Abstract
Background
Atrial fibrillation (AF) is a common complication in elderly patients with atrial septal defect (ASD). The purpose of this study was to examine the efficacy of the maze procedure in these patients.
Materials and Methods
Between February 2000 and May 2011, 46 patients underwent the maze procedure as a concomitant operation with ASD closure. Three patients who underwent a right-sided maze were excluded, and one patient was lost to follow-up. The mean follow-up duration was 3.2±2.5 years. Electrocardiography was performed 1 month, 3 months, 6 months, and 1 year after surgery, and checked annually after that.
Results
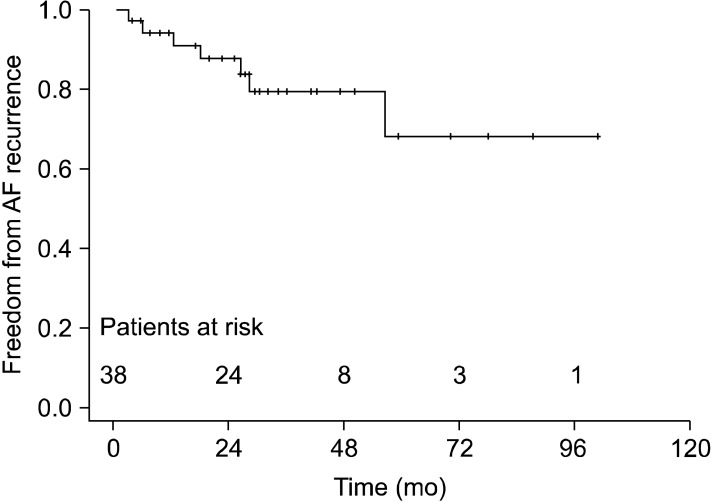
AF persisted in 4 patients after surgery. One year after surgery, among 38 patients, 55.3% remained in sinus rhythm without antiarrhythmic drugs. However, when including the patients who took antiarrhythmic drugs, 92.1% were in sinus rhythm. Freedom from AF recurrence at 3 months, 6 months, 1 year, 2 years, 3 years, and 5 years after surgery were 97.4±2.6, 94.4±3.8, 91.2±4.9, 87.8±5.8, 79.5±7.6, and 68.2±12.4, respectively. There was no early mortality after operation.
Conclusion
Concomitant treatment with the maze procedure and ASD closure is safe and effective for restoring the sinus rhythm.
Keywords: Arrhythmia surgery; Atrial fibrillation; Anti-arrhythmic agents; Congenital heart disease; Heart septal defects, atrial; Survival analysis
INTRODUCTION
Atrial fibrillation (AF) occurs frequently in patients who have atrial septal defect (ASD), which causes heart failure in elderly patients. Murphy et al. [1] reported the incidence of AF among patients who had ASD. The range of age among patients was between 25 and 41 years old and the incidence was 41% [1]. However, surgical closure of ASD did not lead to regression of the AF incidence [2]. In addition, AF is associated with a risk of thromboembolic complications, which requires patients to take drugs chronically. Therefore, restoring the sinus rhythm after ASD closure is crucial. During the past decade, the maze operation was recommended to patients with unsuccessful AF medication treatment. More recently, a concomitant operation of the maze procedure with surgical closure of ASD has been proposed [3]. However this treatment strategy is controversial due to the technical complexity, which may lead to prolonged surgical time due to aortic cross-clamping and cardiopulmonary bypass. In this study, we examined the efficacy of the maze procedure on AF with ASD. In addition, we searched for factors that could affect the recurrence of AF after the maze procedure in these patients.
MATERIALS AND METHODS
From January 2000 to December 2011, 46 consecutive patients with ASD and AF underwent the maze procedure combined with surgical closure of ASD. Among them, one patient was lost to follow-up after discharge. Forty-two patients underwent the modified Cox maze III procedure. There were some cases where right atriotomy was used only for ASD. In such cases Maze procedure was limited to the right side. However, since there were only three cases and such procedures were executed in the early stages of the study, they were excluded from the subject group. Medical and surgical records were reviewed retrospectively. The mean follow-up duration was 3.2±2.5 years. Electrocardiography (ECG) was routinely performed at 1 month, 3 months, 6 months, and 1 year after surgery, and checked annually from then on. The 3 month records were considered to be blank periods. During this 3 month period, transient rhythm change was not considered to be a treatment failure, and amiodarone was prescribed as an antiarrhythmic drug in patients with AF. The success of the maze procedure was defined as any rhythm other than atrial fibrillation, atrial flutter, and atrial tachycardia 3 months after the maze procedure. Junctional rhythm or atrioventricular block that required pacemaker insertion was regarded as a complication rather than a treatment failure.
