Abstract
Background
Mitral valve repair for posterior mitral leaflet (PML) prolapse has been considered to be a standard treatment because of its high success rate and high level of patient satisfaction. The aim of this study was to evaluate the clinical results of two different techniques of PML prolapse, quadrangular resection (QR) and chordal replacement (CR).
Materials and Methods
The subjects consisted of 56 patients who had undergone mitral valve repair for PML prolapse between November 1997 and December 2010. The patients were divided into two groups according to surgical technique. Among them, 31 patients underwent QR (group QR) and 25 patients had CR (group CR). We reviewed the medical records of the patients retrospectively to compare the clinical outcomes of both groups.
Results
After mitral valve repair, the degree of mitral regurgitation (MR) in both groups decreased to the to a mild degree or less and the amount of remnant MR was slightly higher in the CR group but it was not statistically different. Three patients received mitral valve-related reoperation (2 in the QR group and 1 in the CR group). Freedom from mitral valve-related reoperation at 7 years was 93% for the QR group and 96% for the CR group and was not significantly different between the two groups.
Conclusion
Both QR and CR showed excellent long-term results and were considered equally effective methods for PML prolapse.
Keywords: Mitral valve, Mitral valve prolapse, Chordae tendineae
INTRODUCTION
Mitral valve repair is the treatment of choice for patients with severe mitral regurgitation (MR) of posterior mitral leaflet (PML) prolapse. Although a variety of techniques are available, quadrangular resection (QR) or chordal replacement (CR) is the most frequently performed technique for the repair of PML prolapse. QR has been the standard technique with documented excellent long term results [1]. However, several problems, such as left ventricular outflow tract obstruction, kicking in the circumflex artery and leaflet restriction have been reported in this technique [2,3]. To overcome these problems and restore a larger coaptation surface for the mitral valve, a method for CR preserving PML tissue with extended polytetrafluoroethylene (ePTFE) has been developed to facilitate mitral valve repair and numerous studies have reported excellent long term results [4-6]. However, little is known of the results of CR in comparison to leaflet resection. The aim of the present study is to evaluate the clinical results of mitral valve repair, comparing CR and QR.
MATERIALS AND METHODS
1) Patients
From November 1997 to December 2010, 56 patients with PML prolapse who underwent mitral valve repair were included in the present study. Based on the surgical technique, the patients were classified into one of two groups: group QR (n=31) or group CR (n=25). Details on preoperative patient characteristics and echocardiographic findings are summarized in Table 1. The longest follow-up interval was 161 months in group QR and 124 in group CR, and the median follow-up period was 58 months in group QR and 69 in group CR.
Table 1.
Preoperative patient characteristics and echocardiographic findings
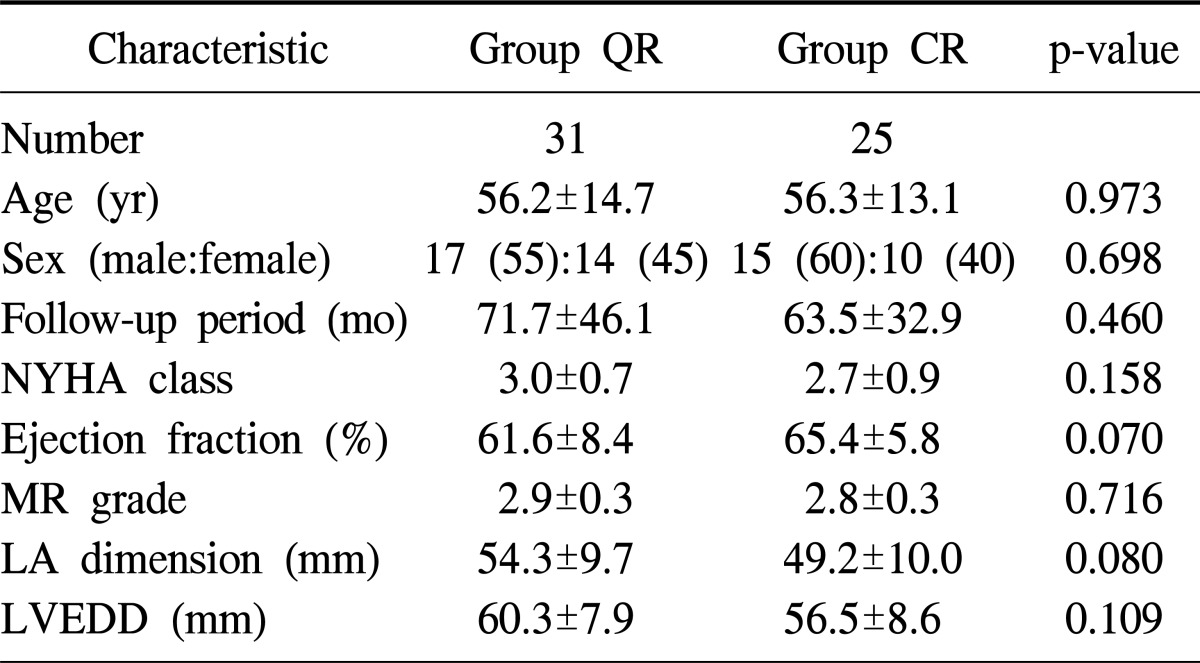
Values are presented as mean±standard deviation or number (%). Ordinal values are expressed as follows: none, 0; mild, 1; moderate, 2; severe, 3.
