Abstract
Background
The inverse, dose-dependent association between cardiorespiratory fitness and mortality is well-established; however, the pattern of the association between low fitness and mortality across short- (0 to 10 years), intermediate- (10 to 20 years), and long-term (>20 years) follow-up has not been studied.
Methods and Results
We included 46 575 men and 16 151 women (mean age 44 years) from the Cooper Center Longitudinal Study. Participants were categorized as either “low fit” or “not low fit,” based on age- and sex- adjusted treadmill times, and were followed for mortality, determined from the National Death Index. Multivariable-adjusted Cox proportional hazards models were constructed to compare the association between fitness and traditional risk factors, with mortality outcomes across short-, intermediate-, and long-term follow-up. After a median follow-up of 16 years, there were 1295 cardiovascular disease and 2840 noncardiovascular disease deaths. Low fitness was associated with all-cause mortality across all periods in men [0 to 10 years: hazard ratios (HR), 1.99 (95% confidence interval [CI], 1.66 to 2.40); 10 to 20 years: HR, 1.61 (95% CI, 1.41 to 1.84); and >20 years: HR, 1.42 (95% CI, 1.27 to 1.60)] and in women [0 to 10 years: HR, 1.98 (95% CI, 1.27 to 3.10); 10 to 20 years: HR, 1.90 (95% CI, 1.40 to 2.56); and >20 years: HR, 1.54 (95% CI, 1.15 to 2.07)]. Similar results were seen for both cardiovascular disease and noncardiovascular disease mortality. Although these associations were also consistent across most subgroups, low fitness appeared to be most strongly associated with mortality in the short term among individuals at highest short-term risk (ie, older age, abnormal exercise test).
Conclusions
Similar to traditional risk factors, fitness is associated with mortality across short-, intermediate-, and long-term follow-up.
Keywords: fitness, epidemiology, risk factors, survival analysis
Traditional cardiovascular disease (CVD) risk factors are associated with mortality across short-term (ie, <10 years), intermediate-term (ie, 10 to 20 years), as well as long-term (>20 years) follow-up.1–4 Although most traditional risk factors (ie, blood pressure, etc) are associated with mortality across both short-term and long-term follow-up,5,6 risk factors that reflect the presence of existing disease (ie, major ECG abnormalities) appear to be strongest in the short term, with no association across longer periods of follow-up.1 Therefore, the association between a risk factor and CVD across short-, intermediate-, and long-term follow-up can provide insight into the nature of the association between the risk factor and mortality.
The inverse association between cardiorespiratory fitness (fitness) and both CVD and non-CVD mortality has been well-characterized.7–10 Low fitness is also associated with both preexisting disease and with the development of risk factors such as diabetes11–13 and hypertension12,14,15 in the future; however, the pattern of association between fitness and mortality across different periods of follow-up remains uncertain, and, to our knowledge, it has not been well-studied. Therefore, we sought to characterize the association between fitness and both CVD and non-CVD mortality across short- (0 to 10 years), intermediate- (10 to 20 years), and long-term (>20 years) follow-up in a healthy cohort of men and women in the Cooper Center Longitudinal Study (CCLS). We hypothesized that low fitness would be associated with both CVD and non-CVD mortality across short-, intermediate-, and long-term follow-up. We further hypothesized that low fitness would confer the greatest risk in the short term among individuals at the highest short-term risk.
Methods
For our primary analysis, we included 46 575 men and 16 151 women, who underwent clinical examination at the Cooper Clinic in Dallas, Tex., between 1971 and 2006, after excluding participants with a history of myocardial infarction (n=739) and abnormal exercise ECG (n=3585). Participants with an abnormal ECG response were excluded for all primary analyses, with the exception of 1 prespecified analysis among participants with and without an abnormal exercise ECG (see below for further details).
Individuals in the CCLS were either self-referred or were referred by their employer or personal physician. Details of the clinical examination and the study cohort have been published previously.16,17 Participants completed a comprehensive clinical examination, which included a self-reported personal and family history; standardized medical examination by a physician; fasting blood levels of total cholesterol, triglycerides, and glucose; as well as a maximal treadmill exercise test. Body mass index was calculated from measured height and weight. Participants signed an informed consent for the clinical examinations and inclusion in the research database, and the study was reviewed and approved annually by the institutional review board of The Cooper Institute, as well as The University of Texas Southwestern Medical Center.
