Abstract
Purpose
In the diagnosis of femoroacetabular impingement (FAI), magnetic resonance imaging (MRI) and X-ray are widely accepted methods for detection. When evaluating the hip head-neck junction using MRI, oblique axial sequences are required. However, the construction and analysis of these images are restricted to specialist radiologists and surgeons in the field of hip joint MRI. This study sought to investigate whether ultrasound, a simple and inexpensive method, can be used as a reliable tool for diagnosing Cam-type FAI.
Methods
Forty patients, with a mean age of 39 years (range, 18–61 years), were consecutively included in this prospective study, following a diagnosis of Cam-type FAI on an oblique axial MRI. All patients underwent ultrasound examination in the ventral longitudinal section at 20° external rotation, neutral position and 20° internal rotation. The alpha angle, anterior offset, offset-ratio, and anterior femoral distance (AFD) were measured using MRI and ultrasound.
Results
No significant differences were detected between the alpha angle on MRI and that using ultrasound in the neutral position or in 20° internal rotation, with strong correlations observed between these parameters (r = 0.67 for neutral position, r = 0.77 for 20° internal rotation). The Pearson’s correlation coefficient for the alpha angle on MRI and the ratio of AFD/anterior offset on ultrasound in internal rotation was 0.76 (p < 0.0001).
Conclusions
The results show strong correlations between MRI and ultrasound measurements in patients with Cam-type FAI. Consequently, ultrasound may provide a useful tool for the early diagnosis of Cam-type FAI in daily practice.
Introduction
Femoroacetabular impingement (FAI) is postulated to be a major cause of early osteoarthritis of the hip [1–3]. CAM-type FAI is characterised by insufficient anterior head-neck offset, which leads first to labral tears and second to acetabular hyaline cartilage damage [1]. Therefore, the early diagnosis of CAM-type impingement before the cartilage is damaged is of major importance in orthopaedics. Patient history and physical examination are still important information required for the diagnosis of the CAM-type FAI [4]. After this, first choice for imaging is an X-ray with anteroposterior (AP) and lateral projections of the hip. But, for X-rays to be reliable, the correct technique must be used to produce images of a high quality [5–7]. In some cases, computed tomography (CT) is used to provide a more detailed visualisation of the bony structures; however, this method imposes a high radiation exposure to the patient and lacks any soft-tissue information.
In contrast to these methods, magnetic resonance imaging (MRI) is now routinely used to assess both bone and soft-tissue structures for patients with hip dysfunction. In addition, the use of contrast material can further improve the diagnostic potential of labral and cartilage pathologies in these images. For evaluation of the femoral head-neck junction using MRI, angled axial sequences or radial sections are required. These images are then analysed using established parameters, such as the alpha angle, as described by Nötzli [8], and the anterior offset, as described by Eijer [9], both of which aid in giving precise information about the extent of the FAI in the joint. However, the examination time and costs involved in taking and interpreting these images are high, as only radiologists and specialised hip joint surgeons are capable of constructing and analysing these tilted scans. Current developments have involved the use of biochemical MRI techniques, such as delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) [10], which can detect cartilage damage before morphological transformation. But these technical advances are not widely known or available to most surgeons and their patients.
A quick, cheap and widespread alternative imaging modality for the hip joint could be ultrasonography. In the past, only one group has published data concerning the use of ultrasound for the diagnosis of intra-articular pathologies of the hip [11, 12]. In their studies, they examined the sonographic diagnosis of labral tears. Indeed, the paucity of available literature concerning the use of ultrasonography to image the hip could be because of the difficulty of imaging a ball-in-socket joint. It might be expected that acoustic attenuation caused by the ball joint would impede the use of ultrasound to obtain adequate imaging. However, the prominence, or “bump”, in patients with CAM-type FAI is situated peripherally, outside the acetabulum. This led us to the hypothesis that these bumps could be detected and measured using ultrasound. Thus, the aim of this study was to prospectively examine patients with CAM-type FAI using standard MRI and compare this with the potential diagnostic utility of ultrasound imaging.
