Abstract
OBJECTIVE
Hypoglycemia is associated with increased mortality in hospitalized patients. We investigated the relationship between spontaneous hypoglycemia versus insulin-associated hypoglycemia and mortality in hospitalized patients.
RESEARCH DESIGN AND METHODS
Data for this retrospective cohort study were obtained from electronic databases of patients admitted between 1 April 2008 and 30 November 2010. Patients with one or more blood glucose values ≤50 mg/dL on point-of-care glucose testing were considered hypoglycemic. Patients treated with insulin were assumed to have insulin-associated hypoglycemia. Age-, sex-, and race-matched patients with all blood glucose values >70 mg/dL were selected as controls. The Charlson comorbidity index (CCI) was used to control for severity of illness.
RESULTS
There were four groups: 1) noninsulin-treated hypoglycemia (NTH) (n = 135), 2) insulin-treated hypoglycemia (ITH) (n = 961), 3) noninsulin-treated control (NTC) (n = 1,058), and 4) insulin-treated control (ITC) (n = 736). Mortality was higher in the ITH group compared with the ITC group (20.3 vs. 4.5%, P < 0.0001), with a relatively higher CCI (1.8 vs. 1.5%, P < 0.0001), but much higher in the NTH group compared with the NTC group (34.5 vs. 1.1%, P < 0.0001), with much higher CCI (2.4 vs. 1.1%, P < 0.0001). Mortality was higher in the NTH group compared with the ITH group (P < 0.0001) but lower in the NTC group compared with the ITC group (P < 0.0001). After controlling for age, sex, CCI, and admission to the intensive care unit, insulin treatment was associated with a lower mortality among the hypoglycemic patients; hazard ratio of death in the ITH group relative to the NTH group was 0.34 (95% CI 0.25–0.47, P < 0.0001).
CONCLUSIONS
Insulin-associated and spontaneous hypoglycemia are associated with increased mortality among hospitalized patients.
Hypoglycemia among hospitalized patients is a common problem. In previous studies, 7–10% of the patients admitted to the hospital were reported to have at least one episode of hypoglycemia (1,2). Most of these hypoglycemic episodes were treatment related, but spontaneous hypoglycemia is also known to be frequent (1). Hypoglycemia is associated with increased mortality (2–6). However, a cause and effect relationship between hypoglycemia and mortality has not been established (5). Patients with more severe illnesses are more likely to develop hypoglycemia irrespective of insulin treatment and have a higher risk of mortality (3,5). However, insulin-induced hypoglycemia may have different consequences than spontaneous hypoglycemia. A study of patients with acute myocardial infarction suggested that iatrogenic hypoglycemia is associated with lower mortality than spontaneous hypoglycemia (7). Another study of patients admitted to the general wards showed that drug-induced hypoglycemia was not associated with increased mortality and the association between spontaneous hypoglycemia and mortality disappeared after adjustment for comorbidities (1). We investigated the association between spontaneous hypoglycemia versus insulin-associated hypoglycemia and mortality among all hospitalized patients.
RESEARCH DESIGN AND METHODS
Data for this retrospective cohort study were obtained from the Research Patient Database Registry (RPDR) and point-of-care glucose meter download data for patients admitted to the Brigham and Women’s Hospital between 1 April 2008 and 30 November 2010. The RPDR is a data warehouse that serves as a central clinical data repository for participating hospitals and clinics within the Partners HealthCare system, an integrated health care delivery network in eastern Massachusetts that includes Massachusetts General Hospital and Brigham and Women’s Hospital. Partners Healthcare Human Research Committee approved the protocol and waived the requirement for written informed consent.
Hypoglycemic group
Hospitalized patients with one or more blood glucose values ≤50 mg/dL on point-of-care blood glucose testing were included in this study. The exact date and time of hypoglycemia were extracted from the point-of-care glucose meter download data.
