Abstract
OBJECTIVE
To develop and validate a risk engine that calculates the risks of macro- and microvascular complications in type 2 diabetes.
RESEARCH DESIGN AND METHODS
We analyzed pooled data from two clinical trials on 1,748 Japanese type 2 diabetic patients without diabetes complications other than mild diabetic retinopathy with a median follow-up of 7.2 years. End points were coronary heart disease (CHD), stroke, noncardiovascular mortality, overt nephropathy defined by persistent proteinuria, and progression of retinopathy. We fit a multistate Cox regression model to derive an algorithm for prediction. The predictive accuracy of the calculated 5-year risks was cross-validated.
RESULTS
Sex, age, HbA1c, years after diagnosis, BMI, systolic blood pressure, non-HDL cholesterol, albumin-to-creatinine ratio, atrial fibrillation, current smoker, and leisure-time physical activity were risk factors for macro- and microvascular complications and were incorporated into the risk engine. The observed-to-predicted (O/P) ratios for each event were between 0.93 and 1.08, and Hosmer-Lemeshow tests showed no significant deviations between observed and predicted events. In contrast, the UK Prospective Diabetes Study (UKPDS) risk engine overestimated CHD risk (O/P ratios: 0.30 for CHD and 0.72 for stroke). C statistics in our Japanese patients were high for CHD, noncardiovascular mortality, and overt nephropathy (0.725, 0.696, and 0.767) but moderate for stroke and progression of retinopathy (0.636 and 0.614). By combining macro- and microvascular risks, the classification of low- and high-risk patients was improved by a net reclassification improvement of 5.7% (P = 0.02).
CONCLUSIONS
The risk engine accurately predicts macro- and microvascular complications and would provide helpful information in risk classification and health economic simulations.
Risk classification for vascular complications is of particular importance in diabetes care, and there is a need for validated diabetes-specific risk engines (1,2). Asian populations account for >60% of the world’s diabetes patients (3,4), but data used for most of the engines specific to diabetes include only a limited number of Asians (5–9). Asian patients with diabetes have several important features. We previously reported that Japanese patients have a markedly low prevalence of obesity and low incidence rates of overt nephropathy and diabetic retinopathy (10–13). Furthermore, the risk factor profiles of diabetes complications are quite different between Japanese and Western subjects with diabetes (14). In cohort studies of multiple ethnic groups, lower incidence rates of cardiovascular disease (CVD) were observed in Asian patients than in whites (15,16). Given the overestimation of risks of coronary heart disease (CHD) and stroke in Chinese patients by the UK Prospective Diabetes Study (UKPDS) risk engine (17,18), risk engines for non-Asian populations may not be transportable to Asian patients. To our knowledge, only the Hong Kong Diabetes Registry (HKDR) has developed risk engines for Asian patients with diabetes (17–20).
Most risk engines have focused on classical cardiovascular risk factors such as control of HbA1c, blood pressure, and lipids (5–9,17–20), but, increasingly, studies have suggested the importance of lifestyle factors. In fact, exercise has been shown to reduce all-cause mortality (21,22) and is encouraged by guidelines for type 2 diabetes (23,24). A recent survey of general practitioners in Germany indicated that those physicians thought that to be useful, risk engines should link estimated risks with appropriate recommendations for lifestyle changes (25). Another concern is the lack of capacity to assess multiple diseases simultaneously (25). However, just combining the results of risk engines specific to each vascular complication may yield biased estimates of absolute risks since it is likely that each engine was developed independently, and a correlation between incidences of vascular complications is not accounted for in the development process.
Data from the 1,748 patients with type 2 diabetes in the Japan Diabetes Complications Study (JDCS) (26) and the Japanese Elderly Diabetes Intervention Trial (J-EDIT) (27) provide an opportunity to develop a comprehensive risk engine for Asian patients with type 2 diabetes. The aim of the current study was therefore to develop and validate an algorithm that separately calculates each risk of the first occurrence for five events: fatal and nonfatal CHD, fatal and nonfatal stroke, noncardiovascular mortality, overt nephropathy, and progression of retinopathy. This was done by fitting a multistate Cox regression model (28), an extension of the Cox model to multiple time-to-event end points, to the pooled data from these trials.