QR, quadrangular resection; CR, chordal replacement; NYHA, New York Heart Association; MR, mitral regurgitation; LA, left atrium; LVEDD, left ventricular end diastolic dimension.
2) Surgical procedures
The operative approach was a standard median sternotomy and cardiopulmonary bypass was initiated with an ascending aortic and two vena caval cannulations in all patients. Cold blood cardioplegia was used for heart arrest and protection. The mitral valve was exposed through an interatrial groove and tested with a valve hook and saline test. Prosthetic ring annuloplasty (Carpentier-Edwards ring, Edwards Lifesciences, Irvine, CA, USA; Duran annuloplasty ring, Medtronic, Minneapolis, MN, USA) was performed with 10 to 14 interrupted 2-0 Ticron sutures. The size of the ring was chosen according to the intertrigonal or intercommissural distance. In group QR, a prolapsed segment of the PML was resected and the leaflet continuity was restored with several simple interrupted sutures and ring annuloplasty was performed. In group CR, a 4-0 or 5-0 double armed ePTFE suture was passed through the tip of a papillary muscle. The two arms of the suture were passed through the free margin of the prolapsed segment of PML at 2 to 3 mm distance. The suture was tied, adjusting the appropriate chorda length, and ring annuloplasty was performed.
3) Statistical analysis
All analyses were performed with IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA). Continuous variables are expressed as the mean±standard deviation and categorical variables as percentages. Categorical data were compared by the χ2 test and continuous data by the Student's unpaired t-test and paired t-test. The Kaplan-Meier test was used to estimate the actuarial freedom from reoperation and survival rate. The log-rank method was used to determine statistical differences between groups.
RESULTS
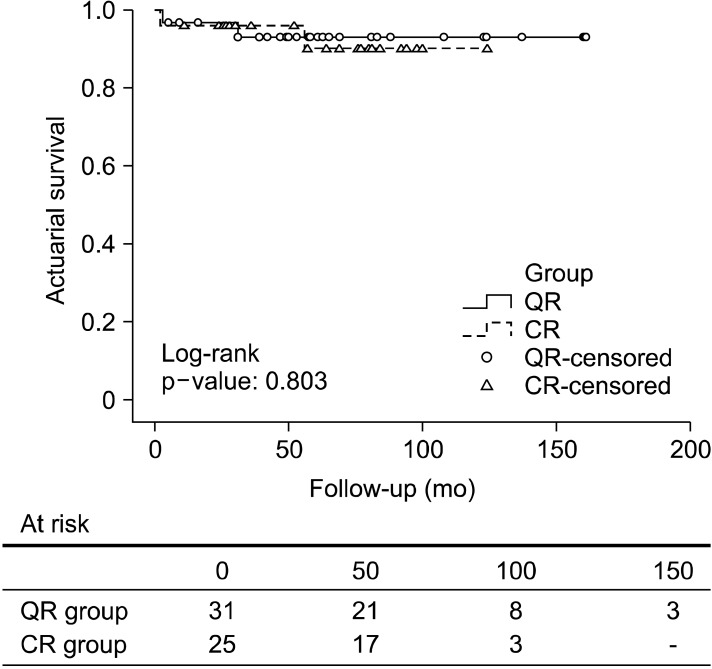
The mean operation time was 265.3±54 minutes, the mean cardiopulmonary bypass time was 96.4±30.8 minutes, and the mean aortic cross clamp time was 68.5±25.8 minutes. The chordal rupture was the most common cause of PML prolapse and the P3 segment was the most frequently involved. The prosthetic ring was not inserted in 10 patients (Table 2). One patient in group CR died in the early postoperative period, and the cause of death was sepsis. Three patients (2 in group QR, 1 in group CR) died in the late postoperative period and the reasons for the late deaths were traumatic intracerebral hemorrhage, renal failure in group QR, and acute myocardial infarction in group CR. The actuarial survival rate at 1, 5, and 7 years was 97%, 93%, and 93% in group QR and 96%, 90%, and 90% in group CR with no significant difference in the two groups' survival rates (log-rank p=0.803) (Fig. 1).