Materials and methods
In this prospective study, 40 patients, with a mean age of 39 years (range, 18–61 years) were consecutively included after indication for hip arthroscopy between June 2010 and January 2012. Approval for this study was granted by our local ethics committee (Ethic Committee no. 1110–2011). Inclusion criteria were the existence of a preoperative MRI with axial oblique sequences and a diagnosis of CAM-type FAI. Exclusion criteria were patients who presented with osteoarthritis or pincer-type impingement. The use of a contrast material was not relevant, because we focused on the bony structure, which can be visualised irrespective of a contrast medium. Only patients who had an MRI performed at our institution were included, to ensure a consistent MRI protocol. The examinations were carried out on a 1.5-T scanner (Symphony Quantum; Siemens, Erlangen, Germany) with a flexible surface coil. The protocol included a three-dimensional isotropic, T1-weighted spoiled gradient echo (MPRAGE/Turbo-FLASH) sequence with water excitation (25-cm field of view, 1-mm slice thickness, 256 9 256 matrix, TR/TE/flip angle = 1970 ms/7 ms/158, 1 average). Multiplanar reformation was carried out to generate 2-mm-thick oblique axial plane images, parallel to the long axis of the femoral neck.
All patients underwent a preoperative ultrasound of the hip joint. Sonographic examination was conducted in the ventral longitudinal section in 20° external rotation, neutral position and 20° internal rotation. In this standard section, the ultrasonic transducer was positioned along the course of the long axis of the femoral neck. The acetabular edge, capsule, femoral head and femoral neck were visible as anatomical reference points. In addition, this section also presented the following muscles: sartorius, rectus femoris, tensor fascia lata, iliopsoas, and gluteus medius. The same ultrasonic device (Nemio XG, Toshiba Medical Systems GmbH, Neuss, Germany), with a 5 MHz linear transducer, was used for all examinations.
Anonymised ultrasound and MR images were analysed independently throughout the study period using JiveX DICOM Viewer (Version 4.5, © VISUS Technology Transfer GmbH, Bochum, Germany) by an experienced orthopaedic surgeon specialised in hip joint diseases. On the angled axial MR image, we measured through the midfemoral neck to determine the alpha angle, as per the method of Nötzli et al. [8], the anterior head-neck offset, as described by Eijer et al. [9], the anterior femoral distance (AFD), as described by Lohan et al. [13], and the diameter of the head. The offset-ratio, defined as the quotient of the head-neck offset divided by the head diameter, was also assessed. All ultrasound measurements were repeated by the same orthopaedic surgeon with more than ten years’ experience in ultrasound examinations, followed by a second surgeon with five years’ experience and by a third surgeon with two years’ experience to determine the intra-observer and interobserver reliability.
On all three sonographs (20° external rotation, neutral position and 20° internal rotation), measurements of the same parameters were adjusted for the lack of the visible long axis of the femoral neck and the whole circumference of the femoral head. Briefly, on the visible sector of the femoral head, three points were selected to construct a circle. The diameter of this circle corresponded to the diameter of the femoral head. The first arm of the alpha angle was a line running parallel to the visible surface of the femoral neck through the centre of this circle. The second arm of the angle was drawn from the centre of this circle to the point where the head extended beyond the margin of this circle (Fig. 1). For the anterior head-neck offset, a tangent was drawn to the visible surface of the femoral neck, and another line parallel to the first along the anterior outer part of the head; the distance between these two lines was determined as the offset (Fig. 2). For the AFD, we measured the distance between these same first and second lines drawn parallel to the first along the greatest perpendicular depth of epiphyseal overgrowth at the anterior femoral head-neck junction (Fig. 3).
Fig. 1.
