Abstract
Objective
To investigate the abundance and seasonal dynamics of mosquitoes, and to detect Japanese encephalitis virus (JEV) in these mosquitoes at the nesting colony of ardeid birds.
Methods
Mosquitoes were collected bimonthly from July 2009 to May 2010 by Centers for Disease Control. Light traps and dry ice, as a source of CO2, were employed to attract mosquitoes. Mosquitoes were first identified, pooled into groups of upto 50 mosquitoes by species, and tested for JEV infection by viral isolation and reverse transcriptase polymerase chain reaction.
Results
A total of 20 370 mosquitoes comprising 14 species in five genera were collected. The five most abundant mosquito species collected were Culex tritaeniorhynchus (95.46%), Culex vishnui (2.68%), Culex gelidus (0.72%), Anopheles peditaeniatus (0.58%) and Culex quinquefasciatus (0.22%). Mosquito peak densities were observed in July. All of 416 mosquito pools were negative for JEV.
Conclusions
This study provides new information about mosquito species and status of JEV infection in mosquitoes in Thailand. Further study should be done to continue a close survey for the presence of this virus in the ardeid birds.
Keywords: Mosquito, Japanese encephalitis virus, Vector, Abundance, Ardeid bird
1. Introduction
The Japanese encephalitis virus (JEV) is a mosquito-borne zoonotic infection recognized as the major causes of encephalitis in Eastern and Southern Asia[1]. It has been estimated an annual incidence of 45 000 humans cases and 10 000 deaths[2],[3]. This virus is a member of the Japanese encephalitis (JE) serogroup of the genus Flavivirus, family Flaviviridae. Other important members in this serogroup are West Nile virus, St. Louis encephalitis virus, Kunjin virus and Murray Valley encephalitis virus[4]. JEV was first isolated in 1935 in Japan, and it has spread throughout Asia and Australia[3]. Since the first epidemic of JEV in 1969, this virus became endemic in Thailand with 1 500 to 2 500 reported cases of viral encephalitis each year during 1970-1985[2]. At present, this virus remains an important cause of encephalitis among hospitalized patients in Thailand[2].
JEV is maintained in enzootic transmission cycles among mosquitoes, wild birds and pigs[5]. The principal vector of JEV throughout Asia is Culex tritaeniorhynchus (Cx. tritaeniorhynchus) whereas other Culex mosquitoes also play a role as vectors. Pigs are one of the primary amplification hosts and probably the major determinant of human epidemic activity. Wild birds, particularly ardeid birds (e.g. egrets and herons) are also primary amplification hosts of JEV including black-crowned night herons (Nycticorax nycticorax), little egrets (Egretta garzetta), and intermediate or plumed egrets (Egretta intermedia)[1]. This virus can infect humans and horses, showing transient and low levels of viremia and are considered as dead-end hosts[1],[5]. Several places in Thailand contain important colonies of resident and migratory birds. In particular, Ban Wang Pet (Bang Rakam, Phitsanulok) is one of the most important sites for ardeid birds, especially egrets. The objective of our study was to investigate the abundance, seasonal dynamics, and potential JEV infection in these mosquitoes at the nesting colony of ardeid birds in Ban Wang Pet. The present study was designed to investigate the abundance and seasonal dynamics of mosquitoes, and to detect JEV in these mosquitoes at the nesting colony of ardeid birds. The information obtained from this study will be useful for future research on epidemiological studies, detection and prevention of JEV in Thailand.
2. Materials and methods
2.1. Study site
Ban Wang Pet (Bang Rakam, Phitsanulok) is one of the most important sites for ardeid birds, especially egrets. This place is actually classified as the largest colony of egrets in Thailand. The bird species found in this area include cattle egret (Bubulcus ibis), little egret (Egretta garzetta), intermediate egret (Egretta intermedia), great egret (Egretta alba), Chinese egret (Egretta eulophotes), black-crowned night heron (Nycticorax nycticorax) and little cormorant (Phalacrocorax niger). Therefore, the site might potentially be an important source vector borne diseases.