The 42 patients who underwent the modified Cox maze III procedure as a concomitant operation with an ASD closure consisted of 25 men and 17 women. Their age at surgery ranged from 31 to 72 years with a mean±standard deviation of 52.5±9.5 years. Twenty-nine patients had persistent AF and 13 patients had paroxysmal AF. The average duration of AF was 27±29 months and average ASD size was 28.8±9.7 mm. Forty-one patients had ostium secundum type ASD and 1 had a sinus venosus type ASD. The cardiothoracic ratio was measured by a chest X-ray taken before the operation. The mean cardiothoracic ratio was 63.4%±7.5%. The left atrial diameter, left ventricular end diastolic diameter, and left ventricular end systolic diameter were also measured with echocardiography before the operation (Table 1). The ASD was closed with a pericardial patch fixed with glutamine aldehyde, which was harvested from the patients themselves in 38 cases, and direct primary closure was performed in 4 cases. The modified Cox maze III procedure was performed to achieve sinus rhythm with an energy source of cryoablation in 35 patients, radiofrequency in 1, and both in 5 patients. One patient underwent only the cut-and-sew technique. In most cases, maze lesions were made with the following protocol. The standard left atriotomy was extended slightly downwards. Around the pulmonary vein orifices, cryoablation was performed with the cryoablation probe at -60℃ for 2 minutes 30 seconds. Thereafter, the lesion was extended to the annulus of the posterior leaflet at the mitral valve and left atrial auricle. Below the coronary sinus and upper part above the inferior vena cava, cryoablation was conducted perpendicularly towards the tricuspid valve annulus. Accordingly, the final cryoablation proceeded from the counterpart of the standard right atriotomy to the tricuspid valve annulus. Radiofrequency ablation was performed only for pulmonary vein isolation when it was used as an energy source. Simultaneous cardiac procedures were tricuspid regurgitation (TR) repair in 15 patients and TR repair with mitral regurgitation repair in 20 patients.