Fitness was measured in the CCLS by a maximal treadmill exercise test, using the modified Balke protocol. In this protocol, treadmill speed is initially set at 88 m/min. In the first minute, the grade is set at 0%, followed by 2% in the second minute, and an increase of 1% for every minute thereafter. After 25 minutes, the grade remains unchanged, but the speed is increased 5.4 m/min for each additional minute until the test is terminated. Participants were encouraged not to hold onto the railing and were given encouragement to exert maximal effort. The test was terminated by volitional exhaustion reported by the participant or by the physician for medical reasons. As described previously, the test time using this protocol correlates highly with directly measured maximal oxygen uptake (r=0.92).18
Mortality Surveillance
Study participants were followed up for mortality from the date of the initial, complete clinical examination through 2006. Before 1979, follow-up was completed by direct mail, telephone, contact with employer, and matching of records with Social Security Administration files. After the development of the National Death Index in 1979, all-cause mortality and deaths due to CVD (as indicated by the International Classification of Diseases, Ninth Edition codes 390.0 to 458.9 or equivalent codes from the International Classification of Diseases, Eighth Edition or International Classification of Diseases, Tenth Edition) were included. Non-CVD mortality was defined as any death not meeting these criteria for CVD death. Additional details regarding follow-up of the CCLS cohort have been described previously in detail.16,17
Statistical Analyses
In accordance with standard approaches to the analysis of fitness data, treadmill times were compared with age- and sex-specific normative data on treadmill performance within the CCLS, allowing each individual’s treadmill time to be classified into an age- and sex-specific quintile of fitness. Individuals in quintile 1 were categorized as “low fit,” and individuals in quintiles 2 to 5 were categorized as “not low fit.” In addition to categorizing fitness in these categories, we examined the association between fitness and mortality with fitness as a continuous variable (ie, per metabolic equivalent). Using well-characterized regression equations, treadmill times from the Balke protocol allow for estimation of fitness level in metabolic equivalents.18
To determine the strength of the association between fitness and mortality across time, the follow-up period was divided into 3 separate, mutually exclusive time periods: 0 to 10 years, 10 to 20 years, and >20 years. For example, a participant surviving for 25 years provided 10 years of follow-up for the first follow-up interval (0 to 10 years), 10 years of follow-up for the second interval (10 to 20 years), and 5 years of follow-up for the third interval (>20 years).
Cox proportional hazards models were constructed for each follow-up period for all outcomes separately, including CVD mortality, non-CVD mortality, and total mortality. All models were multivariable and included baseline continuous measurements for age, systolic blood pressure, serum total cholesterol, body mass index, and triglycerides. In addition, all models included baseline categorical assessments of smoking (current smoking yes versus no), diabetes (yes versus no), and low fitness (low-fit versus not low-fit, see above for details). In secondary analyses, fitness was also assessed as a continuous variable, using treadmill times from the Balke protocol to estimate fitness level in metabolic equivalents.18
We also examined for effect modification by assessing the association between fitness and CVD, non-CVD, and total mortality across prespecified subgroups: diabetes (yes/no), current smoking (yes/no), hypertension (yes/no), body mass index (BMI) (above/below median), and age (above/below median). In all subgroup analyses, we combined men and women to conserve statistical power because of the overall similar pattern of results in men and women. All models were adjusted for continuous variables, including age, systolic blood pressure, total cholesterol, body mass index, triglycerides, as well as sex, for subgroups other than the categorical stratification variable. For instance, when we evaluated the association between fitness and mortality among participants with and without diabetes, we adjusted for all continuous covariates and sex and not for diabetes status. For models stratified by continuous variables, the continuous variable was still included in the subgroup model. We also examined the association between fitness and mortality across different periods of follow-up stratified by the presence or absence of an abnormal ECG response. For this particular secondary analysis, we examined the association between fitness and total mortality across different follow-up times among participants with (N=3579) and without an abnormal ECG response (N=62 726). Finally, to test for a birth cohort effect for fitness, we estimated the association between fitness and total mortality among men and women with a median birth year <1947 and median birth year ≥1947. In both of these secondary analyses, men and women were combined, and all models were multivariable-adjusted for age, sex, systolic blood pressure, total cholesterol, body mass index, triglycerides, smoking status, and diabetes.
To compare the relative strength of the association between each risk factor and mortality in the separate follow-up periods, standardized coefficients and standard errors for each risk factor were compared across the 3 follow-up intervals. Because the estimated coefficients from the 3 time intervals are independent under the Cox proportional hazards model, we examined for trends in the associations by testing the changes in the coefficients from the 3 time intervals using a χ2 test with 2 degrees of freedom. We interpreted a probability value of <0.05 to suggest that the strength of the association between the risk factor and CVD death was different across the follow-up periods. Aside from the analysis by median age, this technique was not applied to subgroup analyses, given the large variations in sample size among most subgroups. All statistical analyses were performed using SAS for Windows (release 9.2; SAS Institute, Inc).
Results
Baseline characteristics among the 46 575 men and 16 151 women in the study sample reveal expected sex differences in risk factor levels, with higher traditional risk factor burden in men compared with women (Table 1). After a median follow-up of 16 years, there were 1295 CVD deaths and 2840 non-CVD deaths. Because of the large study sample with long-term follow-up, there were a large number of person-years of follow-up across each decade, with higher mortality rates in the second and third decade (Table 2). Additionally, there were more non-CVD deaths for both men and women, and the number of CVD deaths in women across all decades of follow-up was smaller as compared with men.
Table 1.
