Abstract
Background
The use of computerized provider order entry (CPOE) has been widely linked to improvements in patient safety. We hypothesized that electronic routing of CPOE-generated orders through individual pagers would improve the efficiency of STAT radiographic studies and respiratory treatments.
Methods
The study was conducted in two periods before and after implementing pager notification of STAT orders. In the Baseline Period, CPOE-generated STAT orders were communicated to radiology technicians or respiratory therapists through the use of printed orders, manual paging and/or telephone communication. The time to process the order and deliver a radiology result or respiratory treatment was tracked. In the Intervention Period CPOE-generated STAT orders were electronically routed to the radiology technician’s or respiratory therapist’s pager. During both time periods, clinicians completed user satisfaction surveys.
Results
Using pager notification, there was a significant reduction in radiology technician arrival time (16.8±2.1 vs 7.9±0.7 mins, p<0.001). Similarly there was a significant reduction in the cumulative time required to capture the radiographic image, image availability in the picture archiving and communication system (PACS) and the verbal report from the radiologist (p<0.05). The time required in obtaining a preliminary or final radiographic written report and the total cycle times were not significantly reduced. For STAT respiratory therapy orders there was a significant reduction in the mean time from ordering to administration of respiratory therapy treatments (124.7±14.1 vs 49.8±11.4 minutes, p<0.01). Radiologists, respiratory therapists and ordering clinicians reported improved satisfaction after implementation of pager notification.
Conclusion
Computer-generated orders for STAT radiographic studies and respiratory treatments can be carried out significantly faster through the use of direct pager notification. The implementation of this process has resulted in improved care delivery and widespread clinician satisfaction.
Keywords: Computerized provider order entry, Efficiency, Care orders, Radiology, Respiratory therapy
Introduction
The pursuit of high quality, safe and efficient care delivery is a recurring theme in today’s health care environment [1,2]. Computerized provider order entry (CPOE) allows clinicians to enter complete, legible, unambiguous orders accompanied by clinician name and contact information. While CPOE has been associated with improved patient safety and quality of care, little information is available regarding the impact of CPOE on clinician and patient care efficiency [3-7]. Efficiency is particularly important when it comes to the delivery of urgent care such as STAT laboratory and radiology testing and essential medication delivery [8,9]. At Cincinnati Children’s Hospital Medical Center (CCHMC), CPOE was implemented throughout the institution in 2002. In an effort to improve the efficiency of care delivery surrounding STAT radiology and respiratory therapy orders, a pager notification system was interfaced with the CPOE platform to speed the delivery of these STAT orders to the appropriate health care provider.
Objectives
We hypothesized that the efficiency of care delivery and overall satisfaction with STAT radiology studies and respiratory therapy treatments would be improved after implementation of pager notification for these services.
Methods
Institutional background
This study took place at CCHMC, a 475 bed tertiary care pediatric institution with 799,917 patient encounters, 89,953 Emergency Department visits and 23,496 admissions in 2005. Between April and December 2002, CCHMC implemented the Integrating Clinical Information System (ICIS), whose core (Siemens INVISION®, Siemens Medical Systems, Malvern, PA) includes a web-based access portal, CPOE, clinical documentation, an electronic medication administration record, and a data storage repository. In addition to these core components, the ICIS includes workflow-integrated clinical decision support and electronic links to intranet and internet-based resources including institutional policies, medication formulary, internet medical search functions and other reference materials. The ICIS also allows for the development of system edits and rules for support of clinicians in their prescribing and documentation roles. Each week, over 30,000 patient care orders are entered into the ICIS. Over ninety percent of these orders are generated directly by physicians or advanced practice nurses with the remainder generated by verbal order.
Radiology Studies
Baseline Period
STAT Orders for Radiology Studies
Between March and May 2002, CPOE-generated STAT radiology orders were routed to a STAT printer in the radiology department. Subsequent transmission of these orders to the STAT radiology technician relied on standard methods such as telephone or oral communication or paging of the technician upon receipt of the printed order. Occasionally, in addition to placing the order in CPOE, the unit clerk would call the radiology department directly. During this period, time-motion studies were conducted to ascertain the amount of time required to complete each step in the process of carrying out a STAT portable radiology study. Six processing times were tracked: 1=technician arrival, 2=radiograph exposure taken, 3=image available in the PACS, 4=radiologist verbal report available, 5=radiologist preliminary written report available, 6=radiologist final written report available.