2.2. Mosquito collection
Mosquitoes were collected bimonthly by using CO2-baited CDC light traps (John W. Hock Company, Gainesville, USA) with dry ice used as a source of CO2 to attract mosquitoes from July 2009 to May 2010. Five traps were operated from 6 p.m. until 6 a.m. on each study day. Mosquitoes were transported alive to laboratory for species identification by using description and illustrated keys[6]. They were pooled by species ranged from 1 to 50 and stored at -80 °C until tested for virus.
2.3. Viral isolation
A pool of mosquitoes was homogenized in 1 000 µL of minimum essential medium (MEM 10×, Penicillin G, Streptomycin and Fungizone) in 1.5 mL Eppendorf tube by using plastic pestle. The homogenated mosquito was centrifuged at 4 000 rpm for 10 min and supernatant was passed 0.45 µm syring filter. The 200 µL of samples were inoculated into baby hamster kidney (BHK-21) cells and incubated at 37 °C in a 5% CO2 incubator for 2 h. About 150 µL of the samples of BHK-21 cells were discarded and added 500 µL of maintenance medium (2% fetal bovine serum in MEM) and then incubated at 37 °C in 5% CO2. The presence of cytopathic effect (CPE) was checked daily for 3 d. Positive CPE was confirmed by reverse transcription polymerase chain reaction (RT-PCR).
2.4. Viral ribonucleic extraction and reverse transcription polymerase chain reaction
Viral ribonucleic acid (RNA) was extracted from mosquitoes by using a viral nucleic acid extraction kit (Geneaid Biotech Ltd., Taiwan). The RT-PCR was performed using a one-step RT-PCR kit (QIAGEN Ltd., Germany) for detection of JEV infection. Briefly, the reaction mixture contained 0.125 µL of forward primer JE/WN-OF 5′-GRA ARM GDG ARG ACA TYT GGT GTG G-3′, 0.125 µL of reverse primer JE/WN-OR 5′-CGG GGT CTC CTC TAA CCT CTA GTC C-3′, 2 µL of template DNA, 5 µL of 5× one-step RT-PCR buffer (QIAGEN), 1 µL of 10 mmol/L dNTP mix (QIAGEN), 1 µL of one-step RT-PCR enzyme (QIAGEN) and RNase-free water was added to a total volume of 25 µL. PCR cycling conditions were as follows: 1 cycle at 50 °C for 30 min; 1 cycle at 95 °C for 15 min; 35 cycles at 94 °C for 45 seconds followed by 70 °C for 45 seconds, 72 °C for 90 seconds and final extension at 72 C° for 10 min. Positive control was obtained from JE vaccine strain Beijing-1. Negative control consisted of master mix minus RNA templates. PCR products were separated by gel electrophoresis and visualized under UV light. The specific size of PCR product for JEV was 591 base pairs. The RT-PCR positive specimens will be confirmed for JEV by using specific method, SYBR I-based real-time RT-PCR with primer JE-multi-forward 5′-AGA ACG GAA GAY AAC CAT GAC TAA-3′ and JE-multi-reverse 5′-CCG CGT TTC AGC ATA TTG AT-3′ as described by Shirato et al[7].