Baseline Characteristics of Men and Women in the Cooper Center Longitudinal Study
| Overall N=62 726 | Men N=46 575 | Women N=16 151 | |
|---|---|---|---|
| Age, y | 43.98 (9.77) | 43.99 (9.53) | 43.98 (10.44) |
| Systolic blood pressure, mm Hg | 119.6 (14.21) | 121.9 (13.37) | 113.07 (14.52) |
| Diastolic blood pressure, mm Hg | 80.2 (9.91) | 81.62 (9.62) | 76.17 (9.62) |
| Hypertension | 18 035 (29%) | 15 118 (32%) | 2917 (18%) |
| Total cholesterol, mg/dL | 205.27 (39.64) | 207.55 (39.93) | 198.69 (38.03) |
| Body mass index, kg/m2 | 25.89 (4.31) | 26.74 (3.94) | 23.44 (4.41) |
| Triglycerides, mg/dL | 126.95 (102.27) | 138.37 (110.25) | 94.03 (64.09) |
| Smokers, N (%) | 9839 (16%) | 8274 (18%) | 1565 (10%) |
| Diabetes, N (%) | 2296 (4%) | 1950 (4%) | 346 (2%) |
| Glucose, mg/dL | 98.42 (16.42) | 100.15 (16.92) | 93.45 (13.73) |
| Low fitness, N (%) | 9935 (16%) | 7932 (17%) | 2003 (12%) |
Data are presented as mean (SD) or N (%).
Table 2.
Cardiovascular and Noncardiovascular Mortality Rates for 0 to 10 y, 10 to 20 y, and >20 y of Follow-Up Among Participants From the Cooper Center Longitudinal Study
| 0–10 y
|
10–20 y
|
> 20 y
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Events | Person-Years | Total N | Rate* | Events | Person-Years | Total N | Rate* | Events | Person-Years | Total N | Rate* | |
| Cardiovascular mortality | ||||||||||||
| Men | 188 | 389 827 | 46 575 | 0.48 | 423 | 257 443 | 31 171 | 1.64 | 556 | 124 640 | 19 414 | 4.46 |
| Women | 18 | 124 949 | 16 151 | 0.14 | 51 | 71 772 | 9019 | 0.71 | 59 | 28 895 | 5042 | 2.04 |
| 0–10 y
|
10–20 y
|
> 20 y
|
||||||||||
| Events | Person-Years | Total N | Rate* | Events | Person-Years | Total N | Rate* | Events | Person-Years | Total N | Rate* | |
| Noncardiovascular mortality | ||||||||||||
| Men | 460 | 389 827 | 46 575 | 1.18 | 878 | 257 443 | 31 171 | 3.41 | 1069 | 124 640 | 19 414 | 8.58 |
| Women | 101 | 124 949 | 16 151 | 0.81 | 175 | 71 772 | 9019 | 2.44 | 157 | 28 895 | 5042 | 5.43 |
per 1000 person-years.
The multivariable-adjusted hazard ratios for total mortality demonstrate expected differences in the strength and significance of the associations between traditional risk factors and total mortality across short-, intermediate-, and long-term follow-up (Table 3). Most risk factors tended to decrease in significance across later periods of follow-up, whereas other risk factors, such as body mass index, tended to increase in magnitude across later periods of follow-up. Similar to these latter risk factors, the association between fitness and total mortality also remained significant over all follow-up periods, with slightly lower hazard ratios in the final decades of follow-up. When fitness was examined as a continuous covariate, the pattern of results was similar in men [0 to 10 years: HR, 1.22 (95% CI, 1.17 to 1.27), 10 to 20 years: HR, 1.14 (95% CI, 1.10 to 1.17), and >20 years: HR, 1.09 (95% CI, 1.06 to 1.12)] and women [0 to 10 years: HR, 1.23 (95% CI, 1.10 to 1.38), 10 to 20 years: HR, 1.07 (95% CI, 0.99 to 1.16), and >20 years: HR, 1.24 (95% CI, 1.12 to 1.36)]. In general, these findings were similar in both men and women, with wider confidence intervals in women. Additionally, there was no difference in these findings when glucose levels, diastolic blood pressure, and hypertension status were added as additional covariates in the model (data not shown).
Table 3.
