Abstract
Objectives
The aims of this study were to develop detailed clinical models (DCMs) for nursing problems related to perinatal care and to test the applicability of these detailed clinical models.
Methods
First, we extracted entities of nursing problems by analyzing nursing-problem statements from nursing records, reviewing the literature, and interviewing nurse experts. Second, we extracted attributes and possible values needed to describe the entities in more detail by again analyzing nursing statements, reviewing the literature, and consulting nurse experts. Third, DCMs were modeled by linking each entity with possible attributes with value sets and optionalities. Fourth, entities, attributes and value sets in the DCMs were mapped to the International Classification for Nursing Practice (ICNP) version 2. Finally, DCMs were validated by consulting a group of experts and by applying them to real clinical data and nursing care scenarios published in the literature. The adequacy of the entities, attributes, value sets, and optionalities of the attributes were validated.
Results
Fifty-eight entities were identified, 41 entities from nursing records, 12 entities from literature review and 5 entities from nurse experts. Sixty-five attributes with values were identified, 25 attributes from nursing records, 34 attributes from literature review, and 6 attributes from nurse experts. In total 58 DCMs were developed and validated.
Conclusions
The DCMs developed in this study can ensure that electronic health records contain meaningful and valid information, and support the semantic interoperability of nursing information.
Keywords: Information sharing, model, standards; data collection; knowledge representation
1. Introduction
The potential benefits of electronic medical records include improvements in patient safety and quality of care, and a reduction in the number of medical errors. These benefits depend on the semantic interoperability of data to be shared and exchanged. According to the Joint Initiative for Global Standards Harmonization, semantic interoperability is defined as the ability for data shared by systems to be understood at the level of fully defined domain concepts [1]. There are different levels of semantic interoperability, according to Elkin et al [2].
There are three critical factors in achieving high-level semantic interoperability
-
1.
Reference models for representing clinical data,
-
2.
Clinical terminology systems, and
-
3.
Agreed clinical data structure definitions [3].
Reference models such as HL7 CDA (Clinical Document Architecture), the openEHR Reference Model, and the ISO reference terminology model for nursing [4] are high-level logical models that permit the mapping of corresponding parts of information structures between systems [3]. However, they are too general to use in clinical practice. Clinical terminology systems – such as the International Classification of Diseases (ICD), Current Procedural Terminology (CPT), and SNOMED CT – facilitate the entry and analysis of healthcare data, but are also difficult for use in clinical practice due to the great variation in the scope and granularity of clinical terminologies.
Therefore, to ensure high-level semantic interoperability, it is necessary to have an agreed clinical data structure which can link reference models and terminologies [3]. That is, irrespective of which sets of Reference Models and Terminologies are adopted, structured clinical data are needed to achieve high-level semantic interoperability. Agreed data structures may be referred to under many different names, such as detailed clinical models (DCMs), clinical element models, generic templates, care information models, clinical content models, clinical templates, archetypes, clinical fragments, general purpose information components, and more [5]. A DCM is a relatively small, standalone information model designed to express a clinical concept in a standardized and reusable manner [6]. DCMs consist of entity-attribute-value triplets. An entity is a core or focus concept of a data element. An attribute is a qualifier that represents a data entity in more detail, and is associated with possible values. A value set, in turn, represents a uniquely identifiable set of valid concept representations of an attribute.
Several different approaches have been used in the development of agreed data structures; IMH Clinical Elements from Intermountain Healthcare as part of Detailed Clinical Models [7], ISO 13606 Archetypes [8], Clinical Templates Scotland [9], Clinical Contents Models [10], HL7 templates [11], and Detailed Clinical Model instances [12, 13]. However, the efforts in these approaches so far have been limited to the domain of medical knowledge. While the importance of developing a detailed clinical model for nursing has been addressed by nurse informaticists [14], there are only a few reports on this topic in nursing literature. An example is archetypes of nursing problems for breast cancer patients developed and tested in Korea [15]. However, archetypes developed for breast cancer patients do not possess the data types or attribute optionalities necessary for use in an electronic nursing records system.
2. Objectives
The aim of this study was to develop detailed clinical models for nursing problems faced in perinatal care, to be implemented in the electronic nursing records system. Specifically, we looked at the nursing problems of pregnant women who were hospitalized to give birth, because pregnant women exhibit comparatively few comorbidities and complications. With a DCM-based electronic nursing records system, data can be accumulated and integrated in a meaningful manner.