RESEARCH DESIGN AND METHODS
Patients and measurements
Design of the JDCS and the J-EDIT has been described in detail elsewhere (26,27). In the JDCS, 2,033 Japanese type 2 diabetes patients 40–70 years of age whose HbA1c levels were ≥7.0% were randomized to a conventional treatment group and a lifestyle intervention group; throughout the paper, we present the National Glycohemoglobin Standardization Program value of HbA1c calculated as follows: 0.25 + 1.02 × JDC value (29). The latter group received education on lifestyle modification by telephone counseling and at each outpatient clinic visit in addition to usual care. The J-EDIT is a randomized, controlled trial of intensive and conventional treatments for diabetes that registered a total of 1,173 Japanese type 2 diabetes patients 65–85 years of age whose HbA1c levels were ≥8.1%, or ≥7.5% with at least one of the following criteria: BMI ≥25 kg/m2; blood pressure ≥130/85 mmHg; serum total cholesterol ≥200 mg/dL (5.17 mmol/L) or LDL cholesterol ≥120 mg/dL (3.10 mmol/L) in participants without CHD; serum total cholesterol ≥180 mg/dL (4.65 mmol/L) or LDL cholesterol ≥100 mg/dL (2.59 mmol/L) in participants with CHD; triglycerides ≥150 mg/dL (1.68 mmol/L); and HDL cholesterol <40 mg/dL (1.03 mmol/L). The protocols of the JDCS and J-EDIT received approval from the ethical committees of all of the participating institutes, and written informed consent was obtained from all patients before enrollment. The present analysis excluded patients who had any history of angina pectoris, myocardial infarction, stroke, peripheral artery disease, familial hypercholesterolemia (diagnosed clinically by markedly elevated LDL cholesterol levels with enlarged Achilles tendons and/or family history of premature coronary artery disease), type III hyperlipidemia (diagnosed by broad β-band on electrophoresis), nephrotic syndrome, serum creatinine levels >1.3 mg/dL (120 μmol/L), mean values of two spot urine examinations for an albumin excretion rate of 150 mg/g creatinine (17.0 mg/mmol) or more, microscopic hematuria, or other clinical findings indicating other renal diseases, preproliferative and proliferative retinopathy, and major ocular disease (e.g., glaucoma, dense cataract, or history of cataract surgery). Baseline data were collected for demographics, results of clinical examinations, laboratory measurements performed at local laboratories, and lifestyle factors such as dietary content and smoking status determined by self-reported questionnaires. Leisure-time physical activity (LTPA) was also assessed at baseline by a self-administered questionnaire, which was almost identical to that used and validated in the Health Professionals’ Follow-up Study (30). The patients were asked to report their average frequency (times/week) and duration (min/time) of normal walking, brisk walking, jogging, golfing, tennis, swimming, aerobics dancing, cycling, and other miscellaneous exercise as specified by each patient. The duration engaged in each activity in min/time was multiplied by that activity’s typical energy expenditure, expressed in metabolic equivalents (METs), and overall activities were summed to yield a MET/h score per week (31). Data management was conducted by a central data center. Follow-up data were collected through a standardized annual report from each investigator. Non-HDL cholesterol (NHDL-C) levels were calculated by total cholesterol subtracted by HDL cholesterol. LDL cholesterol levels were calculated using the Friedewald formula, that is, NHDL-C subtracted by triglycerides divided by 5 if triglyceride levels are <400 mg/dL (4.48 mmol/L); otherwise, LDL cholesterol levels were treated as missing data.
End points
End points were five time-to-event variables: fatal or nonfatal CHD, fatal or nonfatal stroke, noncardiovascular mortality, overt nephropathy defined by persistent proteinuria, and progression of retinopathy since randomization. The definitions of the events have been described in detail elsewhere (12,13,27,32). In brief, diabetic retinopathy was determined annually by qualified ophthalmologists at each institute using the international diabetic retinopathy and diabetic macular edema disease scales (33) with minor modification: stage 0, no retinopathy; stage 1, hemorrhage and hard exudates; stage 2, soft exudates; stage 3, intraretinal microvascular abnormalities and venous changes, including beading, loop, and duplication; and stage 4, new vessels, vitreous hemorrhage, fibrous proliferation, and retinal detachment. A retinopathy event was progression to stage 3 or 4. A nephropathy event was defined as the development of overt nephropathy (spot urinary albumin excretion >33.9 mg/mmol creatinine in two consecutive samples) (12). Macrovascular events included the occurrence of fatal and nonfatal definite CHD (angina pectoris or myocardial infarction) and fatal and nonfatal stroke. The diagnosis of angina pectoris and myocardial infarction was according to criteria defined by the Multinational Monitoring of Trends and Determinants in Cardiovascular Disease project, and diagnosis of stroke was according to guidelines defined by the Ministry of Health, Labour, and Welfare of Japan (32). Adjudication of end points was performed by central committees comprised of experts in each complication based on additional data such as those obtained by computed tomography or magnetic resonance imaging of the brain or sequential changes in electrocardiograms.
Statistical analysis
The JDCS/J-EDIT (JJ) risk engine calculates each risk of the first occurrence within a user-specified time point for the five events described above. The occurrences of these events are viewed as transitions between disease states and were modeled by a multistate model that follows the Markov renewal process (28). The disease states and transitions assumed in the multistate model are detailed in Supplementary Data. We fit a multistate model using a standard procedure for the stratified Cox regression model. That is, we assumed that baseline intensities for any of the transitions were possibly different but that transition intensities to a disease state share common hazard ratios (HRs) for risk factors. The following risk factors were screened through a backward variable selection with the critical value of P = 0.1: age, sex, HbA1c, years after diagnosis, BMI, systolic blood pressure (SBP), NHDL-C, LDL cholesterol, HDL cholesterol, log-transformed triglycerides, log-transformed urine albumin-to-creatinine ratio (ACR), estimated glomerular filtration rate, atrial fibrillation, smoking status, alcohol intake, and LTPA. BMI was categorized by cutoff points of 18.5 and 25 kg/m2. LTPA was categorized by the cutoff point of 3.8 METs-h/week, which corresponds to the intensity of home activity or conditioning exercise (31). HRs in this model were estimated by maximizing the partial likelihood, and then baseline intensity functions were calculated by the Breslow estimator. Missing data were substituted using the multiple imputation method.
We assessed the predictive accuracy of the 5-year risks based on the JJ risk engine using 10-fold cross-validation, i.e., we performed 10 rounds of cross-validation using different partitions. One round of cross-validation involved randomly partitioning a sample of data on 1,748 patients into complementary subsets, fitting the stratified Cox regression model to one subset of 90% of patients, and validating the model on the remaining subset with the criteria described below. We compared hazards for end points between tertiles of the calculated 5-year risks from the 10-fold cross-validation by the Cox regression. Calibration, namely, how closely the prediction reflected observed events, was assessed for each event by the Hosmer-Lemeshow test and the mean of observed-to-predicted (O/P) ratios, which was calculated as the mean of ratios of the observed-to-expected events across the strata used in the Hosmer-Lemeshow test. Discrimination, the ability to distinguish between those who experienced the event and those who did not, was evaluated using Harrell C statistics, the proportion of all patient pairs in which the predictions of the model and observed events were concordant. Further, we constructed a reclassification table of macro- and microvascular complications (34).