Implementation of Pager Notification for Stat Radiology Studies
In June 2002, pager notification of orders for STAT radiology studies was implemented throughout ICIS. Upon completion of a STAT CPOE order, a message containing the patient’s unit, bed location and order description (i.e. stat chest radiograph) is sent via Arch Net communication servers (USA Mobility, Inc., Alexandria, VA) to a designated pager carried by the STAT radiology technician (►Figure 1). Upon entering the order in the ICIS, an OASGold software product (Siemens INVISION®, Siemens Medical Systems, Malvern, PA) calls an external application on the client PC. The function provided is called a graphical user interface action controller (GAC). This GAC can be programmed on the screen and can be triggered automatically. The radiology order pathways include a screen that uses a GAC to send the page. A call is sent to Internet Explorer 6.0 (Microsoft Corporation, Redmond, WA) using a GAC with the appropriate parameters to send the required message and pager number information to an internal CCHMC web page. The internal web page reformats the information and forwards it to the Arch Net web page that is used to send pages. The Arch Net web page is then displayed on the PC as a confirmation of success to the ordering clinician. Prior to going live, this pathway was extensively tested by physicians, radiology technicians, respiratory therapists, and an analyst from Information Services. Pilot validation consisted of a test sample of 50 test orders entered into CPOE with sampling according to the algorithm below. Each step was analyzed electronically to ensure the intact flow of data (►Figure 2). Reading of order by the technician required manual query as there were no electronic data points to analyze. All 50 entered test orders were received by the technician.
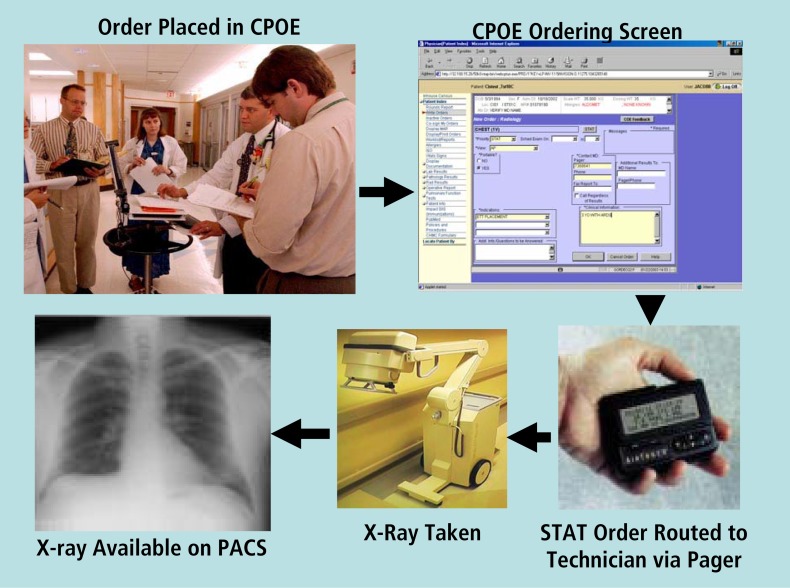
Figure 1.
CPOE radiology ordering process. STAT radiology orders are entered into ICIS via a wireless device and are routed directly to the STAT radiology technician’s pager. The technician arrives to take the radiograph and the image is then available in PACS.
Figure 2.
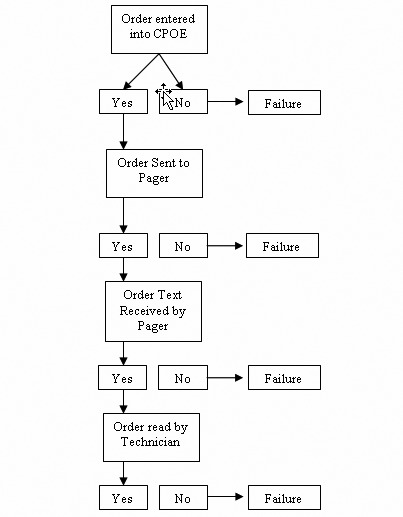
CPOE radiology ordering process. STAT radiology orders are entered into ICIS via a wireless device and are routed directly to the STAT radiology technician’s pager. The technician arrives to take the radiograph and the image is then available in PACS.
