Abstract
Objectives. To characterize the use of high-fidelity mannequins and standardized patients in US pharmacy colleges and schools.
Methods. A survey instrument was sent to 105 doctor of pharmacy (PharmD) programs to collect data on the use of simulation and to identify barriers to using simulation-based teaching methods.
Results. Eighty-eight colleges and schools completed the survey instrument (response rate 84%). Of these, 14 did not use high-fidelity mannequins or standardized patients within the curriculum. Top barriers were logistical constraints and high resource cost. Twenty-three colleges and schools used simulation for introductory pharmacy practice experiences (IPPEs), 34 for interprofessional education, and 68 for evaluation of at least 1 core competency prior to advanced pharmacy practice experiences (APPEs).
Conclusions. Although the majority of US colleges and schools of pharmacy use simulation-based teaching methodologies to some extent in the pharmacy curricula, the role of simulation in IPPEs, interprofessional education, and assessment of competency-based skills could be expanded.
Keywords: simulation, high-fidelity mannequins, standardized patients, survey research
INTRODUCTION
According to Gaba, “Simulation is a technique…to replace or amplify real experiences with guided experiences that evoke or replicate substantial aspects of the real world in a fully interactive manner.”1 In the pharmacy literature, simulation-based teaching methodologies have been used to teach technical, communication, interprofessional, and clinical skills.2-31 In nursing and medical education, simulation-based teaching methodologies are routinely used within the curricula. A survey by the Association of American Medical Colleges found that more than 80% of medical schools had incorporated simulation-based instruction within all 4 years of the curriculum.32 Most medical schools have a simulation center that includes high-fidelity mannequins. Among nursing schools, 87% have incorporated simulation-based training with high- or medium-fidelity mannequins within the curriculum.33 A majority have incorporated simulation into 5 or more courses.
The extent of the use of simulation-based teaching methodologies use by pharmacy colleges and schools is not fully known; however, a search on Academic Search Complete with the criteria “simulation AND pharmacy” revealed a number of studies highlighting the use of simulation in pharmacy education.2-31 The majority of evidence regarding simulation-based instruction is with the use of high-fidelity mannequins.2-15 Fifteen studies showed an increase in the areas of student knowledge, self-perceived clinical skills, improved attitudes regarding death, patient safety awareness, and interprofessional teamwork skills, and improved clinical technical skills such as blood pressure assessment, emergency management, and/or management of pediatric patients. One of the most cited of these papers is by Seybert and colleagues who used simulation to teach performance-based pharmacotherapeutics.7 Vyas described an introductory pharmacy practice experience (IPPE) in which 3 acute care simulations using high-fidelity mannequins were conducted to reinforce pharmacotherapy concepts.4 The study showed increased knowledge retention among students in the study group compared to students in the control group. Six studies were found in the literature describing the use of standardized patients to teach physical assessment skills, anticoagulant management, interprofessional teamwork skills, communication skills, and patient safety concepts.16-21 To determine the use of simulation in interprofessional education, a search with the search criteria “interprofessional AND pharmacy” was conducted on Academic Search Complete and a small number of studies was found.6,9,14-17,21 Shrader and colleagues showed improvements in interprofessional teamwork and communication skills, while Marken used simulation to teach students how to engage patients in difficult conversations.6,15 Vyas incorporated a 4-week interprofessional course using simulation to teach patient safety concepts and teamwork skills in the IPPE curriculum that resulted in improvements in students’ knowledge, skills, and attitudes pre- and post-simulation.14
Despite the growing body of evidence regarding the outcomes of teaching with simulation, the full extent to which pharmacy school education has incorporated simulation-based teaching methodologies into the curricula is not yet known. Among those colleges and schools that have not yet incorporated simulation into their curriculum, barriers need to be identified which preclude the routine use of simulation. Additionally, understanding how simulation is used within IPPE and its’ role in teaching and assessing Accreditation Council for Pharmacy Education (ACPE) pre-APPE core domains will provide educators with valuable information.34
The purpose of this study was to assess the current status of simulation-based teaching methodologies using high-fidelity mannequins and standardized patients in US pharmacy colleges and schools. In this paper, the term simulation refers to the use of high-fidelity mannequins and standardized patients.
