Abstract
Developmental dysplasia of the hip (DDH) denotes a wide spectrum of conditions ranging from subtle acetabular dysplasia to irreducible hip dislocations. Clinical diagnostic tests complement ultrasound imaging in allowing diagnosis, classification and monitoring of this condition. Classification systems relate to the alpha and beta angles in addition to the dynamic coverage index (DCI). Screening programmes for DDH show considerable geographic variation; certain risk factors have been identified which necessitate ultrasound assessment of the newborn. The treatment of DDH has undergone significant evolution, but the current gold standard is still the Pavlik harness. Duration of Pavlik harness treatment has been reported to range from 3 to 9.3 mo. The beta angle, DCI and the superior/lateral femoral head displacement can be assessed via ultrasound to estimate the likelihood of success. Success rates of between 7% and 99% have been reported when using the harness to treat DDH. Avascular necrosis remains the most devastating complication of harness usage with a reported rate of between 0% and 28%. Alternative non-surgical treatment methods used for DDH include devices proposed by LeDamany, Frejka, Lorenz and Ortolani. The Rosen splint and Wagner stocking have also been used for DDH treatment. Surgical treatment for DDH comprises open reduction alongside a combination of femoral or pelvic osteotomies. Femoral osteotomies are carried out in cases of excessive anteversion or valgus deformity of the femoral neck. The two principal pelvic osteotomies most commonly performed are the Salter osteotomy and Pemberton acetabuloplasty. Serious surgical complications include epiphyseal damage, sciatic nerve damage and femoral neck fracture.
Keywords: Developmental dysplasia of the hip, Congenital, Pavlik harness, Ultrasound screening, Pelvic osteotomy
INTRODUCTION
Developmental dysplasia of the hip (DDH) denotes a wide spectrum of pathologic conditions, ranging from subtle acetabular dysplasia to irreducible hip dislocation with proximal femoral displacement[1]. The reported incidence of DDH varies from 1.5 to 2.5 per 1000 live births[1-3]. Unlike “congenital dysplasia of the hip”, DDH is not restricted to congenital malformation, but also includes developmental disturbance[4]. The radiological definition relies on the presence of an intact Shenton line (Figure 1)[5]. The Shenton line remains intact in “subluxation” but disrupted in “dysplasia”[6]. The term dysplasia tends to be used for a hip with a positive Ortolani sign, i.e., a dislocated hip that can be relocated back into the acetabulum. The typical dysplastic hip has a ridge in the superior-posterior and inferior aspects of the acetabulum. The ridge, or neo-limbus, as described by Ortolani, is composed of very cellular hyaline cartilage. The femoral head glides in and out of the acetabulum, producing the palpable sensation known as Ortolani’s sign. An additional diagnostic test used to detect dysplasia is the “Barlow manoeuvre”, whereby hip flexion and adduction causes the femoral head to leave the acetabulum[7]. Good evidence exists to suggest that untreated dysplasia will culminate in degenerative joint disease. The term “dislocation” is reserved for any hip with a negative Ortolani’s sign, i.e., an unreducible hip, that is associated with “secondary adaptive changes of shortening, decreased abduction and asymmetry of the folds”[8].
Figure 1.
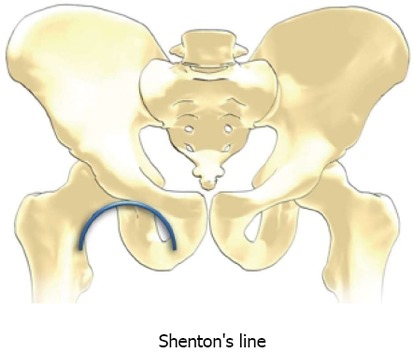
Diagram to demonstrate location of Shenton line. Shenton line is disrupted in developmental dysplasia of the hip[5].
CLASSIFICATION OF DDH
Graf classified DDH according to various ultrasound measurements (Table 1). The infant remains in a lateral decubitus position and coronal images are taken with subsequent measurement of alpha and beta angles[9]. The alpha angle refers to the angle between the acetabular roof and vertical cortex of the ilium. The beta angle is the angle formed between the vertical cortex of the ilium and the triangular labral fibrocartilage (echogenic triangle). Type 1 hips are deemed mature, type 3 are referred to as immature (Table 1). Dynamic coverage index (DCI) refers to ultrasound measured femoral head coverage with the hip in coronal flexion and adduction. Grill et al[10] and Alexiev et al[11] used DCI to help formulate a DDH classification system. DCI was greater than 50% in stable hips, DCI was 30%-50% in moderate subluxation, DCI was 10%-35% for severe subluxation; DCI was less than 10% for dislocation.
Table 1.
The Graf classification[11]
| Graf type | Angles |
| All type I | Alpha angle > 60 degrees (normal) |
| Type Ia | Beta angle < 55 degrees |
| Type Ib | Beta angle > 55 degrees |
| All type II | |
| Type IIa | Alpha angle 50-59 degrees |
| Type IIb | Alpha angle 50-59 degrees |
| Type IIc | Alpha angle 43-49 degrees |
| Beta angle < 77 degrees | |
| Type D ("about to decenter") | Alpha angle 43-49 degrees |
| Beta angle > 77 degrees | |
| Type III | Alpha angle < 43 degrees |
| Type IIIa and IIIb distinguished on the grounds of structural alteration of the cartilaginous roof | |
| Type IV (dislocated with labrum interposed between femoral head and acetabulum) | Alpha angle < 43 degrees |
SCREENING FOR DDH
Screening for DDH may be based upon clinical and/or ultrasound methodology. With clinical screening only, the late dislocation rate is reported as between 0.5 and 0.8 per 1000 live births[9,12]. Some studies[13,14] have suggested that clinical examination for DDH should be delayed until after the newborn period, due to the high rate of spontaneous stabilisation in the first 4 wk of life. Vedantam et al[15] suggested that dislocatable hips at birth could be safely monitored with ultrasound for two weeks before determining the course of treatment, reducing the number of infants requiring treatment, without prejudicing the final outcome. Clegg et al[16] reported a late dislocation rate of 0% in the 11-year history of their universal ultrasound screening program, but an operative rate of 0.21/1000 live births. They attempted to make a financial case for universal ultrasound screening due to reduction in mean surgical cost by earlier diagnosis of dysplasia/dislocation with subsequent need for fewer, less invasive procedures. Universal ultrasound screening of newborns however, is not deemed cost-effective by most North American authors, although in Europe, non-selective screening is more widely used[17]. van der Sluijs et al[13] reported the terms of the Dutch screening programme, which recommended clinical and ultrasound screening of infants between the ages of three and five months with one or more of the following risk factors: breech delivery, family history, leg length discrepancy or limited abduction of the hip. The current United Kingdom programme recommends ultrasound screening of high risk infants at six weeks[18,19]. Sampath et al[14] reported a late dislocation rate of 0.22-0.68/1000 live births in selective ultrasound screening programs.