Intervention (Pager Notification) Period
STAT Orders for Radiology Studies
After pager notification was implemented, 1-month was allowed to elapse to allow users to become familiar with the system. The study data collection resumed between July and September 2002. The time required to complete each step in the process of carrying out a STAT portable radiology study was studied as in the Baseline Period.
Radiology User Satisfaction
Ordering clinicians, radiology technicians and radiologists completed user satisfaction surveys during both study periods. A five point modified Likert scale was used for the survey (1=Very Poor, 2=Poor, 3=Adequate, 4=Good, 5=Very Good) [10]. Prescribing clinicians and radiology faculty were asked 3 questions: 1) How adequate is the response time to performing a radiologic study after a STAT request? 2) How adequate is the response time to providing a radiologic verbal report after a STAT request? 3) How efficient is the radiology verbal reporting system. Radiology technicians were asked the first two questions above.
Respiratory Treatments
Baseline Period
STAT Orders for Respiratory Treatments
Prior to October 2003, CPOE-generated orders for STAT respiratory treatments were routed to the active orders display within the ICIS platform. Respiratory therapist notification of such orders occurred in a variety of ways including: 1) Discovery of the STAT order by nursing or respiratory therapy staff via routine log-in into ICIS; 2) Direct verbal communication of the order from physician or nurse to respiratory therapist; or 3) Initiation of a page from a physician, nurse or unit clerk to the respiratory therapist informing them of the order. Respiratory therapists were required to document the time of respiratory treatment administration in the ICIS upon completion. During the Baseline Period, a query was performed between April and September 2003 to determine the time from STAT respiratory treatment order generation in ICIS to treatment administration by the respiratory therapist.
Intervention (Pager Notification) Period
STAT Orders for Respiratory Treatments
After successful implementation, pager notification was utilized in communicating STAT respiratory treatment orders to the respiratory therapists for all units (►Figure 3). STAT orders for respiratory treatments were routed to specific respiratory therapist pagers allowing them to receive notification of the order immediately after it was entered in ICIS. After a 2-month familiarization period, ICIS was queried between January and June 2004 to determine the time from STAT respiratory treatment order generation in ICIS to treatment administration by the respiratory therapist. Intensive care units were not included in the data analysis as these locations have dedicated respiratory therapy staff residing at all times on the unit. Non-critical care units at CCHMC rely on a mix of dedicated respiratory therapists and floating respiratory therapists that cover a broad area of the hospital.
Figure 3.
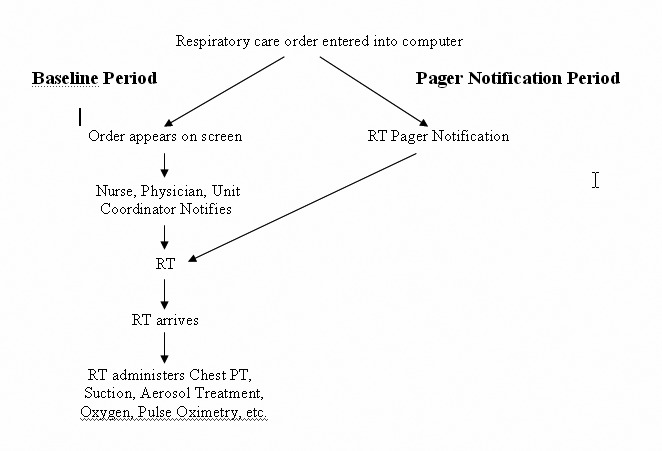
Respiratory therapy order processing before and after implementation of the pager notification system. The time expended contacting the respiratory therapist is avoided with pager notification. RT=respiratory therapist, PT=physical therapy
Respiratory Therapy User Satisfaction
Respiratory therapists completed user satisfaction surveys during both study periods. Respondents were asked to provide a yes or no answer to each question along with comments if appropriate. The questions included: 1) Do you feel that ICIS has made any impact on patient safety? 2) Are there fewer unintended consequences? 3) Has the medication alerting system impacted safety? 4) Has your workflow efficiency as an RT improved or become worse? 5) Has the time from when the order is written until it is carried out been decreased? 6) Do you feel that the quality of care delivered has been positively impacted by ICIS? 7) Do you think the ICIS system is more cost effective? 8) Rate your overall user satisfaction with the ICIS system.
Analysis
Categorical variables were compared using Pearson’s chi-square or Fischer’s Exact Test. Continuous variables were evaluated using the Student’s t test for parametric distributions and the Mann-Whitney Rank Sum test for non-parametric distributions. A p value of ≤ 0.05 was considered significant.
