 %) had other pathology identified. Two thirds of patients diagnosed with facet joint arthropathy received steroid guided injections following their scans. In the lumbar spine group 34 (69.4 %) patients had scintigraphically active lumbar facet joint arthropathy and eight had other pathology identified. Twenty patients (58.8 %) diagnosed with facet joint arthropathy subsequently received steroid guided injections.
Conclusions
Hybrid SPECT/CT imaging identified potential pain generators in 92 % of cervical spine scans and 86 % of lumbar spine scans. The scan precisely localised SPECT positive facet joint targets in 65 % of the referral population and a clinical decision to inject was made in 60 % of these cases.
Introduction
Degenerative facet joints are a recognised cause of persistent chronic spinal pain [1]. Facet joint arthropathy has been identified as a source of pain in 15–45 % of patients with chronic low back pain lasting over six weeks that have failed conservative management and in 39 % of patients with chronic cervical pain [2, 3]. Spinal facets can cause localised spinal pain as well as referred dermatomal pain to the head, chest wall, upper and lower extremities [4, 5].
Magnetic resonance imaging (MRI) has been the gold standard for spinal imaging. However, diagnosis of facet joint arthropathy continues to pose a challenge to clinicians. Conventional radiological techniques such as MRI, plain computed tomography (CT), dynamic bending films and planar radionuclide bone scanning are inconsistently reliable when diagnosing or accurately localising facetogenic pain generators [6]. Controlled comparative local anaesthetic blocks have become an acceptable alternative for confirming the diagnosis in patients clinically suspected of having characteristic facet joint arthropathy [7, 8].
Radionuclide bone scintigraphy with single photon emission computed tomography (SPECT) provides functional imaging and is used to detect microcalcification due to increased osteoblastic activity. In the absence of other pathology the foci of increased osteoblastic activity reflect areas of mechanical stress and degenerative change in the skeleton [9–11]. SPECT has been widely used to evaluate patients with spinal pain and facet joint arthropathy [12, 13]. For the detection of clinically significant facetal arthropathy, SPECT has been reported to have a sensitivity of 85–100 % and specificity of up to 71 % [12, 14]. However, with just SPECT imaging in isolation there can be difficulty in precise localisation of the spinal segment affected due to anatomical variants and the low spatial resolution of the scan (approximately 7 mm) [12, 14]. Development of multimodality SPECT/CT has allowed the high sensitivity of SPECT to be combined with the specificity of CT. The CT component improves the SPECT image quality by correcting for soft tissue attenuation, thus improving sensitivity of the scan for areas of abnormal tracer activity. The CT has a higher spatial resolution of 1 mm and fusion of the scan images allows better localisation of areas of abnormal tracer activity and defines anatomical variants that may affect segmental nomenclature. The anatomy on the CT component also improves scan specificity by defining the structural pathology causing increased tracer activity. SPECT/CT is gaining popularity and has already been shown to improve diagnostic accuracy in the staging of skeletal metastases [15–17], patellofemoral disorders [18] and anterior cruciate ligament reconstructions [19].
The role for SPECT/CT in relation to the gold standard of magnetic resonance imaging when evaluating patients with benign skeletal disease remains unclear. McDonald et al. have described the use of SPECT/CT to identify facetal pain generators in a series of patients undergoing evaluation for posterior dynamic stabilisation [20]. Currently, there is still only limited data on the usefulness of SPECT/CT in clinical practice [9, 10, 21, 22].
The aim of this retrospective study is to assess the value of SPECT/CT imaging in patients with chronic spinal pain from a spinal outpatient clinic population and its utility as a diagnostic tool in determining further clinical management.
Materials and methods
Patients population
A retrospective study was conducted of consecutive patients who underwent SPECT/CT scanning for chronic neck or back pain in the Nuclear Medicine Department at the Royal Free Hospital NHS Trust, London, from October 2009 until February 2011.
Inclusion criteria were (1) chronic (>six weeks) back or neck pain, (2) localised or referred pain clinically suggestive of facet joint arthropathy, (3) MRI findings insufficient to determine further clinical management, (4) patients who have failed conservative management in the primary care setting, namely, analgesia and rest. Patients who had cauda equina syndrome, acute onset of spinal pain, malignancy or pregnancy were all excluded.