METHODS
Pharmacy practice faculty members with expertise in teaching with simulation wrote and revised an initial pool of survey items based on their experiences and the simulation literature. The survey instrument was pretested with 2 pharmacy practice department chairs, both of whom completed the survey online. They provided feedback about the clarity of the questions and also reported the time (in minutes) it took them to complete the survey instrument. Based on the feedback received, survey items were revised. The final survey instrument included 18 items and an introductory paragraph explaining the project and the consent process.
The survey instrument was divided into 3 sections. Section 1 contained questions regarding school demographics and access to simulation resources and all respondents were asked to complete it. Section 2 contained survey items regarding barriers to implementation of simulation, so only those colleges and schools that did not use high-fidelity mannequins or standardized patients in the curriculum were asked to complete the items. An additional item in section 2 inquired about alternative simulation modalities used within the curriculum. Section 3 of the survey instrument contained items about incorporation of simulation into the curriculum, use of simulation for formative or summative assessment, for IPPE, and if the program used simulation to teach or assess pre-APPE core domains as outlined by ACPE. All colleges and schools that used high-fidelity mannequins and/or standardized patients were asked to complete this section. The final item asked for the number of faculty members involved in simulation-based education.
The respondent pool for the survey instrument was identified through the American Association of Colleges of Pharmacy (AACP) faculty database. Inclusion criteria were individuals listed as department chairs of the pharmacy practice department and/or individuals responsible for curriculum at 105 accredited US colleges and schools of pharmacy.
The survey instrument and study methods were declared exempt from review by the Washington State University Institutional Review Board. The finalized survey items were loaded into SurveyMonkey (SurveyMonkey, Palo Alto, CA, www.surveymonkey.com), a proprietary electronic survey administration tool. The study was conducted February 27, 2012, through April 30, 2012. An initial e-mail with a brief study description and the survey link was sent to the chairs of the pharmacy practice department at each of the 105 colleges and schools of pharmacy in the United States. IRB exemption and the process for giving consent were explained to potential respondents in the introduction to the survey instrument. Respondents implied their consent by participating in the survey instrument.
To improve the response rate, 2 additional e-mails were sent to the chairs at those colleges and schools that had not responded to the survey instrument. For those not responding after 3 requests, an e-mail was sent out to the person whose special area of responsibility was identified as curriculum by the AACP faculty roster. Data were collated in Microsoft Excel and analyzed using descriptive statistics.
RESULTS
In response to the 105 invitations sent out, 108 survey instruments were submitted. Twenty of the submitted survey instruments were duplicate/subsequent attempts by a program to submit a response. Twelve of these were incomplete and eliminated from the study. Another 4 of the 20 were found to be identical to the original response from the same program so they also were eliminated from the study. The remaining 4 survey instruments represented a unique second response from a college or school from which a valid response had already been received, so the responses were combined and included as 1 survey instrument in the assessment.