Results
Radiology Studies
Efficiency
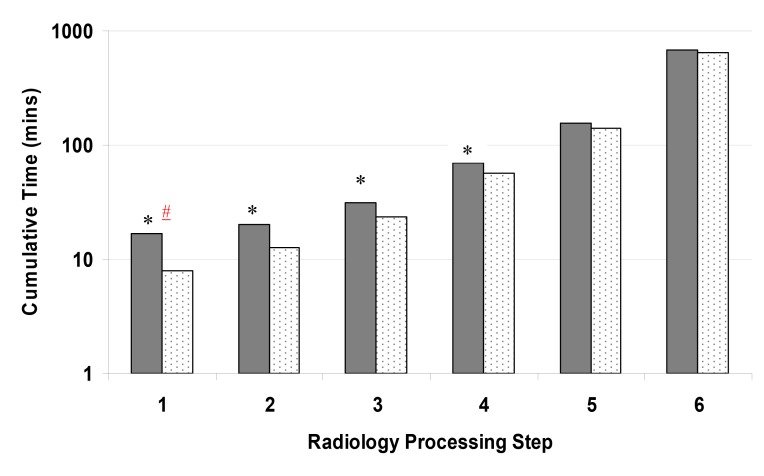
In the Baseline Period there were 27 STAT radiology studies ordered. Twenty three (85%) studies were chest radiographs, and 4 (15%) studies were abdominal radiographs. In the Pager Notification Period there were 20 STAT radiology studies ordered. Fifteen (75%) studies were chest radiographs and 5 (25%) were abdominal radiographs (p=0.47). The time required for each step of the radiology cycle was analyzed. There was a significant reduction in technician arrival time (16.8±2.1 vs 7.9±0.7 mins, p<0.001), cumulative time to acquiring the radiographic image (20.2±2.4 vs 12.5±1.6 mins, p=0.012), cumulative time for image availability for viewing in the PACS system (31.2±3.2 vs 23.2±2.4 mins, p=0.005) and cumulative time required to obtain a verbal radiologist report on the study (70.3±11.4 vs 56.6±7.9, p=0.048), (►Figure 4). The cumulative time required to obtain a preliminary or final written radiologist report and total cycle time were not significantly changed after implementing pager notification.
Figure 4.
Time to completion for each of six stages during a ‘STAT’ radiographic order study (Baseline Period – dark bars, and Pager Notification Period – light bars). The Baseline Period represents the mean time required for each stage in 27 studies. Pager Notification Period represents the mean time required for each stage in 20 studies. Stage 1 = time from STAT order to technicians arrival, Stage 2 = time from technicians arrival to obtaining the radiographic image, Stage 3 = time to image available for viewing in the PACS system, Stage 4=time to verbal radiologist report, Stage 5 =time to preliminary written report, and Stage 6 = time to final written report. * = p < 0.05 for cumulative results, # = p<0.05 for stepwise results.
User Satisfaction
In the Baseline Period, 157 surveys were sent out to Radiologists, ordering clinicians and radiology technicians and 129 (82.2%) were completed. In the Pager Notification Period, 123 surveys were sent out and 90 (73.2%) were completed. Overall satisfaction was rated in the adequate to good range during both study periods. Prescribing physicians, radiologists and radiology technicians tended to be more satisfied after pager notification was implemented. However, with one exception, these results did not achieve statistical significance (►Table 2). Radiologists reported significantly greater satisfaction with the response time in providing a verbal report after a STAT request. Survey results after implementation of pager notification included the following comments from prescribing physicians: “Overall, I think the system is now very effective and efficient”. “The current system has a great response time”. “I think the current system functions very well and will only improve”. Technicians commented that “having the CPOE information before doing the X-Ray is very helpful and gives me more useful information”.
Table 2.