All analyses were conducted by the central data center with the use of SAS software version 9.2 (SAS Institute, Cary, NC). The authors had full access to the data and take responsibility for their integrity. All reported P values for statistical tests are two tailed, and P < 0.05 was taken to indicate statistical significance.
RESULTS
The mean ± SD (range) age and HbA1c level at baseline of the 1,748 Japanese type 2 diabetic patients was 62.1 ± 8.6 (40–84) years and 7.9 ± 1.2 (6.0–15.8)%, respectively, and 49.9% of the subjects were women. Their mean baseline values indicated that the subjects had good control of weight (BMI = 23.2 ± 3.1 kg/m2; waist circumference = 80.3 ± 9.6 cm), blood pressure (SBP = 132.9 ± 16.0 mmHg), and serum cholesterol levels (NHDL-C = 3.78 ± 0.90 mmol/L; LDL cholesterol = 3.16 ± 0.82 mmol/L; HDL cholesterol = 1.43 ± 0.44 mmol/L; triglycerides = 1.39 ± 0.88 mmol/L). Their baseline ACR levels were quite low, with a median ± IQR of 1.8 ± 3.0 mg/mmol, as we excluded those with ACR of 17.0 g/mmol or more. Current smokers and past smokers accounted for 24.4 and 24.0%, respectively, of patients. The median (IQR) LTPA at baseline was 10.5 (1.6–22.5) METs-h/week, and 34.0% of patients had no exercise habit (<3.8 METs-h/week). During the median follow-up of 7.2 years, among the 1,748 subjects, we observed 96 (5.5%) events of fatal or nonfatal CHD, 89 (5.1%) fatal or nonfatal strokes, 71 (4.1%) overt nephropathies defined by persistent proteinuria, and 64 (3.7%) noncardiovascular deaths. Of the 1,297 patients without retinopathy at baseline, 415 (32.0%) developed retinopathy. Of the 866 patients who had retinopathy or developed retinopathy after baseline, 113 (13.0%) had progression to retinopathy of stage 3 or 4.
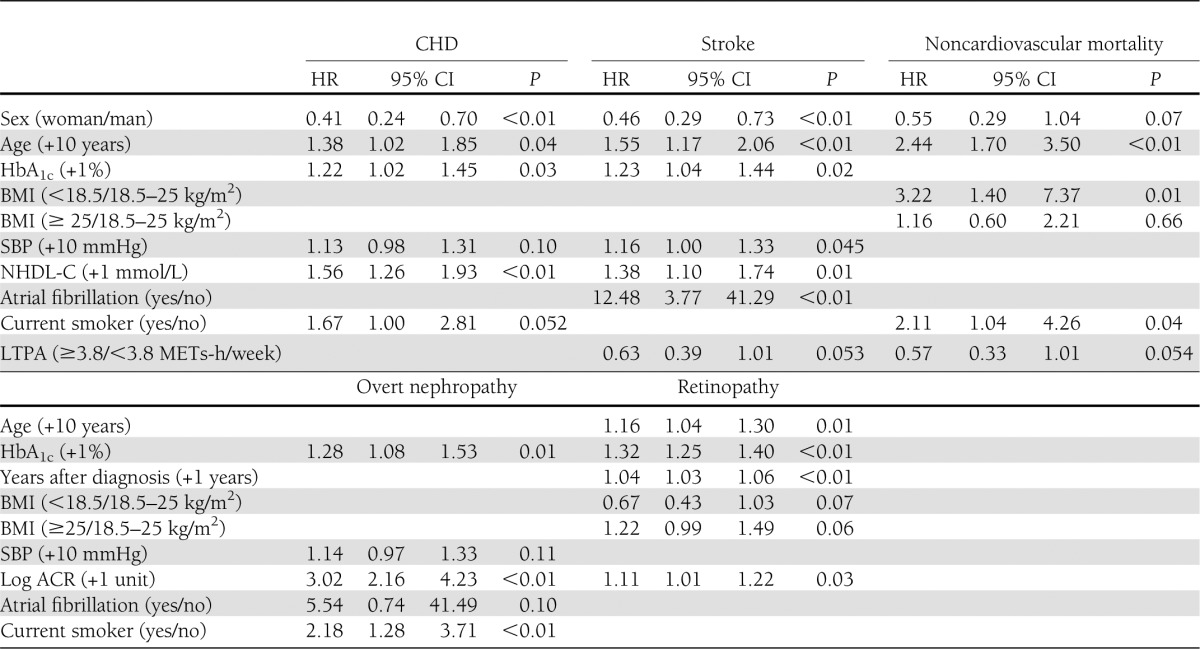
The backward variable selection procedure identified 11 baseline risk factors for macro- and microvascular complications and noncardiovascular mortality. Table 1 shows the HRs, 95% CIs, and P values for these risk factors. Significant modifiable risk factors were HbA1c and NHDL-C for CHD, HbA1c, SBP, and NHDL-C for stroke, BMI <18.5 kg/m2 and being a current smoker for noncardiovascular mortality, HbA1c and being a current smoker for overt nephropathy, and HbA1c for retinopathy. Having an exercise habit was associated with reduced risks of stroke and mortality, although with only borderline statistical significance. All of the risk factors that were retained through the variable selection procedure were incorporated into the JJ risk engine. The algorithm of the JJ risk engine is described in Supplementary Data.
Table 1.