NON-SURGICAL TREATMENT OF DDH: "A HISTORICAL EVOLUTION"
The treatment of children with DDH evolved markedly during the last century. Lorenz first proposed his method of forceful closed reduction and plastering in fixed maximal abduction. At the turn of the last century, most infants were not diagnosed to have dysplasia/dislocation until they started walking. The early 1900’s saw the advent of the radiograph and blood transfusion, facilitating lower rates of morbidity from open reductions. Ortolani was the first to highlight the recognition of dislocation in infants below the age of 12 mo, using the clinical manoeuvre that would come to bear his name. He supplemented this with his own version of an abduction brace.
In the 1950’s, Arnold Pavlik published articles on hip dysplasia and “functional treatment” in response to high rates of avascular necrosis (AVN) and failed reductions using previous conservative treatments[2]. A system of a harness and stirrups was developed which is still in use today. The Pavlik harness is well established as the orthosis of choice for infants with DDH superseding multiple preceding devices[4,10,20-30]. The concept of manual, forceful reduction of the infant’s hip with maintenance of limb flexion and abduction was updated to one of hip movement (“dynamic splintage”) within a non-pathological range. This reduces the hip and corrects the acetabular dysplasia whilst also minimising the risk of femoral head AVN[7]. The principle centres upon the hip being a “basic joint of movement”. Therefore, active and spontaneous motion results in “non-violent and unforced abduction and reduction”. His landmark paper, Zeitschrift fur Orthopaedie, reported on 1912 hips, with an 85% rate of successful reduction and a 2.8% rate of AVN. This is in marked contrast to success rates of 30% using previously prevalent “passive mechanical” methods[9].
The Pavlik harness consists of two shoulder straps crossing on the back and fastened to a broad thoracic belt anteriorly (Figure 2)[31]. The legs are held in slings consisting of two straps and the hips are flexed to at least 90°. This flexion lines the proximal femoral metaphysis to point towards the triradiate cartilage, the conjoined physeal plate of the pelvic bones. The anterior strap keeps the hips in flexion, limiting extension. The posterior strap is adjusted to stop the lower limb breaking the midline, i.e., to prevent adduction, rather than forcing abduction. Grill et al[10] noted that this is remarkably similar to the position of prenatal flexion of the thigh and the position of babies when traditionally carried on a mothers’ back[2,32].
Figure 2.
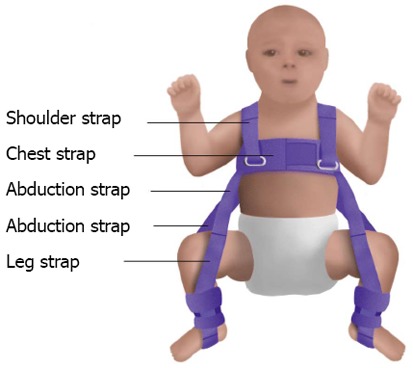
The Pavlik harness[31].
The main objective of harness application remains atraumatic, expedient relocation and maintenance of the hip to resume normal development. Controlled reduction of the hip depends primarily on flexion and passive abduction. The concept of a “safe zone” for this movement was defined by Ramsey et al[27] as the “arc between the angle of abduction that can be comfortably attained and the angle that allows redislocation”. Suzuki et al[33] reported that in some cases of dislocation, AVN rates could be reduced by the use of under thigh pillows during harness application. However, in cases of severe dislocation, some groups have stated that prevention of extreme abduction with under thigh pillows, was useless in reducing AVN[32]. In such cases, factors such as an inverted labrum, intraarticular interposition of pulvinar, elevated transverse ligament and hypertrophied round ligament are thought to be involved in the pathogenesis of AVN[3].
Weinstein et al[2] first highlighted the importance of quadriceps and gluteal muscle activity for optimal harness function. Iwaya et al[34] attributed the activity of the hamstrings in reducing dislocation. Relief of the adductor contracture was recognised by Pavlik as being indispensable for reduction. Early studies suggested that this was achieved via spontaneous lower limb movements. Modern thinking suggests the weight of the lower extremities plays a more significant role.
Use of the Pavlik harness is contraindicated when there is a major muscle imbalance, as in myelomeningocele (L2 to L4 functional level); major stiffness, as in arthrogryposis; or ligamentous laxity; as in Ehlers-Danlos syndrome[2].
PAVLIK HARNESS TREATMENT REGIMES
Various studies have recommended different durations of harness treatment. Erlacher[30] instructed his patients to wear the harness for approximately 6 mo, whilst Hirsch et al[35] believed in an average duration of 3 mo. Others have proposed regimes centred upon age at initiation of harness. Mubarak et al[36] suggested the harness should be worn for at least 3 mo by children younger than 3 mo of age, whereas in children older than 4 mo, it should be worn for approximately double their age. They proposed weekly follow up with ultrasonography and appropriate harness adjustment. They believed such a regime would normally achieve hip stability within three weeks in cases of newborn true dislocation. Ramsey et al[27] recommended a mean treatment duration of 3.6 mo when treatment commenced before 1 mo, 7.0 mo between 1 and 3 mo, and 9.3 mo between 3 and 9 mo.
van der Sluijs et al[13] noted that one disadvantage of prolonged harness treatment destined to failure was a delay in the management of DDH using alternative strategies which could potentially be successful. Closed reduction at increasing ages is problematic, resulting in an increased incidence of open reductions and possibly higher rates of AVN. They concluded that the use of the Pavlik harness could be prolonged in patients with Graf type III hips only if physical examination and ultrasonography showed improvement. A number of studies, including one in a cohort of Graf type III/IV hips by Uçar et al[37] report that the likelihood of Pavlik harness treatment leading to a stable reduction markedly decreases after 3-4 wk duration. If the hip is not improved or reduced after 3 wk, some studies have suggested that the use of the harness be discontinued and the treatment plan changed[3,12,27,37-39].