Multivariable-Adjusted* Hazard Ratios for Total Mortality Across 0 to 10 y, 10 to 20 y, and >20 y of Follow-Up Among Participants From the Cooper Center Longitudinal Study
| Variable | 0 to 10 y | 10 to 20 y | > 20 y | P* |
|---|---|---|---|---|
| Men | ||||
| Systolic blood pressure (per SD) | 1.22 (1.10 to 1.35) | 1.23 (1.14 to 1.32) | 1.19 (1.12 to 1.27) | 0.032 |
| Diabetes (yes vs no) | 1.76 (1.38 to 2.25) | 1.26 (1.04 to 1.52) | 1.14 (0.97 to 1.34) | 0.007 |
| Cholesterol (per SD) | 1.13 (1.04 to 1.22) | 0.92 (0.87 to 0.98) | 1.04 (0.99 to 1.10) | <0.0001 |
| Smoking (yes vs no) | 1.60 (1.33 to 1.91) | 1.72 (1.52 to 1.95) | 1.65 (1.47 to 1.84) | 0.488 |
| Triglycerides (per SD) | 0.99 (0.94 to 1.04) | 1.05 (1.03 to 1.08) | 1.04 (1.01 to 1.06) | 0.089 |
| BMI (per SD) | 0.97 (0.91 to 1.03) | 1.07 (1.02 to 1.12) | 1.10 (1.05 to 1.15) | <0.0001 |
| Continuous METs | 1.22 (1.17 to 1.27) | 1.14 (1.10 to 1.17) | 1.09 (1.06 to 1.12) | 0.0001 |
| Low fitness (vs not low fitness) | 1.99 (1.66 to 2.40) | 1.61 (1.41 to 1.84) | 1.42 (1.27 to 1.60) | <0.0001 |
| Women | ||||
| Systolic blood pressure (per SD) | 1.25 (0.99 to 1.58) | 1.27 (1.08 to 1.51) | 1.09 (0.91 to 1.29) | 0.825 |
| Diabetes (yes vs no) | 1.09 (0.40 to 3.02) | 2.16 (1.30 to 3.60) | 1.69 (0.95 to 2.98) | 0.208 |
| Cholesterol (per SD) | 0.97 (0.80 to 1.19) | 0.89 (0.77 to 1.03) | 1.00 (0.87 to 1.16) | 0.878 |
| Smoking (yes vs no) | 1.59 (0.93 to 2.74) | 1.96 (1.38 to 2.78) | 2.44 (1.78 to 3.35) | 0.413 |
| Triglycerides (per SD) | 0.87 (0.67 to 1.14) | 1.03 (0.89 to 1.19) | 1.11 (1.01 to 1.21) | 0.247 |
| BMI (per SD) | 0.98 (0.86 to 1.13) | 1.06 (0.95 to 1.17) | 1.11 (1.00 to 1.24) | 0.130 |
| Continuous METs | 1.23 (1.10 to 1.38) | 1.07 (0.99 to 1.16) | 1.24 (1.12 to 1.36) | 0.038 |
| Low fitness (vs not low fitness) | 1.98 (1.27 to 3.10) | 1.90 (1.40 to 2.56) | 1.54 (1.15 to 2.07) | 0.310 |
BMI indicates body mass index; METs, metabolic equivalents.
“Low fitness” is defined as individuals who, when compared with age- and sex-specific normative data on treadmill performance, were in the lowest quintile of treadmill time.
All models were performed in men and women separately and multivariable-adjusted for age, systolic blood pressure, serum total cholesterol, body mass index, and triglycerides, as well as categorical variables, including smoking (yes/no) and diabetes (yes/no).
P<0.05 suggests that the strength of the association between fitness and the risk factor was different across the follow-up periods.
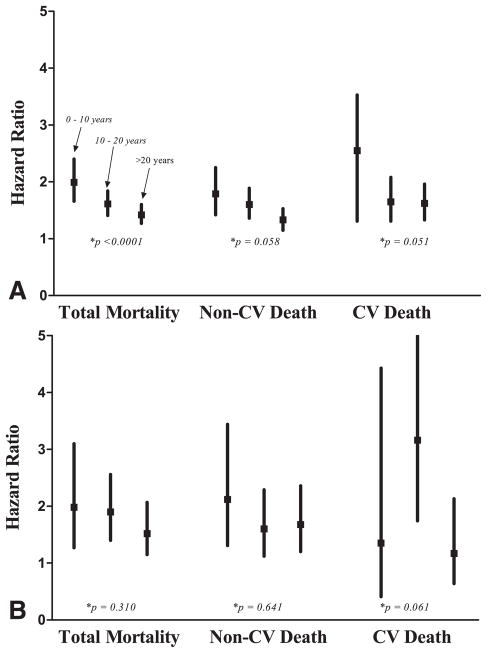
Figure 1 demonstrates the temporal stability of the association between fitness and CVD, non-CVD, and total mortality across short- (0 to 10 years), intermediate- (10 to 20 years), and long-term (>20 years) follow-up. When we analyzed fitness as a continuous variable, we observed a similar pattern of results (data not shown). Overall, the patterns of these associations were consistent across most subgroups for both CVD and non-CVD mortality (Table 4); however, among participants with diabetes, the association between low fitness and non-CVD mortality was strongest in the first 10 years and attenuated across later follow-up periods and was no longer significant at >20 years of follow-up [HR, 1.1 (95% CI, 0.7 to 1.7)]. In our analysis, stratified by median birth year, there was no difference in the association between fitness and all-cause mortality over the entire follow-up period (P=0.86), suggesting the absence of a birth cohort effect in our findings.
Figure 1.
A, Multivariable-adjusted hazard ratios (95% confidence intervals [CI]) for low fitness and Total Mortality, Non-CVD Death, and CVD Death for 0 to 10 years, 10 to 20 years, and >20 years of follow-up in men. B, Multivariable-adjusted hazard ratios (95% CI) for low fitness and Total Mortality, Non-CVD Death, and CVD Death for 0 to 10 years, 10 to 20 years, and >20 years of follow-up in women. Both models were adjusted for baseline continuous variables, including age, systolic blood pressure, serum total cholesterol, body mass index, and triglycerides as well as categorical variables, including smoking (yes/no) and diabetes (yes/no). P<0.05 suggests that the strength of the association between fitness and the outcome was different across the follow-up periods.
Table 4.