Ultrasound of the hip joint in 20° internal rotation, showing the circle constructed on the visible sector of the femoral head. The alpha angle is the angle between a line parallel to the visible surface of the femoral neck (dotted line) through the centre of the circle and a line from the centre of this circle to the point where the anterior femoral head-neck junction exits the circle
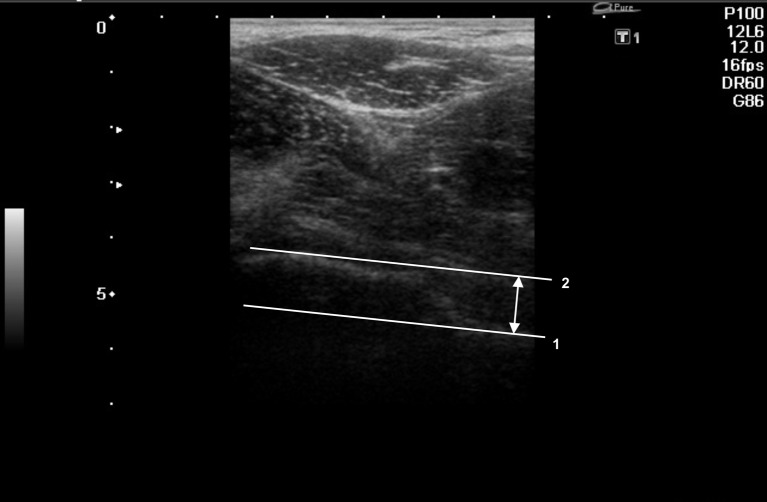
Fig. 2.
Ultrasound of the hip joint in neutral position. The anterior head-neck offset is measured as the distance between the two lines. The first line (1) is placed as a tangent to the visible surface of the femoral neck; the second line (2) is drawn parallel to the first along the anterior outer part of the femoral head
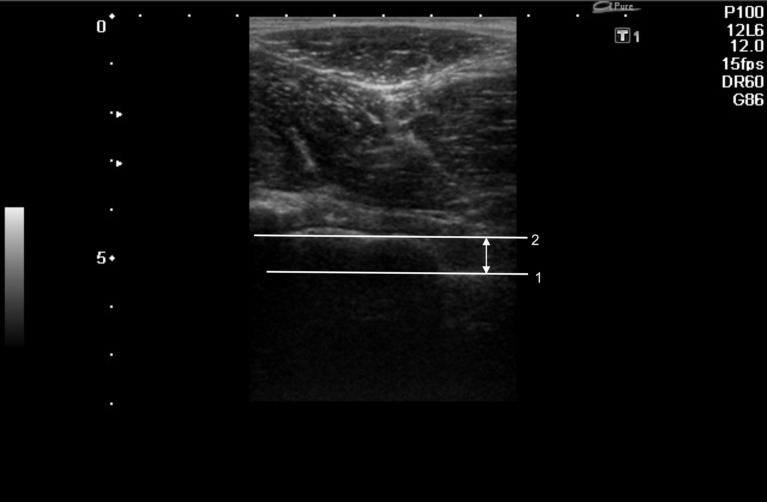
Fig. 3.
Ultrasound of the hip joint in 20° internal rotation. The anterior femoral distance is measured as the distance between the two lines. The first line (1) is placed as a tangent to the visible surface of the femoral neck; the second line (2) is drawn parallel to the first along the greatest perpendicular depth of epiphyseal overgrowth at the anterior femoral head-neck junction
In each hip joint position, the head diameter was measured by ultrasound and compared to the head diameter determined using MRI, to assess the accuracy of the head circle constructed in the sonographs. Furthermore, with the three head diameter values obtained from one hip, the reproducibility of this method was analysed. Statistical analyses were performed using SPSS® software (Version 17.0; SPSS Inc., Chicago, IL, USA). A t-test was used to evaluate differences between parameters on images from MRI and ultrasound. Pearson’s correlation coefficients were used to determine the degree of agreement between measurements obtained from ultrasound and MRI. Bland and Altman plots were further conducted to provide a visual assessment of the agreement between parameters determined using the two techniques. This plot included horizontal lines depicting the level of bias and the limits of agreement [14].
Results
The mean head diameter was 45.9 mm on the oblique axial MR image. For the three ultrasound positions, the mean head diameters were 45.1 mm in 20° external rotation, 44.4 mm in neutral position and 45.1 mm in 20° internal rotation. There was no significant difference between the head diameter values.
On the angled axial MR image, the mean alpha angle was determined to be 64.8°; this was comparable to the mean alpha angle in the ultrasound positions of 61.2° in the neutral position, and 65.6° in 20° internal rotation. Again, no significant differences were observed between the alpha angle on MRI and that detected using ultrasound in the neutral position or in 20° internal rotation. However, the mean alpha angle for the ultrasound in 20° external rotation was 41.6°, which was significantly different from that on MRI.