Detailed demographic data and hospitalization records that included all diagnoses, some laboratory reports, and prescribed medications were obtained from the RPDR. The date of hypoglycemia was matched to the hospitalization period. If multiple hospitalizations were present for a particular patient, the last hospitalization was used in the analysis. If a patient had suffered more than one hypoglycemic episode during hospitalization, the first episode of hypoglycemia was considered the key event. When insulin was used during hospitalization, hypoglycemia was assumed to be insulin related. When no insulin was used, hypoglycemia was assumed to be of spontaneous origin. Patients receiving oral antidiabetic agents during hospitalization were excluded. Mortality data during hospitalization were obtained, and the time period between hypoglycemia and death was noted.
Control group
A control group of patients admitted during the same time period (1 April 2008 to 30 November 2010) with no blood glucose value <70 mg/dL on point-of-care blood glucose testing was selected. For each sex/race/age decade characteristic combination among hypoglycemic patients, we obtained matched controls with the same characteristic combination, aiming for the number of controls to be twice the number of cases for each characteristic combination. The resulting number of controls was less than twice the number of hypoglycemic patients due to limited availability. If there were multiple hospitalizations for a control patient, the last hospitalization was used in the analysis. Insulin usage and death during hospitalization were noted.
Statistical analysis
The primary outcome was death during the hospital stay. Data were summarized as numbers with percentage or means and SD. The Charlson comorbidity index (CCI) was calculated from the ICD-9 codes (8). Patient characteristics were compared between groups using Wilcoxon rank sum test, χ2 test, or logistic regression for mortality. Groups were compared in terms of the time from hypoglycemia to death during hospitalization or censoring at discharge using the log-rank test and Kaplan-Meier plot. Cox regression was used to assess the significance of single and simultaneous multiple predictors of death, with hazard ratios (HRs) and 95% CIs, accounting for intracluster dependence resulting from the method of selecting the control group (9). Potential confounders of group comparisons included the CCI and admission to the intensive care unit (ICU), insulin, age, sex, and race. The retention of covariates in the final model depended on the association with mortality (P < 0.10). Statistical analyses were performed using SAS version 9.2 (Cary, NC).