Radiology User Satisfaction Survey Results. Prescribing clinicians and radiology faculty were asked the following questions: (1) How adequate is the response time to performing a radiologic study after a STAT request? (2) How adequate is the response time to providing a radiologic verbal report after a STAT request? (3) How efficient is the radiology verbal reporting system? Radiology technicians were asked only the first 2 questions. The rating system ranged from 1 to 5 (1=Very Poor, 2=Poor, 3=Adequate, 4=Good, 5=Very Good). Results are expressed as mean±SEM.
| Question | Baseline Period (n=129) |
Pager Notification Period (n=90) |
P |
|---|---|---|---|
| Ordering Clinicians | (n=91) | (n=57) | |
| Question 1 | 3.9±0.1 | 4.1±0.1 | 0.12 |
| Question 2 | 3.5±0.1 | 3.5±0.1 | 0.58 |
| Question 3 | 3.4±0.1 | 3.5±0.1 | 0.92 |
| Radiologists | (n=23) | (n=19) | |
| Question 1 | 4.0±0.1 | 4.4±0.2 | 0.14 |
| Question 2 | 3.6±0.2 | 4.3±0.2 | 0.02 |
| Question 3 | 3.0±0.2 | 3.2±0.3 | 0.53 |
| Radiology Technicians | (n=15) | (n=14) | |
| Question 1 | 4.0±0.1 | 4.2±0.2 | 0.51 |
| Question 2 | 3.2±0.1 | 3.7±0.3 | 0.14 |
Respiratory Treatments
Efficiency
In the Baseline Period there were 132 STAT respiratory therapy treatments ordered. These treatments included albuterol 72/132 (54.5%), racemic epinephrine 35/132 (26.5%), ipratropium 15/132 (11.4%) and levalbuterol 10/132 (7.6%).
In the Pager Notification Period there were 133 STAT respiratory therapy treatments ordered. These treatments included albuterol 71/133 (53.4%), racemic epinephrine 43/133 (32.3%), ipratropium 5/133 (3.8%) and levalbuterol 14/133 (10.5%). There was a significant reduction in the time from ordering to administration of STAT respiratory therapy treatments after implementation of pager notification (mean 124.7±14.1 vs 49.8±11.4 minutes, p<0.001) (►Table 1).
Table 1.
Respiratory Therapy Pager Notification Efficiency Results (* = p<0.001 in comparison to Baseline)
| Baseline Period (n=132 orders) | Pager Notification Period (n=133 orders) | |
|---|---|---|
| Mean Time from STAT Order to Rx Administration | 124.7 ± 14.1 Minutes | 49.8 ± 11.4 minutes* |
| Median time | 64.5 minutes | 17 minutes* |
| Range | 0-722 minutes | 0-1,117 minutes |
User Satisfaction
In the Baseline Period, 80 surveys were sent out to respiratory therapists and 59 (73.8%) were completed. In the Pager Notification Period, 87 surveys were sent out and 70 (80.4%) were completed. Respiratory therapists had significantly improved satisfaction in the areas of patient safety, unintended consequences, workflow efficiency, time to carrying out an order, and in overall quality of care (questions 1,2,4,5 and 6) after implementation of pager notification (►Table 3). Overall satisfaction (question 8) was similarly improved (3.4±0.1 vs 4.2±0.1, p<0.001). Survey results after implementation of pager notification included the following comments from respiratory therapists: “Information is at your fingertips and is more accessible”. “We are now notified immediately after an order is placed”. “The time in which orders are placed and that the care giver is notified has lessened greatly and care giver can check the orders from any computer more quickly instead of having to find a chart”.
Table 3.
Respiratory Therapist User Satisfaction Survey Results. Respiratory therapists were asked to respond yes or no to the following questions: 1) Do you feel that ICIS has had a positive impact on patient safety? 2) Are there fewer unintended consequences since ICIS was implemented? 3) Has the medication alerting system impacted safety? 4) Has your workflow efficiency as an RT improved? 5) Has the time decreased from when the order is generated until it is carried out? 6) Do you feel that the quality of care delivered has been positively impacted upon by ICIS? 7) Do you think the ICIS system is more cost effective than paper? In addition, in question number 8, respiratory therapists were asked to rate their overall user satisfaction with the ICIS system and pager notification (response range 1 to 5: 1=Very Poor, 2=Poor, 3=Adequate, 4=Good, 5=Very Good).