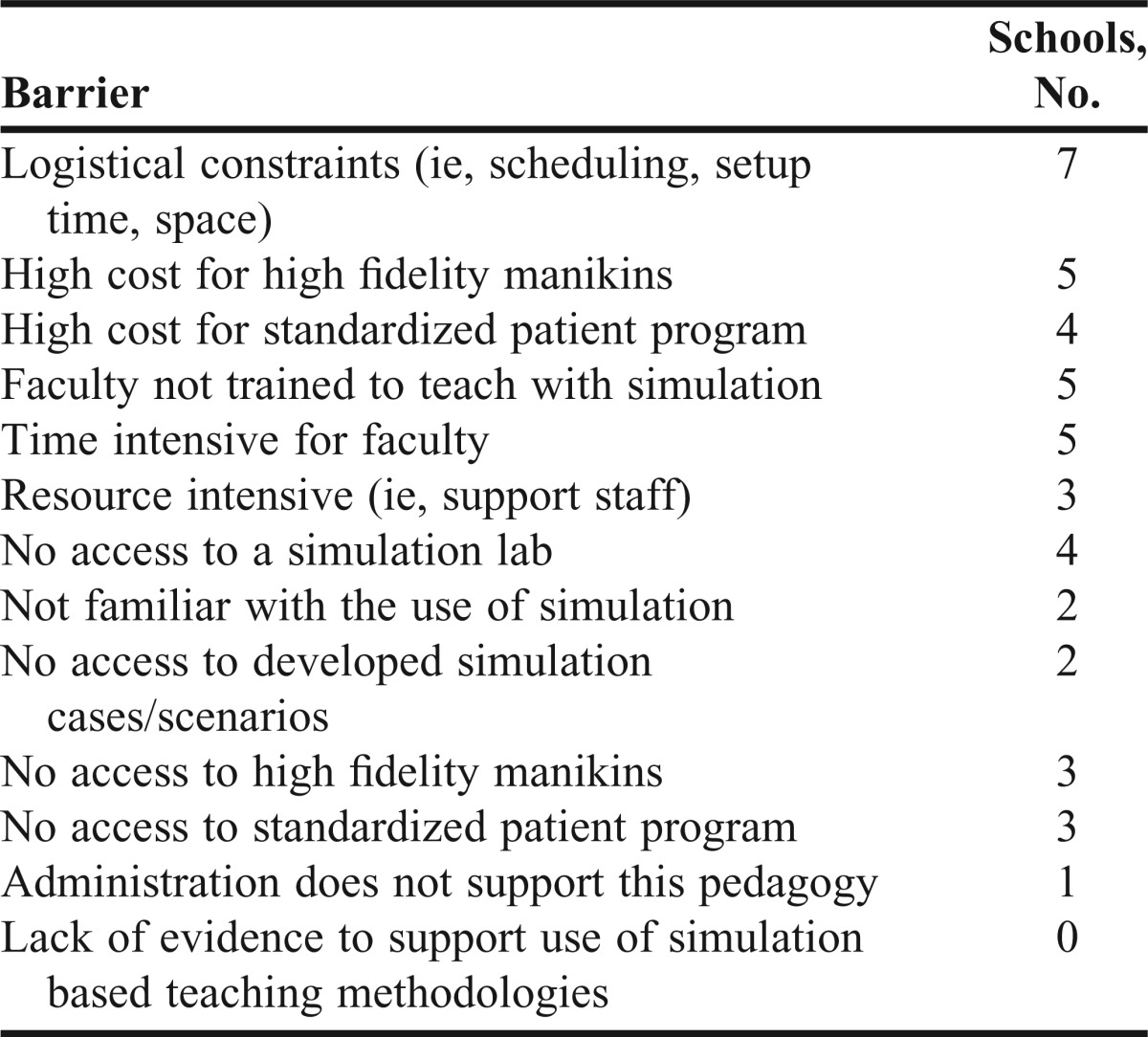
This resulted in 88 distinct completed survey instruments (response rate 84%). Of the 88 usable responses, 10 were from private standalone programs, 29 were from private university systems, and 49 were from public universities. Thirty respondents indicated that their college or school owned high-fidelity mannequins, 47 had access to a formal simulation center, and 50 had access to a formal standardized patient program. Fourteen of the 88 respondents (15.9%) stated that they did not use high-fidelity mannequins or standardized patients within the curriculum. Ten of the 14 (71.4%) had a class size greater than or equal to 100 students. Five colleges and schools that had access to a simulation center, and 3 others that had access to a formal standardized patient program did not currently use those services. The most frequently reported barriers to the use of simulation were high cost of the high-fidelity mannequin (42.5%) and logistical constraints (50%). The barriers cited to the use of simulation are summarized in Table 1. No respondents (0%) perceived a lack of evidence to support the use of simulation, and only 1 indicated their administration did not support simulation pedagogy. Of the colleges and schools not using simulation, 12 of 14 used peer-to-peer role playing, 7 used partial task trainers, and 6 schools used low-fidelity mannequins to educate their students.