HRs of risk factors incorporated in the best-fitting multistate Cox regression model
The performance of the JJ risk engine was evaluated by several validation criteria. Tertile Cox regression showed that the 5-year risks calculated by the JJ risk engine effectively classified populations at low and high risk for each complication. The HRs (95% CI) of the second and third tertiles compared with the first tertile were 2.09 (1.07–4.09) and 5.22 (2.84–9.58) for CHD; 1.78 (0.96–3.30) and 3.32 (1.86–5.92) for stroke; 2.14 (1.09–4.18) and 3.17 (1.65–6.09) for noncardiovascular mortality; 1.54 (0.55–4.34) and 10.59 (4.56–24.59) for overt nephropathy; and 1.18 (0.58–2.40) and 2.56 (1.37–4.81) for progression of retinopathy.
Table 2 shows the predictive accuracy of the JJ risk engine regarding calibration and discrimination. The O/P ratios for each complication, including noncardiovascular mortality, ranged between 0.93 and 1.08, and Hosmer-Lemeshow tests did not show any significant deviations between the observed and predicted events. In contrast, the UKPDS risk engine (5,6) overestimated CHD risk in Japanese patients (O/P ratios [Hosmer-Lemeshow P]: 0.30 [P < 0.01] for CHD and 0.72 [P = 0.54] for stroke) (Table 2). Discrimination according to C statistics was high for CHD, noncardiovascular mortality, and overt nephropathy (0.696–0.767) but was moderate for stroke and progression of retinopathy (0.636 and 0.614).
Table 2.
Predictive accuracy of the JJ risk engine in 1,748 patients
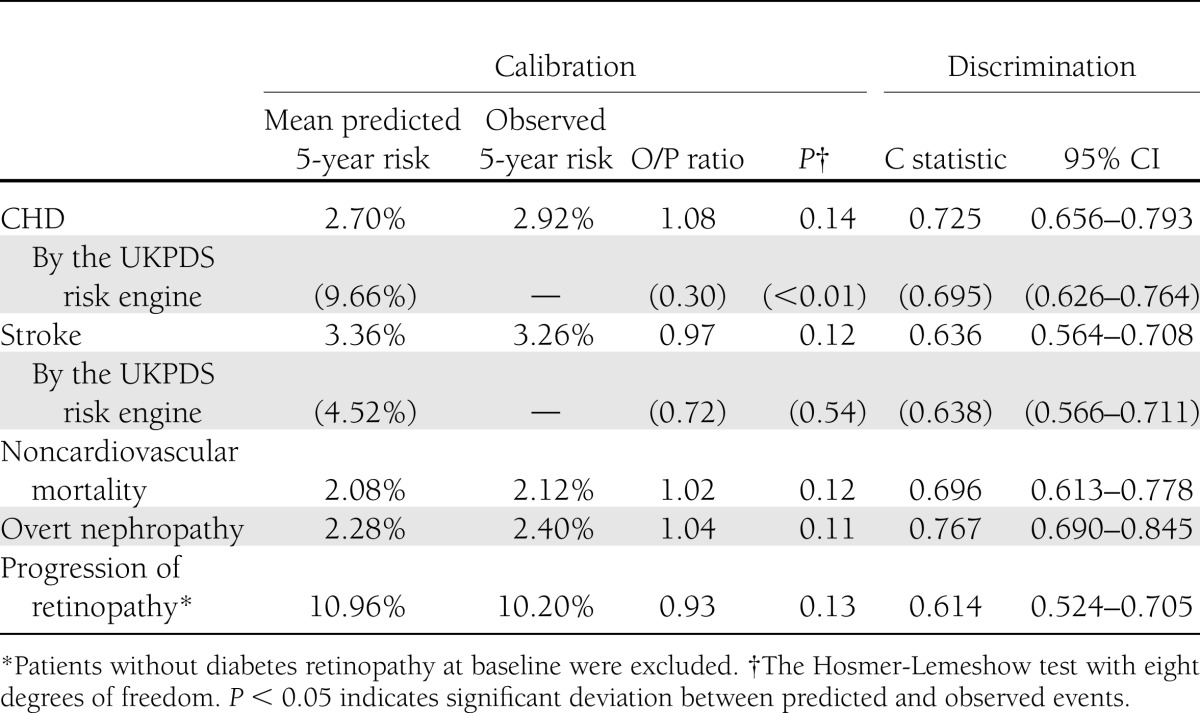
Table 3 compares risk classification by the 5-year risk of macrovascular disease based on the JJ risk engine with that based on the UKPDS risk engine. By the UKPDS risk engine, more than half of patients had a macrovascular risk of 10% or more (249 of the 376 cases and 697 of the 1,372 noncases), as expected by the tendency of overestimation The sensitivity and specificity of the UKPDS risk engine with a cutoff value of 10% risk were 66.2 and 49.2%, respectively. In contrast, only 101 of the 376 cases (26.9%) who developed any of the events had a macrovascular risk of 10% or more based on the JJ risk engine, yielding sensitivity of 26.9% and specificity of 89.1%.
Table 3.