Table 2.
Surgical data
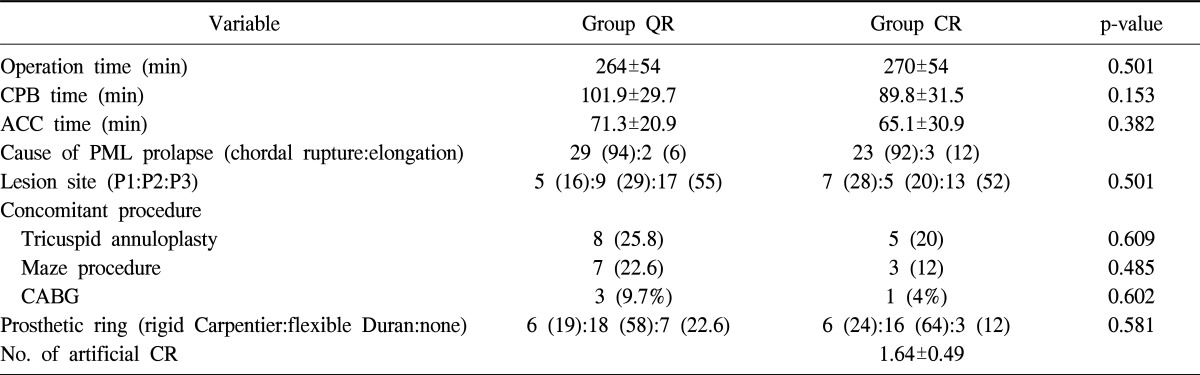
Values are presented as mean±standard deviation or number (%).
QR, quadrangular resection; CR, chordal replacement; CPB, cardiopulmonary bypass; ACC, aortic cross clamp; PML, posterior mitral leaflet; CABG, coronary artery bypass grafting.
Fig. 1.
Kaplan-Meier estimate of actuarial survival for 51 patients who underwent quadrangular resection (QR) or chordal replacement (CR).
The echocardiographic data were obtained at least 6 months after surgery at last follow-up in all patients except one reoperative case in group CR (mean interval, 35.1±36.3 months). When the ordinal grade of MR was transformed into a numerical value (none, 0; mild, 1; moderate, 2; severe, 3), the mean grade of remnant mitral regurgitation (rMR) was decreased to less than mild in the patients overall (0.73±0.69). The mean grade of rMR was 0.66±0.73 in the QR group and 0.82±0.64 in the CR group, with no significant difference between the two groups. In this series, there was no benefit for the CR group compared with the QR group with respect to mitral orifice area (MOA). Overall, the mean MOA was 2.25±0.62 cm2 and the two groups did not differ significantly (Table 3). When comparing data within each group, it was recognized that the echocardiographic outcomes were improved after the surgery (Table 4).
Table 3.