3. Methods
3.1. Development of DCMs
First, we extracted entities of nursing problems by analyzing nursing statements, reviewing the literature, and consulting nurses. We analyzed nursing diagnoses and statements used to describe signs and symptoms in the electronic nursing records of 118 women who were hospitalized to give birth from October 1 to October 31, 2008, at a tertiary teaching hospital in Korea. The number of electronic nursing records reviewed was determined by the data saturation point at which new data could not be extracted from the records.
For example, we extracted the entity “pain” from the nursing statements “mild back pain” and “continuous back pain”. We also reviewed nursing literature and consulted nurses in the process of extracting entities. The extracted entities were then evaluated and confirmed by a group of experts that comprised a head nurse, three nurses with master’s degrees, and four nurse experts with more than 7 years of clinical experience in maternal nursing.
Second, we extracted attributes and possible values needed to describe the entities in more detail by analyzing nursing statements, reviewing the literature, and consulting nurses. For example, attributes of the entity “pain” such as “anatomical site_Fx”, “severity”, and “frequency” were identified from the nursing statement “continuous mild back pain”. The attributes were named by referring to characterizing categories of the Conceptual Framework for Patient Findings and Problems in Terminologies published by ISO [16]. In turn, the attribute “frequency” for the entity “pain” has values such as “rarely”, “sometimes”, “often”, and “always”; a value set represents a uniquely identifiable set of valid concepts of an attribute. Frequently used values include numerical data, text, dates and times, and enumerations of lists and formats such as pictures. These will be handled in a DCM according to ISO 21090 data types specifications [17].
The data type of each attribute was assigned based on the ISO 20190 Health data types Standard. For example, the attribute of “frequency” in the entity “pain” has the data type of a character string with code. Optionality was assigned to attributes in order to express whether an attribute is optional or mandatory in describing the entity. The optionality of each attribute was determined by consulting staff nurses, and attributes with value sets, data types, and optionalities were validated by eight nurse experts.
Third, detailed clinical models were created by linking entities, attributes, and value sets. Then we bound the concepts in entity-attribute-value triplets to ICNP version 2, a reference terminology in nursing.
3.2. Validation of detailed clinical models
All DCMs were validated by eight nurse experts. The expert group comprised three doctoral students in nursing informatics, one head nurse with experience in informatics and maternal care, two informatics nurse specialists, and two nurses with more than 7 years of clinical experience in maternal nursing. Nurse experts were asked to evaluate whether entities were comprehensive enough to represent the nursing problems in perinatal care, and whether they were clearly named. They were also asked to evaluate whether attributes and value sets were mutually exclusive, relevant, and exhaustive enough to describe each entity; whether optionalities of attributes reflected nursing practice; and whether the term binding of DCM concepts with the ICNP was correct. When there was a conflict among experts, we convened another meeting to reach a consensus. When there was a conflict between experts and the research team, we followed the experts’ recommendation most of the time. However, if there was rationale not to follow, we did not accept their recommendation.
DCMs were also evaluated using real clinical data and two nursing care scenarios published in nursing literature. Real clinical data used for validation were nursing diagnoses and statements used to describe signs and symptoms in electronic nursing records of 141 women who were hospitalized to give birth from October 1 to October 31, 2009 at a tertiary teaching hospital in Korea. The nursing care scenarios used for validation were case studies of aplastic anemia arising in pregnancy [18] and of methods to stimulate the onset of labor [19]. We identified entities, attributes, and value sets from the electronic nursing records and the nursing care scenarios, and then tested whether the DCMs developed in this study could cover all concepts identified from the electronic nursing records and the nursing care scenarios by mapping the concepts to the DCMs.
4. Results
4.1. Development of DCMs
In order to extract nursing problems, we analyzed the nursing records of 118 patients who were hospitalized to give birth, which spanned 711 days in total. During the analysis, we reached the data saturation point at the 33rd patient where new problems were no longer extracted from the records. ►Table 1 shows the characteristics of the patients whose nursing records were analyzed. The mean age of the patients was 33.16 years (SD = 4.95) and the mean length of the hospital stay was 4.54 days (SD = 3.98 days), ranging from 2 to 28 days. Three-fourths (73%) of the patients had a normal delivery, including spontaneous vertex deliveries and normal full term vacuum extractor deliveries.
Table 1.