3. Results
3.1. Seasonal abundance of mosquitoes
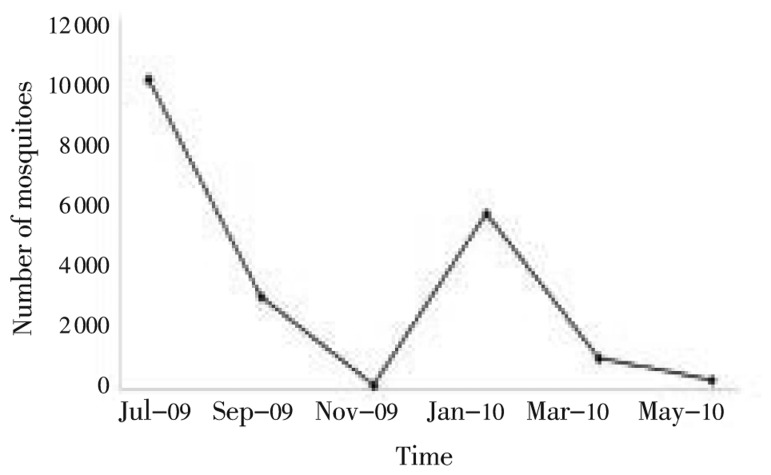
There were 20 370 mosquitoes collected in this study. Five genera in 14 species of mosquitoes were collected including Aedes, Anopheles, Armigeres, Culex and Mansonia. The five most abundant mosquito species collected were Cx. tritaeniorhynchus (95.46%), Culex vishnui (Cx. vishnui) (2.68%), Culex gelidus (Cx. gelidus) (0.72%), Anopheles peditaeniatus (An. peditaeniatus) (0.58%) and Culex quinquefasciatus (Cx. quinquefasciatus) (0.22%) (Table 1). The number of mosquitoes in July 2009, September 2009, November 2009, January 2010, March 2010 and May 2010 were 10 070, 3 035, 187, 5 691, 1 052 and 335 respectively (Figure 1).
Table 1. Total number of each mosquito species collected and their test outcome for JEV at the nesting colony of ardeid birds in Phitsanulok Province, Thailand.
| Mosquito species | CollectionNo. | Percent (%) | Pools No. | Positive pools |
| Ae. aegypti | 1 | 0.00 | 1 | 0 |
| An. argyropus | 2 | 0.01 | 1 | 0 |
| An. barbirostris | 2 | 0.01 | 1 | 0 |
| An. peditaeniatus | 118 | 0.58 | 2 | 0 |
| Ar. subalbatus | 3 | 0.01 | 1 | 0 |
| Cx. bitaeniorhynchus | 2 | 0.01 | 1 | 0 |
| Cx. fascocephala | 4 | 0.02 | 1 | 0 |
| Cx. gelidus | 146 | 0.72 | 3 | 0 |
| Cx. pseudovishnui | 36 | 0.18 | 1 | 0 |
| Cx. quinquefasciatus | 44 | 0.22 | 1 | 0 |
| Cx. tritaeniorhynchus | 19 445 | 95.46 | 390 | 0 |
| Cx. vishnui | 545 | 2.68 | 11 | 0 |
| Mansonia indiana | 18 | 0.09 | 1 | 0 |
| Mansonia uniformis | 4 | 0.02 | 1 | 0 |
| Total | 20 370 | 100.00 | 416 | 0 |
Figure 1. Mosquito seasonal dynamics at the nesting colony of ardeid birds in Phitsanulok Province, Thailand.
3.2. JEV infection in mosquitoes
We tested a total of 416 mosquito pools, and all of them were negative for JEV isolation. These results were confirmed by using RT-PCR, and all of them were negative (Table 1).
4. Discussion
This study reports the mosquito abundance at the nesting colony of ardeid birds at Ban Wang Pet site. The site is located near the Yom River and surrounded by rice fields which are suitable breeding place for Culex sp. and Hyrcanus group of Anopheles sp.[8],[9], especially Cx. tritaeniorhynchus, Cx. vishnui, Cx. gelidus and An. peditaeniatus. However, other mosquito genera in this study such as Aedes, Armigeres and Mansonia were also found in this area but in smaller numbers. Culex mosquitoes were the genus most frequently collected in this study. These mosquitoes are known to have a nocturnal feeding pattern and many of them have been collected in large numbers at night by using light traps[8]. Ae. aegypti was the mosquito species least collected in this study, probably because this species has a predominant diurnal activity[6].