Table 1.
Barriers to Incorporating High Fidelity Mannequins and Standardized Patients Into the Curriculum (N=14)
Of the 74 colleges and schools that used simulation, 17 used only high-fidelity mannequins, 27 used only standardized patients, and only 30 used both modalities within their program. Forty-two (56.8%) of the 74 colleges and schools had a class size greater than or equal to100 students. Fourteen schools had 1 to 2 faculty members, 33 had 3 to 5, and 27 had greater than 5 faculty members involved in simulation-based education. Twenty-eight colleges and schools used simulation in both required and elective courses, while 5 colleges and schools used simulation in elective courses only. The most frequent use of simulation within the PharmD curriculum was within patient care laboratory courses (55%) and patient/physical assessment (41%) courses. Less frequently simulation was incorporated into communication courses (24%), self-care courses (14%), and therapeutics courses (26%). Fifty percent of schools reported using simulation in 1 to 2 courses, while 43% reported using simulation in 3 or more courses. Of the 22 colleges and schools (29.7%) that used simulation for IPPEs, only 3 used it for the fully allowable 60 hours. Almost half of the 74 colleges and schools that used simulation (34 [45.9%]) reported using it to provide interprofessional education.
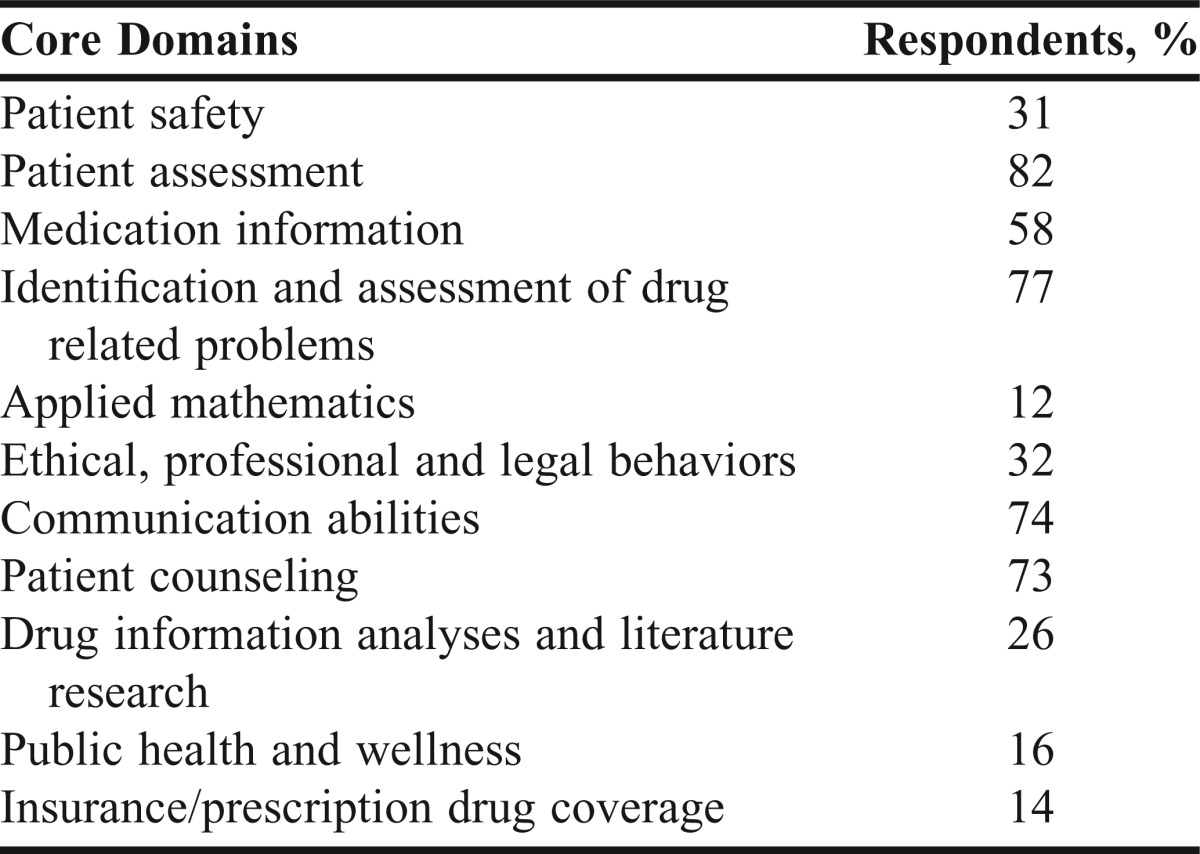
From a student learning assessment perspective, 33 colleges and schools used these techniques for high-stakes examinations, 57 for low-stakes examinations, and 34 for formative assessments. Fifteen colleges and schools used these techniques for all 3 types of assessment. Of the colleges and schools that used simulation, simulation-based teaching methodologies had been incorporated into 68 programs (approximately 91.9%) as an approach to teach and/or assess at least 1 ACPE pre-APPE core domain (Table 2). The most frequently reported pre-APPE core domains that used simulation were patient assessment (82%) and identification and assessment of drug-related problems (77%). The least frequently reported pre-APPE core domains were applied mathematics (14%) and insurance/prescription drug coverage (13.5%).
Table 2.
Pre-APPE Core Domains Assessed by Simulation at Colleges and Schools of Pharmacy (N=68)
DISCUSSION
To the authors’ knowledge, this is the first study highlighting and characterizing the use of high-fidelity mannequins and standardized patients within the pharmacy curriculum. The high percentage of colleges and schools that are using these simulation techniques clearly suggests that faculty members are beginning to embrace the use of simulation in pharmacy education. Even among those colleges and schools that were not using these teaching modalities (14/88 respondents), none felt that there was a lack of evidence supporting the use of simulation to educate student pharmacists. The primary reasons reported for not using simulation were high resource requirements and logistical constraints. This is in contrast to medical schools, the majority of which have a high level of resource commitment to simulation-based education and have fully incorporated simulation throughout the curriculum.32