Characteristics of patients whose nursing records were analyzed (n=118)
| Variables | Mean SD (Range) | Frequency(%) |
|---|---|---|
| Age (years) | 33.16±4.95 (16–43) | |
| Length of stay (days) | 4.54±3.98 (2–28) | |
| Types of delivery | ||
| Normal delivery | 86 (73%) | |
| Spontaneous vertex delivery | 47 | |
| Normal full-term vacuum extractor delivery | 22 | |
| Preterm spontaneous delivery | 11 | |
| Rupture of membrane in labor | 6 | |
| Cesarean section | 32 (27%) | |
| Placenta previa with hemorrhage | 4 | |
| Previous Cesarean section | 11 | |
| Failed trial of labor, unspecified | 7 | |
| Elective cesarean delivery | 1 | |
| Breech presentation of fetus | 4 | |
| Transverse lie of fetus | 3 | |
| Severe preeclampsia | 2 | |
►Table 2 shows the 58 entities we identified for perinatal nursing care. Examples of 41 entities identified from the nursing records include concepts unique to maternal nursing, such as “uterine contraction”, “show”, “fetal heart sound”, and “lochia”, and general nursing concepts such as “gas emissions”, “constipation”, and “pain”. In addition, 12 entities such as “bishop score”, “guilt”, and “inverted nipples” were identified through literature review. Five more entities such as “body weight”, “abdominal circumference”, “abscess”, “fall”, and “arrhythmia” were identified from the experts” evaluation. These entities included not only physical signs and symptoms such as “dyspnea” and “seizure”, but also psychosocial problems such as “grief”, “guilt”, “depression”, and “parent role”. Furthermore, there were complex entities that comprised multiple other entities, such as “vital signs”, which comprised “blood pressure”, “pulse”, “respiration”, and “body temperature”.
Table 2.
A list of entities identified by source
| Sources | Entities | Frequency | ||
|---|---|---|---|---|
| Nursing Records |
|
|
|
41 |
| Literature Review |
|
|
|
12 |
| Nurse Experts |
|
|
|
5 |
| Total | 58 | |||
►Table 3 shows a list of attributes we identified by source. Twenty-five attributes were identified by analyzing nursing statements. For example, we identified the attribute “severity” with a value set of “absent”, “mild”, and “severe” by analyzing nursing statements such as “severe pain”, “mild pain”, and “no pain”. The attribute “Pain_Character” was identified with values such as “sharp”, “burning”, and “fulgurating” by analyzing nursing statements such as “burning pain”, “sharp pain”, and “fulgurating pain”. An additional 34 attributes were identified from a literature review, such as “intensity” with a value set of “none”, “weak”, “strong”, and “very strong”, and “Bwt_Clothing” with a value set of “lightly clothed/underwear” and “fully dressed”. Six more attributes were identified through consultation with the expert group, such as “level” with a value set of”–”,”±”,”+”, and “++” to describe the presence and amount of protein or ketone in the urine. In total, 65 attributes were identified. When we encountered an attribute with different value sets with different granularities, we used the more granular value set because the less granular value set can be inferred from the more granular value set.
Table 3.
A list of attributes identified by source
| Source | Attributes | Frequency | ||
|---|---|---|---|---|
| Nursing records | • Anatomical site_BP | • Frequency | • Rate | 25 |
| • Anatomical site_BT | • Interpretation | • Rhythm | ||
| • Anatomical site_Fx | • Interval | • Severity | ||
| • Anatomical site_PR | • Laterality | • SystolicPressure | ||
| • Circumference | • Occurrence | • Temperature | ||
| • Color | • Onset | • Volume | ||
| • Depth | • Pain_Character | • Weight | ||
|
|
|||
| Literature review |
|
|
|
34 |
| Nurse experts |
|
|
|
6 |
| Total | 65 | |||
Detailed clinical models were created by linking entities, attributes, and value sets. As an example, the DCM for “Breastfeeding” is listed in ►Table 4 and presented diagrammatically in ►Figure. 1. “Breastfeeding” has a “has_interpretation” relationship with the attribute “interpretation”, and a “has_duration” relationship with “duration”. The data type of the “interpretation”, “frequency”, “laterality”, and “position” attributes is “character string with code”; the data type of the “duration” attribute is “integer number”; the data type of “occurrence” is “point in time”; and the data type of “volume” is “physical quantity”. The optionality for “interpretation” is mandatory, and the optionality for “duration”, “frequency”, “occurrence”, “laterality”, “position”, and “volume” is optional.
Table 4.