Risk classification of the 1,748 patients according to 5-year risks of macrovascular disease based on the JJ risk engine and the UKPDS risk engine
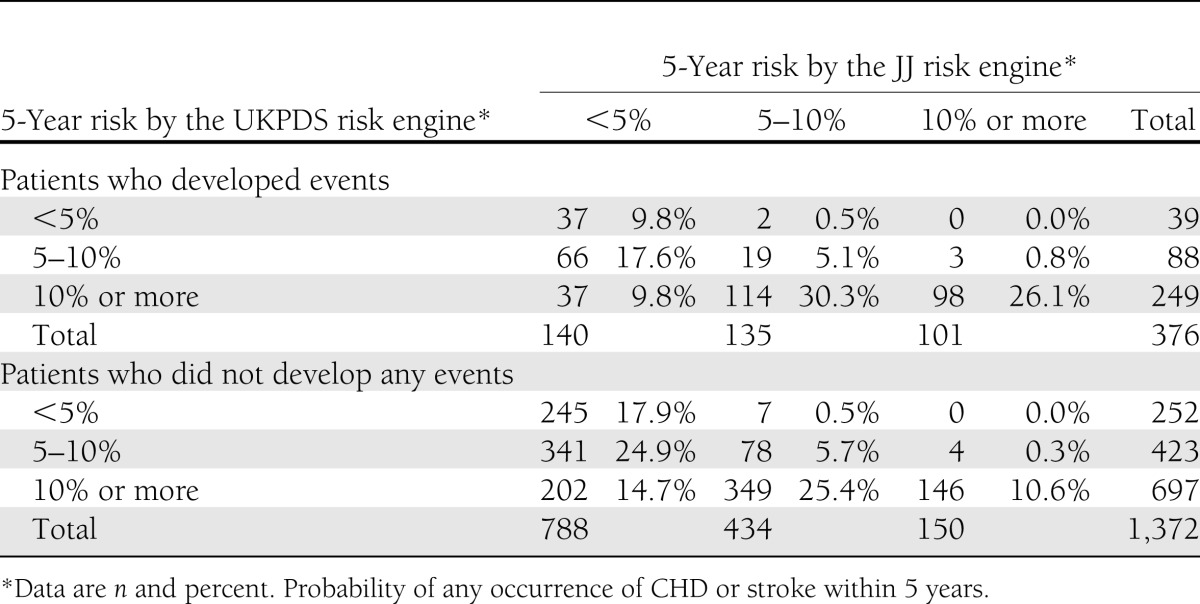
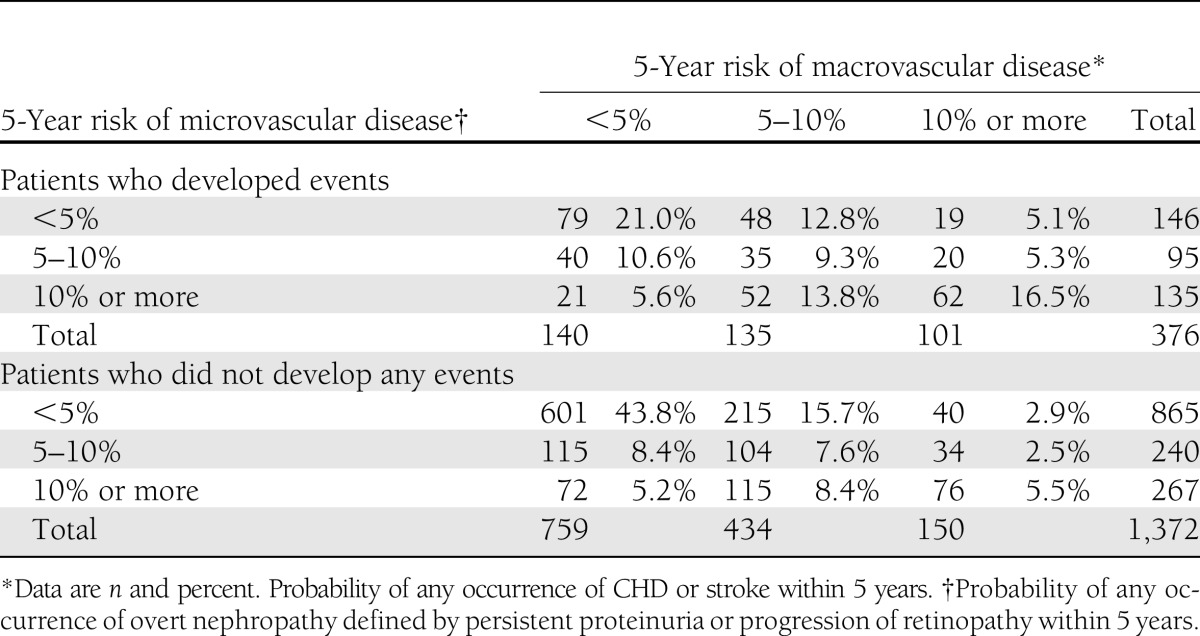
Table 4 shows how the combination of 5-year risks of macro- and microvascular complications based on the JJ risk engine classified low-risk and high-risk patients. If we combined macro- and microvascular risks, 73 of 376 cases (19.4%) and 187 of 1,372 noncases (13.6%) were newly classified as a high-risk population, and sensitivity increased up to 46.3% while specificity was maintained at 75.4%. The net reclassification improvement (total of sensitivity and specificity in this case) was improved by 5.7% (P = 0.02).
Table 4.
Risk classification of the 1,748 patients according to 5-year risks of macro- and microvascular diseases based on the JJ risk engine
To illustrate the use of the JJ risk engine, consider two Japanese men 60 years of age with simple diabetic retinopathy and without atrial fibrillation who do not have smoking and exercise habits. The clinical characteristics of both patients are HbA1c = 9%, duration of diabetes = 20 years, BMI = 23 kg/m2, NHDL-C = 3.88 mmol/L, and ACR = 6.79 mg/mmol creatinine. The SBP of one patient is 120 mmHg. His leading risk is estimated to be the progression of retinopathy (5-year risk, 15.5%), and his macrovascular risks are moderate (9.2% for CHD and 9.6% for stroke). His 5-year risks of noncardiovascular death and overt nephropathy are low (4.8 and 3.7%, respectively). The other patient has an SBP of 180 mmHg. His leading risks are macrovascular diseases (16.1% for CHD and 17.6% for stroke), and his microvascular risks are moderate (7.8% for nephropathy and 13.6% for retinopathy). The risk of noncardiovascular mortality is estimated to be 4.0%.