Cx. tritaeniorhynchus, the most abundant mosquito species collected in this study, is the principal vector of JEV[1]. This species was identified as a JEV vector species in Thailand since the stains of the disease, when it was isolated from this species in Chiangmai Valley during 1970[10]. Other species of Culex mosquito frequently collected in our study i.e., Cx. gelidus, Cx. fuscocephala and Cx. vishnui were also reported as JEV vectors in Thailand[10],[11]. Cx. pseudovishnui and Cx. bitaeniorhynchus, also found in our study, were reported to transmit JEV in India and Malaysia[12],[13]. It is also important to remark that Cx. quinquefasciatus has recently became another potential mosquito vector for JEV in Thailand[14]. In addition, JEV has been isolated from other genera of mosquitoes such as Aedes sp., Anopheles sp. and Mansonia sp.[15],[16]. An. peditaeniatus, the 4th most abundant mosquito species in this study, has been found to be the secondary vector of JEV in India[16]. This mosquito species has been found abundantly and widely distributed in Thailand[17], but the role as vector of JEV in Thailand remains unclear.
The highest and lowest numbers of mosquitoes collected in this study occurred in July and November respectively. Such peaks in mosquito abundance concords with the study carried out by Somboon et al. in Northern Thailand[18]. They found a peak of rice field mosquitoes occurred during rainy season and showed a sharp rise in the population in July when most of the rice fields were ploughed, and a marked decline in mosquito population densities occurred after transplanting in August when the fields were flooded. In addition, they also showed that the average number of larvae plus pupae per square meter in rice fields was the highest in July when the fields were ploughed, but in the period from transplanting to harvesting (August to November), the densities were very low. Furthermore, the study of Takagi et al. also supported rice cultural practices that have the effect on the abundance of mosquitoes in Northern Thailand[19]. At any rate, the number of mosquitoes may also vary depending on several factors such as rice field density, insect predators and artificial control of the water supply to the rice field[20],[21].
Our study shows no evidence of JEV for the collected mosquitoes. A recent study of mosquito surveillance for JEV also found JEV negative in the mosquitoes collected at the Asian open-billed stork nested area and bat cave in Thailand[22],[23]. Although these are promising results on the status of JEV in Thailand, mosquito active surveillance should be continuously conducted because 1) we can not definitively rule out that other sites are affected by JEV, 2) mosquitoes at important bird areas will continue being a potential disease vector, 3) JEV remains an important cause of encephalitis in Thailand, and 4) to prevent any potential JEV epidemics. In a further study JEV antigens and antibodies should be studied in order to help conclude whether ardeid birds are a natural important reservoir for JEV in Thailand.
Acknowledgments
This work was supported by the Monitoring and Surveillance Center for Zoonotic Diseases in Wildlife and Exotic Animals, Faculty of Veterinary Science, Mahidol University (Grant number 0517.131/5944). Special thanks go to Dr. Norberto Asensio, Faculty of Environment and Resource studies, Mahidol University for a critical review of this manuscript.
Comments
Background
JE has a wide geographical distribution in Asia. JEV is a mosquito-borne member of the family Flaviviridae, genus Flavivirus, and mainly affects humans. Infection can occur in a number of animal species including horses and pigs. The virus is transmitted by mosquitoes and is maintained by a mosquito-aquatic bird cycle. The primary mosquito vector of JEV is Cx. tritaeniorhynchus, although species such as Cx. gelidus, Cx. fuscocephala, and Cx. annulirostris are important secondary or regional vectors.
Research frontiers
This work is performed to investigate the abundance and seasonal dynamics of mosquitoes collected from Ban Wang Pet sites classified as the largest colony of egrets in Thailand. The mosquitoes were used as materials to detect JEV infection using reverse transcription polymerase chain reaction.
Related reports
Results in this study correspond to previous studies reported by Somboon et al. (1989) and Tiawsirisup (2010). The former found a peak of rice field mosquitoes occurred in July and markedly declined in August in Northern Thailand, and the latter reported that they could not detect any JEV in mosquitoes collected from nested area in central Thailand.
Innovations and breakthroughs
This study has shown that the highest and the lowest numbers of mosquitoes were collected in July and November, respectively, and Cx. tritaeniorhynchus is the most common encountered mosquito species among five genera in 14 species collected. However, there are no any mosquito vectors harboring JEV agents.