Breastfeeding detailed clinical model
| Entity | Attribute | Relationship | Data type | Optionally | Value |
|---|---|---|---|---|---|
| Breastfeeding (100036 45 Breast Feeding) | Interpretation (10010981 Positive Or Negative Judgment) | has_interpretation | Character string with code | Mandatory | Effective (10014956 Effective) |
| Ineffective (10012938 Impaired) | |||||
| Duration (10006379 Duration) | has_duration | Integer number | Optional | Minute | |
| Hour | |||||
| Day (10005502 Day) | |||||
| Year (10021270 Year) | |||||
| Frequency (10008234 Frequency) | has_frequency | Character string with code | Optional | Rarely (10016374 Rarely) |
|
| Sometimes (10018508 Sometimes) | |||||
| Often (10013658 Often) | |||||
| Always (10002192 Always) | |||||
| Occurrence (10019721 Time Point Or Time Interval) | has_ocurrence | Point in time | Optional | Allow all yyyymmdd | |
| Laterality (10011163 laterality) | has_laterality | Character string with code | Optional | Left (10011267 Left) |
|
| Right (10017234 Right) | |||||
| Both | |||||
| Position (10003433 body position) | has_position | Character string with code | Optional | Lying (10019103 Supine) |
|
| Sitting (10018195 Sitting) | |||||
| Volume (10008062 fluid volume) | has_volume | Physical quantity | Optional | Unit: cc≥ 0 |
Fig. 1.
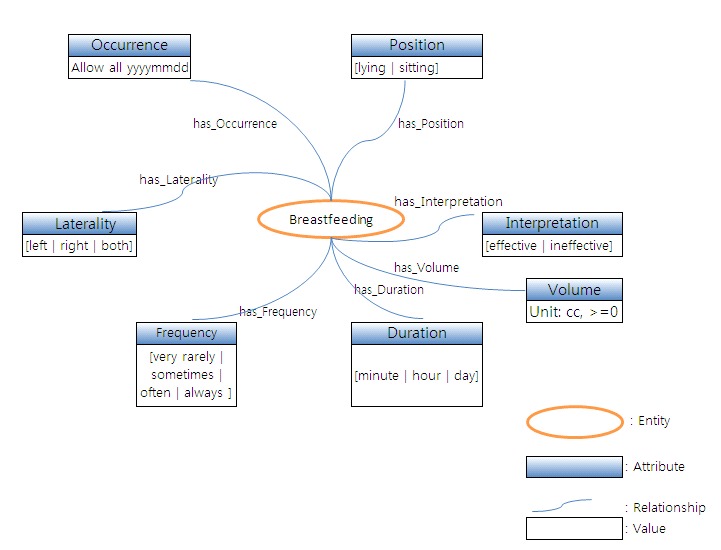
Diagrammatical representation of breastfeeding detailed clinical model
The entity concepts, attributes concepts, and values concepts were then mapped to 18 concepts of ICNP version 2. For example, the concept of “breastfeeding” was mapped to “10003645 Breast Feeding” of the ICNP. Another example, the DCM of “vital sign”, is presented in ►Figure. 2. The “vital sign” DCM is a complex model which is represented as a combination of the “blood pressure”, “pulse”, “respiration”, and “body temperature” DCMs. With the exception of a few value concepts, most of the entity and attribute concepts in entity-attribute-value triplets were mapped to ICNP version 2.
Fig. 2.
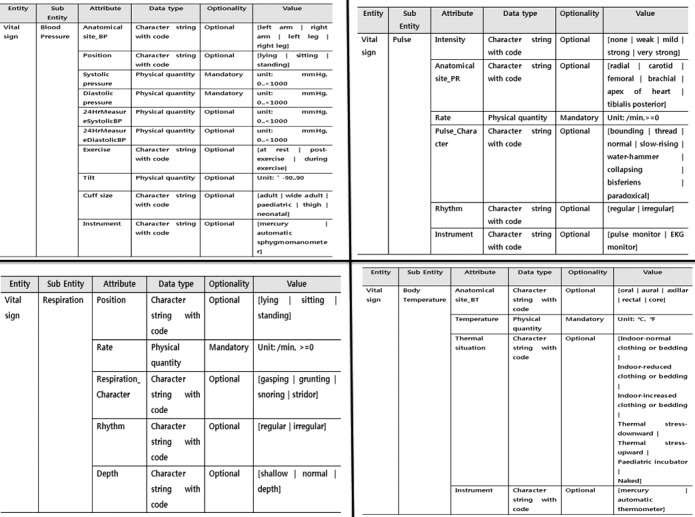
Diagrammatical representation of vital sign detailed clinical model
4.2. Validation of detailed clinical models
Detailed clinical models were validated by a group of experts, and tested by applying them to real clinical data and nursing care scenarios published in literature.