MONITORING PAVLIK HARNESS TREATMENT WITH IMAGING
Grissom et al[40] and Polanuer et al[41] reported the results of ultrasound evaluation of the harness treatment in two cohorts of fifty patients. Their subjects remained in the harness with periodic adjustments to ensure proper fit and position with interval radiographs to monitor hip position. Ultrasound was deemed particularly useful in allowing good antero-posterior assessment of femoral-acetabular association in two dimensions. Several papers have reported the increased sensitivity of ultrasound scanning when compared with clinical examination[40,42]. One such study reported 100% sensitivity and 94% specificity for all dislocation/significant instability and noted the benefit of ultrasound monitoring for visualisation of soft tissue structures alongside the ability to assess hip position during harness adjustment. Viere et al[43] described “surreptitious reduction” as the process whereby hips treated by the harness remain dislocated and locked behind the posterior rim of the acetabulum. Ultrasound allows visualisation of such cases which can result in posterolateral acetabular deficiency with prolonged harness use.
Suzuki[44] reported the use of ultrasound in providing us with an indication of the likelihood of harness success by identifying three degrees of residual head displacement. Type A dislocations demonstrate contact between the femoral head and the acetabular wall, with no significant obstruction to the head returning to the bottom of the fossa. In type B dislocations the femoral head contacts the posterior margins of the socket. In type C dislocations the femoral head is displaced outside the socket, with its centre posterior to the acetabular rim. They suggested that the Pavlik harness was indicated in type A hips, appropriate for type B hips along with daily ultrasound monitoring and contraindicated in type C hips.
Whilst many authors showed that static ultrasound imaging could be a reliable way of detecting abnormality, Engesaeter et al[45] and Dias et al[46] reported poor reliability of static ultrasound and advocated solely dynamic assessment. A landmark study by Graf indicated that static and dynamic images should be used in conjunction[47]. Some studies have suggested the use of ultrasound in the prediction of poor acetabular development after walking age[11,48]. At a mean follow-up of 5 years, Alexiev et al[11] found that dynamic sonographic measures of stability such as a reduced DCI < 22% and a beta angle of < 43° showed 100% sensitivity for medium-term instability. They suggested that increased echogenicity of the cartilaginous roof on initial ultrasound was the most specific single predictor of residual dysplasia (sensitivity 100% and specificity 88%). The structurally normal cartilaginous roof is non-echogenic except for the labrum and ultrasound showed that in all successfully reduced hips in this series[11], the echogenic cartilage reverted to non-echogenic tissue. White et al[49] agreed that a DCI < 22% was predictive of failure. An inverted labrum and superior femoral head displacement correlated with poor outcome. Authors reported that a femoral head positioned below the labrum was strongly correlated with Pavlik harness success. They found that hips which displayed Pavlik failure had a significantly greater beta angle and significantly less lateral femoral head coverage at the time of presentation. Such cases are more likely to have an inverted labrum and to present later. They identified two new ultrasonographic markers, superior femoral head displacement relative to the labrum and total femoral head displacement. They found the latter to be the more reliable marker of failure.
The use of ultrasonography is not problem-free. Gwynne Jones[48] showed the considerable inter- and intra-observer variability of ultrasound measurement in neonatal hips. Ultrasound can detect abnormalities in the first few weeks of life which resolve spontaneously and scans at 4, 6 or 9 wk are more specific than earlier scans but this limits usefulness in screening.
In spite of these issues, many authors agree that the use of ultrasonography is the most significant development in the management of DDH since the development of the Pavlik harness itself[50-53].
PAVLIK HARNESS TREATMENT OUTCOMES
Overall, success rates of 7%-99% have been reported in cases of DDH using the Pavlik harness[8,38,39,54-58]. Certain studies have given lower peak success rates of 50%-80%[8,13,15,43,59]. Weinstein et al[2] highlighted the role of the harness in infants with limited hip abduction and documented acetabular dysplasia with or without subluxation. Following appropriate harness application, the contracted hip adductors stretch, allowing a full range of abduction within two weeks. Relief of adductor contracture is a key component of success, necessitating adductor tenotomy in some instances as originally proposed by Pavlik.
Failure of the device has been linked to improper use and poor compliance as noted by Lerman et al[38] and Mubarak et al[36]. The reported incidence of AVN ranges from 0%-28%[60-64]. Use of the Pavlik harness is associated with excessive flexion causing injury to the femoral nerve, excessive abduction causing AVN, and conversely insufficient flexion or abduction for maintenance of a stable reduction[65]. The maximum period for use of the harness is unknown. Some studies have suggested that long-term unsuccessful treatment is associated with a high rate of AVN, deformity of the femoral head and deficiency of the posterior acetabulum. van der Sluijs et al[13] disagreed with this and suggested that continued use of the harness could increase the number of successful reductions as long as abduction of the hip was continually improving, without risk of AVN or residual dysplasia[66]. By 12 wk, they reported that half of the type III hips which eventually responded to bracing were not yet reduced. Consequently, a substantial proportion of these hips would have been potentially treated by surgery if Pavlik harnessing was limited to the conventional 4 wk. They reported that development of the hip was related to Graf type, rather than duration of bracing. The authors reported that prolonged bracing did not increase AVN, with their rates of AVN in Graf type III and IV hips (16%), being equivalent to that of a previous study[33] where bracing was shorter. Suzuki[44] described the “type 1 error”, occurring with incorrect prolonged use of the Pavlik harness in hips that remained unreduced in a posteriorly dislocated position. In such hips, the femoral head became adherent to the posterior capsule. This was reported to require open reduction from an anterior approach. The “type 2 error” occurs in hips that are too loose for successful treatment with the harness and require a more stable orthosis. Excessive duration of Pavlik harness use can therefore lead to erosion of the posterior acetabulum. Swaroop et al[18] highlighted the benefits of ultrasound in recognising failed improvement in abduction at three weeks.
The treatment of dislocated but reducible hips has proved problematic, with previous studies reporting success rates of 60%-70%[67,68]. The failed cases ultimately require operative treatment with closed or open reduction and hip spica casting. Swaroop et al[18] reported an increase in successful reductions of Ortolani positive hips, with two specific changes in treatment protocol; routine use of serial office based ultrasound examinations and transition to fixed hip abduction orthosis in hips remaining stable after three weeks in a Pavlik harness. The use of abduction braces in failed Pavlik harness treatment is contentious. Hedequist et al[69] suggested that it may be successful because cases of inferior dislocation were often resistant to Pavlik treatment and could be aggravated by flexion. Whilst numerous studies have highlighted the increased risk of AVN with more rigid devices, Hedequist et al[69] and Eberle[70] reported on a series of Ortolani positive hips treated with rigid devices after Pavlik failure, who were followed up until the development of a normal appearing ossific nucleus. They reported no incidence of AVN in their patients. Clearly, the numbers in these series were small and further study could establish more accurate incidence of AVN with abduction orthosis.