| Baseline Period (n=59) | Pager Notification Period (n=70) | P | |
|---|---|---|---|
| Responded Yes | Responded Yes | ||
| Question 1 | 44/59 (75%) | 68/70 (97%) | <0.001 |
| Question 2 | 19/59 (32%) | 59/70 (84%) | <0.001 |
| Question 3 | 51/59 (86%) | 53/70 (76%) | 0.19 |
| Question 4 | 43/59 (73%) | 70/70 (100%) | <0.001 |
| Question 5 | 43/59 (73%) | 66/70 (94%) | 0.002 |
| Question 6 | 37/59 (63%) | 64/70 (100%) | <0.001 |
| Question 7 | 48/59 (81%) | 53/70 (76%) | 0.58 |
| Question 8 | 3.4±0.1 | 4.2±0.1 | <0.001 |
Discussion
In the inpatient setting, important decisions are often made based on the results of radiographic studies. These studies frequently detect such abnormalities as pneumonia, pneumothorax, malpositioned devices (endotracheal tubes, central venous catheters), free intraperitoneal air and other abnormalities requiring alteration in the care plan [11]. Efficient delivery of STAT radiographic testing, availability of the image and the associated interpretation are essential for optimal patient care. Similarly, inpatients with respiratory distress rely on timely delivery of respiratory therapy. Failure to provide care in an efficient manner can result in adverse events in the inpatient setting. Inefficient notification of critical laboratory values has previously been shown have an important relationship with preventable adverse events [3]. In addition, inefficient care can contribute to patient and provider dissatisfaction [12,13]. Inefficient and poor quality care has been associated with significantly longer risk-adjusted length of stay than in cases where care was of acceptable quality [14].
Many studies have noted a positive impact of CPOE systems in reducing medical errors in patients [4-7]. The Leapfrog Group, a coalition of more than 175 public and private organizations that provide health care benefits, has identified CPOE as a primary hospital safety standard due to the benefits of improved safety and reduced costs [15]. In addition to creating complete, unambiguous, legible orders including clinician contact information, CPOE systems may include advanced clinical decision support capabilities to further enhance prescribing safety and consistency. Studies examining the effect of CPOE on healthcare efficiency have noted mixed results [16]. Kuperman, et al. conducted a randomized controlled trial examining the impact of delivering critical laboratory results in an automated fashion [17]. These investigators noted a significantly reduced delivery time for these critical values to physicians.
We hypothesized that implementation of a pager notification system linked to CPOE would result in improved efficiency in STAT radiographic testing and results reporting and in STAT respiratory therapy delivery. We noted that the use of pager notification resulted in a 53% absolute reduction (16.8 to 7.9 minutes) in the time required for a technician to arrive at the bedside and a 26% absolute reduction (31.2 to 23.2 minutes) in the time necessary for a clinician to view a PACS image after a STAT radiograph order is generated. Furthermore, we noted a 19% absolute reduction (70.3 to 56.6 minutes) in the time required for a verbal report of the STAT radiology result from the Radiologist to the ordering clinician. In the inpatient setting, STAT radiograph orders are often utilized to search for potentially life threatening problems such as a malpositioned endotracheal tube or central venous catheter, the presence of a pneumothorax or free air in the peritoneum. Recognition time and appropriate intervention are directly related to problem resolution and favorable outcome for these problems [18]. The improvements noted in our study have been maintained in the years following study completion. Clinicians and patients continue to experience the advantages afforded by rapid availability of radiographic imaging and results reporting.
Our data also indicate important improvements in the delivery of respiratory therapy. Pager notification of STAT respiratory therapy orders resulted in a 60% improvement (124.7 to 49.8 minutes) in the mean time to delivery of this treatment to patients. STAT respiratory therapy orders are often initiated for urgent or emergent conditions such as delivery of oxygen to a patient who is hypoxemic or administration of a bronchodilator aerosol treatment to a patient with status asthmaticus. In these circumstances, rapid delivery of respiratory therapy is essential for optimal patient outcome [19].
In addition to improvements in efficient delivery of radiographic studies and respiratory therapy, we hypothesized that these changes would result in improved job satisfaction for ordering clinicians, radiology technicians, Radiologists and respiratory therapists. A recent study by Wilbright, et al. noted a close association between improved job efficiency and greater job satisfaction [13]. In the current study, ordering clinicians, Radiologists and radiology technicians responded to the satisfaction survey more favorably after the implementation of pager notification, however, statistical significance was reached only amongst Radiologists regarding the response time to providing a radiologic verbal report after a STAT request. In contrast, we noted a statistically significant improvement amongst respiratory therapists when they were surveyed regarding patient safety, efficiency and quality of care after implementation of the pager notification system.