Nurse experts pointed out that three entities were named irrelevantly; “engorgement”, “urinary incontinence”, and “bowel incontinence”. Nurse experts suggested changing “engorgement” to “breast engorgement”, and combining “urinary incontinence” and “bowel incontinence” into “incontinence”. We changed “engorgement” to “breast engorgement” based on experts’ recommendations. However, we did not combine “urinary incontinence” and “bowel incontinence” into “incontinence”, because the “urinary incontinence” and “bowel incontinence” DCMs have different attributes and value sets.
One nurse expert recommended the addition of one entity, “meconium”. We also did not accept the recommendation of adding “meconium” as an entity, because “meconium” is not a focus concept of the nursing care of pregnant women; rather, it is a focus concept of the nursing care of infants.
Nurse experts also pointed out that ten DCMs lacked attributes and values sets. They were “position”, “interpretation”, “progression”, “causative agent”, and “occurrence” in the DCMs of “dyspnea”, “arrhythmia”, “depression”, “fall”, “syncope”, “blood pressure”, “body temperature”, “body weight”, and “blood sugar”. We added the “position” attribute with a value set of “supine”, “sitting”, and “standing” to the “dyspnea” DCM; the “interpretation” attribute with a value set of “absent” and “present” to the “arrhythmia” DCM; and the “progression” attribute with a value set of “acute” and “chronic” to the “depression” DCM.
However, we decided not to add the “causative agent” attribute with a value set of “bleeding” and “seizure” to the “fall” and “syncope” DCMs, because it is difficult for nurses to determine the cause of a “fall” or “syncope”. We decided not to follow the suggestion of adding “occurrence” as an attribute to describe the measurements in the “blood pressure”, “body temperature”, “body weight”, and “blood sugar” DCMs, because when nurses document blood pressure or blood sugar in nursing records, the recording time implies the time of measurement.
One nurse expert pointed out that attributes in three DCMs were not mutually exclusive; for example, the “interpretation” and “glucose” attributes in the “blood sugar” DCM, the “interpretation” and “rate” attributes in the “pulse” DCM, and the “interpretation” and “weight” attributes in the “body weight” DCM. We removed the “interpretation” attribute from the “blood sugar”, “body weight”, and “pulse” DCMs, because the values of the interpretation attributes of these three DCMs can be inferred from the “glucose”, “weight”, and “rate” attributes describing the actual level of the “blood sugar”±, “body weight”, and “pulse” DCMs.
Three nurse experts pointed out that two attributes in two DCMs were not relevant. They were the “volume” attribute in the “urinary frequency” DCM and the “severity” attribute in the “grief” DCM. We removed the “volume” attribute from the “urinary frequency” model and changed the “severity” attribute in the “grief” DCM from a former value set of “absent”,“tolerable”, “mild”, “moderate”, and “severe” to an “intensity” attribute with a value set of “none”, “weak”, “mild”, “strong”, and “very strong”.
One nurse expert recommended adding “greenish” as a value to the “color” attribute in the “rupture of membranes” and “abscess” DCMs. Two nurse experts recommended adding “week” as a value to the “duration” attribute in the “constipation” DCM and “10 minutes” as a value to the “occurrence” attribute in the “APGAR score” DCM. We added “greenish” as a value of the “color” attribute in the “rupture of membranes” and “abscess” DCMs, “week” as a value of the “duration” attribute in the “constipation” DCM, and “10 minutes” as a value of the “occurrence” attribute in the “APGAR score” DCM.
Five experts rated 14 out of 58 DCMs as having an irrelevant optionality of attributes. They recommended changing the optionalities of the following attributes from optional to mandatory; the “severity” attribute in the “depression”, “allergy”, “after pain”, “blurred vision”, “breast engorgement”, “constipation”, “diarrhea”, “dyspnea”, “dysuria”, and “flatulence” DCMs; the “interpretation” attribute in the “breastfeeding” DCM; the “anatomical site_Fx” attribute in the “abscess” DCM; the “intensity” attribute in the “grief” DCM; and the “stage” attribute in the “hemorrhoid” DCM.
