SUMMARY
Osteomas are benign lesions composed of mature compact and/or cancellous bone that grow continuously. Their pathogenesis is unknown. It has been considered to be a neoplasm, a developmental or reactive osteogenic lesion resulting from muscle traction on the periosteum, or due to trauma. Herein, we report an unusual case of giant osteoma of the mandible depressing the lateral pharyngeal wall, interfering with normal respiration during the night. The uniqueness of this case is related to snoring and sleep apnoea symptoms. In fact, he presented to our Department because daytime sleepiness hindered his work, and not for the evident facial swelling. We reported our experience in diagnosis, treatment and follow-up of this uncommon disease. Polysomnography, CT scan and 3-D PAS volume analysis are useful tools to study in detail the aetiology of apnoea and assess outcomes.
KEY WORDS: Obstructive sleep apnoea syndrome, Giant osteoma, Mandible tumours
RIASSUNTO
Gli osteomi dei mascellari sono lesioni ossee costituite da matrice ossea compatta e spongiosa che si accresce in maniera incontrollata. La patogenesi non è ben conosciuta. Queste lesioni sono state variamente considerate come neoplasie, neoformazioni di natura reattiva risultanti da trazioni muscolari sul periostio, o secondarie a traumi. In questo articolo presentiamo un caso atipico di osteoma gigante della mandibola dislocante la parete laterale del faringe e causante un'interferenza con la respirazione notturna del paziente. L'unicità di questo caso è correlata, oltre che alle dimensioni dell'osteoma, alla sintomatologia di presentazione, compatibile con un quadro di sindrome delle apnee ostruttive del sonno. Di seguito riportiamo la nostra esperienza nella diagnosi, trattamento e follow-up di questo caso. Esami polisonnografici TC e morfologico-volumetrici dello spazio aereo posteriore sono stati di utile ausilio per l'identificazione dell'eziologia e la valutazione degli outcomes successivi al trattamento.
Introduction
Osteomas are benign lesions composed of mature compact and/or cancellous bone that grow continuously. Osteomas are histologically characterized by the proliferation of either compact or cancellous bone. They may arise from endosteal or periosteal surfaces and occur as single or multiple lesions with considerable variation in size 1-3. Osteomas are essentially tumours of craniofacial bone, rarely affecting the extragnathic skeleton, although cases of soft tissue osteomas arising within the bulk of skeletal muscles have been reported 4. Their pathogenesis is unknown. It has been considered to be a neoplasm, a developmental or reactive osteogenic lesion resulting from muscle traction on the periosteum, or due to trauma 3-5.
Osteomas exhibit continuous growth rather than growth cessation at adulthood, and this characteristic is the major feature distinguishing them from other bony exostoses such as tori 6 7.
In addition, bony exostoses such as tori, unlike osteomas, have a predilection for specific sites in jawbones 8. Osteomas of the jaws may arise on the surface of the bone as a polypoid or sessile mass (periosteal osteoma), in the medullary bone (endosteal osteoma) or in the soft tissue (extraskeletal osteoma). Osteomas occur more frequently in the mandible than the maxilla, and males are affected more frequently than females with a ratio of about 2:1 9.
Age at presentation has ranged from 14 to 58 years, with a mean of about 29.4 years 9.
Here, we report an unusual case of giant osteoma of the mandible depressing the lateral pharyngeal wall, which interfered with normal respiration during the night causing sleep apnoea. Diagnostic procedures, surgical management, follow-up and the available literature are discussed.
Case report
A 41-year-old Caucasian man was seen with a slowly progressive, painless swelling of the mandible. The patient was a bus driver, and his chief complaint was snoring and daytime sleepiness. He also stated that the swelling had existed since the age of 14 years, when a diffuse bony enlargement of the right side of the mandible was first noted. The patient was in good health with no history of previous facial trauma or contributory medical factors. The continuous growth resulted in dysphagia and facial asymmetry.
On extraoral examination, a hard, subcutaneous, painless mass of the right mandible angle was found. The sensibility of the lower lip was undisturbed. On intraoral inspection, a shift of the right oropharyngeal wall was seen (Fig. 1). Polysomnography, orthopantomography and CT scan were performed.
