Abstract
An increase in cardiac radiofrequency catheter ablation for treating refractory atrial fibrillation has resulted in an increased prevalence of complications. Among numerous complications of radiofrequency catheter ablation, atrio-esophageal fistula, although rare, is known to have fatal results. We report a case of successful management of an atrio-esophageal fistula as a complication of cardiac radiofrequency catheter ablation.
Keywords: Atrium, Esophageal surgery, Fistula, Radiofrequency, Complication
CASE REPORT
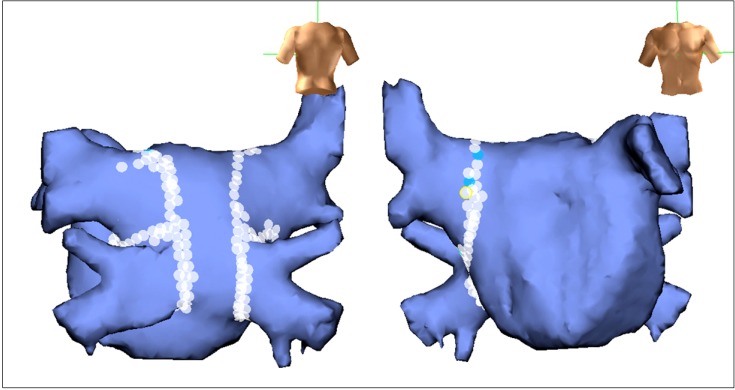
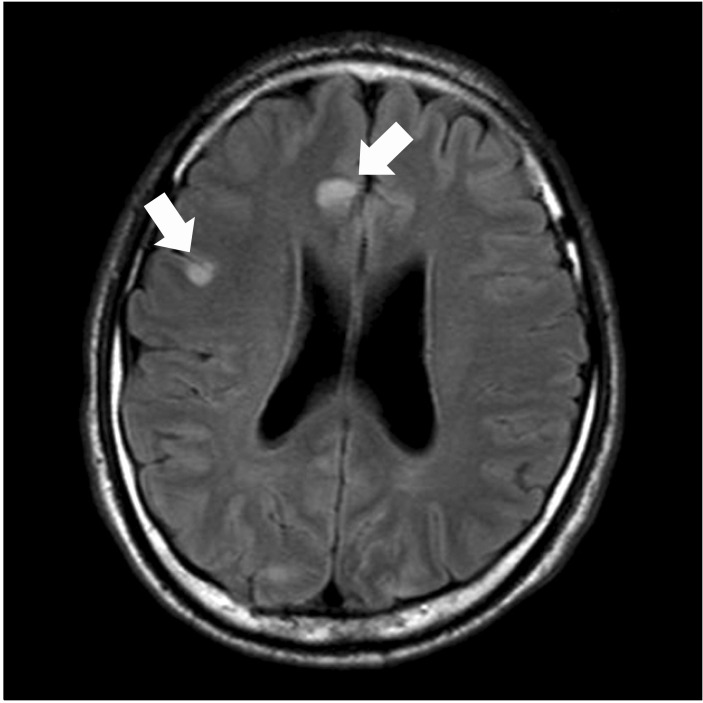
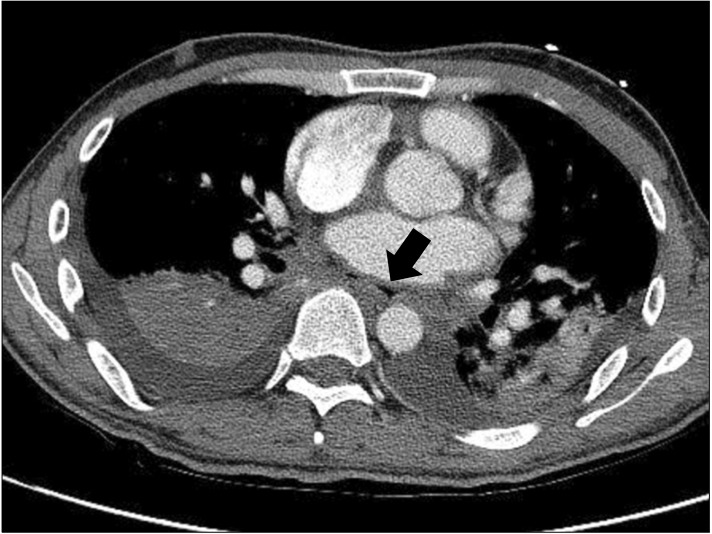
A previously healthy, 46-year-old man with a 2-year history of atrial fibrillation presented with fever, headache, and dizziness. Three weeks earlier, he had undergone cardiac radiofrequency catheter ablation for symptomatic atrial fibrillation refractory to medical management by a cardiologist. Circumferential ablation of a wide area encircling the four pulmonary vein antra was performed point by point (Fig. 1). The energy was delivered under power control with a maximum pre-set power of average 30 to 35 watts using a Lasso catheter (Lasso; Biosense Webster, Diamond Bar, CA, USA). Three days after the ablation, the patient had a single episode of headache and all other symptoms were resolved. Two weeks later, he developed fever, chills, cough, and headache. Two days after the symptoms started, he visited the emergency room. He was febrile (temperature, 39℃) and hypotensive (blood pressure, 70/55 mmHg) with an irregular heart rate of 120 beats/min. Atrial fibrillation was confirmed by electrocardiography and then he underwent synchronized direct current cardioversion. Although the rhythm was restored by cardioversion, he was noted to be confused, with generalized tonic-clonic seizures. His blood leukocyte count was 16,500 cells/mL, with 87% neutrophilic predominance. Findings of a chest radiograph were unremarkable, and a transthoracic and transesophageal echocardiogram showed no thrombus or vegetation. Empiric treatment with ceftriaxone was initiated, which resulted in resolution of the fever. Magnetic resonance imaging of the brain revealed multifocal infarcts (Fig. 2). Computed tomography of the chest showed a minute air pocket around the left atrium near the level of the esophagus, suggesting an atrio-esophageal fistula (AEF) (Fig. 