CONSEQUENCES OF PAVLIK HARNESS FAILURE
Harness failure has historically been associated with impaired femoral head/acetabular development and AVN. Rates of AVN following Pavlik treatment vary widely in historical studies from 0% to 28%[23,24,27,71], due to differences in definition of AVN and length of follow-up, indication for treatment and severity of dislocation.
The diagnosis of AVN has traditionally been made according to the Salter criteria[63]: (1) Failure of appearance of the ossific nucleus of the femoral head during 1 year or more after reduction; (2) Failure of growth in an existing ossific nucleus during 1 year or more after reduction; (3) Broadening of the femoral neck during 1 year after reduction; (4) Increased radiographic density of the femoral head followed by the radiographic appearance of fragmentation; and (5) Residual deformity of the femoral head and neck when reossification is complete.
Early studies did not analyse the reasons for any failure. Felipe and Carlioz mentioned 7 failures in 112 hips without discussing contributing factors or subsequent management, whilst the European Paediatric Society reported a failure rate of 14%, and also did not analyse reasons for failures[43]. An early study by Wilkinson suggested that an irreducible dislocation (Ortolani negative) hip was a contraindication to the use of the harness. Others[2,8,38,59,63,72] have disagreed. Viere et al[43] reported an early series in which despite recognition of an increased risk of harness failure, 11 of 27 such patients were treated successfully with the harness. They recommended a harness trial in patients with an Ortolani negative dislocation below the age of 7 mo, with discontinuation of treatment if concentric reduction was not achieved within 4 wk.
A number of early studies have highlighted delay in treatment beyond the age of 3 wk[67] and 7 wk[43], poor stability of the reduced hip, the initial acetabular index and an Ortolani negative clinical examination as risk factors for Pavlik harness failure[63]. Inoue et al[73] highlighted poor treatment technique, including improper application of the harness leading to rigid fixation of the hip in a “frog-leg” position. Traditionally, there have been differing opinions concerning the relationship between instability and acetabular dysplasia, with some authors finding that instability could lead to dysplasia[63,74] and vice-versa[33,59].
Male gender is a recently cited factor[75] with some disagreement between studies[38]. Viere et al[43] and Lerman et al[38] found a statistically increased likelihood of failure with bilateral involvement, whereas Harding et al[67] and more recently, Borowski et al[76] found no increased association with bilaterality. A retrospective study by Kitoh et al[7] found that patients with bilateral DDH were approximately six times as likely to fail Pavlik harness treatment as those with unilateral DDH, whereas Borowski et al[76] found no significant association. Despite progression in radiological imaging, a number of studies have reported the severity of initial clinical examination to be the most powerful univariate predictor of failure of Pavlik harness treatment[38,43].
ALTERNATIVE NON-SURGICAL TREATMENT METHODS FOR DDH
Historically, there have been a number of alternative reduction devices used in DDH, such as stirrup devices proposed by LeDamany, Frejka, Lorenz and Ortolani[72]. However, the majority of the literature has shown the Pavlik harness to be superior in terms of successful reduction and AVN rates. The Frejka pillow for example has been associated with poor outcomes and high rates of AVN because it has the tendency to forcibly abduct the hips. Czubak et al[77] showed 89% successful reduction using the Frejka pillow, compared to 95% with the Pavlik harness and found the Pavlik harness to be more effective in hips diagnosed before 24 wk. They noted AVN in 12% and 7% of hips treated with the Frejka pillow and Pavlik harness respectively. The Rosen splint[72] is still used in many Scandinavian centres. Whilst reported to have high rates of success and few complications, it is only of use in newborns. Its use otherwise is associated with AVN and increased risks of skin irritation and pressure sores[18].
Recently various devices essentially based on the Pavlik harness have shown promising results. The “Wagner stocking” was reported by Pach et al[78] to have high rates of successful reduction and AVN rates in the region of 2.6%, comparable to some studies of the Pavlik harness. Clearly the evidence behind this is small compared to that concerning the Pavlik harness and longitudinal studies of outcomes are needed for significant comparison.
SURGICAL TREATMENT OF DDH
Failure to achieve hip reduction via closed techniques may dictate surgical open reduction techniques combined with femoral or pelvic osteotomy. Femoral osteotomies are performed to correct excessive anteversion or valgus deformity of the femoral neck. The pelvic osteotomies principally used for DDH include: (1) Salter innominate osteotomy[79-91] or (2) Pemberton pericapsular osteotomy[83,92-94]. Selection of a or b has been linked to the acetabular index (Figure 3)[31,95]. The Acetabular Index is the angle between the Hilgenreiner line and a line drawn from the triradiate epiphysis to the lateral edge of the acetabulum. This angle should decline with age and typically is less than 20 degrees by the time the child is 2-year-old. The Pemberton osteotomy tends to be favoured in cases where the acetabular index is greater than 40 degrees[96]. The Salter osteotomy is an open wedge osteotomy which retroverts and extends the acetabulum around a fixed axis such that the acetabular roof covers the femoral head both superiorly and anteriorly[97,98]. This osteotomy is designed to deliver more anterior femoral head coverage with less posterior coverage provided par consequence. Success depends upon a mobile pubic symphysis[99]. Böhm et al[100] reviewed the cases of 61 patients who had 73 Salter osteotomies and reported 15 failures; defined by the need for revision surgery or obtaining a Harris Hip Score of less than 70 points. The Pemberton Osteotomy is an incomplete transiliac osteotomy which starts approximately 10 mm superior to the anterior inferior iliac spine and advances posteriorly, ending at the ilioischial limb of the triradiate cartilage[101]. Wu et al[102] evaluated the results of 106 children (116 hips) with DDH treated with a Pemberton acetabuloplasty, reporting good to excellent results in 87% (with follow up ranging from 2 to 10 years). Complications of surgery for DDH include: AVN of the femoral head, sciatic nerve damage, K-wire breakage or migration, damage to the epiphyseal centre, femoral fracture and leg-length discrepancy[83].
Figure 3.
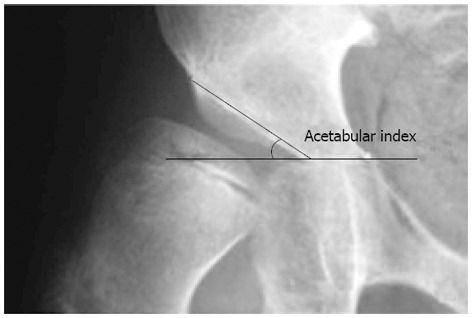
Calculation of acetabular index[95].