CONCLUSIONS
In this study, we developed a novel risk engine that integrates modifiable lifestyle and clinical risk factors, including HbA1c, BMI, SBP, NHDL-C, current smoking, and LTPA into the risks of a first occurrence of macro- and microvascular complications. We confirmed that the risk engine performed reasonably well and that combining macro- and microvascular risks improved the classification of low-risk and high-risk patients by a net reclassification improvement of 5.7%. In contrast, the UKPDS risk engine overestimated CHD risk, and this tendency is consistent with a previous report in Asian patients (18). A web application for the JJ risk engine, which works in both Windows and Macintosh environments, is available at http://www.biostatistics.jp/prediction/jjre.
With the advent of modern therapeutics, especially hypoglycemic and antihypertensive agents, the early identification of high-risk patients is an appealing strategy (35). A novelty of the JJ risk engine is that it allows risk classification based on the risk not only of CVD but also of renal and eye diseases. Although the prevalence of micro- or macroalbuminuria in Asian hypertensive diabetes is alarmingly high (36), most of the progression to overt nephropathy occurs in a small fraction of patients with elevated HbA1c and SBP values and a smoking habit (12). In this study, patients in the fourth quartile of the calculated risk developed overt nephropathy at a rate 10 times greater than those in the first quartile. Most risk engines are specific to CVD; however, greater emphasis on the risk of microvascular diseases should be placed when assessing risk among diabetic patients given that diabetic nephropathy and retinopathy are major causes of ESRD and blindness, respectively. Combining macro- and microvascular risks resulted in the net reclassification improvement of 5.7% (P = 0.02) and a sensitivity and specificity of 46.3 and 75.4%, respectively; only 16.5% of cases were classified as the high-risk population for macro- and microvascular diseases and only 43.8% of noncases were in the low-risk population (Table 4). Thus, the discriminatory power of the JJ risk engine was only moderate, despite the statistically significant improvement in prediction, and exploring novel risk factors would be of particular importance for more accurate risk classification.
The JJ risk engine shares features similar to those with previously developed risk engines. The predictors of CHD are the same as in the UKPDS risk engine (5) except for the inclusion of NHDL-C instead of the total cholesterol–to-HDL cholesterol ratio. Donnan et al. (7) added diabetes duration, treated hypertension, height, and two interaction terms into their model, and the risk equation of the HKDR includes diabetes duration, estimated glomerular filtration rate, and ACR additionally but does not use HbA1c (18). A recent cohort study in Japan also suggested that the progression of the albuminuria stage is a risk factor of CVD (37). In contrast, log ACR was not associated with CHD or stroke in our study. This discordant observation would be attributable to the exclusion of low microalbuminuria in our study. The elevation of ACR within a range of normoalbuminuria may not lead to an increase in the risk of CVD. We also found that the UKPDS risk engine overestimated CHD risk (Table 2) and the C statistic of the JJ risk engine (0.725) was slightly higher than that of the risk equation of the HKDR (0.704) (18), indicating that the JJ risk engine may outperform the previously developed risk engines for the prediction of CHD. For the prediction of stroke, we did not identify smoking status and years after diagnosis as predictors, which are included in the UKPDS risk engine (6). The risk equation from the Swedish National Diabetes Register incorporates the use of antihypertensive drugs and lipid-lowering drugs as predictors (9). However, medical therapies are not considered in the current analysis, since the effects of medications on vascular complications were likely to be confounded by other clinical factors. In contrast to CHD, the C statistic of the JJ risk engine (0.636) was similar to the UKPDS risk engine (0.638) and lower than the risk equation of the HKDR (0.749) (17). With regard to lifestyle factors, we identified LTPA as a risk factor for stroke and noncardiovascular mortality, although the statistical significance was borderline. On the other hand, BMI, which has been recognized as one of the most important risk factors in the deterioration of type 2 diabetes, was not associated with CVD. We previously reported that the BMI of Japanese patients is much lower than that of white patients, although in those reports, other patient characteristics were similar in terms of age, HbA1c, and daily energy intake (10,11). Our findings run contrary to the results of studies of white patients, but data on diet in diabetic patients are sparse, particularly in Asia. In this study, the contribution of lifestyle factors to the risk assessment appears to be limited, and the associations between lifestyle and diabetes complications are worthy of further research.
One important feature of this study is that we analyzed pooled data from two nationwide clinical trials in Japan. The end points were defined similarly in both trials and follow-up was performed by diabetes specialists, ensuring data of relatively high quality. Patients generally had fair or good glycemic, weight, blood pressure, and lipid control. The major difference between the two trials was eligible age, i.e., age between 40 and 70 years in the JDCS and age between 65 and 85 years in the J-EDIT. Prior to pooling the datasets, we compared important clinical factors between patients in the two trials and found no notable differences except for age; therefore, pooling of the datasets was considered to be valid. Consequently, the study population in the present analysis included subjects spanning several decades, i.e., those from 40 to 84 years. This can be expected to enhance the generalizability of the algorithm.
Statistical modeling can be much more complex if we handle multiple events simultaneously. To the best of our knowledge, this is the first study that applies a multistate model to the construction of a risk engine. It is notable that these events are not inherently independent and the JJ risk engine calculates each probability of the first occurrence for five events. Thus, if the risk of an event (e.g., overt nephropathy) was increased by a risk factor (e.g., log ACR), the probability of the first occurrence of other events (e.g., stroke) can decrease theoretically even if there are no direct associations with the risk factor.