Postoperative echocardiographic data
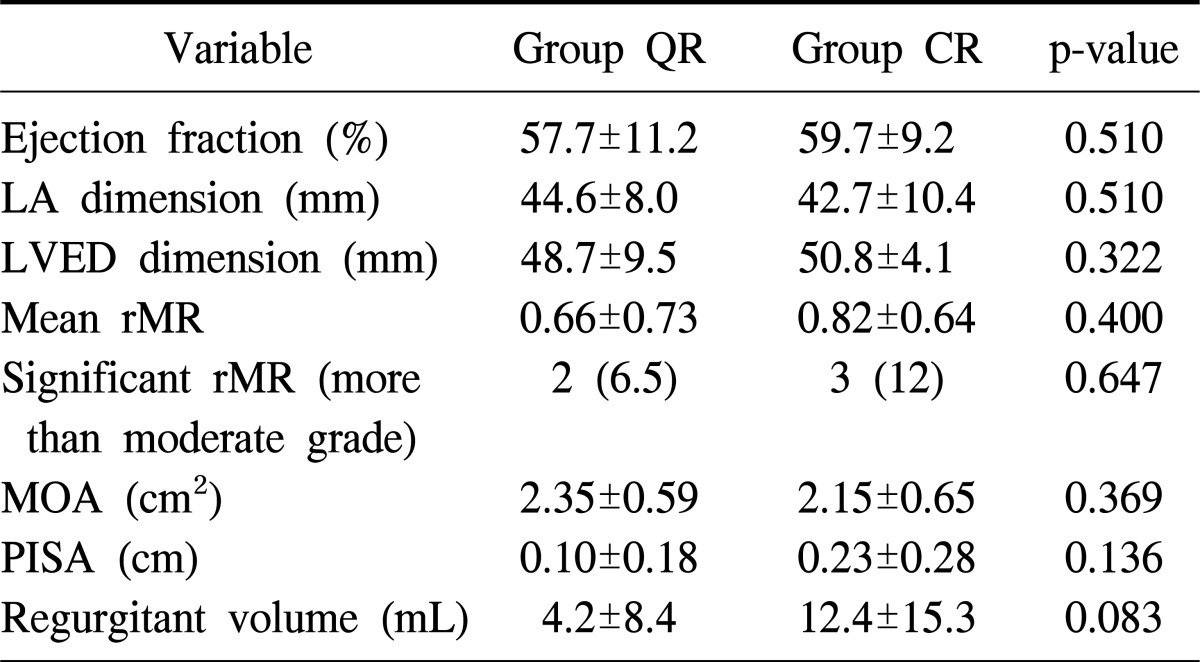
Values are presented as mean±standard deviation or number (%). Ordinal values are expressed as follows: none, 0; mild, 1; moderate, 2; severe, 3.
QR, quadrangular resection; CR, chordal replacement; LA, left atrium; LVED, left ventricular end diastolic; rMR, remnant mitral regurgitation; MOA, mitral orifice area; PISA, proximal isovelocity surface area.
Table 4.
Echocardiographic data before and after the surgery
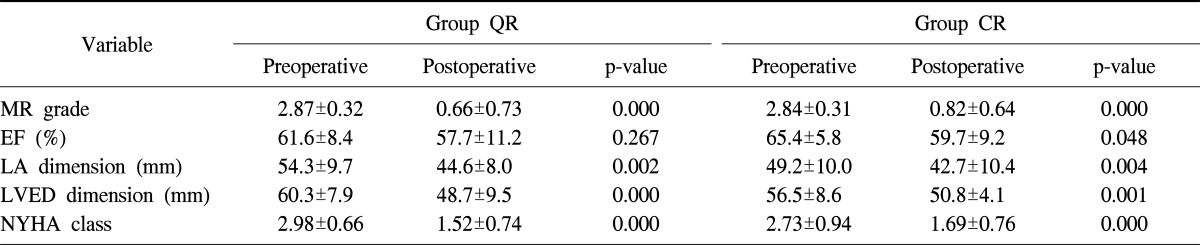
Values are presented as mean±standard deviation. Ordinal values are expressed as follows: none, 0; mild, 1; moderate, 2; severe, 3.
MR, mitral regurgitation; EF, ejection fraction; LA, left atrium; LVED, left ventricular end diastolic; NYHA, New York Heart Association; QR, quadrangular resection; CR, chordal replacement.