CONCLUSION
DDH refers to a broad spectrum of conditions from mild acetabular dysplasia to irreducible hip dislocation. Screening programmes for DDH still vary worldwide and more large-scale, longitudinal studies are needed to allow standardisation of policy across regions. Ultrasound imaging allows DDH classification based upon alpha/beta angles and the DCI. The appropriate management of DDH can have lasting consequences for lifetime morbidity. Non-surgical treatment methods for DDH have undergone historical evolution with the Pavlik harness remaining the treatment of choice worldwide. The Pavlik harness has undoubtedly led to progression in the successful treatment of DDH with a reduction in the incidence of short-term complications and developmental disturbance. Pavlik harness treatment does require meticulous clinical follow up often in conjunction with routine ultrasound imaging. Harness failure can however lead to femoral and acetabular developmental disturbance along with devastating AVN. Alternative non-surgical treatment methods have been reported for DDH such as the Wagner stocking and Frejka Pillow. Surgical management is a last resort for patients where harness treatment has failed. A combination of open reduction with femoral/pelvic osteotomy may be required.
Footnotes
P- Reviewers Kongtawelert P, Trieb K S- Editor Song XX L- Editor A E- Editor Xiong L
References
- 1.Ponseti IV. Morphology of the acetabulum in congenital dislocation of the hip. Gross, histological and roentgenographic studies. J Bone Joint Surg Am. 1978;60:586–599. [PubMed] [Google Scholar]
- 2.Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: Part II. Instr Course Lect. 2004;53:531–542. [PubMed] [Google Scholar]
- 3.Suzuki S, Seto Y, Futami T, Kashiwagi N. Preliminary traction and the use of under-thigh pillows to prevent avascular necrosis of the femoral head in Pavlik harness treatment of developmental dysplasia of the hip. J Orthop Sci. 2000;5:540–545. doi: 10.1007/s007760070002. [DOI] [PubMed] [Google Scholar]
- 4.Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg. 2000;8:232–242. doi: 10.5435/00124635-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Gaillard F. Shenton’s Line [cited 2012 Sep 16] Available from: http: //radiopaedia.org/images/516.
- 6.Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;(175):79–85. [PubMed] [Google Scholar]
- 7.Kitoh H, Kawasumi M, Ishiguro N. Predictive factors for unsuccessful treatment of developmental dysplasia of the hip by the Pavlik harness. J Pediatr Orthop. 2009;29:552–557. doi: 10.1097/BPO.0b013e3181b2f200. [DOI] [PubMed] [Google Scholar]
- 8.Gabuzda GM, Renshaw TS. Reduction of congenital dislocation of the hip. J Bone Joint Surg Am. 1992;74:624–631. [PubMed] [Google Scholar]
- 9.Pavlik A. The functional method of treatment using a harness with stirrups as the primary methods of conservative therapy for infants with congenital dislocation of the hip. Z Orthop Ihre Grenzgeb. 1957;89:341–352. [PubMed] [Google Scholar]
- 10.Grill F, Bensahel H, Canadell J, Dungl P, Matasovic T, Vizkelety T. The Pavlik harness in the treatment of congenital dislocating hip: report on a multicenter study of the European Paediatric Orthopaedic Society. J Pediatr Orthop. 1988;8:1–8. doi: 10.1097/01241398-198801000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Alexiev VA, Harcke HT, Kumar SJ. Residual dysplasia after successful Pavlik harness treatment: early ultrasound predictors. J Pediatr Orthop. 2006;26:16–23. doi: 10.1097/01.bpo.0000187995.02140.c7. [DOI] [PubMed] [Google Scholar]
- 12.Bjerkreim I, Hagen O, Konomou N, Kase T, Kristiansen T, Arseth P. Late Diagnosis of Developmental Dislocation of the Hip in Norway During the Years 1980-1989. J Pediatr Orthop B. 1993;2:112–114. [Google Scholar]
- 13.van der Sluijs JA, De Gier L, Verbeke JI, Witbreuk MM, Pruys JE, van Royen BJ. Prolonged treatment with the Pavlik harness in infants with developmental dysplasia of the hip. J Bone Joint Surg Br. 2009;91:1090–1093. doi: 10.1302/0301-620X.91B8.21692. [DOI] [PubMed] [Google Scholar]
- 14.Sampath JS, Deakin S, Paton RW. Splintage in developmental dysplasia of the hip: how low can we go? J Pediatr Orthop. 2003;23:352–355. [PubMed] [Google Scholar]
- 15.Vedantam R, Bell MJ. Dynamic ultrasound assessment for monitoring of treatment of congenital dislocation of the hip. J Pediatr Orthop. 1995;15:725–728. doi: 10.1097/01241398-199511000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Clegg J, Bache CE, Raut VV. Financial justification for routine ultrasound screening of the neonatal hip. J Bone Joint Surg Br. 1999;81:852–857. doi: 10.1302/0301-620x.81b5.9746. [DOI] [PubMed] [Google Scholar]
- 17.Smergel E, Losik SB, Rosenberg HK. Sonography of hip dysplasia. Ultrasound Q. 2004;20:201–216. doi: 10.1097/00013644-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Swaroop VT, Mubarak SJ. Difficult-to-treat Ortolani-positive hip: improved success with new treatment protocol. J Pediatr Orthop. 2009;29:224–230. doi: 10.1097/BPO.0b013e31819bcecf. [DOI] [PubMed] [Google Scholar]
- 19.Gray A, Elbourne D, Dezateux C, King A, Quinn A, Gardner F. Economic evaluation of ultrasonography in the diagnosis and management of developmental hip dysplasia in the United Kingdom and Ireland. J Bone Joint Surg Am. 2005;87:2472–2479. doi: 10.2106/JBJS.D.01997. [DOI] [PubMed] [Google Scholar]
- 20.Fried A, Seelenfreund M. The treatment of congenital dislocation of the hip by the Pavlik strap brace. Bull Hosp Joint Dis. 1969;30:153–163. [PubMed] [Google Scholar]
- 21.Hangen DH, Kasser JR, Emans JB, Millis MB. The Pavlik harness and developmental dysplasia of the hip: has ultrasound changed treatment patterns? J Pediatr Orthop. 1995;15:729–735. doi: 10.1097/01241398-199511000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Iwasaki K. Treatment of congenital dislocation of the hip by the Pavlik harness. Mechanism of reduction and usage. J Bone Joint Surg Am. 1983;65:760–767. [PubMed] [Google Scholar]
- 23.Johnson AH, Aadalen RJ, Eilers VE, Winter RB. Treatment of congenital hip dislocation and dysplasia with the Pavlik harness. Clin Orthop Relat Res. 1981;(155):25–29. [PubMed] [Google Scholar]
- 24.Kalamchi A, MacFarlane R. The Pavlik harness: results in patients over three months of age. J Pediatr Orthop. 1982;2:3–8. [PubMed] [Google Scholar]
- 25.McKinnon B, Bosse MJ, Browning WH. Congenital dysplasia of the hip: the lax (subluxatable) newborn hip. J Pediatr Orthop. 1984;4:422–426. doi: 10.1097/01241398-198408000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Rachbauer F, Sterzinger W, Klestil T, Krismer M, Frischhut B. Acetabular development following early treatment of hip dysplasia by Pavlik harness. Arch Orthop Trauma Surg. 1994;113:281–284. doi: 10.1007/BF00443818. [DOI] [PubMed] [Google Scholar]
- 27.Ramsey PL, Lasser S, MacEwen GD. Congenital dislocation of the hip. Use of the Pavlik harness in the child during the first six months of life. J Bone Joint Surg Am. 1976;58:1000–1004. [PubMed] [Google Scholar]
- 28.Mubarak SJ, Leach J, Wenger D. Management of congenital dislocation of the hip in the infant. Contemp Orthop. 1987;15:29–44. [Google Scholar]
- 29.Hensinger RN. Congenital dislocation of the hip. Clin Symp. 1979;31:1–31. [PubMed] [Google Scholar]
- 30.Erlacher PJ. Early treatment of dysplasia of the hip. J Internat Coll Surg. 1962;38:348–354. [Google Scholar]
- 31. Available from: http: //www.lpch.org/DiseaseHealthInfo/HealthLibrary/hrnewborn/0239-pop.html.