RESULTS
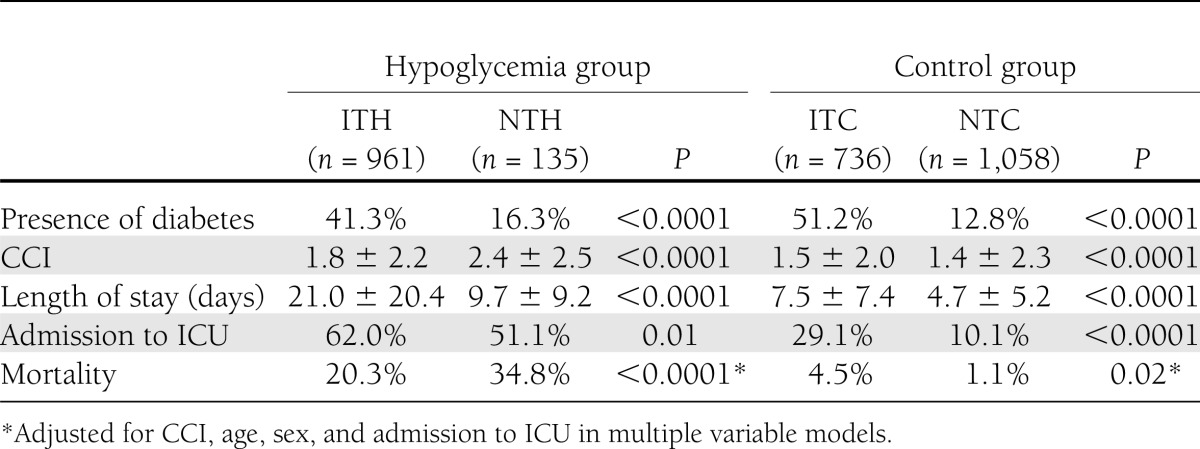
A total of 2,890 patients were included in this study and divided into four groups: 1) noninsulin-treated hypoglycemia (NTH) (n = 135), 2) insulin-treated hypoglycemia (ITH) (n = 961), 3) noninsulin-treated control (NTC) (n = 1,058), and 4) insulin-treated control (ITC) (n = 736). Hypoglycemic patients were more likely to have diabetes and receive insulin treatment. They were sicker, as indicated by higher CCI and more admissions to the ICU. Mortality among hypoglycemic patients was nine times higher than mortality among control patients (22.1 vs. 2.5%; P < 0.0001). Differences between insulin-treated versus noninsulin-treated groups are shown in Table 1. Insulin-treated hypoglycemic patients as well as the ITC patients were older and more likely to have a diagnosis of diabetes. Patients in the NTH group were sicker with a higher CCI and more admissions to the ICU as compared with the ITH group, a relation that was reversed in the control group, with NTC patients having a lower CCI than ITC patients. Mortality during hospitalization was higher in the NTH group compared with the ITH group (P < 0.0001) but lower in the NTC group compared with the ITC group (P < 0.0001). Mortality was higher in the ITH group compared with the ITC group (20.3 vs. 4.5%, P < 0.0001), with a relatively small difference in the CCI (1.8 vs. 1.5%, P < 0.0001), but much higher in the NTH group compared with the NTC group (34.5 vs. 1.1%, P < 0.0001), with much higher CCI (2.4 vs. 1.1%, P < 0.0001). Mortality during hospitalization was highest in the NTH group followed by the ITH and ITC groups.
Table 1.
Patient characteristics and group comparisons
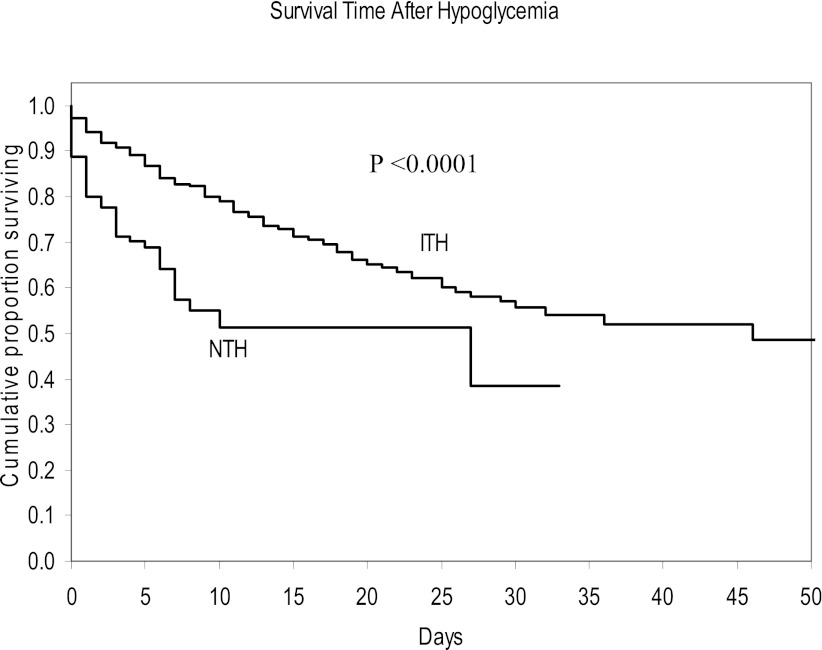
On univariate regression analysis, the CCI and admission to the ICU were associated with higher mortality, whereas female sex and insulin treatment were associated with lower mortality (Table 2). The HR for death in the ITH group relative to the NTH group in a multiple variable model that included CCI, age, sex, and admission to the ICU as covariates was 0.34 (95% CI 0.25–0.47, P < 0.0001) (Table 3). The Kaplan-Meier plot depicts better survival after hypoglycemia in insulin-treated patients compared with spontaneous hypoglycemic patients, especially in the first 2 weeks, where most of the data were concentrated (Fig. 1).