Though the results of this study clearly demonstrate that electronic pager notification can improve patient care efficiency and user satisfaction, the query methodology detected occasional significant outliers in response time to STAT orders (i.e. 1,117 minutes, or over 18 hours for the delivery of a STAT respiratory therapy treatment). In this particular circumstance, the STAT order was cancelled by verbal order, which was not entered into the computer, after it was deemed unnecessary by the ordering clinician. The order was then verbally reactivated the following day. Therefore, electronic queries must be designed in a way to provide meaningful information for those receiving such summary data.
Our study was also limited in its ability to detect differences in important outcome measures, (i.e. length of stay, morbidity and cost effectiveness), which may have resulted from implementation of pager notification. Future studies should focus on the role of electronic health record efficiencies on these important patient-centric outcome variables.
Conclusions
The use of CPOE-generated orders for STAT radiographic studies and respiratory treatments can be carried out a lot more efficiently through the use of direct pager notification of technicians. This process has resulted in improved patient care delivery and significant clinician satisfaction.
Clinical Relevance
The results from STAT radiologic studies and the delivery of respiratory therapy treatments are often delayed as a result of inefficient technician notification processes. In this paper we found that routing STAT CPOE orders for these services directly to pagers carried by technicians, results in more efficient conveyance of these important diagnostic studies and treatments.
References
- 1.Kohn L, Corrigan J, Donaldson M, eds. To err is human: building a safer health system. Washington, DC: National Academy Press, 1999 [PubMed] [Google Scholar]
- 2.The Leapfrog Group Available athttp://www.leapfroggroup.orgaccessed Feb 5, 2010
- 3.Bates DW, O’Neil AC, Boyle D, Teich J, Chertow GM, Komaroff AL, et al. Potential identifiability and preventability of adverse events using information systems. J Am Med Inform Assoc. 1994;1:404-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741-7 [DOI] [PubMed] [Google Scholar]
- 5.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998;280:1311-16 [DOI] [PubMed] [Google Scholar]
- 6.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Potts AL, Barr FE, Gregory DF, Wright L, Patel NR. Computerized physician order entry and medication errors in a pediatric critical care unit. Pediatrics. 2004;113:59-63 [DOI] [PubMed] [Google Scholar]
- 8.Saxena S, Kempf R, Wilcox S. Critical laboratory value notification: A failure mode effects and criticality analysis. Joint Commission Journal on Quality and Patient Safety. 2005;31:495-506 [DOI] [PubMed] [Google Scholar]
- 9.Joint Commission on Accreditation of Healthcare Organizations http://www.jointcommission.org Accessed Feb 5, 2010
- 10.Likert R. A technique for the measurement of attitudes. Archives of Psychology 1932;140:55-59 [Google Scholar]
- 11.Hauser GJ, Pollack MM, Sivit CJ, Taylor GA, Bulas DI, Guion CJ. Routine chest radiographs in pediatric intensive care: a prospective study. Pediatrics 1989;83:465-70 [PubMed] [Google Scholar]
- 12.Xakellis GC. Improving efficiency in a residency training clinic: results from addressing a root cause of inefficiency. Fam Med 2003;35:514-8 [PubMed] [Google Scholar]
- 13.Wilbright WA, Marier R, Abrams A, Smith L, Tran D, Thriffiley A, Jr, et al. Building a results review system: a critical first step in transitioning from paper medical records. AMIA Annu Symp Proc. 2005;3:819-23 [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas JW, Guire KE, Horvat GG. Is patient length of stay related to quality of care? Hosp Health Serv Adm 1997;42:489-507 [PubMed] [Google Scholar]
- 15.The Leapfrog Group Computer physician order entry (CPOE) fact sheet. Available at: http://www.leapfroggroup.org/media/file/FactSheet_CPOE.pdfaccessed February 5, 2010
- 16.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006:144:E12-E22 [DOI] [PubMed] [Google Scholar]
- 17.Kuperman GJ, Teich JM, Tanasijevic MJ, Ma’Luf N, Rittenberg E, Jha A, et al. Improving response to critical laboratory results with automation: Results of a randomized controlled trial. JAMIA 1999:6:512-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bacon AK, Paix AD, Williamson JA, Webb RK, Chapman MJ. Crisis management during anaesthesia: pneumothorax. Qual Saf Health Care 2005;14:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fallot A. Respiratory distress. Pediatr Ann 2005;34:885-91 [DOI] [PubMed] [Google Scholar]