Table 1.
Preoperative measurements in echocardiography
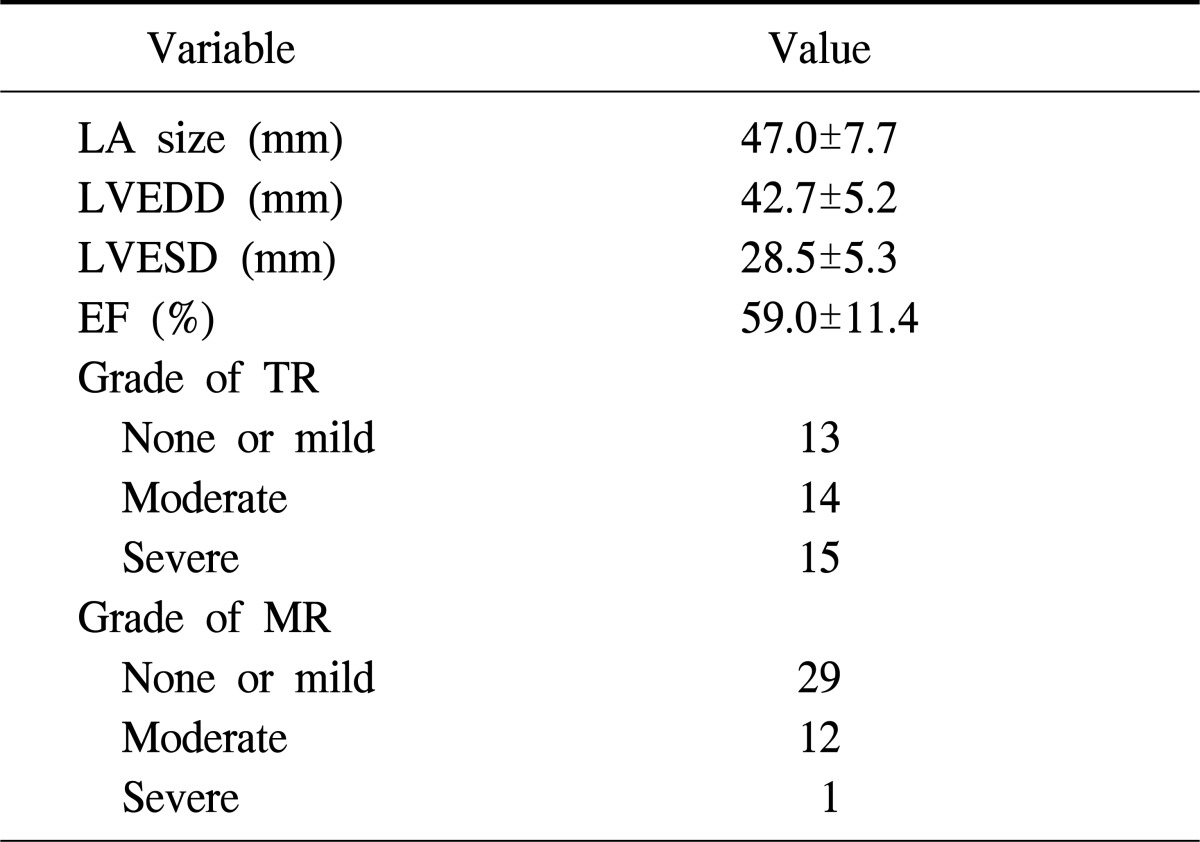
Values are presented as mean±standard deviation or number.
LA, left atrium; LVEDD, left ventricular end diastolic diameter; LVESD, left ventricular end systolic diameter; EF, ejection fraction; TR, tricuspid regurgitation; MR, mitral regurgitation.
In order to analyze the factors that influence restoration of sinus rhythm after the maze procedure, continuous variables were expressed as the mean±standard deviation. The Student's t-test was used and categorical variables were expressed in relative frequencies. Also, Fisher's exact test was used at the p<0.05 level. The data from 38 patients who achieved a restored sinus rhythm after the modified Cox maze III procedure were analyzed to assess the correlation using Spearman's rank correlation coefficient (ρ) and a Cox regression model at the significance level p<0.05 with IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). The sinus rhythm maintenance rate was calculated according to the Kaplan-Meyer method.
RESULTS
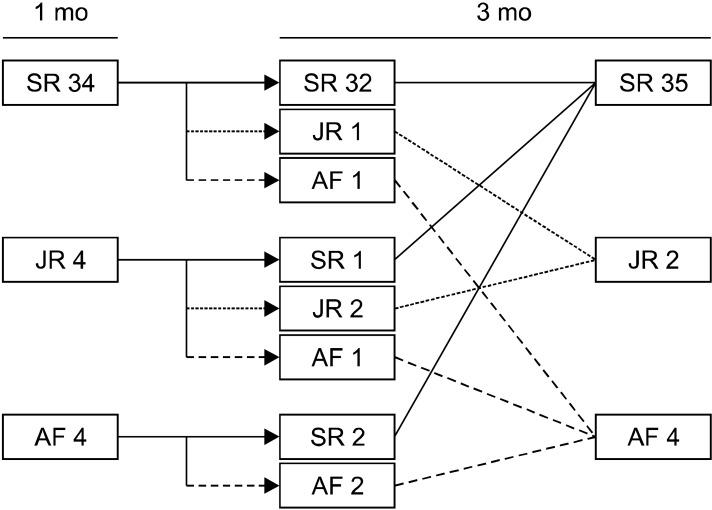
The mean cardiopulmonary bypass time was 134.7±41.8 minutes and mean aortic cross-clamp time was 104.9±33.4 minutes. AF persisted in 4 patients after the modified Cox maze III procedure. Three months after surgery, 35 patients achieved restored sinus rhythm (Fig. 1). One year after the operation, 21 patients (55.3%) remained in sinus rhythm without any antiarrhythmic drugs. However, when we included the patients who took antiarrhythmic drugs such as amiodarone, 35 patients (92.1%) were in sinus rhythm. The last follow-up ECG showed a sinus rhythm in 31 patients, AF in 9 (including 4 persistent AF patients), and junctional rhythm in 1. One patient needed implantation of a permanent pacemaker for tachy-brady syndrome (Table 2). There were no significant differences in patients' characteristics between patients who escaped from AF after the maze operation and patients who did not (Table 3). Freedom from AF recurrence at 3 months, 6 months, and 1 year, 2 years, 3 years, and 5 years after surgery was 97.4±2.6, 94.4±3.8, 91.2±4.9, 87.8±5.8, 79.5±7.6, and 68.2±12.4, respectively (Fig. 2). There was no relationship observed between the variables and recurrence of AF. Spearman's correlation with a preoperative cardiothoracic ratio and recurrence of AF showed the smallest p-value of 0.058, but it was not statistically significant (Table 4). Additionally, Cox regression analysis showed that none of the variables were related to the recurrence (Table 5). There was no early mortality after surgery, but only two late mortalities. The first patient died from right heart failure four months after ASD closure during hospitalization. This patient had already had right heart failure and severe pulmonary hypertension preoperatively. The patient's pulmonary arterial pressure was assumed using right ventricular pressure only with TR velocity. However, this patient had high right ventricular end diastolic pressure and the pulmonary arterial pressure was underestimated. The other patient died from diabetic nephropathy three years after surgery in another hospital.
Fig. 1.
Early results after surgery. SR, sinus rhythm; JR, junctional rhythm; AF, atrial fibrillation.
Table 2.
Effects of maze procedure (last checked rhythm of patients who regained sinus rhythm after maze procedure)
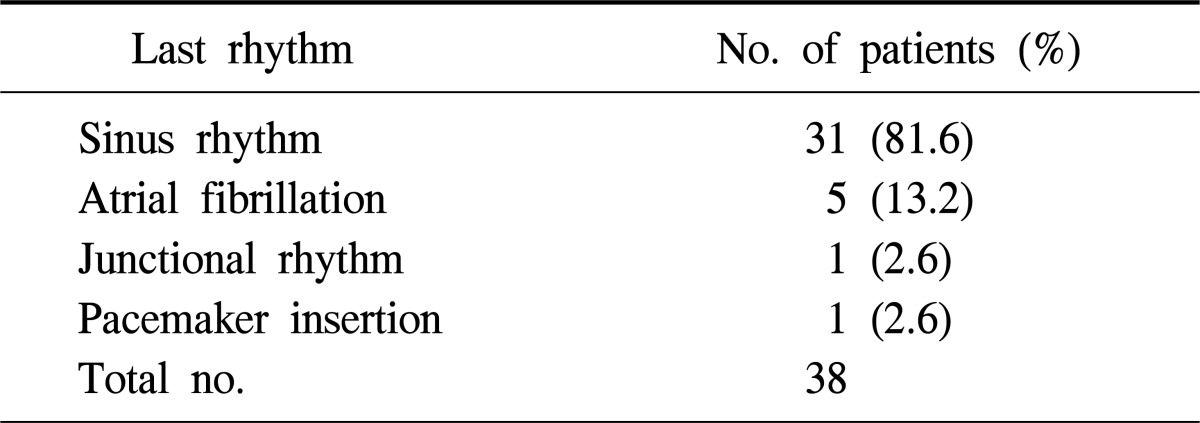
Table 3.