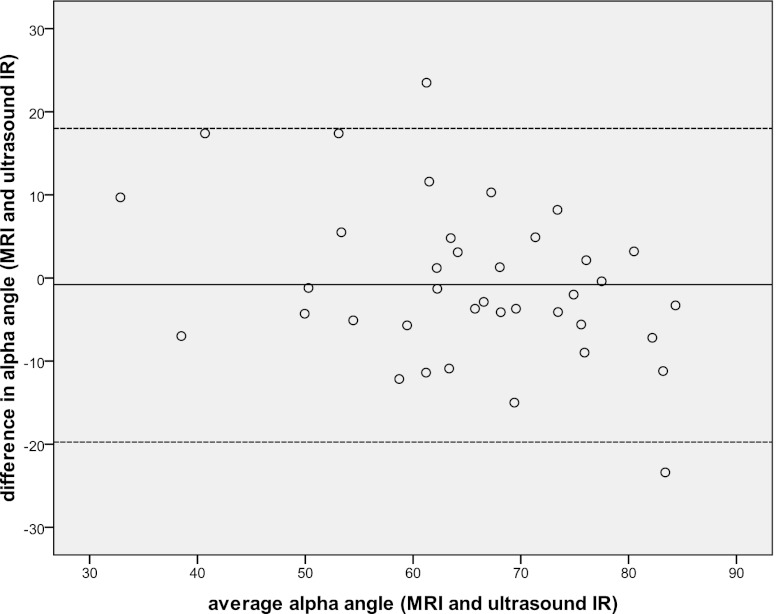
We observed a significant correlation for the alpha angle between the MRI values and those for ultrasound in the neutral position and 20° internal rotation (r = 0.67, p < 0.0001 for neutral position; r = 0.77, p < 0.0001 for 20° internal rotation). The Bland-Altman plot also shows this high level of agreement (Fig. 4). The average value of the alpha angle on MRI and ultrasound (x-axis) was plotted against the difference between them (y-axis). As expected, no correlation for the alpha angle was found between MRI and ultrasound in 20° external rotation.
Fig. 4.
Bland-Altman plot of the alpha angle measured on MRI and ultrasound in 20° internal rotation (ultrasound IR). The x-axis plots the mean angle of both values (MRI and ultrasound) against the difference between them on the y-axis. The line in the middle represented the mean value, the two dotted lines represented two standard deviations of the differences
We observed significant correlations for the AFD between MRI and ultrasound in the neutral position, and for the AFD and offset ratio between MRI and ultrasound in 20° internal rotation. However, values for the AFD and anterior offset were always greater on the ultrasound images than were those on MR images (Table 1). For the 11 (27 %) hips with a strict anterior femoral bump (described intraoperatively), we found no significant difference for the AFD, and the anterior offset between the MRI and ultrasound in 20° internal rotation and the Pearson’s correlation coefficient was high (r = 0.93, p < 0.001 for the AFD; r = 0.80, p < 0.019 for the anterior offset).
Table 1.
Comparison of the means and standard deviations of parameters measured on MRI or ultrasound in the neutral position and in 20° internal rotation. The Pearson’s correlation coefficient is listed for correlations between ultrasound and MRI
| MRI | Ultrasound in neutral position | Ultrasound in 20° internal rotation | |
|---|---|---|---|
| AFD (anterior femoral distance) | 4.6 ± 1.7 | 6.8 ± 3.8 | 6.2 ± 3.1 |
| 0.346 (p < 0.033) | 0.491 (p < 0.002) | ||
| Anterior offset | 7.1 ± 2.2 | 10.8 ± 3.6 | 8.7 ± 3.1 |
| No correlation | No correlation | ||
| Offset ratio | 0.16 ± 0.05 | 0.25 ± 0.07 | 0.20 ± 0.07 |
| No correlation | 0.428 (p < 0.008) | ||
| Ratio AFD/ anterior offset | 0.72 ± 0.35 | 0.66 ± 0.35 | 0.74 ± 0.36 |
| 0.561 (p < 0.0001) | 0.693 (p < 0.0001) |
The Pearson’s correlation coefficients for the ratio of AFD/anterior offset were 0.56 (p < 0.0001) between MRI and ultrasound in neutral position and 0.69 (p < 0.0001) between MRI and ultrasound in 20° internal rotation (Table 1). The Pearson’s correlation coefficient was 0.76 (p < 0.0001) between the alpha angle on MRI and the ratio of AFD/anterior offset on ultrasound in 20° internal rotation.