Data was retrieved from the medical records and imaging archive. Demographic characteristics including patient’s age and gender were collected. The indication for the scan by the referring clinician, imaging reports and clinical management following the SPECT/CT results were reviewed.
SPECT acquisition and imaging protocol
Imaging was performed on a dual-headed, hybrid SPECT/CT γ-camera (Siemens Symbia T16 True Point) with a low energy high resolution (LEHR) collimator. SPECT images were acquired in a 60-step (20 s/stop), 360° non-circular orbit and reconstructed in a 128 × 128 matrix using a three -dimensional ordered-subsets expectation maximization (OSEM) algorithm. Data was reconstructed by Iterative Reconstruction using Flash 3D with four subsets and eight iterations, utilising a Gaussian filter.
A low-dose CT transmission scan was acquired after the SPECT study. The CT parameters used were 130 kVp and 65–100 mAs (65mAs for lumbar spine and 100mAs for cervical spine). Reconstruction was performed in a 512 × 512 matrix at slice thickness of 5 mm. The CT was co- registered with the SPECT using the nuclear medicine workstation (Siemens eSoft). CT attenuation correction was applied to SPECT images. SPECT/CT studies were viewed in the coronal, axial, and sagittal planes and in 3-dimensional mode.
Statistical analysis
SPSS 16.0 software (SPSS Inc, IL, USA) was used for descriptive statistical analysis. Results are presented as frequencies, percentages and descriptive statistics.
Results
Seventy-two patients met the inclusion criteria and were included in the analysis. There were 37 females and 35 males with a mean age of 53.9 years (SD 17.3, range 22–84). Two patients had cervical and lumbar spine scans. Therefore, a total of 74 scans were included in the study: 25 cervical and 49 lumbar spine.
Cervical spine group
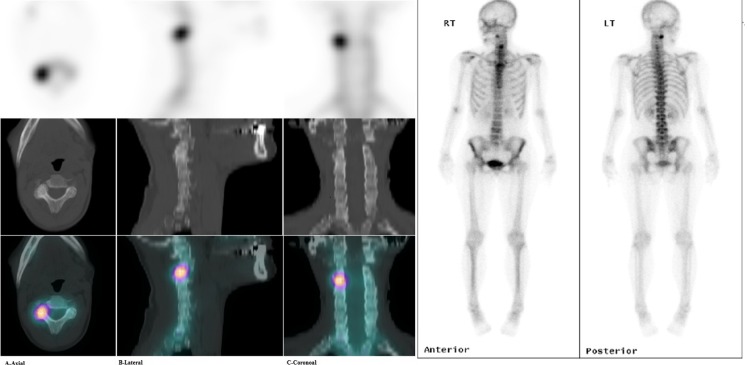
Twenty-five scans were included, 13 (52 %) patients were found to have evidence of facet joint arthropathy as likely pain generator (Fig. 1), nine (36 %) had other changes compatible with degenerative disc disease, one had an osteoid osteoma and one had a normal study as shown in Table 1. Referring specialists had clinically identified localised tenderness in eight/25 (32 %) patients, however this correlated with SPECT/CT findings in only one/eight (12.5 %) patient. Almost two thirds of patients (8/13) diagnosed with facet joint arthropathy received steroid injections while the rest had physiotherapy or conservative management as shown in Table 2.
Fig. 1.
Images of 75-year-old man with clinically generalised chronic neck pain. Planar images suggest activity in the cervical spine. SPECT images, low dose CT and fused SPECT/CT images show localised right C2/C3 facet joint arthropathy. SPECT single photon emission computed tomography
Table 1.