Comparison of patients who escaped from AF and who have persistent AF
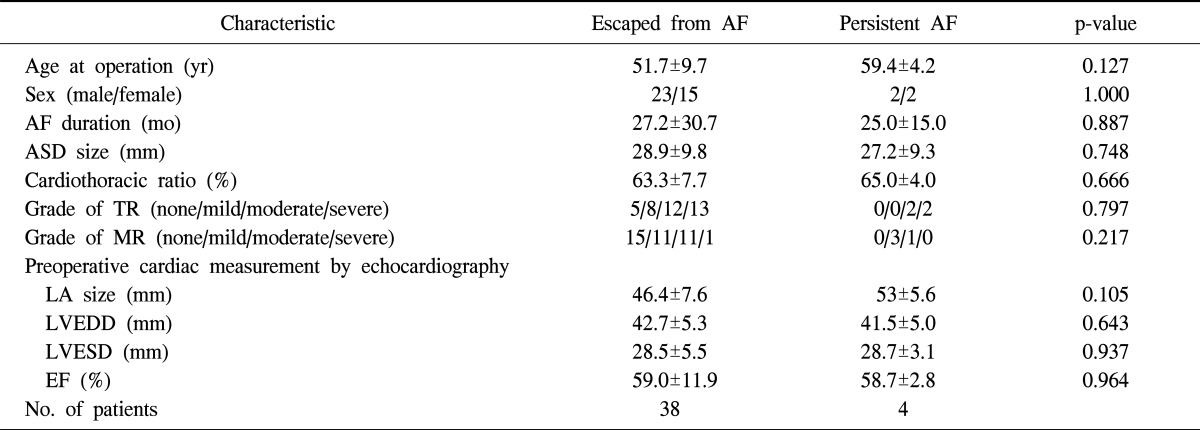
Values are presented as mean±standard deviation or number.
AF, atrial fibrillation; ASD, atrial septal defect; TR, tricuspid regurgitation; MR, mitral regurgitation; LA, left atrium; LVEDD, left ventricular end diastolic diameter; LVESD, left ventricular end systolic diameter; EF, ejection fraction.
Fig. 2.
Freedom from atrial fibrillation recurrence at 3 months, 6 months, and 1 years, 2 years, 3 years, and 5 years was 97.4±2.6, 94.4±3.8, 91.2±4.9, 87.8±5.8, 79.5±7.6, and 68.2±12.4, respectively. AF, atrial fibrillation.
Table 4.
Correlations between preoperative variables and recurrence rate of AF
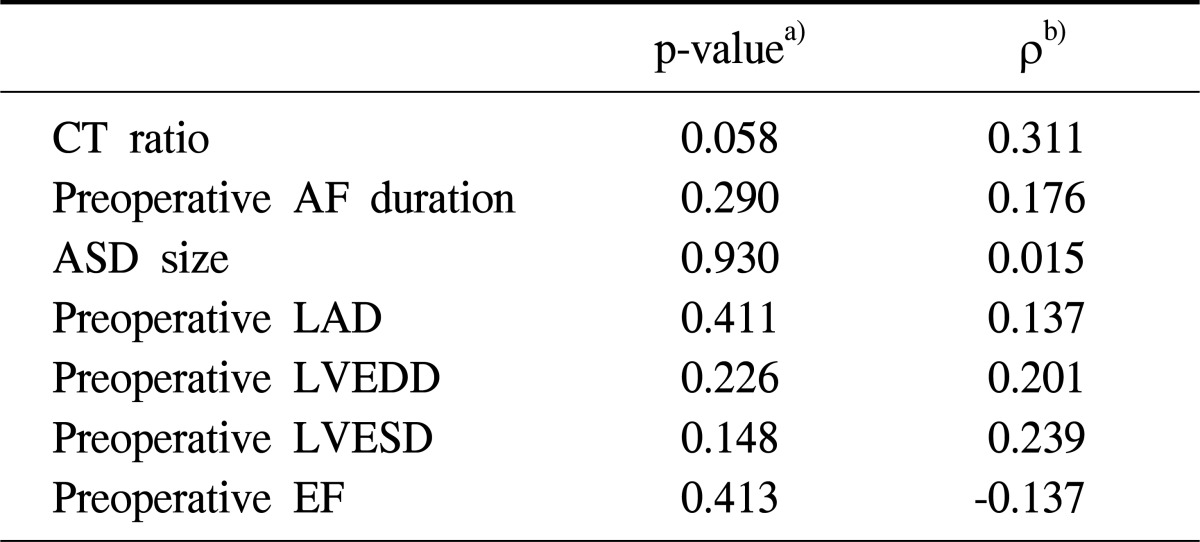
AF, atrial fibrillation; CT ratio, cardiothoracic ratio; ASD, atrial septal defect; LAD, left atrial diameter; LVEDD, left ventricular end diastolic diameter; LVESD, left ventricular end systolic diameter; EF, ejection fraction.
a)Statistical significance level was defined at p-value <0.05.
b)Spearman's rank correlation coefficient.
Table 5.