The intraclass reliability ranged from 0.81 to 0.98. The interobserver reliability for the two more experienced surgeons (ten and five years) ranged from 0.86 to 0.95. The interclass correlation for all three observers ranged from 0.77 to 0.88.
Discussion
In recent years, femoro-acetabular impingement has been classified as an early cause of osteoarthritis of the hip joint [1–3]. The lack of concavity at the femoral head-neck junction in the case of a CAM-type impingement reduces femoral clearance during flexion [15], adduction and internal rotation movements, and can result in secondary derangements, such as labral tears and acetabular cartilage delamination [1, 4, 16]. The introduction of the alpha angle by Nötzli et al. [8] provided a means to measure the extent of the femoral head-neck deformity on MRI, and was used to develop treatment guidelines. Further studies published additional parameters for the analysis of MRI or plain radiography to quantify the extent of the CAM-type deformity [9, 13]. Others examined the three-dimensional nature of FAI, which led to a better understanding of the biomechanical complexity of the disease in these patients [17–20]. However, many of these findings are not well known amongst clinicians, and there are still many young adult patients with a long history of hip pain. The early diagnosis of CAM-type FAI at the onset of pain is of major importance in order to prevent secondary derangements that further complicate treatment in these patients [1, 16, 21]. Unlike X-rays and MRI, ultrasound is a readily available tool that could be used to disseminate knowledge of FAI.
We found strong correlations between parameters measured on MRI and ultrasound. The alpha angle showed the highest level of agreement between the two imaging modalities, particularly between the alpha angle measured on MRI and ultrasound in 20° internal rotation; these measurements had a Pearson’s correlation coefficient of 0.77. Similar or minor correlations between radiographs and three-dimensional imaging have been shown by others who evaluated the accuracy of the alpha angle on plain radiographs versus MRI or CT [22, 23]. However, radiographs taken in an AP or lateral view are the accepted views to initially screen for CAM-type FAI.
On an oblique axial MRI, the anterior region of the joint can be optimally assessed. We show that 20° of hip internal rotation provided the best overall agreement with MRI measurements. As compared with the other two positions, this internal rotation position allowed for the most similar evaluation of the region of the hip head-neck junction as to that observed with oblique axial imaging. However, on an oblique axial MRI, the more superior aspect of the femoral head-neck junction is visualised suboptimally, and bumps situated in this region can be underestimated. In contrast, we show that ultrasound in 20° internal rotation gives a better evaluation of the more superior region and to the anterior aspect, also because of the possibility to rotate the ultrasonic transducer. Our measurements of the AFD and anterior offset on ultrasound were always greater than those on MRI. Therefore, we found strong correlations for all parameters and no significant differences between both values in the hips of those patients with a strict anterior femoral bump (described intraoperatively). Rakhra et al. [24] also found greater values for the alpha angles on radial plane MR images at one and two o’clock than on oblique axial images. But the AFD/anterior offset ratio again showed a strong correlation between ultrasound and MRI. We also detected a strong correlation of this ratio on ultrasound in 20° internal rotation with the alpha angle on MRI. This is an interesting finding, since the AFD and anterior offset are very easy to measure on ultrasound. In contrast, measurement of the alpha angle on ultrasound with the necessity to construct a circle on the visible sector of the femoral head seems to be more difficult and error-prone, especially in internal rotation. However, we found no significant difference between all three head diameter values on ultrasound and the head diameter on MRI. Thus, construction of a circle on the visible sector of the femoral head on ultrasound is reproducible, irrespective of the hip joint position.
Ultrasound of the hip joint in 20° external rotation evaluated the more inferior aspects of the femoral head-neck junction. Therefore, we found no correlations between MRI and ultrasound measurements in this plane. In neutral position for ultrasound, we found fewer and poorer correlations with MRI as compared with those findings in 20° internal rotation. While it is possible to rotate the ultrasonic transducer, the antetorsion of the femur could be the reason that the region of the head-neck junction, with expected bumps, is not reliably visualised in the neutral position. Thus, we acknowledge limitation of the diagnostic utility of ultrasound for determining patients with CAM-type FAI. At least, the most superior aspect of the head-neck junction cannot be evaluated by ultrasound, because internal rotation of the hip joint and rotation of the ultrasonic transducer are limited.