Perhaps the most intriguing results from this survey center around simulation-based teaching modalities that are not fully incorporated within the PharmD curriculum, but present great opportunities going forward: IPPE, interprofessional education and teaching, and assessing ACPE pre-APPE core domains.
Only 29.7% of schools reported using simulation for IPPE hours. Simulation-based learning activities may provide a viable option for programs struggling to find IPPE sites and experiences for their student pharmacists. ACPE’s approved policy allows simulation-based activities to account for up to 20% of IPPE time, which is equivalent to 60 hours of simulation within the IPPE curriculum.34 Only 3 respondents indicated that their programs used the maximum allowed 60 hours of simulation for IPPEs.
Thirty-five schools (45.9%) reported using simulation for interprofessional learning activities. Interprofessional education for future healthcare professionals targets an essential common goal of a safer, more patient-centered US health care system. This focus on preparing health professions to “deliberatively work together” in interdisciplinary teams is evident in the expert panel report on Core Competencies of Interprofessional Collaborative Practice, which included professionals from pharmacy, nursing, dentistry, medicine, and public health.35 Simulation-based activities provide an option for a “new” educational technology approach to overcoming traditional barriers to interprofessional learning.
There is opportunity to use simulation for high- and low-stakes assessment as simulation serves as an excellent adjunct to traditional paper-based assessments.36 Simulation-based education methodologies could be especially useful when used to evaluate student performance for ACPE pre-APPE core domains and abilities. The pre-APPE core domains specifically include performance-based skills, along with knowledge, and attitudes/values/or behaviors. Also, simulation-based activities may be a good “fit” for programs to incorporate as assessments (high- or low-stakes). This would allow student pharmacists to demonstrate skills-based pre-APPE core domain competencies. PharmD programs seem to be recognizing the value of simulation in this capacity as they reported it being used to assess pre-APPE core domains and abilities at 68 (91.9%) of the colleges and schools that responded.