3). The patient was taken to the operating room to repair the presumed fistula. Through a left posterolateral thoracotomy, adhesion between the esophagus and pericardium was observed, and a fistula between the left atrium and esophagus was found. The atrial lesion (2 cm) was closed with a bovine pericardial patch under cardiopulmonary bypass using a femoral artery and vein. The esophageal lesion (3 cm) was closed with simple interrupted sutures using 3-0 vicryl. Sutures were performed separately in two layers. The mucosal layer was sutured first and the muscle layer was reinforced. No buttressed suture was used because of acute inflammatory tissue around the lesion. Two sets of blood cultures revealed growth of Streptococcus mitis and Streptococcus viridians. He completed a 4-week course of ampicillin/sulbactam and 2-week course of amoxicillin/clavulanate treatment. Seven days after surgery, he underwent a leak test with grape juice and showed no leakage and started to drink water. On the tenth day after surgery, esophagography showed no leakage. He was discharged without any other complications except for mild left arm motor weakness. In follow-up computed tomography (CT) scans after 3 months, ostium of right inferior pulmonary vein stenosis was revealed. In addition, esophagogastroscopy after seven months showed the esophageal defect site to be fully recovered (Fig. 4).
Fig. 1.
The circumferential ablation line around the pulmonary veins.
Fig. 2.
Axial brain magnetic resonance image shows multiple infarcts (arrows).
Fig. 3.
Axial computed tomography images demonstrating pneumomediastinum (arrow).
Fig. 4.
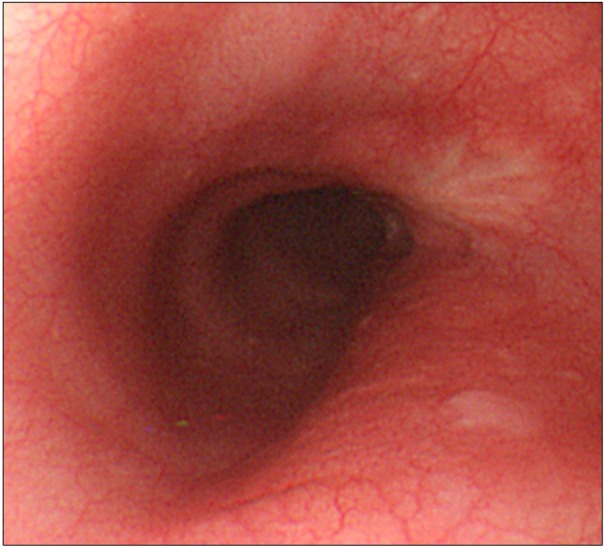
Esophagogastroscopy showed fully recovered esophageal defect site.
DISCUSSION
With an increase in cardiac radiofrequency catheter ablation for the treatment of refractory atrial fibrillation, there has also been a rise in complications. AEF due to thermal injury during cardiac radiofrequency catheter ablation is a rare complication with an incidence rate of 0.2% [1]. Although our patient survived with just minimal residual neurologic deficits, the mortality rate associated with AEF is very high. Cummings et al. [2] reported a mortality rate of 100% in a study with 9 patients. The overall mortality rate from all reported cases is 67% [3]. However, varying clinical presentations make diagnosis of such complications difficult.