Fig. 1.
Intraoral inspection showing a swelling of the right oropharyngeal wall.
Polysomnography showed a severe grade of obstructive sleep apnoea syndrome, with an apnoea-hypopnea index (AHI index) of 31. CT showed a diffuse enlargement of the entire right mandible extending caudally to the lateral and medial side. On the surface polypoid bony swellings were seen. The bony mass protruded into the pharynx and displaced the oropharyngeal lateral wall to the contralateral side (Fig. 2). Colonoscopy was performed and Gardner's syndrome was excluded.
Fig. 2.
Axial CT-scan showing diffuse enlargement of the entire right mandible extending to the lateral and medial side.
Because of the symptoms described, facial asymmetry and the progression of the lesion, it was decided to perform an operative correction of the right mandible. Under general anaesthesia with naso-endotracheal intubation, the mandible was approached extraorally using submandibular access (Fig. 3). The submandibular gland was preserved.
Fig. 3.
Intra-operative image showing the large mandibular mass that was approached extraorally using submandibular access.
Using a saw and chisel, the lobular part of the lateral and medial side of the corpus and ascending ramus were resected and the mandible was reshaped (Fig. 4). Histological examination showed a compact, lamellar bony structure diagnosed as osteoid osteoma.
Fig. 4.
Intra-operative image showing the surgical field after resection of medial side and mandible reshaping.
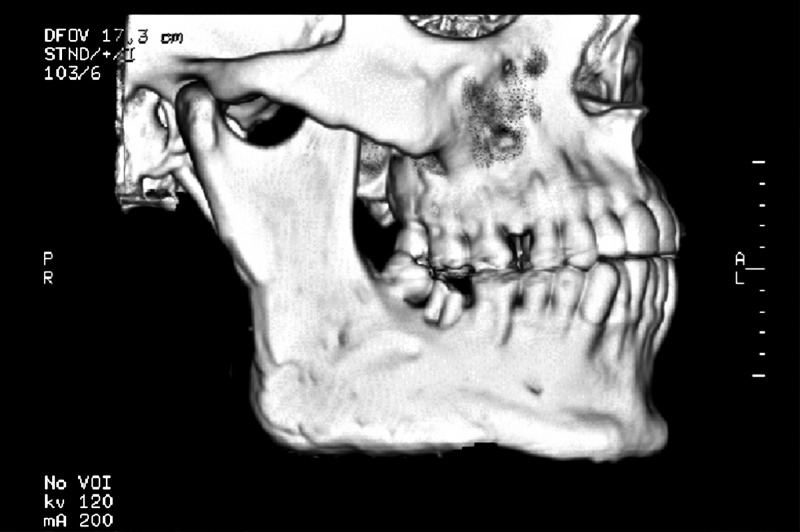
Postoperative three-dimensional CT showed a more acceptable contour of the mandible (Fig. 5).
Fig. 5.
Postoperative three-dimensional CT-scan showing a more acceptable mandible contour.
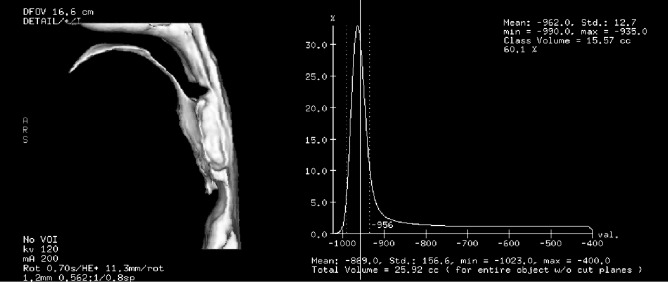
A significant change of posterior airway space (PAS) was achieved leading to normal oropharyngeal anatomy. A 3-dimensional volumetric analysis of PAS was performed using CT data, and showed a normal volume of 25.92 cc (Fig. 6).
Fig. 6.
3-D volumetric analysis of posterior airway space (PAS) performed using 3-D CT data that showed a normal PAS anatomy and an airway volume of 25.92 cc.