Limitations to this study include the 84% response rate, which did not include responses from 17 US colleges and schools of pharmacy. The survey instrument was sent to the chairs of the pharmacy practice (or equivalent) department and therefore may have excluded the use of simulation in basic sciences coursework. While the survey instrument did not mention that only simulation used in pharmacy practice should be included, simulation use in other departments may have been missed in the responses. Another limitation is that this survey instrument focused on the use of high-fidelity mannequins and standardized patients only. Some programs may have used lower-fidelity technology for high-fidelity simulation scenarios. Because the survey instrument did not use the term objective structured clinical examination (OSCE), a form of assessment in which simulated patients are often used, information from programs that use simulation only during OSCEs may have been missed.
CONCLUSION
Simulation-based teaching modalities are being used in many US colleges and schools of pharmacy. However, there appears to be room for increasing the role of simulation for specific aspects of the PharmD curriculum including for IPPE, interprofessional education, and for high- and low-stakes assessment, particularly for assessment of pre-APPE competency domains. It may be necessary for colleges and schools of pharmacy to commit to simulation technology as a necessary addition to the annual budget and/or to explore opportunities for interprofessional collaborations to share simulation resources. This may alleviate the biggest barrier to the use of simulation within pharmacy colleges and schools.
ACKNOWLEDGEMENTS
The authors thank Susan Wright, BS, a Master of Health Policy Administration degree candidate, for her assistance with survey data management.
REFERENCES
- 1.Gaba D. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(Suppl. 1):i2–i10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mieure KD, Vincent WR, III, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seybert AL, Kane-Gill SL. Elective course in acute care using online learning and patient simulation. Am J Pharm Educ. 2011;75:Article 54. doi: 10.5688/ajpe75354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vyas D, Wombwell E, Russell E, Caligiuri F. High-fidelity patient simulation series to supplement introductory pharmacy practice experiences. Am J Pharm Educ. 2010;74(9):Article 169. doi: 10.5688/aj7409169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marken PA, Zimmerman C, Kennedy C, Schremmer R, Smith KV. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am J Pharm Educ. 2010;74(7):Article 120. doi: 10.5688/aj7407120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson JD, Bray BS, Willson NM, Weeks DL. Using Human patient simulation to prepare student pharmacists to manage medical emergencies in an ambulatory setting. Am J Pharm Educ. 2011;75(1):Article 3. doi: 10.5688/ajpe7513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tokunaga J, Takamura N, Ogata K, et al. Vital sign monitoring using human patient simulators at pharmacy schools in Japan. Am J Pharm Educ. 2010;74(7):Article 132. doi: 10.5688/aj7407132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tofil NM, Benner KW, Worthington MA, Zinkan L, White ML. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2):Article 21. doi: 10.5688/aj740221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilliland I, Frei BL, McNeill J, Stovall J. Use of high-fidelity simulation to teach end-of-life care to pharmacy students in an interdisciplinary course. Am J Pharm Educ. 2012;76(4):Article 66. doi: 10.5688/ajpe76466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vyas D, McCulloh R, Dyer C, Gregory G, Higbee D. An interprofessional course using human patient simulation to teach patient safety and teamwork skills. Am J Pharm Educ. 2012;76(4):Article 71. doi: 10.5688/ajpe76471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shrader S, McRae L, King IV WM, Kern D. A simulated interprofessional rounding experience in a clinical assessment course. Am J Pharm Educ. 2011;75(4):Article 61. doi: 10.5688/ajpe75461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2):Article 34. doi: 10.5688/aj700234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dobson R, Taylor J, Cassidy J, Walker D, Proctor P, Perepelkin J. Interprofessional and intraprofessional teams in a standardized patient assessment lab. Pharm Educ. 2007;7(2):159–166. [Google Scholar]