Multivariable Adjusted* Hazard Ratios Low Cardiorespiratory Fitness and CVD and Non-CVD Mortality Across Short-, Intermediate-, and Long-Term Follow-Up Among Selected Subgroups
| Hypertensive N=18 035
|
Nonhypertensive N=44 691
|
High BMI† N=31 201
|
Low BMI† N=31 525
|
|||||
|---|---|---|---|---|---|---|---|---|
| CVD (n=674) | Non-CVD (n=1074) | CVD (n=621) | Non-CVD (n=1766) | CVD (n=803) | Non-CVD (n=1433) | CVD (n=492) | Non-CVD (n=1407) | |
| 0 to 10 y | 2.1 (1.4 to 3.2) | 2.1 (1.6 to 2.9) | 2.9 (1.8 to 4.8) | 1.6 (1.2 to 2.1) | 2.6 (1.7 to 3.8) | 1.8 (1.3 to 2.3) | 2.2 (1.3 to 3.7) | 2 (1.4 to 2.7) |
| 10 to 20 y | 1.7 (1.3 to 2.3) | 1.7 (1.3 to 2.1) | 1.8 (1.3 to 2.5) | 1.5 (1.3 to 1.9) | 1.4 (1.1 to 1.9) | 1.6 (1.3 to 2.0) | 2.5 (1.8 to 3.6) | 1.6 (1.3 to 2.0) |
| > 20 y | 1.5 (1.2 to 2.0) | 1.2 (0.9 to 1.5) | 1.5 (1.2 to 2.0) | 1.5 (1.2 to 1.7) | 1.5 (1.2 to 2.0) | 1.1 (0.9 to 1.4) | 1.6 (1.2 to 2.1) | 1.6 (1.3 to 1.9) |
| Smoker N =9839
|
Non-Smoker N=52 887
|
Diabetic N=2296
|
Non-Diabetic N=60 430
|
|||||
| CVD (n=340) | Non-CVD (n=760) | CVD (n=955) | Non-CVD (n=2080) | CVD (n=179) | Non-CVD (n=240) | CVD (n=1116) | Non-CVD (n=2600) | |
| 0 to 10 y | 2.3 (1.3 to 4.0) | 1.8 (1.2 to 2.6) | 2.5 (1.7 to 3.6) | 1.9 (1.5 to 2.4) | 1.6 (0.7 to 3.4) | 3.5 (2.0 to 6.4) | 2.6 (1.9 to 3.7) | 1.7 (1.4 to 2.1) |
| 10 to 20 y | 1.4 (0.9 to 2.0) | 1.8 (1.4 to 2.2) | 2 (1.6 to 2.6) | 1.5 (1.3 to 1.8) | 1.9 (1.1 to 3.3) | 2.5 (1.5 to 4.3) | 1.8 (1.4 to 2.2) | 1.6 (1.3 to 1.8) |
| > 20 y | 1.3 (0.9 to 1.9) | 1.6 (1.3 to 2.1) | 1.7 (1.3 to 2.1) | 1.3 (1.1 to 1.5) | 1.9 (1.1 to 3.2) | 1.1 (0.7 to 1.7) | 1.5 (1.2 to 1.8) | 1.4 (1.2 to 1.6) |
BMI indicates body mass index; CVD, cardiovascular disease.
In all subgroup analyses, men and women were combined, and models were adjusted for age, systolic blood pressure, serum total cholesterol, body mass index, triglycerides, and sex. See methods for details.
“High BMI” and “low BMI” are defined as above and below the sample median (25.8 kg/m2), respectively; “hypertensive” is defined as a systolic blood pressure ≥140, diastolic blood pressure ≥90, or from self-report of diagnosed hypertension.
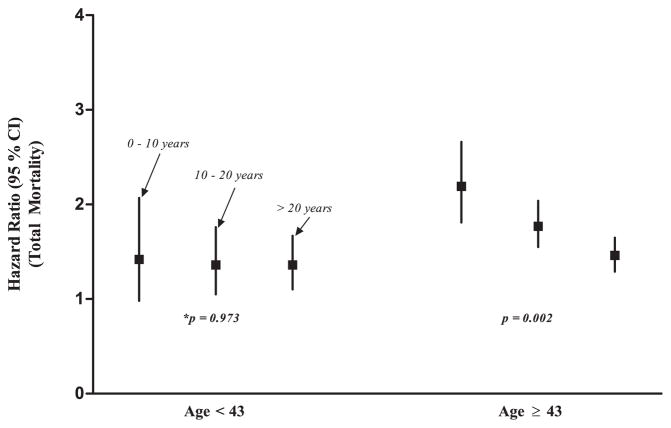
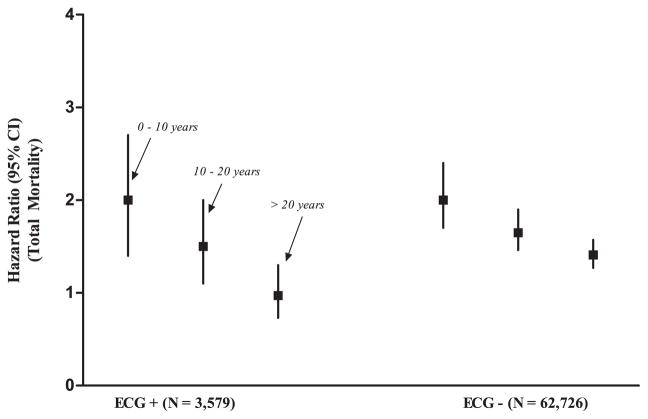
Among individuals above the median age (43 years), the association between fitness and total mortality diminished but remained significant across short-, intermediate-, and long-term follow-up (P=0.002). In contrast, in younger individuals, the association between low fitness and total mortality remained unchanged (P=0.97) (Figure 2). Finally, among individuals with an abnormal ECG response (N=3579), there were 601 all-cause deaths over all 3 follow-up periods. In this group, the association between fitness and total mortality was strongest in the short term but attenuated across longer periods of follow-up and was no longer significant at >20 years (Figure 3).