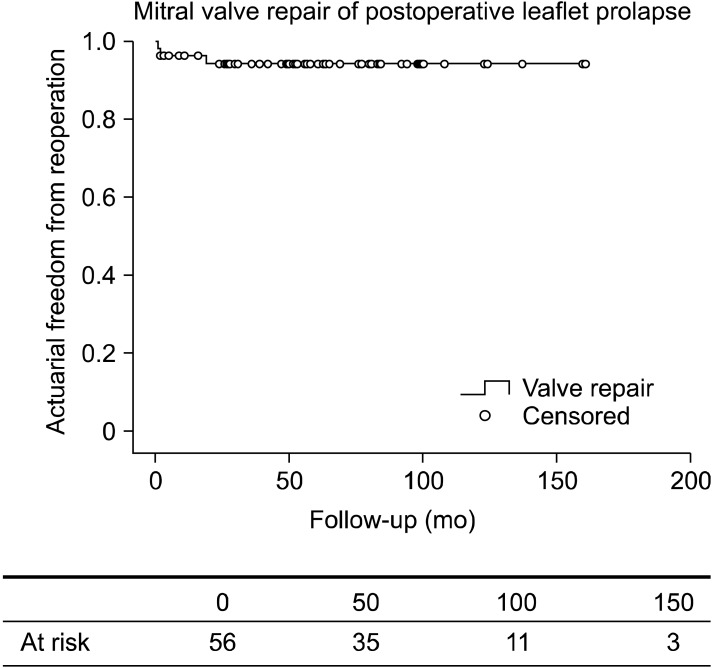
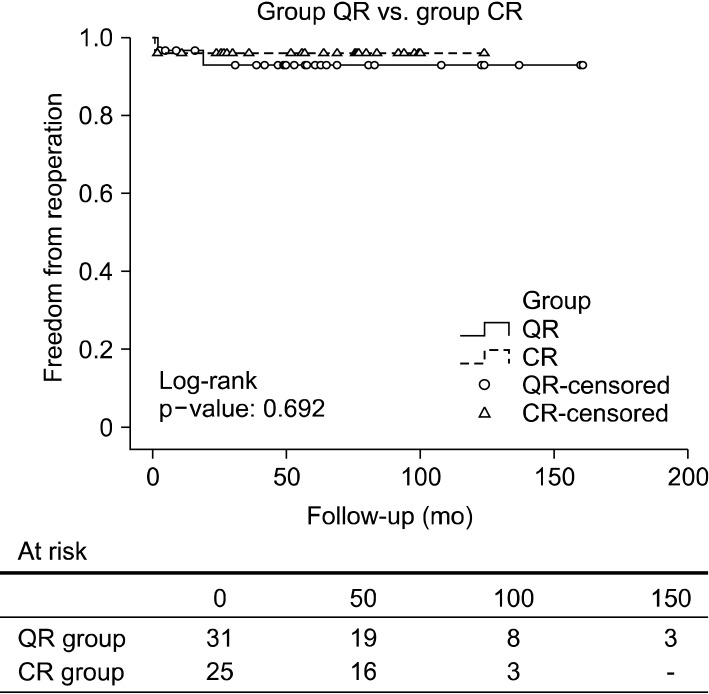
Among the five patients with significant rMR, two patients in group QR and one in group CR required mitral valve-related reoperation and the reasons for reoperation were dehiscence between reapproximated valve remnants and chordal rupture in another PML segment in group QR, and the aggravation of rMR in group CR. Two patients who did not receive reoperation have been observed in the outpatient department because symptoms and pulmonary pressure were within tolerable range. Overall, freedom from mitral valve-related reoperation at 1, 5, and 7 years was 95%, 94%, and 94% (Fig. 2). By group, the freedom from mitral valve-related reoperation at 1, 5, and 7 years was 96%, 93%, and 93% in group QR and 96%, 96%, and 96% in group CR, and there was no statistical difference between the two groups (log-rank p=0.692) (Fig. 3).
Fig. 2.
Kaplan-Meier curve of actuarial freedom from reoperation.
Fig. 3.
Kaplan-Meier curve of actuarial freedom from reoperation between group quadrangular resection (QR) and group chordal replacement (CR).
DISCUSSION
Significant MR should be treated to preserve left ventricular function and improve long term survival [7,8]. With regard to correcting MR, mitral valve repair is preferred to replacement because it has no possibilities of anticoagulant or prosthesis-related complications and is favorable to cardiac function [9-11]. PML prolapse causes significant MR more frequently than anterior mitral leaflet prolapse or prolapse of both leaflets. Several techniques have been proposed to repair PML prolapse. QR and CR are the most popular techniques and have shown excellent long-term results [12-16].
In this series, we compared the clinical outcomes of both techniques for repairing PML prolapse. Both outcomes were relatively favorable, and there were no significant differences between the groups regarding clinical data such as mortality rate, operation time, reexploration rate for bleeding, postoperative cerebral events, and symptomatic status.