Findings of SPECT/CT scans for patients with neck and back pain
| Region | SPECT/CT diagnosis | No. patients (%) |
|---|---|---|
| Cervical spine | Unilateral facet joint disease uni-level | 10 (40) |
| Bilateral facet joint disease multi-level | 3 (12) | |
| Degenerative disease | 9 (36) | |
| Normal cervical spine study | 1 (4) | |
| Osteoid osteoma | 1 (4) | |
| Degenerative spinous process | 1 (4) | |
| Total | 25 (100) | |
| Lumbar spine | Unilateral facet joint disease uni-level | 18 (36.7) |
| Unilateral facet joint disease multi-level | 6 (12.2) | |
| Bilateral facet joint disease uni-level | 7 (14.3) | |
| Bilateral facet joint disease multi-level | 3 (6.1) | |
| Degenerative disease | 6 (12.2) | |
| Discitis | 2 (4.1) | |
| Normal lumbar spine study | 7 (14.3) | |
| Total | 49 (100) |
SPECT single photon emission computed tomography
Table 2.
Clinical outcome for patients with neck and back pain following findings of SPECT/CT scans
| Diagnosis per SPECT/CT | Clinical outcome | No. patients (%) |
|---|---|---|
| Cervical spine | ||
| Cervical facet joints arthropathy (n = 13) | Steroid Injections | 8 (61.5) |
| Conservative management | 3 (23.0) | |
| Physiotherapy | 2 (15.5) | |
| Total | 13 (100) | |
| Degenerative (n = 8) | Surgical treatment | 5 (62.5) |
| Physiotherapy | 2 (25.0) | |
| Conservative management | 1 (12.5) | |
| Total | 8 (100) | |
| Other (n = 4) | Surgical treatment | 1 (25.0) |
| Conservative management | 2 (50.0) | |
| Further investigations | 1 (25.0) | |
| Total | 4 (100) | |
| Lumbar spine | ||
| Lumbar facet joints arthropathy (n = 34) | Steroids injection | 20 (58.8) |
| Conservative management | 7 (20.6) | |
| Physiotherapy | 4 (11.7) | |
| Surgical treatment | 2 (5.90) | |
| Self-limiting symptoms | 1 (3.0) | |
| Total | 34 (100) | |
| Degenerative disease (n = 6) | Steroid injection | 2 (33.4) |
| Physiotherapy | 1 (16.6) | |
| Conservative management | 2 (33.4) | |
| Surgical treatment | 1 (16.6) | |
| Total | 6 (100) | |
| Other (n = 9) | Antibiotics therapy | 2 (22.2) |
| Steroid injection | 2 (22.2) | |
| Conservative management | 2 (22.2) | |
| Physiotherapy | 3 (33.4) | |
| Total | 9 (100) | |
SPECT single photon emission computed tomography
Lumbar spine group
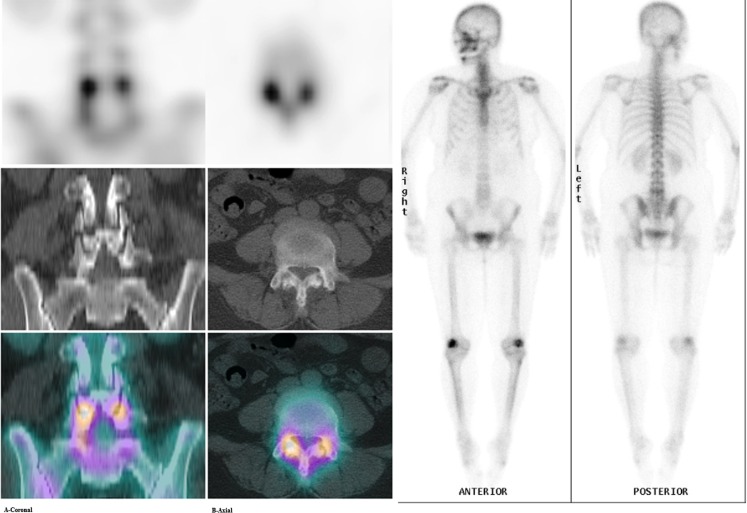
Forty-nine patients were included. Of these, 34 (69.4 %) were found to have evidence of facet joint arthropathy as the likely pain generator (Fig. 2). Six patients had other evidence of degenerative disease, two patients had discitis and seven (14.3 %) patients had a normal lumbar spine study as shown in Table 1. Referring specialists (neurosurgeon, two orthopaedic surgeons) had clinically suspected facet arthropathy in 21/49 (42.9 %) patients, which correlated with SPECT/CT findings in eight/21 (38 %) patients. Twenty patients 20/34 (58.8 %) diagnosed with facet joint arthropathy received steroid injections while the rest had physiotherapy or conservative management as shown in Table 2.