Risk factors for recurrence of AF (Cox regression)
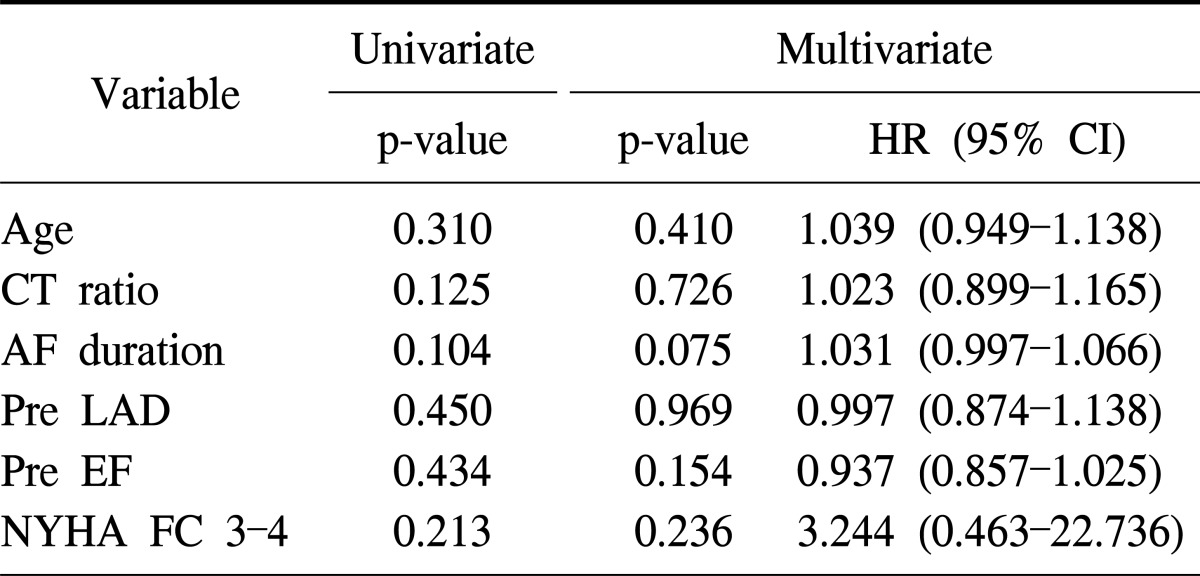
AF, atrial fibrillation; HR, hazard ratio; CI, confidence interval; CT ratio, cardiothoracic ratio; LAD, left atrial diameter; EF, ejection fraction; NYHA FC, New York Heart Association Functional Classification.
DISCUSSION
Atrial arrhythmia including atrial flutter and fibrillation is present in 14% to 22% of adult patients who have untreated ASD [4-6]. Among patients older than 40 years old who underwent ASD closure, more than 50% developed AF after operation [1]. AF increased the risk of thromboembolism and impaired ventricular function due to the lack of an organizing atrial contraction. However, surgical closure of ASD does not lead to regression of the incidence of AF [2]. Thus, despite the successful closure of ASD, patients are at the risk of stroke and bleeding due to anticoagulant administration [4]. From this correlation, an effort to regain sinus rhythm is necessary for patients who have AF associated with ASD. Since the 1980s, the Cox maze procedure has been used as the standard for treating medically refractory AF [7,8]. The mechanism of AF is explained by the multiple wavelet hypothesis and focal activation. AF can be initiated from a focal ectopic trigger focused in the cardiac muscle sleeve around the pulmonary veins. It can be maintained by producing a rapidly firing driver with fibrillatory propagation or by producing multiple irregular reentry circuits caused by rapid focal activity or local reentry [9,10]. The maze procedure is designed to interrupt the multiple wavelet macro reentry circuit on the basis of this theory. It prevents the recurrence of AF in over 90% of adult patients, including those with acquired or congenital heart disease [11,12]. This study reviewed the medical records of 42 patients who underwent the modified Cox maze procedure except one who was lost in the follow up. In only 3 cases, we performed a right-sided maze procedure.