We changed the optionalities of the following attributes from optional to mandatory; the “severity” attribute in the “depression”, “allergy”, “after pain”, “blurred vision”, “breast engorgement”, “constipation”, “diarrhea”, “dyspnea”, “dysuria”, and “flatulence” DCMs; the “interpretation” attribute in the “breastfeeding” DCM; the “anatomical site_Fx” attribute in the “abscess” DCM; the “intensity” attribute in the “grief” DCM; and the “stage” attribute in the “hemorrhoid” DCM.
With real data from electronic nursing records, we identified 43 entities, which included all of the entities we identified from electronic nursing records in the DCM development phase, plus “laceration of perineum” and “inverted nipple”. With two nursing care scenarios from the literature, DCMs unique to antenatal and postnatal care such as “menstruation history”, “gravida”, “parity”, “abortion”, “bishop score”, “uterine contraction”, and “rupture of membranes” were identified and validated. The DCMs developed in the present study completely covered all entities, attributes, and values identified from the electronic nursing records and the two nursing care scenarios.
►Table 5 indicates how the section describing “rupture of membranes” and “uterine contraction” in the scenarios dealing with methods to stimulate the onset of labor [17] was decomposed and mapped to values of attributes in the “rupture of membranes” and “uterine contraction” DCMs. For example, values of the different attributes of the “uterine contraction” DCM, such as “intensity”, “duration”, “occurrence”, “interval”, and “rhythm” were identified; the statement “Two days later, at 7:30 PM, M.S. presented to the birthing center experiencing mild uterine contractions every 5 to 7 minutes lasting 60 seconds since 5:00 PM” has information about the initial time, lasting time, degree, regularity, and interval of the uterine contractions. All of these values were covered by the value sets of the attributes of the “uterine contraction” DCM developed in this study.
Table 5.
Sample validation of DCMs using nursing care scenarios
| DCM | Nursing care scenarios | Value identified | Value in DCM | Attribute in DCM |
|---|---|---|---|---|
| Rupture of membranes | M.S. reported a ‘gush of clear fluid’ at 6:30 p.m. Ruptured membranes was confirmed by sterile speculum exam. | Confirmed | Positive | Interpretation |
| 6:30PM | 6:30PM | Occurrence | ||
| Clear | None | Color | ||
| Speculum exam | Speculum exam | Instrument | ||
| Uterine contraction | Two days later, at 7:30 PM, M.S. presented to the birthing center experiencing mild uterine contractions every 5 to 7 minutes lasting 60 seconds since 5:00 PM. | Mild | Mild | Intensity |
| Lasting 60 seconds | 1 minute | Duration | ||
| Since 5:00PM | 5:00PM | Occurrence | ||
| Every (5 to 7 minutes) | Regular | Rhythm | ||
| (Every) 5 to 7 minutes | 5–7 minutes | Interval |
Discussion
In the present study, we developed DCMs to represent the nursing problems in perinatal care. These DCMs were validated by a group of experts and tested by applying them to real clinical data and nursing care scenarios published in the literature.
We identified 58 entities by analyzing electronic nursing records, reviewing the literature, and consulting nurse experts. Most of the entities were identified by analyzing electronic nursing records that described physical problems such as “pain”, “diarrhea”, and “constipation”. However, most of the entities describing patients’ psychosocial problems – such as “grief”, “guilt”, and “parent role” – were identified by reviewing the literature and by consulting nurse experts. This implies that nurses do not document the psychosocial problems of their patients in their nursing notes as frequently as they document the physical problems of their patients. This concurs with Min’s findings in her work on developing archetypes of nursing problems for breast cancer patients [13]. We found that entities have different abstract levels. For example, the DCM of “vital sign” is more abstract than that of “body temperature”, “blood pressure”, “respiration”, and “pulse”. DCMs of “Body temperature”, “blood pressure”, “respiration”, and “pulse” can be part of the larger DCM of “vital sign”. Since DCMs are often tree-like structures, a DCM can be a node of a larger DCM. This raises debate on the granularity of DCMs and on where a DCM starts and ends.
It was found that the DCMs developed in this study were different from DCMs developed in medicine, due to nurses and doctors often approaching the same problems from different directions. Most DCMs developed in the medical domain have causative agents and confounding factors as attributes. For example, the “blood pressure” model of openEHR has “confounding factors” – such as anxiety and pain – that affect “blood pressure”.