Table 2.
Analysis of individual variables predicting mortality after hypoglycemia (n = 1,096)
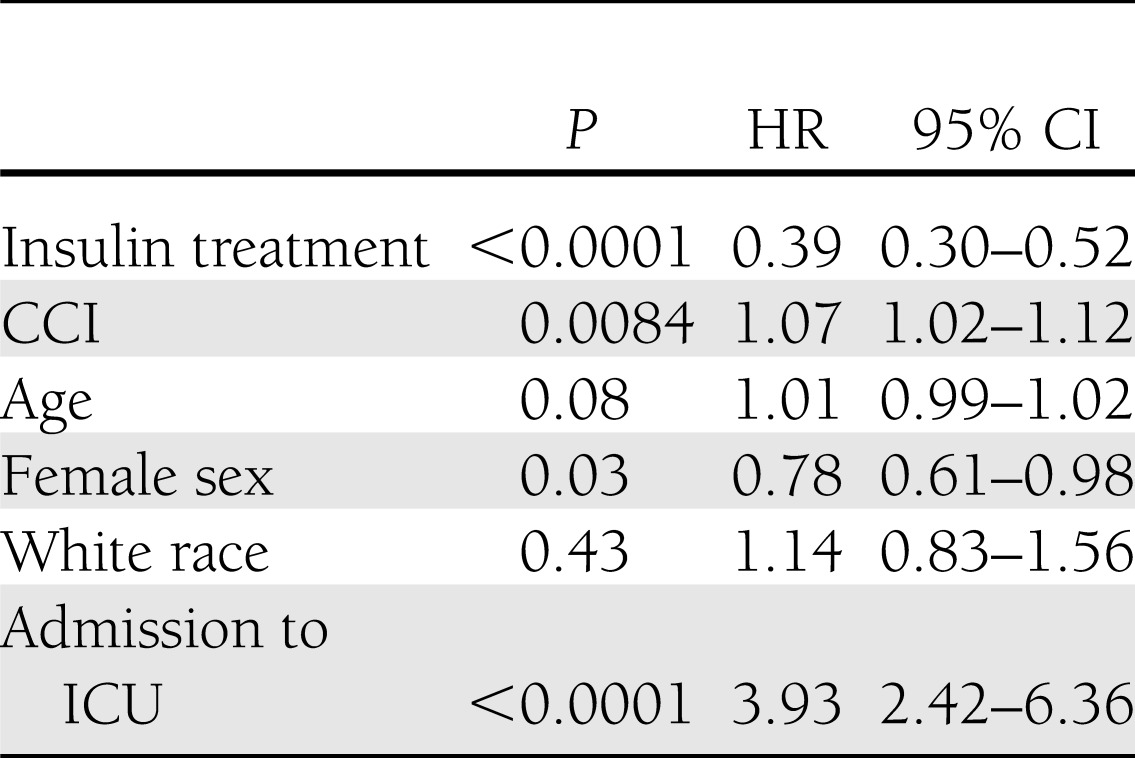
Table 3.