- 32.Herring JA. Developmental Dysplasia of the hip. In: Herring JA, editor. Tachdijan’s paediatrics orthopaedics. 3rd ed. Philadelphia: W.B. Saunders; 2002. pp. 513–654. [Google Scholar]
- 33.Suzuki S, Kashiwagi N, Kasahara Y, Seto Y, Futami T. Avascular necrosis and the Pavlik harness. The incidence of avascular necrosis in three types of congenital dislocation of the hip as classified by ultrasound. J Bone Joint Surg Br. 1996;78:631–635. [PubMed] [Google Scholar]
- 34.Iwaya T, Sakaguchi R, Tsuyama N. The treatment of congenital dislocation of the knee with the Pavlik harness. Int Orthop. 1983;7:25–30. doi: 10.1007/BF00267556. [DOI] [PubMed] [Google Scholar]
- 35.Hirsch PJ, Hirsch SA. The Pavlik Harness for hip dysplasia: A safe and rapid means of treatment. Orthop Rev. 1976;5:81–83. [Google Scholar]
- 36.Mubarak S, Garfin S, Vance R, McKinnon B, Sutherland D. Pitfalls in the use of the Pavlik harness for treatment of congenital dysplasia, subluxation, and dislocation of the hip. J Bone Joint Surg Am. 1981;63:1239–1248. [PubMed] [Google Scholar]
- 37.Uçar DH, Işiklar ZU, Kandemir U, Tümer Y. Treatment of developmental dysplasia of the hip with Pavlik harness: prospective study in Graf type IIc or more severe hips. J Pediatr Orthop B. 2004;13:70–74. doi: 10.1097/01202412-200403000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Lerman JA, Emans JB, Millis MB, Share J, Zurakowski D, Kasser JR. Early failure of Pavlik harness treatment for developmental hip dysplasia: clinical and ultrasound predictors. J Pediatr Orthop. 2001;21:348–353. [PubMed] [Google Scholar]
- 39.Wilkinson AG, Sherlock DA, Murray GD. The efficacy of the Pavlik harness, the Craig splint and the von Rosen splint in the management of neonatal dysplasia of the hip. A comparative study. J Bone Joint Surg Br. 2002;84:716–719. doi: 10.1302/0301-620x.84b5.12571. [DOI] [PubMed] [Google Scholar]
- 40.Grissom LE, Harcke HT, Kumar SJ, Bassett GS, MacEwen GD. Ultrasound evaluation of hip position in the Pavlik harness. J Ultrasound Med. 1988;7:1–6. doi: 10.7863/jum.1988.7.1.1. [DOI] [PubMed] [Google Scholar]
- 41.Polanuer PA, Harcke HT, Bowen JR. Effective use of ultrasound in the management of congenital dislocation and/or dysplasia of the hip. Clin Orthop Relat Res. 1990;(252):176–181. [PubMed] [Google Scholar]
- 42.Bialik V, Reuveni A, Pery M, Fishman J. Ultrasonography in developmental displacement of the hip: a critical analysis of our results. J Pediatr Orthop. 1989;9:154–156. [PubMed] [Google Scholar]
- 43.Viere RG, Birch JG, Herring JA, Roach JW, Johnston CE. Use of the Pavlik harness in congenital dislocation of the hip. An analysis of failures of treatment. J Bone Joint Surg Am. 1990;72:238–244. [PubMed] [Google Scholar]
- 44.Suzuki S. Ultrasound and the Pavlik harness in CDH. J Bone Joint Surg Br. 1993;75:483–487. doi: 10.1302/0301-620X.75B3.8496228. [DOI] [PubMed] [Google Scholar]
- 45.Engesaeter LB, Wilson DJ, Nag D, Benson MK. Ultrasound and congenital dislocation of the hip. The importance of dynamic assessment. J Bone Joint Surg Br. 1990;72:197–201. doi: 10.1302/0301-620X.72B2.2179221. [DOI] [PubMed] [Google Scholar]
- 46.Dias JJ, Thomas IH, Lamont AC, Mody BS, Thompson JR. The reliability of ultrasonographic assessment of neonatal hips. J Bone Joint Surg Br. 1993;75:479–482. doi: 10.1302/0301-620X.75B3.8496227. [DOI] [PubMed] [Google Scholar]
- 47.Graf R. Hip sonography--how reliable? Sector scanning versus linear scanning? Dynamic versus static examination? Clin Orthop Relat Res. 1992;(281):18–21. [PubMed] [Google Scholar]
- 48.Gwynne Jones DP, Vane AG, Coulter G, Herbison P, Dunbar JD. Ultrasound measurements in the management of unstable hips treated with the pavlik harness: reliability and correlation with outcome. J Pediatr Orthop. 2006;26:818–822. doi: 10.1097/01.bpo.0000234999.61595.ec. [DOI] [PubMed] [Google Scholar]
- 49.White KK, Sucato DJ, Agrawal S, Browne R. Ultrasonographic findings in hips with a positive Ortolani sign and their relationship to Pavlik harness failure. J Bone Joint Surg Am. 2010;92:113–120. doi: 10.2106/JBJS.H.01880. [DOI] [PubMed] [Google Scholar]
- 50.Sochart DH, Paton RW. Role of ultrasound assessment and harness treatment in the management of developmental dysplasia of the hip. Ann R Coll Surg Engl. 1996;78:505–508. [PMC free article] [PubMed] [Google Scholar]
- 51.Cashman JP, Round J, Taylor G, Clarke NM. The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. J Bone Joint Surg Br. 2002;84:418–425. doi: 10.1302/0301-620x.84b3.12230. [DOI] [PubMed] [Google Scholar]
- 52.Malkawi H. Sonographic monitoring of the treatment of developmental disturbances of the hip by the Pavlik harness. J Pediatr Orthop B. 1998;7:144–149. doi: 10.1097/01202412-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Taylor GR, Clarke NM. Monitoring the treatment of developmental dysplasia of the hip with the Pavlik harness. The role of ultrasound. J Bone Joint Surg Br. 1997;79:719–723. doi: 10.1302/0301-620x.79b5.7678. [DOI] [PubMed] [Google Scholar]