However, the “blood pressure” DCM developed in this study does not have “confounding factors” as an attribute, because it is not easy for nurses to make judgments on what and how confounding factors may affect the model in question. As another example, the “pain” model developed in openEHR has the attribute “previous episodes” – which describes previous events – and “precipitating factors”, which trigger or bring on symptoms. However, the “pain” DCM developed in this study does not have “previous episodes” or “precipitating factors”, because it is similarly difficult for nurses to make judgment calls regarding previous episodes and precipitating factors. Thus, it is important that nursing develop its own domain knowledge DCMs [12].
On the patient level, some of the DCMs developed in this study would qualify as belonging not only to nursing, but also to the domain of obstetrics, e.g. gravidity and parity. Although they are useful for nursing care for pregnancy and delivery, they would be similarly useful for an obstetrician. Thus it would be important to acknowledge that many entities would be shared among professions. Ideally it would be best for multi-professions to develop a unified DCM and for part of the attributes to be completed by a physician and other attributes by a nurse, jointly forming the logical EHR structure. Then semantic consistency on the patient level and among disciplines can be achieved. DCM development work such as this study will contribute to identifying common attributes belonging to all professions and specific attributes belonging to different professions.
We found 65 attributes to describe entities in more detail, of which only 25 were identified through analyzing the electronic nursing records. Thirty-four out of 65 attributes (53%) were identified from a literature review, and 6 attributes were identified by consultation with nurse experts. This implies that nurses do not document nursing problems as precisely as described in the literature or as recommended by nurse experts.
It was found that DCMs of similar nursing problems can have exactly the same attributes. For example, the DCMs for “grief” and “guilt” have the same attributes of “intensity”, “progression”, “duration”, “frequency”, “onset”, and “occurrence”, with the same value sets. In addition, the “ketonuria” and “proteinuria” DCMs have the same attributes of “frequency”, “level”, and “occurrence”, with the same value sets. Other examples are the “constipation” and “diarrhea” DCMs, with the same attributes of “severity”, “progression”, “duration”, “frequency”, “onset”, and “occurrence”, with the same value sets.
On the other hand, DCMs of similar entities can also have different attributes. For example, even though “after pain” and “labor pain” are types of pain, they have different attributes from those of “pain”. In addition, the “pain” DCM has an attribute describing the site of the pain, whereas “after pain” and “labor pain” do not. Such groupings or patterns present in DCMs may prove useful in the further development and validation process.
It was also found that DCMs of nursing problems with directions of judgment – either negative or positive – can have specific attributes. For examples, DCMs associated with a negative judgment, such as “dyspnea” and “guilt”, and DCMs associated with a positive judgment, such as “breastfeeding”, always have the “occurrence” attribute. However, DCMs without any directions of judgment, such as “blood pressure”, “body weight”, and “blood sugar” do not have an “occurrence” attribute. It was found that some concepts in entity-attribute-value triplets were not mapped to ICNP version 2. We would like to propose adding these concepts to ICNP version 2.
Through validation, a group of experts recommended changing, adding, or deleting certain entities, attributes, values, or optionalities in the DCMs developed in this study. We did not accept all of their recommendations. For example, we did not combine “urinary incontinence” and “bowel incontinence” into “incontinence”, because they have different attributes and value sets. We also did not accept the recommendation of adding “meconium” as an entity, because it is not a focus concept of the nursing care of pregnant women; rather, it is a focus concept of the nursing care of infants. We decided not to add the “causative agent” attribute to the “fall” and “syncope” DCMs, because it is difficult for nurses to determine the cause of a “fall” or “syncope”. We decided not to follow the suggestion of adding “occurrence” as an attribute to the “blood pressure” and “blood sugar” DCMs, because when nurses document blood pressure or blood sugar in nursing records, the recording time implies the time of measurement.
Even though this paper addresses an important area of developing DCMs in nursing, the work needs to be further validated by applying them to other locations in Korea and worldwide.
Conclusions
The DCMs developed in this study can be used to guide the structured documentation of nursing records. If data are collected in a structured way using DCMs, a richer and more granular data set will be collected and stored, which can be reused for nursing research and education. In addition, if data are collected in a structured way using a value specified in the value set, data can be shared and exchanged with semantic interoperability between different information systems and different healthcare institutions. However, it is important to recognize that unless DCMs are standardized nationally or internationally, semantic interoperability to the highest possible degree cannot be achieved [2].
The procedures and methods used to develop DCMs in this model could be expanded to other areas of nursing. If the DCMs developed in this study are used in electronic nursing records, semantic interoperability of information will be ensured. Currently, we are in the process of implementing DCMs in an electronic nursing record system at a tertiary hospital in Korea.