Applications
It is significant to know the distribution of vector-borne diseases and related viruses in migrating birds. The present study suggests that mosquito active surveillance should be continuously conducted due to several reasons including they cannot definitively rule out that other sites are affected by JEV, and mosquitoes at important bird areas will continue being a potential disease vector. Therefore, it is important to monitor globally the distribution of mosquitoes associated with JEV, including other Flavivirus.
Peer review
This is one of the most important studies on vector-borne zoonotic disease surveillance researches in view of increasing worldwide travelers and globally climate changes. The authors evaluated the seasonal abundance of mosquitoes vector transmitted JE and indicated that it is related with rice field status.
Footnotes
Foundation Project: This work was supported by the Monitoring and Surveillance Center for Zoonotic Diseases in Wildlife and Exotic Animals (MOZWE), Faculty of Veterinary Science, Mahidol University (Grant No. 0517.131/5944).
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Van den Hurk AF, Ritchie SA, Mackenzie JS. Ecology and geographical expansion of Japanese encephalitis virus. Annu Rev Entomol. 2009;54:17–35. doi: 10.1146/annurev.ento.54.110807.090510. [DOI] [PubMed] [Google Scholar]
- 2.Olsen SJ, Supawat K, Campbell AP, Anantapreecha S, Liamsuwan S, Tunlayadechanont S, et al. et al. Japanese encephalitis virus remains an important cause of encephalitis in Thailand. Int J Infect Dis. 2010;14(10):888–892. doi: 10.1016/j.ijid.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Mackenzie JS, Williams DT. The zoonotic flaviviruses of southern, south-eastern and eastern Asia, and Australasia: the potential for emergent viruses. Zoonoses Public Health. 2009;56(6–7):338–356. doi: 10.1111/j.1863-2378.2008.01208.x. [DOI] [PubMed] [Google Scholar]
- 4.Weissenbock H, Hubálek Z, Bakonyi T, Nowotny N. Zoonotic mosquito-borne flaviviruses: worldwide presence of agents with proven pathogenicity and potential candidates of future emerging diseases. Vet Microbiol. 2010;140(3–4):271–280. doi: 10.1016/j.vetmic.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 5.Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emerg Infect Dis. 2009;15(1):1–7. doi: 10.3201/eid1501.080311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rattanarithikul R, Harrison BA, Panthusiri P, Coleman RE. Illustrated keys to the medically important mosquitoes of Thailand I. Background; geographic distribution; lists of genera, subgenera, and species; and a key to the genera. Southeast Asian J Trop Med Public Health. 2005;36(Suppl 1):1–80. [PubMed] [Google Scholar]
- 7.Shirato K, Miyoshi H, Kariwa H, Takashima I. Detection of West Nile virus and Japanese encephalitis virus using real-time PCR with a probe common to both viruses. J Virol Methods. 2005;126(1–2):119–125. doi: 10.1016/j.jviromet.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Rattanarithikul R, Harbach RE, Harrison BA, Panthusiri P, Jones JW, Coleman RE. Illustrated keys to the mosquitoes of Thailand II. Genera Culex and Lutzia. Southeast Asian J Trop Med Public Health. 2005;36(Suppl 2):1–97. [PubMed] [Google Scholar]
- 9.Rattanarithikul R, Harrison BA, Harbach RE, Panthusiri P, Coleman RE, Panthusiri P. Illustrated keys to the mosquitoes of Thailand. IV. Anopheles. Southeast Asian J Trop Med Public Health. 2006;37(Suppl 2):1–128. [PubMed] [Google Scholar]