It is known that the incidence of reoperation is equally low with CR and QR [17,18]. When comparing both methods for mitral valve-related reoperation, it was reported that CR is slightly better than QR in other series [19]. However, we found that they were not statistically different and showed high freedom from mitral valve-related reoperation. It is thought that if PML prolapse is successfully repaired, the long-term durablility of mitral valve structure can be equally achieved by both techniques.
It is important how often MR recurs after mitral valve repair. In other series, only a small portion of patients (3.8%) who underwent CR showed moderate MR at follow-up [20]. In the present series, 2 of 31 patients (6.5%) who underwent QR showed moderate to severe MR and 3 of 26 patients (12%) who had CR showed moderate to severe MR. Our results showed a slightly higher recurrence rate of moderate to severe MR than other studies. Postoperative echocardiography revealed that group CR had a higher volume of remnant regurgitation than group QR even though it was not significantly different. Thus it should be noted that CR is usually successful for repairing PML prolapse but is technically more demanding and has a possibility of leaving more remnant MR than QR in spite of intraoperative echocardiographic examination. For this reason, we have initially performed CR for PML prolapse to preserve the leaflet tissue. However, in case it was not successful, it was abandoned and QR was employed.
CR is superior for preserving native leaflet tissue, leaflet motion, and mitral valve orifice area and avoiding the possibility of left outflow tract obstruction compared to QR [21]. However, QR can be easily performed and has more extensive evidence of excellent results in repairing PML prolapse than CR. Therefore, it is thought that both techniques have their own benefits relative to each other.
To achieve a larger MOA is one of the major goals of mitral valve repair [22]. It was reported that CR would produce a longer coaptation line than QR, but it failed to demonstrate a greater MOA [20]. We found that CR did not show a larger MOA (2.35 cm2 vs. 2.15 cm2, p=0.369) and it is presumed that the amount of resected leaflet tissue was not excessive by QR because most of the prolapsed segments were not P2.
This study is a retrospective analysis with all of its weak points and had a relatively small number of patients. Follow-up echocardiography for each patient was performed at different intervals and might have been more likely to be performed in symptomatic patients than asymptomatic patients.
CONCLUSION
Clinical results of both QR and CR were excellent and equally effective for repair of PML prolapse, and the majority of patients experienced symptomatic improvement. Therefore, the choice between QR and CR should be individualized corresponding to the technical feasibility and valvular structure.
Footnotes
This article was presented at the 43th autumn scientific meeting of The Korean Society for Thoracic and Cardiovascular Surgery.
No potential conflict of interest relevant to this article was reported.
References
- 1.Deloche A, Jebara VA, Relland JY, et al. Valve repair with Carpentier techniques: the second decade. J Thorac Cardiovasc Surg. 1990;99:990–1001. [PubMed] [Google Scholar]
- 2.Jebara VA, Mihaileanu S, Acar C, et al. Left ventricular outflow tract obstruction after mitral valve repair: results of the sliding leaflet technique. Circulation. 1993;88(5 Pt 2):II30–II34. [PubMed] [Google Scholar]
- 3.Da Col U, Di Bella I, Bardelli G, Koukoulis G, Ramoni E, Ragni T. Triangular resection and folding of posterior leaflet for mitral valve repair. J Card Surg. 2006;21:274–276. doi: 10.1111/j.1540-8191.2006.00231.x. [DOI] [PubMed] [Google Scholar]
- 4.David TE, Omran A, Armstrong S, Sun Z, Ivanov J. Longterm results of mitral valve repair for myxomatous disease with and without chordal replacement with expanded polytetrafluoroethylene sutures. J Thorac Cardiovasc Surg. 1998;115:1279–1285. doi: 10.1016/S0022-5223(98)70210-7. [DOI] [PubMed] [Google Scholar]