Figure 2.
Multivariable-adjusted hazard ratios for low fitness and total mortality across 0 to 10 years, 10 to 20 years, and >20 years of follow-up, stratified by age <43 or ≥43. Men and women were combined, and models were adjusted for sex, as well as age, systolic blood pressure, serum total cholesterol, body mass index, triglycerides, current smoking (yes/no), and diabetes (yes/no). P<0.05 suggests that the strength of the association between fitness and total mortality was different across the follow-up periods.
Figure 3.
Multivariable-adjusted hazard ratios for low fitness and total mortality across 0 to 10 years, 10 to 20 years, and >20 years of follow-up, stratified by exercise ECG response (positive versus negative). Men and women were combined, and models were adjusted for sex, as well as age, systolic blood pressure, serum total cholesterol, body mass index, triglycerides, current smoking (yes/no), and diabetes (yes/no).
Discussion
In the present study, we observed several important findings. First, the association between a single, baseline measure of low fitness and all-cause mortality persisted across 0 to 10, 10 to 20, and >20 years of follow-up in a large cohort of healthy men and women. We observed an overall similar pattern of results in both men and women for both CVD and non-CVD mortality, with wider confidence intervals in women, reflecting the smaller number of CVD deaths in women. Second, similar to other traditional risk factors, the relative strength of the association between low fitness and total, CVD, and non-CVD mortality attenuated somewhat across 0 to 10, 10 to 20, and >20 years of follow-up, with stronger associations between fitness and mortality in short-term as compared with long-term follow-up periods. Although these associations were consistent across most subgroups, low fitness appeared to be most strongly associated with mortality in the short term among individuals at highest short-term risk (ie, older age, abnormal exercise test).
Numerous studies, including the Harvard Alumni Health Study,19,20 British Regional Heart Study,4 and a Copenhagen study,21 among others,22 have demonstrated an inverse association between physical activity and mortality. A similar association has been demonstrated between physical fitness and mortality.17,23,24 Additionally, metabolic equivalent levels and heart rate recovery have been shown to be predictive of CVD mortality across a period of >20 years of follow-up in patients studied in the Lipid Research Clinics Prevalence Study.25,26 Recently, we observed that a single measurement of fitness was associated with the lifetime risk for CVD mortality, even after adjustment for competing risks from non-CVD mortality27; however, this approach does not allow for the direct assessment of the temporal stability of the association between fitness and both non-CVD and CVD mortality across unique periods of follow-up.
Prior studies have examined the association between risk factors and mortality across different periods of follow-up, demonstrating 3 different patterns in the strength of the associations for different risk factors and mortality across short-, intermediate-, and long-term follow-up.5,6 First, most traditional risk factors (such as total cholesterol, systolic blood pressure, and diabetes) appear to attenuate across longer periods of follow-up, reflecting subsequent changes in risk factor levels across time (ie, treatment effects).1,2 Second, other risk factors, such as obesity, confer the greatest risk in the long term because of their contribution to the development of additional traditional risk factors in the future.28 Third, risk factors that reflect the presence of preexisting disease (ie, major ECG abnormalities) are strongest in the short term and do not appear to confer an increased risk across later follow-up periods.1
In the present study, we observed that the association between low fitness and mortality was similar to most traditional risk factors and was strongest in the short term, with some slight attenuation across longer periods of follow-up. The association between a risk factor and mortality diminishes across time for several different reasons, including changes in the risk factor over time, downstream treatment effects, and competing risks.1 It is likely that the attenuation of fitness across time reflects 1 or more of these mechanisms. For example, low fitness in midlife is associated with an increased risk of diabetes11–13 and hypertension12,14,15 in the future; however, downstream treatment of these risk factors across longer periods of follow-up would lessen the overall effect of fitness on mortality. Although low fitness in early and midlife is strongly associated with the development of future CVD risk factors such as diabetes11–13 and hypertension,12,14,15 we did not observe an increase in mortality risk across time for fitness as we did for BMI (Table 3); however, among younger adults at lowest risk in the short term, we observed a consistent association between low fitness and mortality across all follow-up intervals, suggesting the potential contribution of low fitness in midlife to the development of traditional risk factors in later life (Figure 2).