Multiple variable model predicting mortality after hypoglycemia (n = 1,096)
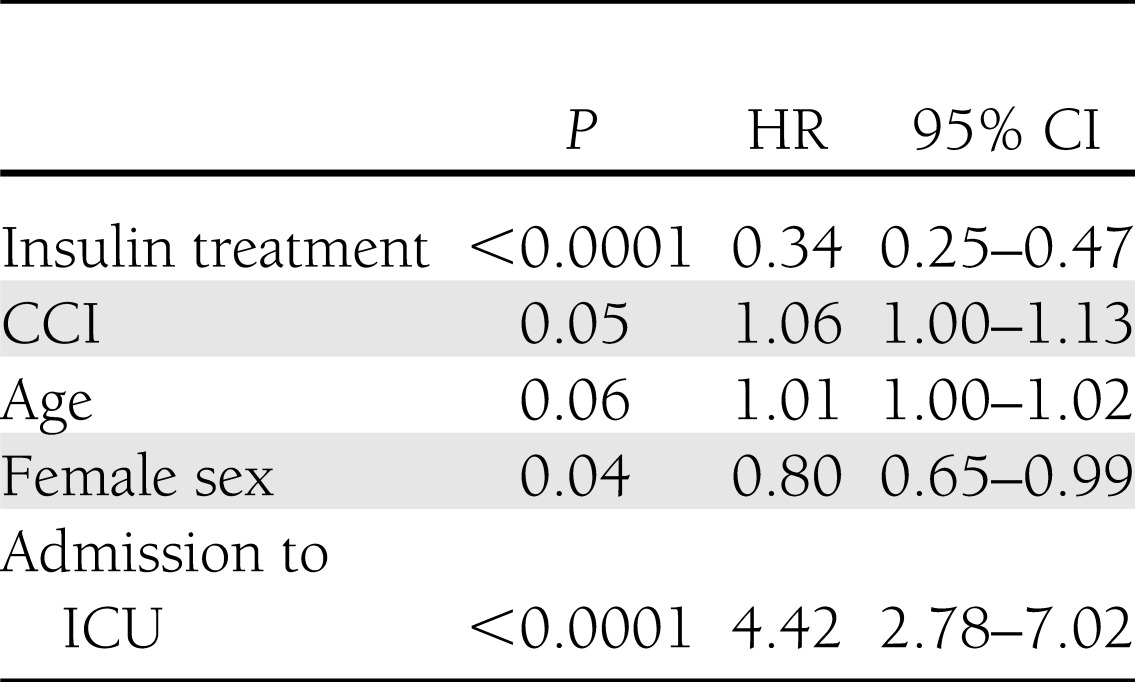
Figure 1.
Plot of survival after the first episode of hypoglycemia for the ITH group versus the NTH group.
CONCLUSIONS
This study shows that hypoglycemia in hospitalized patients, whether insulin induced or spontaneous, is associated with increased mortality as compared with absence of hypoglycemia. As expected, insulin-treated patients in our study were more likely to have diabetes and were older than the noninsulin-treated patients. Higher mortality in the ITC group compared with the NTC group may be due to their older age and higher prevalence of diabetes. However, the presence of hypoglycemia in insulin-treated patients increased their risk of death several-fold compared with ITC patients, even though this risk was lower than that in spontaneously hypoglycemic patients. This finding is in contrast to the previous studies that showed that insulin-induced hypoglycemia (<70 mg/dL) was not associated with increased risk of mortality (1,7). Our study is different from previous studies due to a different patient population and inclusion of patients with more severe hypoglycemia. Nonetheless, in our study, insulin was highly associated with longer survival and ICU admission was highly associated with shorter survival in patients with hypoglycemia.
Although early trials of tight glycemic control in critically ill hospitalized patients showed benefits of tight glycemic control, subsequent trials either failed to show benefits or ended early due to the risk of hypoglycemia (10–14). One of the potential explanations for the failure of tight glycemic control has been the high risk of hypoglycemia. Current American Diabetes Association guidelines recommend avoiding hypoglycemia in hospitalized patients (15). Hypoglycemic patients often have more severe illnesses. Most studies, in the inpatient setting as well as in the outpatient setting, have demonstrated that spontaneous hypoglycemia is associated with increased mortality as compared with insulin-induced hypoglycemia, and our study supports these data (7,16,17). However, our study also shows that mortality in the ITH group was still very high, suggesting only a partial, if any, protective effect of insulin. We think insulin administration may unmask hypoglycemia more easily in sicker patients. Whether hypoglycemia causes increased mortality remains unclear.