Fig. 2.
Images of 59-year-old woman with 12 months history of non-localised low back pain. Planar images suggest degenerative activity in the lower lumbar spine. SPECT images, low dose CT and fused SPECT/CT images show localised bilateral L4/L5 facet joint joints arthropathy. SPECT single photon emission computed tomography
Discussion
Facet joint injection is an invasive procedure that carries a risk of complications, particularly in the cervical spine [6, 7, 23]. The literature evaluating the utility of this intervention has produced conflicting evidence and the National Institute and Clinical Excellence (NICE), the UK’s healthcare watchdog, has not supported its widespread use in patients with chronic back pain [24]. One of the reasons for the difficulties in producing a consistent response arises due to inappropriate selection of targets for therapeutic injection. Gorbach et al. [23] found the extent of facet joint arthropathy defined anatomically on MRI and CT was not a significant predictor for outcome in a cohort of 42 patients undergoing facet joint blocks (p = 0.57–0.95). Carrino et al. [25] used weighted Kappa statistics for measuring inter-observer agreement between four specialist readers of MR lumbar spine for facet arthropathy in 111 scans and found inter-observer variability of 0.54 (CI 95 %, 0.50–0.57). Inconsistent interobserver variability suggests that the test does not provide an easily interpretable assessment and both MRI and CT reports can be inconclusive regarding the presence or absence of facetal arthropathy. Even when it is reported on scans the facetal degeneration is often widespread, without an obvious target for injection defined on the basis of the anatomy.
The fusion of anatomic and molecular images obtained with integrated SPECT/CT systems allows more accurate attenuation correction and precise anatomic localisation of lesions with increased tracer uptake. SPECT/CT increases reporter confidence in the correct localisation of uptake compared to simple planar or SPECT studies [11, 22, 26]. SPECT/CT also enables the detection of tracer avid lesions that are not appreciated by simple planar scintigraphy or SPECT performed without co-registered CT [15, 27, 28]. When performed supplementary to conventional imaging techniques, the SPECT/CT images have an incremental diagnostic value that can influence clinical management by selecting only SPECT positive facet joint targets [9, 20, 29].
Chronic spinal pain with mechanical features and no conclusive diagnosis after conventional imaging is a common clinical problem in the orthopaedic and spinal outpatient clinic. The group of patients in this study were heterogeneous, with the final clinical diagnosis including facet joint arthropathy, other degenerative spinal disease, discitis and osteoid osteoma. Whilst the mixed sample population could be seen as a limitation of the study, we believe it adds credence to the use of SPECT/CT as this patient group is typical of that commonly encountered in routine clinical practice. Once the diagnostic information provided by the SPECT/CTs was available to the treating clinicians, patients proceeded to have either steroids injections, conservative or surgical interventions. The effectiveness of these interventions were not evaluated in this study since the main aim was to assess the diagnostic value of SPECT/CTs.
There is a paucity of literature investigating the use of hybrid SPECT/CT imaging in benign orthopaedic and spinal conditions. Our data corroborate that of McDonald et al. [20], which looked at the use of SPECT/CT to identify facet joint arthropathy in patients who were being considered for posterior stabilisation. In his case series, SPECT/CT provided localisation of lesions in all 36 patients. Similarly, Even-Sapir et al. [30], who assessed the role of SPECT/CT in 76 consecutive non-oncologic patients, found that SPECT/CT was of incremental clinical value in 89 % of patients. To our knowledge, there are no studies evaluating the use of SPECT/CT for the diagnosis of cervical facet joint arthropathy with which to compare to our findings.
Summary
In the majority of patients studied, the SPECT/CT scan guided the referring clinicians in determining further clinical management, mainly by providing precise localisation of SPECT positive fact joint arthropathy.
Contributor Information
Hosam E. Matar, Email: hematar@doctors.org.uk
Shaunak Navalkissoor, Email: s.navalkissoor@nhs.net.