In contrast, we observed a different pattern of results among individuals with an abnormal exercise ECG response, with a very strong association in the short term but no association in the long term, suggesting that low fitness in this subgroup reflects the presence of preexisting disease (Figure 3). Thus, the mechanisms through which low fitness confers an increased risk on mortality are likely not uniform across all participants. In higher-risk individuals, low fitness reflects, at least in part, the presence of preexisting disease. In contrast, among lower-risk individuals earlier in life, low fitness behaves more like a traditional risk factor.
This study has several important limitations. First, given that patients in the CCLS cohort tend to be well-educated, of high socioeconomic status, and have a lower traditional risk factor burden, caution must be taken in generalizing these results to the general population. Despite these differences, the fitness levels and influence of traditional risk factors in the CCLS are similar to those in the general population.29 Second, it has been shown that there can be misclassification of non-CVD deaths as CVD death among older individuals using death certificates to determine cause of death.30 Thus, the influence of fitness on CVD mortality may be underestimated in this analysis, particularly, across later follow-up periods among older adults. Finally, we examined the association between 1 measurement of fitness and mortality across long-term follow-up, and, therefore, the attenuation in the association between fitness and mortality could also reflect downstream changes in fitness levels.
In summary, we observed that low fitness was associated with all cause, CVD, and non-CVD mortality across short-term (0 to 10 years), intermediate-term (10 to 20 years), and long-term (>20 years) follow-up. Similar to other traditional risk factors, the strength of the association between low fitness and mortality was strongest in the short term, with some attenuation across long-term follow-up.
WHAT IS KNOWN
Cardiorespiratory fitness, like traditional cardiovascular risk factors, is associated with mortality over short-term and long-term follow-up.
Low fitness is associated with preexisting disease and the development of future risk factors, including diabetes and hypertension.
WHAT THE STUDY ADDS
A single baseline measure of low fitness is associated with both CVD and non-CVD mortality across 3 decades of follow-up.
The pattern of the association between low fitness and mortality across time differs among high- and low-risk individuals.
Among higher-risk individuals, the association between low fitness and mortality appeared to be stronger in the short term, likely reflecting the presence of preexisting disease.
Among lower-risk individuals, low fitness appears more similar to a traditional risk factor, with a more consistent association with mortality across each follow-up period.
Acknowledgments
Sources of Funding
Dr Berry receives funding from (1) the Dedman Family Scholar in Clinical Care endowment at The University of Texas Southwestern Medical Center, (2) grant K23 HL092229 from the National Heart, Lung, and Blood Institute, and (3) grant 10BG1A4280091 from the American Heart Association. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication. All authors have read and agree to the manuscript as written.
Footnotes
Disclosures
Dr Berry has received honoraria from Merck/Schering. All other authors report no conflicts of interest.
This article was handled independently by Guest Editor, Jonathan Myers, PhD and Senior Guest Editor Paul A. Heidenreich, MD.
References
- 1.Berry JD, Dyer A, Carnethon MR, Tian L, Greenland P, Lloyd-Jones DM. Association of traditional risk factors with cardiovascular death across 0 to 10, 10 to 20, and >20 years follow-up in men and women. Am J Cardiol. 2008;101:89–94. doi: 10.1016/j.amjcard.2007.07.079. [DOI] [PubMed] [Google Scholar]
- 2.Pekkanen JTM, Nissinen A, Karvonen MJ. Does the predictive value of baseline coronary risk factors change over a 30-year follow-up? Cardiology. 1993;82:181–190. doi: 10.1159/000175867. [DOI] [PubMed] [Google Scholar]
- 3.Menotti A, Lanti M. Coronary risk factors predicting early and late coronary deaths. Heart. 2003;89:19–24. doi: 10.1136/heart.89.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wannamethee SG, Shaper AG, Whincup PH, Walker M. Role of risk factors for major coronary heart disease events with increasing length of follow up. Heart. 1999;81:374–379. doi: 10.1136/hrt.81.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilhelmsen L, Lappas G, Rosengren A. Risk of coronary events by baseline factors during 28 years follow-up and three periods in a random population sample of men. J Intern Med. 2004;256:298–307. doi: 10.1111/j.1365-2796.2004.01372.x. [DOI] [PubMed] [Google Scholar]
- 6.Menotti A, Lanti M, Kromhout D, Kafatos A, Nedeljkovic S, Nissinen A. Short and long term association of a single serum cholesterol measurement in middle-aged men in prediction of fatal coronary and other cardiovascular events: A cross-cultural comparison through Europe. Eur J Epidemiol. 2005;20:597–604. doi: 10.1007/s10654-005-7918-8. [DOI] [PubMed] [Google Scholar]