Our study has several limitations that are expected of retrospective studies. This was a single-center study, and the sample size for the spontaneous hypoglycemia group was rather small. We did not have data on the nutritional status of the patients. Also, we did not have details about the type of diabetes, duration of diabetes, insulin regimens, or glucose control. We assumed that hypoglycemia in insulin-treated patients was insulin associated even though we did not have information about the exact time of insulin injection and the relation between insulin injection and hypoglycemia. Furthermore, our analyses did not include adjustments for several confounders, including serum creatinine, hematocrit, albumin, and the use of other medications, including steroids. However, we did control for comorbidity and the severity of illness by including the CCI and admission to the ICU. We think these data provide valuable information on the relation between hypoglycemia and mortality in the inpatient setting.
We conclude that insulin-induced hypoglycemia as well as spontaneous hypoglycemia is associated with increased mortality among hospitalized patients. Prospective studies are needed to determine whether the prevention of hypoglycemia improves outcome in hospitalized patients.
Acknowledgments
This study was supported by the Brigham and Women's Hospital and Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 RR025758 and financial contributions from Harvard University and its affiliated academic health care centers).
No potential conflicts of interest relevant to this article were reported.
R.G. conceived the idea, procured funding, collected and interpreted data, and wrote the manuscript. S.H. conducted statistical analysis and wrote the manuscript. A.Tu. interpreted the data, contributed to discussion, and reviewed the manuscript. A.Tr. organized and cleaned up the database and provided useful suggestions for data analysis. All authors contributed to the manuscript and take full responsibility for its originality. R.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was presented in poster form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, Pennsylvania, 8–12 June 2012.
The authors thank Rie Maurer (Brigham and Women’s Hospital Center for Clinical Investigation) for help with calculating the CCI.
References
- 1.Boucai L, Southern WN, Zonszein J. Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med 2011;124:1028–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care 2009;32:1153–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egi M, Bellomo R, Stachowski E, et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc 2010;85:217–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fischer KF, Lees JA, Newman JH. Hypoglycemia in hospitalized patients. Causes and outcomes. N Engl J Med 1986;315:1245–1250 [DOI] [PubMed] [Google Scholar]
- 5.Kagansky N, Levy S, Rimon E, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med 2003;163:1825–1829 [DOI] [PubMed] [Google Scholar]
- 6.Mortensen EM, Garcia S, Leykum L, Nakashima B, Restrepo MI, Anzueto A. Association of hypoglycemia with mortality for subjects hospitalized with pneumonia. Am J Med Sci 2010;339:239–243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kosiborod M, Inzucchi SE, Goyal A, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA 2009;301:1556–1564 [DOI] [PubMed] [Google Scholar]
- 8.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–1251 [DOI] [PubMed] [Google Scholar]
- 9.Lee EW, Wei LJ, Amato D. Cox-Type Regression Analysis for Large Numbers of Small Groups of Correlated Failure Time Observations. Netherlands, Kluwer Academic, 1992, p. 237–247 [Google Scholar]
- 10.Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006;354:449–461 [DOI] [PubMed] [Google Scholar]
- 11.van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001;345:1359–1367 [DOI] [PubMed] [Google Scholar]
- 12.Finfer S, Chittock DR, Su SY, et al. NICE-SUGAR Study Investigators Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–1297 [DOI] [PubMed] [Google Scholar]
- 13.Brunkhorst FM, Engel C, Bloos F, et al. German Competence Network Sepsis (SepNet) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 2008;358:125–139 [DOI] [PubMed] [Google Scholar]
- 14.Preiser JC, Devos P, Ruiz-Santana S, et al. A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 2009;35:1738–1748 [DOI] [PubMed] [Google Scholar]
- 15.Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists. American Diabetes Association American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 2009;32:1119–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ 2010;340:b4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zoungas S, Patel A, Chalmers J, et al. ADVANCE Collaborative Group Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–1418 [DOI] [PubMed] [Google Scholar]