The reliability of ultrasound thus depends on the observer’s experience in ultrasound examinations. As shown in other sonographic diagnostic fields, the successful use of the technique and the correct interpretation of the images require an experienced examiner. However, our intra-observer and interobserver reliability are comparable to those on plain radiographs [7, 25, 26].
In conclusion, CAM-type deformity can be detected with ultrasound by employing parameters from MRI or plain radiography. While the information gained from ultrasound is less than that attained by MRI, ultrasound still offers a readily available and inexpensive method that would be helpful in the early diagnosis of CAM-type FAI in daily practice.
Acknowledgments
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- 1.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 3.Tanzer M, Noiseux N (2004) Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res 429:170-7 [PubMed]
- 4.Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop. 2011;35:1427–1435. doi: 10.1007/s00264-011-1278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kusma M, Bachelier F, Schneider G, Dienst M. Femoroacetabular impingement. Clinical and radiological diagnostics. Orthopade. 2009;38:402–411. doi: 10.1007/s00132-008-1384-4. [DOI] [PubMed] [Google Scholar]
- 6.Mamisch TC, Werlen S, Zilkens C, et al. Radiological diagnosis of femoroacetabular impingement. Radiologe. 2009;49:425–433. doi: 10.1007/s00117-009-1833-z. [DOI] [PubMed] [Google Scholar]
- 7.Cavaignac E, Chiron P, Espie A, et al. Experimental study of an original radiographic view for diagnosis of cam-type anterior femoroacetabular impingement. Int Orthop. 2012;36:1783–1788. doi: 10.1007/s00264-012-1550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 9.Eijer H, Leunig M, Mahomed MN, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 10.Burstein D, Velyvis J, Scott KT, et al. Protocol issues for delayed Gd(DTPA)(2-)-enhanced MRI (dGEMRIC) for clinical evaluation of articular cartilage. Magn Reson Med. 2001;45:36–41. doi: 10.1002/1522-2594(200101)45:1<36::AID-MRM1006>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 11.Troelsen A, Jacobsen S, Bolvig L, et al. Ultrasound versus magnetic resonance arthrography in acetabular labral tear diagnostics: a prospective comparison in 20 dysplastic hips. Acta Radiol. 2007;48:1004–1010. doi: 10.1080/02841850701545839. [DOI] [PubMed] [Google Scholar]
- 12.Troelsen A, Mechlenburg I, Gelineck J, et al. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop. 2009;80:314–318. doi: 10.3109/17453670902988402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lohan DG, Seeger LL, Motamedi K, et al. Cam-type femoral-acetabular impingement: is the alpha angle the best MR arthrography has to offer? Skeletal Radiol. 2009;38:855–862. doi: 10.1007/s00256-009-0745-3. [DOI] [PubMed] [Google Scholar]
- 14.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 15.Casartelli NC, Leunig M, Item-Glatthorn JF, et al. Hip flexor muscle fatigue in patients with symptomatic femoroacetabular impingement. Int Orthop. 2012;36:967–973. doi: 10.1007/s00264-011-1385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 17.Dudda M, Albers C, Mamisch TC, et al. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res. 2009;467:651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ito K, Minka MA, Leunig M, et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 19.Meyer DC, Beck M, Ellis T, et al. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 20.Pfirrmann CW, Mengiardi B, Dora C, et al. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 21.Papalia R, Del BA, Franceschi F, et al. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012;36:903–914. doi: 10.1007/s00264-011-1443-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Domayer SE, Ziebarth K, Chan J, et al. Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol. 2011;80:805–810. doi: 10.1016/j.ejrad.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 23.Nepple JJ, Martel JM, Kim YJ, et al. Do plain radiographs correlate with CT for imaging of Cam-type femoroacetabular impingement? Clin Orthop Relat Res. 2012;470:3313–3320. doi: 10.1007/s11999-012-2510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rakhra KS, Sheikh AM, Allen D, Beaule PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:660–665. doi: 10.1007/s11999-008-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469:464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36:505–510. doi: 10.1007/s00264-011-1302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]