- 10.Gould DJ, Edelman R, Grossman RA, Nisalak A, Sullivan MF. Study of Japanese encephalitis virus in Chiangmai Valley, Thailand. IV. Vector studies. Am J Epidemiol. 1974;100(1):49–56. doi: 10.1093/oxfordjournals.aje.a112008. [DOI] [PubMed] [Google Scholar]
- 11.Ali A, Igarashi A, Paneru LR, Hasebe F, Morita K, Takagi M, et al. et al. Characterization of two Japanese encephalitis virus strains isolated in Thailand. Arch Virol. 1995;140(9):1557–1575. doi: 10.1007/BF01322530. [DOI] [PubMed] [Google Scholar]
- 12.Mourya DT, Mishra AC, Soman RS. Transmission of Japanese encephalitis virus in Culex pseudovishnui & C. tritaeniorhynchus mosquitoes. Indian J Med Res. 1991;93:250–252. [PubMed] [Google Scholar]
- 13.Vythilingam I, Oda K, Chew TK, Mahadevan S, Vijayamalar B, Morita K, et al. et al. Isolation of Japanese encephalitis virus from mosquitoes collected in Sabak Bernam, Selangor, Malaysia in 1992. J Am Mosq Control Assoc. 1995;11(1):94–98. [PubMed] [Google Scholar]
- 14.Nitatpattana N, Apiwathnasorn C, Barbazan P, Leemingsawat S, Yoksan S, Gonzalez JP. First isolation of Japanese encephalitis from Culex quinquefasciatus in Thailand. Southeast Asian J Trop Med Public Health. 2005;36(4):875–858. [PubMed] [Google Scholar]
- 15.Zhang HL. The natural infection rate of mosquitoes by Japanese encephalitis B virus in Yunnan Province. Zhonghua Yu Fang Yi Xue Za Zhi. 1990;24(5):265–267. [PubMed] [Google Scholar]
- 16.Upadhyay RK, Ahmad S. Japanese encephalitis virus (JEV): it's epidemiology, disease and vector control with special reference to immune surveillance and safety measures: A review. J Pharm Res. 2011;4(8):2409–2429. [Google Scholar]
- 17.Changbunjong T, Weluwanarak T, Toawan N. Mosquito distribution and West Nile Virus infection in zoos and in important sites of migratory and resident birds, Thailand. Asian Pac J Trop Dis. 2012;2(4):268–272. [Google Scholar]
- 18.Somboon P, Choochote W, Khamboonruang C. Studies on the Japanese encephalitis vectors in Amphoe Muang, Chiang Mai, Northern Thailand. Southeast Asian J Trop Med Public Health. 1989;20(1):9–17. [PubMed] [Google Scholar]
- 19.Takagi M, Suwonkerd W, Tsuda Y, Sugiyama A, Wada Y. Effects of rice culture practices on the abundance of Culex mosquitoes (Diptera: Culicidae) in northern Thailand. J Med Entomol. 1997;34(3):272–276. doi: 10.1093/jmedent/34.3.272. [DOI] [PubMed] [Google Scholar]
- 20.Richards E, Masuoka P, Brett-Major D, Smith M, Klein TA, Kim HC, et al. et al. The relationship between mosquito abundance and rice field density in the Republic of Korea. Int J Health Geogr. 2010;9:32. doi: 10.1186/1476-072X-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abu Hassan A, Hamady D, Tomomitsu S, Michael B, Jameel SLAS. Breeding patterns of the JE vector Culex gelidus and its insect predators in rice cultivation areas of northern peninsular Malaysia. Trop Biomed. 2010;27(3):404–416. [PubMed] [Google Scholar]
- 22.Tiawsirisup S, Nuchprayoon S. Mosquito distribution and Japanese encephalitis virus infection in the immigration bird (Asian open-billed stork) nested area in Pathum Thani province, central Thailand. Parasitol Res. 2010;106(4):907–910. doi: 10.1007/s00436-010-1757-6. [DOI] [PubMed] [Google Scholar]
- 23.Tiawsirisup S, Punpee A, Nuchprayoon S. Mosquito distribution and Japanese encephalitis virus infection in a bat cave and its surrounding area in Lopburi province, central, Thailand. Thai J Vet Med. 2012;42(1):43–49. [Google Scholar]