- 7.Blair SN, Kampert JB, Kohl HW, III, Barlow CE, Macera CA, Paffenbarger RS, Jr, Gibbons LW. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276:205–210. [PubMed] [Google Scholar]
- 8.Farrel SW, Kampert JB, Kohl HW, III, Barlow CE, Macera CA, Paffenbarger RS, Jr, Gibbons LW, Blair SN. Influences of cardiorespiratory fitness levels and other predictors on cardiovascular disease mortality in men. Med Sci Sports Exerc. 1998;30:899–905. doi: 10.1097/00005768-199806000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Laukkanen JA, Lakka TA, Rauramaa R, Kuhanen R, Venalainen JM, Salonen R, Salonen JT. Cardiovascular fitness as a predictor of mortality in men. Arch Intern Med. 2001;161:825–831. doi: 10.1001/archinte.161.6.825. [DOI] [PubMed] [Google Scholar]
- 10.Kokkinos P, Myers J. Exercise and physical activity. Circulation. 2010;122:1637–1648. doi: 10.1161/CIRCULATIONAHA.110.948349. [DOI] [PubMed] [Google Scholar]
- 11.Wei M, Gibbons LW, Mitchell TL, Kampert JB, Lee CD, Blair SN. The association between cardiorespiratory fitness and impaired fasting glucose and type 2 diabetes mellitus in men. Ann Intern Med. 1999;130:89–96. doi: 10.7326/0003-4819-130-2-199901190-00002. [DOI] [PubMed] [Google Scholar]
- 12.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 13.Carnethon MR, Sternfeld B, Schreiner PJ, et al. Association of 20-year changes in cardiorespiratory fitness with incident type 2 diabetes. Diabetes Care. 2009;32:1284–1288. doi: 10.2337/dc08-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA. 1984;252:487–490. [PubMed] [Google Scholar]
- 15.Carnethon MR, Evans NS, Church TS, Lewis CE, Schreiner PJ, Jacobs DR, Jr, Sternfeld B, Sidney S. Joint associations of physical activity and aerobic fitness on the development of incident hypertension. Hypertension. 2010;56:49–55. doi: 10.1161/HYPERTENSIONAHA.109.147603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273:1093–1098. [PubMed] [Google Scholar]
- 17.Blair SN, Kohl HW, III, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 18.Pollock ML, Bohannon RL, Cooper KH, Ayres JJ, Ward A, White SR, Linnerud AC. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92:39–46. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 19.Lee IM, Paffenbarger RS., Jr Associations of light, moderate, and vigorous intensity physical activity with longevity. Am J Epidemiol. 2000;151:293–299. doi: 10.1093/oxfordjournals.aje.a010205. [DOI] [PubMed] [Google Scholar]
- 20.Paffenbarger RS, Hyde R, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 21.Andersen LB, Schnohr P, Schroll M, Hein HO. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch Intern Med. 2000;160:1621–1628. doi: 10.1001/archinte.160.11.1621. [DOI] [PubMed] [Google Scholar]
- 22.Kokkinos P, Sheriff H, Kheirbek R. Physical inactivity and mortality risk. Cardiol Res Pract. 2011:1–10. doi: 10.4061/2011/924945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328:533–537. doi: 10.1056/NEJM199302253280803. [DOI] [PubMed] [Google Scholar]
- 24.Kokkinos P, Myers J, Faselis C, Panagiotakos DB, Doumas M, Pittaras A, Manolis A, Kokkinos JP, Karasik P, Greenberg M, Papademetriou V, Fletcher R. Exercise capacity and mortality in older men. Circulation. 2010;122:790–797. doi: 10.1161/CIRCULATIONAHA.110.938852. [DOI] [PubMed] [Google Scholar]
- 25.Mora S, Redberg RF, Sharrett AR, Blumenthal RS. Enhanced risk assessment in asymptomatic individuals with exercise testing and Framingham risk scores. Circulation. 2005;112:1566–1572. doi: 10.1161/CIRCULATIONAHA.105.542993. [DOI] [PubMed] [Google Scholar]
- 26.Mora S, Redberg RF, Cui Y, Whiteman MK, Flaws JA, Sharrett AR, Blumenthal RS. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women. JAMA. 2003;290:1600–1607. doi: 10.1001/jama.290.12.1600. [DOI] [PubMed] [Google Scholar]
- 27.Berry J, Willis B, Gupta S, Barlow CE, Lakoski SG, Khera A, Rohatgi A, de Lemos JA, Haskell W, Lloyd-Jones DM. Lifetime risk for cardiovascular disease mortality by cardiorespiratory fitness levels measured at age 45-, 55-, and 65-years in men: the Cooper Center Longitudinal Study. J Am Coll Cardiol. 2011;57:1604–1610. doi: 10.1016/j.jacc.2010.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dyer AR, Stamler J, Garside DB, Greenland P. Long-term consequences of body mass index for cardiovascular mortality: the Chicago heart association detection project in industry study. Ann Epidemiol. 2004;14:101–108. doi: 10.1016/S1047-2797(03)00121-2. [DOI] [PubMed] [Google Scholar]
- 29.Wang CY, Haskell WL, Farrell SW, Lamonte MJ, Blair SN, Curlin LR, Hughes JP, Burt VL. Cardiorespiratory fitness levels among US adults 20–49 years of age: findings from the 1999–2004 National Health and Nutrition Examination Survey. Am J Epidemiol. 2010;171:426–435. doi: 10.1093/aje/kwp412. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd-Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–1026. doi: 10.7326/0003-4819-129-12-199812150-00005. [DOI] [PubMed] [Google Scholar]