Marko Berovic, Email: mberovic@doctors.org.uuk.
Rohit Shetty, Email: rohitrshetty@yahoo.com.
Nicholas Garlick, Email: n.garlick@nhs.net.
Adrian T. H. Casey, Email: adriancasey@nhs.net
Ann-Marie Quigley, Email: ann-marie.quigley@nhs.net.
References
- 1.Bogduk N (2005) The zygapophysial joints. In Clinical Anatomy of the Lumbar Spine and Sacrum. 3rd edn. Churchill Living stone, New York
- 2.Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15. doi: 10.1186/1471-2474-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapophysial joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994;19:1132–1137. doi: 10.1097/00007632-199405001-00006. [DOI] [PubMed] [Google Scholar]
- 4.Fukui S, Ohseto K, Shiotani M, Ohno K, Karasawa H, Naganuma Y. Distribution of referral pain from the lumbar zyg apophyseal joints and dorsal rami. Clin J Pain. 1997;13:303–307. doi: 10.1097/00002508-199712000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Windsor RE, King FJ, Roman SJ, Tata N, Cone-Sullivan LA, Thampi S, Acebey M, Gilhool JJ, Rao R, Sugar R. Electrical stimulation induced lumbar medial branch referral patterns. Pain Physician. 2002;5:347–353. [PubMed] [Google Scholar]
- 6.Boswell MV, Shah RV, Everett CR, Sehgal N, Mckenzie-Brown AM, Abdi S, Bowman RC, Deer TR, Datta S, Colson JD, Spillane WF, Smith HS, Lucas-Levin LF, Burton AW, Chopra P, Staats PS, Wasserman RA, Manchikanti L. Interventional techniques in the management of chronic spinal pain: Evidence-based practice guidelines. Pain Physician. 2005;8:1–47. [PubMed] [Google Scholar]
- 7.Bogduk N. Evidence-informed management of chronic low back pain with facet injections and radiofrequency neurotomy. Spine J. 2008;8:56–64. doi: 10.1016/j.spinee.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Sehgal N, Dunbar EE, Shah RV, Colson JD. Systematic review of diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: an update. Pain Physician. 2007;10:213–228. [PubMed] [Google Scholar]
- 9.Delbeke D, Schöder H, Martin WH, Wahl RL. Hybrid imaging (SPECT/CT and PET/CT): improving therapeutic decisions. Semin Nucl Med. 2009;39:308–340. doi: 10.1053/j.semnuclmed.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Filippi L, Schillaci O. Usefulness of hybrid SPECT/CT in 99mTc-HMPAO-labeled leukocyte scintigraphy for bone and joint infections. J Nucl Med. 2006;47:1908–1913. [PubMed] [Google Scholar]
- 11.Utsunomiya D, Shiraishi S, Imuta M, Tomiguchi S, Kawanaka K, Morishita S, Awai K, Yamashita Y. Added value of SPECT/CT fusion in assessing suspected bone metastasis: comparison with scintigraphy alone and nonfused scintigraphy and CT. Radiology. 2006;238:264–271. doi: 10.1148/radiol.2373041358. [DOI] [PubMed] [Google Scholar]
- 12.Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, Fogelman I, Gibson T. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–1273. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- 13.Dutton JA, Hughes SP, Peters AM. SPECT in the management of patients with back pain and spondylolysis. Clin Nucl Med. 2000;25:93–96. doi: 10.1097/00003072-200002000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Holder LE, Machin JL, Asdourian PL, Links JM, Sexton CC. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. J Nucl Med. 1995;36:37–44. [PubMed] [Google Scholar]