- 54.Mostert AK, Tulp NJ, Castelein RM. Results of Pavlik harness treatment for neonatal hip dislocation as related to Graf’s sonographic classification. J Pediatr Orthop. 2000;20:306–310. [PubMed] [Google Scholar]
- 55.Mafalda Santos M, Filipe G. Pavlik harness for congenital hip dislocation: long term results. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:41–50. [PubMed] [Google Scholar]
- 56.Murakami T, Katada S. A follow-up study of congenital dislocation of the hip using Pavlik harness. Clin Orthop Surg. 1991;26:136–140. [Google Scholar]
- 57.Kumazawa H, Yoshihashi Y. [Long-term results of congenital dislocation of the hip treated with Pavlik harness] Nihon Seikeigeka Gakkai Zasshi. 1991;65:851–861. [PubMed] [Google Scholar]
- 58.Fujioka F, Terayama K, Sugimoto N, Tanikawa H. Long-term results of congenital dislocation of the hip treated with the Pavlik harness. J Pediatr Orthop. 1995;15:747–752. doi: 10.1097/01241398-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Smith MA. Use of the Pavlik harness in nonoperative management of congenital dislocation of the hip. J R Soc Med. 1981;74:591–594. doi: 10.1177/014107688107400807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Suzuki S. Reduction of CDH by the Pavlik harness. Spontaneous reduction observed by ultrasound. J Bone Joint Surg Br. 1994;76:460–462. [PubMed] [Google Scholar]
- 61.Joseph K, MacEwen GD, Boos ML. Home traction in the management of congenital dislocation of the hip. Clin Orthop Relat Res. 1982;(165):83–90. [PubMed] [Google Scholar]
- 62.Gage JR, Winter RB. Avascular necrosis of the capital femoral epiphysis as a complication of closed reduction of congenital dislocation of the hip. A critical review of twenty years’ experience at Gillette Children’s Hospital. J Bone Joint Surg Am. 1972;54:373–388. [PubMed] [Google Scholar]
- 63.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg. 1969;12:44–61. [PubMed] [Google Scholar]
- 64.Segal LS, Boal DK, Borthwick L, Clark MW, Localio AR, Schwentker EP. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19:177–184. doi: 10.1097/00004694-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 65.Köse N, Omeroğlu H, Ozyurt B, Akçar N, Ozçelik A, Inan U, Seber S. [Our three-year experience with an ultrasonographic hip screening program conducted in infants at 3 to 4 weeks of age] Acta Orthop Traumatol Turc. 2006;40:285–290. [PubMed] [Google Scholar]
- 66.Graf R. Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg. 1984;102:248–255. doi: 10.1007/BF00436138. [DOI] [PubMed] [Google Scholar]
- 67.Harding MG, Harcke HT, Bowen JR, Guille JT, Glutting J. Management of dislocated hips with Pavlik harness treatment and ultrasound monitoring. J Pediatr Orthop. 1997;17:189–198. doi: 10.1097/00004694-199703000-00010. [DOI] [PubMed] [Google Scholar]
- 68.Tucci JJ, Kumar SJ, Guille JT, Rubbo ER. Late acetabular dysplasia following early successful Pavlik harness treatment of congenital dislocation of the hip. J Pediatr Orthop. 1991;11:502–505. doi: 10.1097/01241398-199107000-00016. [DOI] [PubMed] [Google Scholar]
- 69.Hedequist D, Kasser J, Emans J. Use of an abduction brace for developmental dysplasia of the hip after failure of Pavlik harness use. J Pediatr Orthop. 2003;23:175–177. [PubMed] [Google Scholar]
- 70.Eberle CF. Plastazote abduction orthosis in the management of neonatal hip instability. J Pediatr Orthop. 2003;23:607–616. doi: 10.1097/00004694-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 71.Filipe G, Carlioz H. Use of the Pavlik harness in treating congenital dislocation of the hip. J Pediatr Orthop. 1982;2:357–362. doi: 10.1097/01241398-198210000-00002. [DOI] [PubMed] [Google Scholar]
- 72.Mubarak SJ, Bialik V. Pavlik: the man and his method. J Pediatr Orthop. 2003;23:342–346. [PubMed] [Google Scholar]
- 73.Inoue T, Naito M, Nomiyama H. Treatment of developmental dysplasia of the hip with the Pavlik harness: factors for predicting unsuccessful reduction. J Pediatr Orthop B. 2001;10:186–191. [PubMed] [Google Scholar]
- 74.Wiersma JA. Use of the Pavlik splint in treatment of congenital dysplasia and dislocation of the hip in the newborn. J Am Osteopath Assoc. 1976;76:119–121. [PubMed] [Google Scholar]
- 75.Borges JL, Kumar SJ, Guille JT. Congenital dislocation of the hip in boys. J Bone Joint Surg Am. 1995;77:975–984. doi: 10.2106/00004623-199507000-00001. [DOI] [PubMed] [Google Scholar]
- 76.Borowski A, Thawrani D, Grissom L, Littleton AG, Thacker MM. Bilaterally dislocated hips treated with the Pavlik harness are not at a higher risk for failure. J Pediatr Orthop. 2009;29:661–665. doi: 10.1097/BPO.0b013e3181b528f8. [DOI] [PubMed] [Google Scholar]
- 77.Czubak J, Piontek T, Niciejewski K, Magnowski P, Majek M, Płończak M. Retrospective analysis of the non-surgical treatment of developmental dysplasia of the hip using Pavlik harness and Frejka pillow: comparison of both methods. Ortop Traumatol Rehabil. 2004;6:9–13. [PubMed] [Google Scholar]