Previous studies [3,11,12] have demonstrated that the outcome in patients with AF was better after the Cox maze III operation than after the limited right-sided atrial maze procedure. Kobayashi et al. [3] reported that the restrictive right-sided maze procedure could not convert AF in any of 3 patients. In this study, among 42 patients who underwent the modified Cox maze III procedure, 38 patients (90.47%) escaped from atrial fibrillation after operation. Ninety-two point one percent of the junctional or sinus restoration group maintained rhythm for 1 year. This result is coherent with the results of previous studies [11,12]. Accordingly, the results of the maze procedure in patients who underwent ASD closure did not differ when compared with other maze procedures. However, there were no significant differences in patient characteristics between the junctional or sinus restoration group and persistent AF group. Atrial remodeling caused by AF itself or progression of underlying heart disease is responsible for persistent AF [13,14]. The so-called "atrial fibrillation begets atrial fibrillation" phenomenon is due to atrial remodeling including electrical, contractile, and structural remodeling [15]. AF alters the expression and function of cardiac ion channels, which shortens the action potential period duration [16-18]. This electrical remodeling contributes to the contractile and structural remodeling of the atrium, which eventually results in persistent AF with a development of functional reentry substrates [13,19]. Wang et al. [20] reported that an aggressive approach to reducing left atrial wall tension significantly improves restoration of sinus rhythm after the maze procedure. This means that structural change of the left atrium directly affects sinus conversion. As atrial disease progresses to irreversible structural changes, AF becomes permanent [13,15]. Long standing ASD can directly cause structural change of the left atrium. In this study, preoperative left atrial size showed no statistically significant relationship to the escape from AF after operation with p=0.105. Furthermore, the cardiothoracic ratio, representing enlarged heart size, showed no statistically significant correlation (p=0.058) to maintaining the sinus rhythm after restoration of sinus rhythm. Unfortunately, none of the variables showed a statistically significant relationship with recurrence of AF after the maze procedure, which could be due to the small sample size. However, reporting the outcomes of the concomitant procedure of ASD closure and the maze procedure is valuable in itself.
1) Limitation of this study
There are a few limitations to the study. First, among different physicians, surgical and postoperative medical management was not uniform. Although the operations were executed in a single center, three surgeons were responsible for the surgery, which caused differences in surgical and postoperative medical management. Second, during the follow-up period, a 12-lead ECG was performed, but 24-hour Holter monitoring was not done. Thus hidden AF arrhythmia expression might have been missed, resulting in more favorable data on the freedom from AF recurrence. Lastly, even though ASD and AF were present in all patients, the number of subjects may have been too small for finding the correlation between ASD and AF due to the diversity of cardiac anomaly. A larger-scale study is thought to be necessary in order to find the correlation independently. There were one hospital death and one non-cardiac-related late death. The hospital death was caused by right heart failure after ASD closure. No deaths related to the maze procedure occurred.
CONCLUSION
The maze procedure is safe and effective in patients who have ASD and AF for restoring sinus rhythm. Since AF is not modified by closure of ASD alone, an intensive procedure to treat the AF should be considered for all of these types of patients. The maze procedure is not an alternative, but rather the main option for controlling AF in patients with ASD.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Murphy JG, Gersh BJ, McGoon MD, et al. Long-term outcome after surgical repair of isolated atrial septal defect. Follow-up at 27 to 32 years. N Engl J Med. 1990;323:1645–1650. doi: 10.1056/NEJM199012133232401. [DOI] [PubMed] [Google Scholar]