- 5.Salvador L, Mirone S, Bianchini R, et al. A 20-year experience with mitral valve repair with artificial chordae in 608 patients. J Thorac Cardiovasc Surg. 2008;135:1280–1287. doi: 10.1016/j.jtcvs.2007.12.026. [DOI] [PubMed] [Google Scholar]
- 6.Perier P, Hohenberger W, Lakew F, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the "respect rather than resect" approach. Ann Thorac Surg. 2008;86:718–725. doi: 10.1016/j.athoracsur.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med. 1996;335:1417–1423. doi: 10.1056/NEJM199611073351902. [DOI] [PubMed] [Google Scholar]
- 8.Wisenbaugh T, Skudicky D, Sareli P. Prediction of outcome after valve replacement for rheumatic mitral regurgitation in the era of chordal preservation. Circulation. 1994;89:191–197. doi: 10.1161/01.cir.89.1.191. [DOI] [PubMed] [Google Scholar]
- 9.Gillinov AM, Blackstone EH, Nowicki ER, et al. Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovasc Surg. 2008;135:885–893. 893.e1–893.e2. doi: 10.1016/j.jtcvs.2007.11.039. [DOI] [PubMed] [Google Scholar]
- 10.Shuhaiber J, Anderson RJ. Meta-analysis of clinical outcomes following surgical mitral valve repair or replacement. Eur J Cardiothorac Surg. 2007;31:267–275. doi: 10.1016/j.ejcts.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Baek MJ, Na CY, Oh SS, et al. Mitral valve reconstruction in patients with moderate to severe left ventricular dysfunction. Korean J Thorac Cardiovasc Surg. 2003;36:812–819. [Google Scholar]
- 12.Johnston DR, Gillinov AM, Blackstone EH, et al. Surgical repair of posterior mitral valve prolapse: implications for guidelines and percutaneous repair. Ann Thorac Surg. 2010;89:1385–1394. doi: 10.1016/j.athoracsur.2009.12.070. [DOI] [PubMed] [Google Scholar]
- 13.Perier P, Stumpf J, Gotz C, et al. Valve repair for mitral regurgitation caused by isolated prolapse of the posterior leaflet. Ann Thorac Surg. 1997;64:445–450. doi: 10.1016/S0003-4975(97)00537-7. [DOI] [PubMed] [Google Scholar]
- 14.Aoyagi S, Tanaka K, Kawara T, Oryoji A, Kosuga K, Oishi K. Long-term results of mitral valve repair for non-rheumatic mitral regurgitation. Cardiovasc Surg. 1995;3:387–392. doi: 10.1016/0967-2109(95)94156-q. [DOI] [PubMed] [Google Scholar]
- 15.Seeburger J, Kuntze T, Mohr FW. Gore-tex chordoplasty in degenerative mitral valve repair. Semin Thorac Cardiovasc Surg. 2007;19:111–115. doi: 10.1053/j.semtcvs.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Lee JW, Lim HJ, Jung SH, et al. Midterm results of mitral valve repair by the new chordae formation technique. Korean J Thorac Cardiovasc Surg. 2001;34:329–337. [Google Scholar]
- 17.Chiappini B, Sanchez A, Noirhomme P, et al. Replacement of chordae tendineae with polytetrafluoroethylene (PTFE) sutures in mitral valve repair: early and long-term results. J Heart Valve Dis. 2006;15:657–663. [PubMed] [Google Scholar]
- 18.Nardi P, Pellegrino A, Scafuri A, et al. Survival and durability of mitral valve repair surgery for degenerative mitral valve disease. J Card Surg. 2011;26:360–366. doi: 10.1111/j.1540-8191.2011.01275.x. [DOI] [PubMed] [Google Scholar]
- 19.Seeburger J, Falk V, Borger MA, et al. Chordae replacement versus resection for repair of isolated posterior mitral leaflet prolapse: a egalite. Ann Thorac Surg. 2009;87:1715–1720. doi: 10.1016/j.athoracsur.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Rankin JS, Orozco RE, Rodgers TL, Alfery DD, Glower DD. "Adjustable" artificial chordal replacement for repair of mitral valve prolapse. Ann Thorac Surg. 2006;81:1526–1528. doi: 10.1016/j.athoracsur.2005.01.042. [DOI] [PubMed] [Google Scholar]
- 21.Filsoufi F, Carpentier A. Principles of reconstructive surgery in degenerative mitral valve disease. Semin Thorac Cardiovasc Surg. 2007;19:103–110. doi: 10.1053/j.semtcvs.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Falk V, Seeburger J, Czesla M, et al. How does the use of polytetrafluoroethylene neochordae for posterior mitral valve prolapse (loop technique) compare with leaflet resection?: a prospective randomized trial. J Thorac Cardiovasc Surg. 2008;136:1205. doi: 10.1016/j.jtcvs.2008.07.028. [DOI] [PubMed] [Google Scholar]