Clinical Relevance
The detailed clinical models developed in this study can be used to guide the structured documentation of nursing records. If the detailed clinical models developed in this study are used in electronic nursing records, semantic interoperability of information will be ensured.
Conflict of Interest
All of the authors of this work hereby declare that there were no conflicts of interest or any other relationships that could have inappropriately influenced this study.
Protection of Human and Animal Subjects
This study was performed after receiving formal approval from the research review department of the study hospital. Patient data were anonymized for this study.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009–0074695, 2010–0028631).
References
- 1.Joint Initiative for Global Standards Harmonization. [cited 2011 March 2]; A available from: http://www.skmtglossary.org/ [Google Scholar]
- 2.Elkin PL, et al. Aequus communis sententia: defining levels of interoperability. Stud Health Technol Inform 2007; 129: 725–729 [PubMed] [Google Scholar]
- 3.Kalra D. Semantic interoperability deployment and research roadmap. EU workshops in Brussels. 2007 [Google Scholar]
- 4.ISO 18104: 2003 Health informatics – integration of a reference terminology model for nursing. International Organization for Standardization, Geneva, Switzerland [Google Scholar]
- 5.Goossen WTF, Goossen-Baremans AT, van der Zel M. Detailed clinical models: a review. Healthc Inform Res 2010; 12, 16(4): 201–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ISO/CEN/Working Draft 13972 Health Informatics – quality criteria and methodology for detailed clinical models draft materials. International Organization for Standardization, Geneva, Switzerland and the European Committee for Standardization, Brussels, Belgium [Google Scholar]
- 7.Oniki T. Clinical element models at Intermountain Healthcare. Paper presented at the EHR Symposium in Seoul. 2008 [Google Scholar]
- 8.openEHR Foundation openEHR clinical archetypes [cited 2010 May 26]; Available from:http://www.ope nehr.org/knowledge/
- 9.Hoy D. Hardiker NR, McNicoll IT, Westwell P.A feasibility study on clinical templates for the national health service in Scotland. Stud Health Technol Inform 2007; 129: 770–774 [PubMed] [Google Scholar]
- 10.Center for Interoperable EHR CiEHR Clinical Contents Manager. Seoul, Korea, Web documents [cited 2010 November 26]; Available from:http://www.Clinicalcontentsmodel.org/main.php
- 11.Health Level 7 Normative Edition of the HL7 Standards 2010. Ann Arbor, HL7 international. [cited 2010 November 21]; Available from: http://www.hl7.org [Google Scholar]
- 12.Goossen WTF. Using detailed clinical models to bridge the gap between clinicians and HIT. In: De Clercq E, et al. (Eds) Collaborative patient centered eHealth. Proceedings of the HIT@Healthcare 2008. IOS press; Amsterdam, 3–10 [PubMed] [Google Scholar]
- 13.Kooij J van der, Goossen WTF, Goossen-Baremans ATM, Plaisier N. Evaluation of documents that integrate knowledge, terminology and information models. : Park HA, Murray P, Delaney C. (Eds). Consumer-centered computer-supported care for healthy people. Proceedings of NI 2006. Amsterdam; etc.IOS Press; Stud Health Technol Inform, 2006; 122: 519–522 [PubMed] [Google Scholar]
- 14.Hovenga E, Garde S, Heard S. Nursing constraint models for electronic health records: a vision for domain knowledge governance. Int J Med Inform 2005; 74: 886–898 [DOI] [PubMed] [Google Scholar]
- 15.Min YH, Park HA. Development and validation of archetypes for nursing problem in breast cancer patients. J Korean Soc Med Inform 2009; 15: 393–401 [Google Scholar]
- 16.ISO/TS 22789:2010 Health informatics – conceptual framework for patient findings and problems in terminologies. International Organization for Standardization, Geneva, Switzerland [Google Scholar]
- 17.ISO 21090: 2011 Health informatics – harmonized data types for information interchange. International Organization for Standaradization, Geneva, Switzerland: [Google Scholar]
- 18.Kang YM, et al. A case of aplastic anemia in pregnancy refractory to platelet transfusion. Korean J Obstet Gynecol 2006; 49: 182–187 [Google Scholar]
- 19.Knoche A, Selzer C, Smolley K. Methods of stimulating the onset of labor: an exploration of maternal satisfaction. J Midwifery Women’s Health 2008; 53: 381–387 [DOI] [PubMed] [Google Scholar]