Several limitations warrant mention. First, transportability of prognostic information is critical, but in this study we evaluated only the internal validity. Thus, external validation is required in other populations. Second, updating the algorithm by long-term follow-up data or pooled analysis with other studies in Asia is desirable given that the size of our cohort is relatively small and the observed events of CVD and overt nephropathy in this population were relatively few. Third, we included angina pectoris and transient ischemic attack as components of the cardiovascular events, although they are soft end points. Consequently, the JJ risk engine would provide macrovascular risks higher than those by other risk engines based on only hard cardiovascular events. Fourth, data on peripheral arterial disease and hemoglobin levels were not available. These factors were included as inputs into the HKDR all-cause mortality risk score (19), and peripheral arterial disease is a clinically relevant cardiovascular outcome. Fifth, the use of aspirin, which might increase the risk of hemorrhagic stroke, was not investigated. Finally, we defined overt nephropathy as the presence of persistent proteinuria, since an elevated urinary albumin excretion due to nondiabetic renal lesions or conditions is not rare.
In conclusion, the risk engine allowed accurate and comprehensive risk assessment of macro- and microvascular complications, although external validation is required in other populations. The calculated absolute risks of vascular complications can be used in risk classification for individual patients, health economic simulations, and estimation of the burden of the disease.
Acknowledgments
This work was funded by the Ministry of Health, Labour, and Welfare of Japan. The sponsor had no role in the design or conduct of the study.
No potential conflicts of interest relevant to this article were reported.
Sh.T., Sa.T., and Y.O. performed statistical analysis and wrote the manuscript. S.I. managed data. H.Y., S.K., Y.A., N.Y., A.A., H.I., and H.S. planned and conducted the JDCS and the J-EDIT. H.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the many diabetologists and patients at the 59 participating institutes of the JDCS and 42 participating institutes of the J-EDIT throughout Japan. The authors thank Satomi Fukuya and Yasuko Maruyama (University of Tsukuba Institute of Clinical Medicine) for their excellent secretarial assistance.
Footnotes
Clinical trial reg. no. UMIN CTR C000000222 for the Japan Diabetes Complications Study and UMIN 000000890 for the Japanese Elderly Diabetes Intervention Trial, www.umin.ac.jp/ctr/.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-0958/-/DC1.
A complete list of the primary investigators and committee members can be found in the Supplementary Data online.
References
- 1.Coleman RL, Stevens RJ, Retnakaran R, Holman RR. Framingham, SCORE, and DECODE risk equations do not provide reliable cardiovascular risk estimates in type 2 diabetes. Diabetes Care 2007;30:1292–1293 [DOI] [PubMed] [Google Scholar]
- 2.Chamnan P, Simmons RK, Sharp SJ, Griffin SJ, Wareham NJP. Cardiovascular risk assessment scores for people with diabetes: a systematic review. Diabetologia 2009;52:2001–2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–1053 [DOI] [PubMed] [Google Scholar]
- 4.Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–2140 [DOI] [PubMed] [Google Scholar]
- 5.Stevens RJ, Kothari V, Adler AI, Stratton IM, United Kingdom Prospective Diabetes Study (UKPDS) Group The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clin Sci (Lond) 2001;101:671–679 [PubMed] [Google Scholar]
- 6.Kothari V, Stevens RJ, Adler AI, et al. UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke 2002;33:1776–1781 [DOI] [PubMed] [Google Scholar]
- 7.Donnan PT, Donnelly L, New JP, Morris AD. Derivation and validation of a prediction score for major coronary heart disease events in a U.K. type 2 diabetic population. Diabetes Care 2006;29:1231–1236 [DOI] [PubMed] [Google Scholar]
- 8.Balkau B, Hu G, Qiao Q, Tuomilehto J, Borch-Johnsen K, Pyörälä K, DECODE Study Group. European Diabetes Epidemiology Group Prediction of the risk of cardiovascular mortality using a score that includes glucose as a risk factor. Diabetologia 2004;47:2118–2128 [DOI] [PubMed] [Google Scholar]
- 9.Cederholm J, Eeg-Olofsson K, Eliasson B, Zethelius B, Nilsson PM, Gudbjörnsdottir S, Swedish National Diabetes Register Risk prediction of cardiovascular disease in type 2 diabetes: a risk equation from the Swedish National Diabetes Register. Diabetes Care 2008;31:2038–2043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sone H, Ito H, Ohashi Y, Akanuma Y, Yamada N, Japan Diabetes Complication Study Group Obesity and type 2 diabetes in Japanese patients. Lancet 2003;361:85. [DOI] [PubMed] [Google Scholar]
- 11.Sone H, Yoshimura Y, Ito H, Ohashi Y, Yamada N, Japan Diabetes Complications Study Group Energy intake and obesity in Japanese patients with type 2 diabetes. Lancet 2004;363:248–249 [DOI] [PubMed] [Google Scholar]
- 12.Katayama S, Moriya T, Tanaka S, et al. Japan Diabetes Complications Study Group Low transition rate from normo- and low microalbuminuria to proteinuria in Japanese type 2 diabetic individuals: the Japan Diabetes Complications Study (JDCS). Diabetologia 2011;54:1025–1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawasaki R, Tanaka S, Tanaka S, et al. Japan Diabetes Complications Study Group Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan Diabetes Complications Study (JDCS). Diabetologia 2011;54:2288–2294 [DOI] [PubMed] [Google Scholar]
- 14.Sone H, Mizuno S, Yamada N. Vascular risk factors and diabetic neuropathy. N Engl J Med 2005;352:1925–1927; author reply 1925–1927 [PubMed] [Google Scholar]