- 18.Schultz KK, Marks A. Community-based collaboration with high school theater students as standardized patients. Am J Pharm Educ. 2007;71(2):Article 29. doi: 10.5688/aj710229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rickles NM, Tieu P, Myers L, Galal S, Chung V. The impact of a standardized patient program on student learning of communication skills. Am J Pharm Educ. 2009;73(1):Article 4. doi: 10.5688/aj730104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. doi: 10.1016/j.pec.2011.05.018. Blom L, Wolters M, TenHoor-Suykerbuyk M, van Paassen J, van Oyen A. Pharmaceutical education in patient counseling: 20h spread over 6 years? Patient Educ Couns. 2011;83(3):465–471. [DOI] [PubMed] [Google Scholar]
- 21.Robins L, Brock DM, Gallagher T, et al. Piloting team simulations to assess interprofessional skills. J Interprof Care. 2008;22(3):325–328. doi: 10.1080/13561820801886438. [DOI] [PubMed] [Google Scholar]
- 22.Curtin LB, Finn LA, Czosnowski QA, Whitman CB, Cawley MJ. Computer-based simulation training to improve learning outcomes in mannequin-based simulation exercises. Am J Pharm Educ. 2011;75(6):Article 113. doi: 10.5688/ajpe756113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benedict N, Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ. 2011;75(2):Article 21. doi: 10.5688/ajpe75221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loke S, Tordoff J. Winikoff M, McDonald J, Vlugter P, Duffull S. SimPharm: how pharmacy students made meaning of a clinical case differently in paper- and simulation-based workshops. Br J Educ Technol. 2011;42(5):865–874. [Google Scholar]
- 25.Begley KJ, Coover KL, Tilleman JA, Ryan Haddad AM, Augustine SC. Medication therapy management training using case studies and the mirixapro platform. Am J Pharm Educ. 2011;75(3):Article 49. doi: 10.5688/ajpe75349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frenzel JE. Using electronic medical records to teach patient-centered care. Am J Pharm Educ. 2010;74(4):Article 71. doi: 10.5688/aj740471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JJ, Sobieraj DM, Kuti EL. Student measurement of blood pressure using a simulator arm compared with a live subject's arm. Am J Pharm Educ. 2010;74(5):Article 82. doi: 10.5688/aj740582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kopacek KB, Dopp AL, Dopp JM, Vardeny O, Sims JJ. Pharmacy students' retention of knowledge and skills following training in automated external defibrillator use. Am J Pharm Educ. 2010;74(6):Article 109. doi: 10.5688/aj7406109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel S, Vincent AH, Abel SR, Jacobs CM, Dunlop SR, Seibert M. A virtual clean room to teach usp 797 regulations for intravenous medications. Am J Pharm Educ. 2011;75(1):Article 7. doi: 10.5688/ajpe7517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sherman JJ, Riche DM, Stover KR. Physical assessment experience in a problem-based learning course. Am J Pharm Educ. 2011;75(8):Article 156. doi: 10.5688/ajpe758156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Darbishire PL, Plake KS, Kiersma Me, White JK. An introductory pharmacy practice experience on improving medication adherence. Am J Pharm Educ. 2012;76(3):Article 42. doi: 10.5688/ajpe76342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Passiment M, Sacks H, Huang G. Medical Simulation in Medical Education: Results of an AAMC Survey. Washington, DC; 2011. https://www.aamc.org/download/259760/data/medicalsimulationinmedicaleducationanaamcsurvey.pdf. Accessed November 6, 2012.
- 33.Hayden J. Use of simulation in nursing education: national survey results. J Nurs Regul. 2010;1(3):52–57. [Google Scholar]
- 34.ACPE. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. S2007, Guidelines 2.0, Preamble Addendum, Appendix D. Chicago. Illinois: 2011. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed on November 6, 2012.
- 35. Interprofessional Education Collaborative Expert Panel: Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel, 2011. Washington, DC, Interprofessional Education Collaborative. http://www.asph.org/userfiles/CollaborativePractice.pdf. Accessed May 3, 2012.
- 36.Bray BS, Schwartz CR, Odegard PS, Hammer DP, Seybert AL. Assessment of human patient simulation-based learning. Am J Pharm Educ. 2011;75(10):Article 208. doi: 10.5688/ajpe7510208. [DOI] [PMC free article] [PubMed] [Google Scholar]