Patients present from 3 to 41 days after the procedure with nonspecific symptoms, including fever, leukocytosis, neurologic symptoms, and chest pain [4]. Fever is one of the most common symptoms that occur in patients with AEF. Among those patients with reported symptoms, fever was noted in 75% of the patients with AEF [3]. However, fever is a nonspecific symptom, which can arise from inflammation after the procedure. Ruby et al. [5] reported that 8% of patients who underwent ablation developed fever within 24 hours after the procedure. Neurological deficits were presented in 69% of patients with clinical signs reported. Additional symptoms were mental status changes, transient ischemic attacks, stroke syndromes with hemiparesis, and seizures. Chest pain was also found in 24% of patients [3]. Leukocytosis was revealed in patients with AEF, presumably secondary to severe bacterial sepsis [6]. Bacterial spread to the systemic circulation from the esophagus through the AEF can produce bacteremia. Although Streptococcus mitis and Streptococcus viridians were detected in our patient's blood, the incidence of bacteremia is very low [3]. Endocarditis is rare as well, at only 0.2% at one high-volume center [1]. Transthoracic echocardiography did not provide useful information for the diagnosis of AEF. Furthermore, a transesophageal echocardiogram has the possibility of producing air embolism. A chest CT showing pneumomediastinum or air in the atrium is the most reliable method for AEF diagnosis. Approximately 90% of the patients studied with this modality were diagnosed with AEF [6]. Invasive esophageal procedures, including esophagogastroscopy, should be avoided for patients who may have an AEF due to the risk of air embolization. Among 9 patients with AEF for whom esophagogastroscopy was performed, 8 experienced immediate deterioration in their clinical status and eventually died [3]. Electrophysiologists have implemented strategies to minimize esophageal injuries. Avoidance of ablation near the esophagus, the titration of radiofrequency energy delivery at the posterior left atrial endocardium, and the use of alternative ablation methods are some of the most well established methods [7]. These methods may be effective for reducing the occurrence of AEF. However, in this case, a complication occurred. More indications at more clinics will increase the possibility that this complication can occur. Although 40% of patients who underwent surgery died, spontaneous resolution of a left atrio-esophageal fistula has not been reported yet. Also, all patients who did not undergo surgery died except for one patient who was successfully treated with an esophageal stent [3,8]. Although our patient had a minor neurologic deficit, early surgical management saved his life. Therefore, early diagnosis, prompt surgical treatment, and appropriate antibiotic therapy are thought to be crucial with regard to the survival rate of patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Dagres N, Hindricks G, Kottkamp H, et al. Complications of atrial fibrillation ablation in a high-volume center in 1,000 procedures: still cause for concern? J Cardiovasc Electrophysiol. 2009;20:1014–1019. doi: 10.1111/j.1540-8167.2009.01493.x. [DOI] [PubMed] [Google Scholar]
- 2.Cummings JE, Schweikert RA, Saliba WI, et al. Brief communication: atrial-esophageal fistulas after radiofrequency ablation. Ann Intern Med. 2006;144:572–574. doi: 10.7326/0003-4819-144-8-200604180-00007. [DOI] [PubMed] [Google Scholar]
- 3.Siegel MO, Parenti DM, Simon GL. Atrial-esophageal fistula after atrial radiofrequency catheter ablation. Clin Infect Dis. 2010;51:73–76. doi: 10.1086/653425. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi A, Kuwahara T, Takahashi Y. Complications in the catheter ablation of atrial fibrillation: incidence and management. Circ J. 2009;73:221–226. doi: 10.1253/circj.cj-08-1097. [DOI] [PubMed] [Google Scholar]
- 5.Ruby RS, Wells D, Sankaran S, et al. Prevalence of fever in patients undergoing left atrial ablation of atrial fibrillation guided by barium esophagraphy. J Cardiovasc Electrophysiol. 2009;20:883–887. doi: 10.1111/j.1540-8167.2009.01464.x. [DOI] [PubMed] [Google Scholar]
- 6.Dagres N, Kottkamp H, Piorkowski C, et al. Rapid detection and successful treatment of esophageal perforation after radiofrequency ablation of atrial fibrillation: lessons from five cases. J Cardiovasc Electrophysiol. 2006;17:1213–1215. doi: 10.1111/j.1540-8167.2006.00611.x. [DOI] [PubMed] [Google Scholar]
- 7.Bahnson TD. Strategies to minimize the risk of esophageal injury during catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2009;32:248–260. doi: 10.1111/j.1540-8159.2008.02210.x. [DOI] [PubMed] [Google Scholar]
- 8.Bunch TJ, Nelson J, Foley T, et al. Temporary esophageal stenting allows healing of esophageal perforations following atrial fibrillation ablation procedures. J Cardiovasc Electrophysiol. 2006;17:435–439. doi: 10.1111/j.1540-8167.2006.00464.x. [DOI] [PubMed] [Google Scholar]