- 15.Lee ET, Keen H, Bennett PH, Fuller JH, Lu M. Follow-up of the WHO Multinational Study of Vascular Disease in Diabetes: general description and morbidity. Diabetologia 2001;44(Suppl. 2):S3–S13 [DOI] [PubMed] [Google Scholar]
- 16.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA 2002;287:2519–2527 [DOI] [PubMed] [Google Scholar]
- 17.Yang X, So WY, Kong AP, et al. Development and validation of stroke risk equation for Hong Kong Chinese patients with type 2 diabetes: the Hong Kong Diabetes Registry. Diabetes Care 2007;30:65–70 [DOI] [PubMed] [Google Scholar]
- 18.Yang X, So WY, Kong AP, et al. Development and validation of a total coronary heart disease risk score in type 2 diabetes mellitus. Am J Cardiol 2008;101:596–601 [DOI] [PubMed] [Google Scholar]
- 19.Yang X, So WY, Tong PC, et al. Hong Kong Diabetes Registry Development and validation of an all-cause mortality risk score in type 2 diabetes. Arch Intern Med 2008;168:451–457 [DOI] [PubMed] [Google Scholar]
- 20.Yang X, Ma RC, So WY, et al. Development and validation of a risk score for hospitalization for heart failure in patients with type 2 diabetes mellitus. Cardiovasc Diabetol 2008;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu G, Jousilahti P, Barengo NC, Qiao Q, Lakka TA, Tuomilehto J. Physical activity, cardiovascular risk factors, and mortality among Finnish adults with diabetes. Diabetes Care 2005;28:799–805 [DOI] [PubMed] [Google Scholar]
- 22.Kokkinos P, Myers J, Nylen E, et al. Exercise capacity and all-cause mortality in African American and Caucasian men with type 2 diabetes. Diabetes Care 2009;32:623–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marwick TH, Hordern MD, Miller T, et al. Council on Clinical Cardiology, American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee. Council on Cardiovascular Disease in the Young. Council on Cardiovascular Nursing. Council on Nutrition, Physical Activity, and Metabolism. Interdisciplinary Council on Quality of Care and Outcomes Research Exercise training for type 2 diabetes mellitus: impact on cardiovascular risk: a scientific statement from the American Heart Association. Circulation 2009;119:3244–3262 [DOI] [PubMed] [Google Scholar]
- 24.Colberg SR, Sigal RJ, Fernhall B, et al. American College of Sports Medicine. American Diabetes Association Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care 2010;33:e147–e167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Müller-Riemenschneider F, Holmberg C, Rieckmann N, et al. Barriers to routine risk-score use for healthy primary care patients: survey and qualitative study. Arch Intern Med 2010;170:719–724 [DOI] [PubMed] [Google Scholar]
- 26.Sone H, Tanaka S, Iimuro S, et al. Japan Diabetes Complications Study Group Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial (the Japan Diabetes Complications Study). Diabetologia 2010;53:419–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Araki A, Iimuro S, Sakurai T, et al. Japanese Elderly Diabetes Intervention Trial Study Group Long-term multiple risk factor interventions in Japanese elderly diabetic patients: the Japanese Elderly Diabetes Intervention Trial—study design, baseline characteristics and effects of intervention. Geriatr Gerontol Int 2012;12(Suppl. 1):7–17 [DOI] [PubMed] [Google Scholar]
- 28.Andersen PK, Keiding N. Multi-state models for event history analysis. Stat Methods Med Res 2002;11:91–115 [DOI] [PubMed] [Google Scholar]
- 29.The Committee on the Standardization of Diabetes Mellitus-Related Laboratory Testing of Japan Diabetes Society. International clinical harmonization of hemoglobin A1c in Japan: from JDS to NGSP values [Internet]. Available from http://www.jds.or.jp/jds_or_jp0/uploads/photos/813.pdf Accessed 31 January 2012
- 30.Tanasescu M, Leitzmann MF, Rimm EB, Hu FB. Physical activity in relation to cardiovascular disease and total mortality among men with type 2 diabetes. Circulation 2003;107:2435–2439 [DOI] [PubMed] [Google Scholar]
- 31.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc 2011;43:1575–1581 [DOI] [PubMed] [Google Scholar]
- 32.Sone H, Tanaka S, Tanaka S, et al. Japan Diabetes Complications Study Group Serum level of triglycerides is a potent risk factor comparable to LDL cholesterol for coronary heart disease in Japanese patients with type 2 diabetes: subanalysis of the Japan Diabetes Complications Study (JDCS). J Clin Endocrinol Metab 2011;96:3448–3456 [DOI] [PubMed] [Google Scholar]
- 33.Wilkinson CP, Ferris FL, 3rd, Klein RE, et al. Global Diabetic Retinopathy Project Group Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003;110:1677–1682 [DOI] [PubMed] [Google Scholar]
- 34.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 2008;27:157–172; discussion 207–212 [DOI] [PubMed] [Google Scholar]
- 35.National Institute for Clinical Excellence. Inherited Clinical Guideline H. Management of type 2 diabetes: management of blood pressure and blood lipids. London: National Institute for Clinical Excellence [article online], 2002. Available from http://www.nice.org.uk/nicemedia/pdf/NICE_INHERITEd_Hv8.pdf Accessed at 25 April 2011
- 36.Wu AY, Kong NC, de Leon FA, et al. An alarmingly high prevalence of diabetic nephropathy in Asian type 2 diabetic patients: the MicroAlbuminuria Prevalence (MAP) Study. Diabetologia 2005;48:17–26 [DOI] [PubMed] [Google Scholar]
- 37.Yokoyama H, Araki S, Haneda M, et al. Japan Diabetes Clinical Data Management Study Group Chronic kidney disease categories and renal-cardiovascular outcomes in type 2 diabetes without prevalent cardiovascular disease: a prospective cohort study (JDDM25). Diabetologia 2012;55:1911–1918 [DOI] [PubMed] [Google Scholar]