- 78.Pach M, Kamínek P, Mikulík J. [Wagner stockings for the treatment of developmental dysplasia of the hip diagnosed early by general screening] Acta Chir Orthop Traumatol Cech. 2008;75:277–281. [PubMed] [Google Scholar]
- 79.Bursali A, Tonbul M. How are outcomes affected by combining the Pemberton and Salter osteotomies? Clin Orthop Relat Res. 2008;466:837–846. doi: 10.1007/s11999-008-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chukwunyerenwa CK, Sehgal R, Vioreanu M, Doyle F, Molony D, McCormack D. Less invasive innominate osteotomy. J Pediatr Orthop B. 2010;19:318–322. doi: 10.1097/BPB.0b013e3283345e55. [DOI] [PubMed] [Google Scholar]
- 81.Domzalski M, Synder M, Drobniewski M. Long-term outcome of surgical treatment of developmental dyplasia of the hip using the Dega and Salter method of pelvic osteotomy with simultaneous intratrochanteric femoral osteotomy. Ortop Traumatol Rehabil. 2004;6:44–50. [PubMed] [Google Scholar]
- 82.Eren A, Pekmezci M, Demirkiran G, Cakar M, Guven M, Yazici M. Modified Salter osteotomy for the treatment of developmental dysplasia of the hip: description of a new technique that eliminated the use of pins for internal fixation. J Bone Joint Surg Br. 2007;89:1375–1378. doi: 10.1302/0301-620X.89B10.18704. [DOI] [PubMed] [Google Scholar]
- 83.Ezirmik N, Yildiz K. Advantages of single-stage surgical treatment with salter innominate osteotomy and Pemberton pericapsular osteotomy for developmental dysplasia of both hips. J Int Med Res. 2012;40:748–755. doi: 10.1177/147323001204000240. [DOI] [PubMed] [Google Scholar]
- 84.Jäger M, Westhoff B, Zilkens C, Weimann-Stahlschmidt K, Krauspe R. [Indications and results of corrective pelvic osteotomies in developmental dysplasia of the hip] Orthopade. 2008;37:556–570, 572-574, 576. doi: 10.1007/s00132-008-1240-6. [DOI] [PubMed] [Google Scholar]
- 85.Liu TJ, Shi YY, Pan SN, Liu ZJ, Zhao Q, Zhang LJ, Ji SJ. [Evaluation of mid-term follow-up after Salter innominate osteotomy in developmental dysplasia of the hip] Zhonghua Waike Zazhi. 2010;48:1149–1153. [PubMed] [Google Scholar]
- 86.López-Carreño E, Carillo H, Gutiérrez M. Dega versus Salter osteotomy for the treatment of developmental dysplasia of the hip. J Pediatr Orthop B. 2008;17:213–221. doi: 10.1097/BPB.0b013e32830850eb. [DOI] [PubMed] [Google Scholar]
- 87.Maheshwari R, Madan SS. Pelvic osteotomy techniques and comparative effects on biomechanics of the hip: a kinematic study. Orthopedics. 2011;34:e821–e826. doi: 10.3928/01477447-20111021-12. [DOI] [PubMed] [Google Scholar]
- 88.Milasinović S. [Results of surgical treatment of developmental dysplasia of hip considering child's age] Srp Arh Celok Lek. 2011;139:58–63. doi: 10.2298/sarh1102058m. [DOI] [PubMed] [Google Scholar]
- 89.Pekmezci M, Yazici M. [Salter osteotomy: an overview] Acta Orthop Traumatol Turc. 2007;41 Suppl 1:37–46. [PubMed] [Google Scholar]
- 90.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am. 2007;89:2341–2350. doi: 10.2106/JBJS.F.00857. [DOI] [PubMed] [Google Scholar]
- 91.Tukenmez M, Tezeren G. Salter innominate osteotomy for treatment of developmental dysplasia of the hip. J Orthop Surg (Hong Kong) 2007;15:286–290. doi: 10.1177/230949900701500308. [DOI] [PubMed] [Google Scholar]
- 92.Cui S, Yu F, Li Q, Xu W, Xiao S, Huo Q. [Treatment of developmental dislocation of the hip with improved Pemberton method] Zhongguo Xiufu Chongjian Waike Zazhi. 2004;18:386–388. [PubMed] [Google Scholar]
- 93.Tavares JO. Modified Pemberton acetabuloplasty for the treatment of congenital hip dysplasia. J Pediatr Orthop. 2004;24:501–507. doi: 10.1097/00004694-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 94.Zhao HY, Li CS, Feng W, Yang C, Yu BF, Liu JG. [Simple Pemberton’s ilium osteotomy and combined unter-trochanter derotation-varisation osteotomy for developmental dysplasia of the hip] Zhongguo Gushang. 2012;25:287–290. [PubMed] [Google Scholar]
- 95.Ege R. Overview to pelvic osteotomies. In: Ege R, editor. Hip Surgery and Problems. Ankara: THK Press; 1994. pp. 313–329. [Google Scholar]
- 96.Rab GT. Containment of the hip: a theoretical comparison of osteotomies. Clin Orthop Relat Res. 1981;(154):191–196. [PubMed] [Google Scholar]
- 97.Salter RB, Dubos JP. The first fifteen year’s personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;(98):72–103. doi: 10.1097/00003086-197401000-00009. [DOI] [PubMed] [Google Scholar]
- 98.Salter RB. Innominate osteotomy in the treatment of congenital hip dislocation and subluxation of the hip. J Bone Joint Surg (Br) 1961;43:518–539. [PubMed] [Google Scholar]
- 99.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–420. [PubMed] [Google Scholar]
- 100.Böhm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg Am. 2002;84-A:178–186. [PubMed] [Google Scholar]
- 101.Tokgozoglu MN, Tokgozoglu AM. Pemberton Osteotomy. In: Ege R, editor. Hip Surgery and Problems. Ankara: THK Press; 1996. pp. 337–344. [Google Scholar]
- 102.Wu TN, Guo HY, Zhang YF. [Pemberton acetabuloplasty for treating the developmental dislocation of hip joint] Zhongguo Gushang. 2008;21:681–683. [PubMed] [Google Scholar]