- 2.Berger F, Vogel M, Kramer A, et al. Incidence of atrial flutter/fibrillation in adults with atrial septal defect before and after surgery. Ann Thorac Surg. 1999;68:75–78. doi: 10.1016/s0003-4975(99)00478-6. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi J, Yamamoto F, Nakano K, Sasako Y, Kitamura S, Kosakai Y. Maze procedure for atrial fibrillation associated with atrial septal defect. Circulation. 1998;98(19 Suppl):II399–II402. [PubMed] [Google Scholar]
- 4.Perloff JK. Surgical closure of atrial septal defect in adults. N Engl J Med. 1995;333:513–514. doi: 10.1056/NEJM199508243330809. [DOI] [PubMed] [Google Scholar]
- 5.Brandenburg RO, Jr, Holmes DR, Jr, Brandenburg RO, McGoon DC. Clinical follow-up study of paroxysmal supraventricular tachyarrhythmias after operative repair of a secundum type atrial septal defect in adults. Am J Cardiol. 1983;51:273–276. doi: 10.1016/s0002-9149(83)80048-4. [DOI] [PubMed] [Google Scholar]
- 6.Gatzoulis MA, Freeman MA, Siu SC, Webb GD, Harris L. Atrial arrhythmia after surgical closure of atrial septal defects in adults. N Engl J Med. 1999;340:839–846. doi: 10.1056/NEJM199903183401103. [DOI] [PubMed] [Google Scholar]
- 7.Cox JL, Boineau JP, Schuessler RB, Kater KM, Lappas DG. Five-year experience with the maze procedure for atrial fibrillation. Ann Thorac Surg. 1993;56:814–823. doi: 10.1016/0003-4975(93)90338-i. [DOI] [PubMed] [Google Scholar]
- 8.Cox JL, Ad N, Palazzo T, et al. Current status of the Maze procedure for the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg. 2000;12:15–19. doi: 10.1016/s1043-0679(00)70011-6. [DOI] [PubMed] [Google Scholar]
- 9.Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–666. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 10.Moe GK, Rheinboldt WC, Abildskov JA. A computer model of atrial fibrillation. Am Heart J. 1964;67:200–220. doi: 10.1016/0002-8703(64)90371-0. [DOI] [PubMed] [Google Scholar]
- 11.Cox JL, Boineau JP, Schuessler RB, Jaquiss RD, Lappas DG. Modification of the maze procedure for atrial flutter and atrial fibrillation: I. rationale and surgical results. J Thorac Cardiovasc Surg. 1995;110:473–484. doi: 10.1016/S0022-5223(95)70244-X. [DOI] [PubMed] [Google Scholar]
- 12.Cox JL, Jaquiss RD, Schuessler RB, Boineau JP. Modification of the maze procedure for atrial flutter and atrial fibrillation: II. surgical technique of the maze III procedure. J Thorac Cardiovasc Surg. 1995;110:485–495. doi: 10.1016/S0022-5223(95)70245-8. [DOI] [PubMed] [Google Scholar]
- 13.Nattel S, Burstein B, Dobrev D. Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol. 2008;1:62–73. doi: 10.1161/CIRCEP.107.754564. [DOI] [PubMed] [Google Scholar]
- 14.de Vos CB, Pisters R, Nieuwlaat R, et al. Progression from paroxysmal to persistent atrial fibrillation clinical correlates and prognosis. J Am Coll Cardiol. 2010;55:725–731. doi: 10.1016/j.jacc.2009.11.040. [DOI] [PubMed] [Google Scholar]
- 15.de Groot NM, Houben RP, Smeets JL, et al. Electropathological substrate of longstanding persistent atrial fibrillation in patients with structural heart disease: epicardial breakthrough. Circulation. 2010;122:1674–1682. doi: 10.1161/CIRCULATIONAHA.109.910901. [DOI] [PubMed] [Google Scholar]
- 16.Sun H, Chartier D, Leblanc N, Nattel S. Intracellular calcium changes and tachycardia-induced contractile dysfunction in canine atrial myocytes. Cardiovasc Res. 2001;49:751–761. doi: 10.1016/s0008-6363(00)00294-7. [DOI] [PubMed] [Google Scholar]
- 17.Nattel S, Maguy A, Le Bouter S, Yeh YH. Arrhythmogenic ion-channel remodeling in the heart: heart failure, myocardial infarction, and atrial fibrillation. Physiol Rev. 2007;87:425–456. doi: 10.1152/physrev.00014.2006. [DOI] [PubMed] [Google Scholar]
- 18.Nattel S. New ideas about atrial fibrillation 50 years on. Nature. 2002;415:219–226. doi: 10.1038/415219a. [DOI] [PubMed] [Google Scholar]
- 19.Allessie M, Ausma J, Schotten U. Electrical, contractile and structural remodeling during atrial fibrillation. Cardiovasc Res. 2002;54:230–246. doi: 10.1016/s0008-6363(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 20.Wang W, Buehler D, Martland AM, Feng XD, Wang YJ. Left atrial wall tension directly affects the restoration of sinus rhythm after Maze procedure. Eur J Cardiothorac Surg. 2011;40:77–82. doi: 10.1016/j.ejcts.2010.10.022. [DOI] [PubMed] [Google Scholar]