- 15.Horger M, Bares R. The role of single-photon emission computed tomography/computed tomography in benign and malignant bone disease. Semin Nucl Med. 2006;36:286–294. doi: 10.1053/j.semnuclmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Husarik DB, Steinert HC. Single-photon emission computed tomography/computed tomography for sentinel node mapping in breast cancer. Semin Nucl Med. 2007;37:29–33. doi: 10.1053/j.semnuclmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Krausz Y, Israel O. Single-photon emission computed tomography/computed tomography in endocrinology. Semin Nucl Med. 2006;36:267–274. doi: 10.1053/j.semnuclmed.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Hirschmann MT, Davda K, Iranpour F, Rasch H, Friederich NF. Combined single photon emission computerised tomography and conventional computerised tomography (SPECT/CT) in patellofemoral disorders: a clinical review. Int Orthop. 2011;35:675–680. doi: 10.1007/s00264-010-1049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirschmann MT, Mathis D, Rasch H, Amsler F, Friederich NF, Arnold MP (2012) SPECT/CT tracer uptake is influenced by tunnel orientation and position of the femoral and tibial ACL graft insertion site. Int Orthop. doi:10.1007/s00264-012-1704-5 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 20.McDonald M, Cooper R, Wang MY. Use of computed tomography-single-photon emission computed tomography fusion for diagnosing painful facet arthropathy. Technical note. Neurosurg Focus. 2007;22:E2. doi: 10.3171/foc.2007.22.1.2. [DOI] [PubMed] [Google Scholar]
- 21.Strobel K, Burger C, Seifert B. Husarik DB, Soyka JD, Hany TF (2007) Characterization of focal bone lesions in the axial skeleton: performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. AJR Am J Roentgenol. 2007;188:W467–W474. doi: 10.2214/AJR.06.1215. [DOI] [PubMed] [Google Scholar]
- 22.Strobel K, Burger C, Seifert B, Husarik DB, Soyka JD, Hany TF. Characterization of focal bone lesions in the axial skeleton: performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. AJR Am J Roentgenol. 2007;188:467–474. doi: 10.2214/AJR.06.1215. [DOI] [PubMed] [Google Scholar]
- 23.Gorbach C, Schmid MR, Elfering A, Hodler J, Boos N. Therapeutic efficacy of facet joint blocks. AJR Am J Roentgenol. 2006;186:1228–1233. doi: 10.2214/AJR.04.1042. [DOI] [PubMed] [Google Scholar]
- 24.Savigny P, Kuntze S, Watson P, Underwood M, Ritchie G, Cotterell M, Hill D, Browne N, Buchanan E, Coffey P, Dixon P, Drummond C, Flanagan M, Greenough C, Griffiths M, Halliday-Bell J, Hettinga D, Vogel S, Walsh D. Low back pain: early management of persistent non-specific low back pain. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners; 2009. [Google Scholar]
- 25.Carrino JA, Lurie JD, Tosteson AN, Tosteson TD, Carragee EJ, Kaiser J, Grove MR, Blood E, Pearson LH, Weinstein JN, Herzog R. Lumbar spine: reliability of MR imaging findings. Radiology. 2009;250:161–170. doi: 10.1148/radiol.2493071999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Even-Sapir E. Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med. 2005;46:1356–1367. [PubMed] [Google Scholar]
- 27.Papathanassiou D, Bruna-Muraille C, Jouannaud C, Gagneux-Lemoussu L, Eschard JP, Liehn JC. Single-photon emission computed tomography combined with computed tomography (SPECT/CT) in bone diseases. Joint Bone Spine. 2009;76:474–480. doi: 10.1016/j.jbspin.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Horger M, Eschmann SM, Pfannenberg C, Vonthein R, Besenfelder H, Claussen CD, Bares R. Evaluation of combined transmission and emission tomography for classification of skeletal lesions. AJR Am J Roentgenol. 2004;183:655–661. doi: 10.2214/ajr.183.3.1830655. [DOI] [PubMed] [Google Scholar]
- 29.Tharp K, Israel O, Hausmann J, Bettman L, Martin WH, Daitzchman M, Sandler MP, Delbeke D. Impact of 131I-SPECT/CT images obtained with an integrated system in the follow-up of patients with thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2004;31:1435–1442. doi: 10.1007/s00259-004-1565-2. [DOI] [PubMed] [Google Scholar]
- 30.Even-Sapir E, Keidar Z, Sachs J, Engel A, Bettman L, Gaitini D, Guralnik L, Werbin N, Iosilevsky G, Israel O. The new technology of combined transmission and emission tomography in evaluation of endocrine neoplasms. J Nucl Med. 2001;42:998–1004. [PubMed] [Google Scholar]