Post-operative polysomnography showed an AH index of 8. The following 6 years were uneventful and there was a decline in dysphagia with a satisfying aesthetic result. Furthermore, the patient reported that he no longer snored.
Discussion
Osteoma of the jaws is rare. In instances of mandibular involvement, the most common sites are the angle and lower border of the body 3 4. The lesions generally arise in close proximity to areas of muscle attachment 3, as in this case. They are mostly unilateral, pedunculated, mushroom- like masses. In the present case, the origin of the osteoma could be both central and peripheral as it caused diffuse enlargement of the mandible.
Since osteomas of the skull can be part of Gardner's syndrome, this possibility has to be excluded. This syndrome is based upon the presence of numerous adenomatous colorectal polyps, soft and hard tissue abnormalities, and congenital hypertrophy of the retinal pigment 10.
Osteomas are often noted in the sixth decade, but reports range from 14 to 58 years, with a mean of 29.4 years 9.
Although the aetiology and pathogenesis of osteoma is still unclear, traumatic, congenital, inflammatory or endocrine causes have been considered as possible aetiologic factors 11. Most peripheral osteomas appear to have a very slow growth rate. They often go undetected, since they are usually asymptomatic, unless incidentally noted on a routine radiographic survey 12.
On occasion, peripheral osteomas may expand to the extent that they cause facial asymmetry and functional impairment as in the current case report.
The uniqueness of this case is related to snoring and sleep apnoea symptoms presented by the patient. In fact, he presented to our Department because of daytime sleepiness which hindered his work rather than for facial swelling.
In recent medical literature, to our knowledge, there are no cases of obstructive sleep apnoea syndrome due to mandible osteoma. We also report our experience in diagnosis, treatment and follow-up of this uncommon disease. Polysomnography, CT scan and 3-D PAS volume analysis are useful tools to study in detail the aetiology of apnoea and assess outcomes.
References
- 1.Bodner L, Gatot A, Sion-Vardy N, et al. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998;56:1446–1449. doi: 10.1016/s0278-2391(98)90414-1. [DOI] [PubMed] [Google Scholar]
- 2.Richards HE, Strider JW, Short SG, et al. Large peripheral osteoma arising from the genial tubercle area. Oral Surg Oral Med Oral Pathol. 1986;61:268–271. doi: 10.1016/0030-4220(86)90373-7. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–470. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 4.Longo F, Califano L, Maria G, et al. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001;59:698–700. doi: 10.1053/joms.2001.23408. [DOI] [PubMed] [Google Scholar]
- 5.Schneider LC, Dolinsky HB, Grodjesk JE. Solitary peripheral osteoma of the jaws: report of a case and review of the literature. J Oral Surg. 1980;38:452–455. [PubMed] [Google Scholar]
- 6.Cutilli BJ, Quinn PD. Traumatically induced peripheral osteoma: report of a case. Oral Surg Oral Med Oral Pathol. 1992;73:667–667. doi: 10.1016/0030-4220(92)90006-c. [DOI] [PubMed] [Google Scholar]
- 7.Ertas U, Tozoglu S. Uncommon peripheral osteoma of the mandible: report of two cases. J Contemp Dent Pract. 2003;4:98–104. [PubMed] [Google Scholar]
- 8.Sayan NB, Ucok C, Karasu HA, et al. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–1301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 9.Bosshardt L, Gordon RC, Westerberg M, et al. A recurrent peripheral osteoma of the mandible: report of a case. J Oral Surg. 1971;29:446–450. [PubMed] [Google Scholar]
- 10.Pierce ER, Weisbord T, McKusick VA. Gardner's syndrome: formal genetics and statistical analysis of a large Canadian kindred. Clin Genet. 1970;1:65–80. [Google Scholar]
- 11.Bessho K, Murakami K, Iizuka T, et al. Osteoma in mandibular condyle. Int J Oral Maxillofac Surg. 1987;16:372–372. doi: 10.1016/s0901-5027(87)80162-5. [DOI] [PubMed] [Google Scholar]
- 12.Viswanatha B. Maxillary sinus osteoma: two cases and review of the literature. Acta Otorhinolaryngol Ital. 2012;32:202–205. [PMC free article] [PubMed] [Google Scholar]