Abstract
All colorectal surgeons are faced from time to time with anastomotic leakage after colorectal surgery. This complication has been studied extensively without a significant reduction of incidence over the last 30 years. New techniques of prevention, by innovative anastomotic techniques should improve results in the future, but standardization and “teachability” should be guaranteed. Risk scoring enables intra-operative decision-making whether to restore continuity or deviate. Early detection can lead to reduction in delay of diagnosis as long as a standard system is used. For treatment options, no firm evidence is available, but future studies could focus on repair and saving of the anastomosis on the one hand or anastomotical breakdown and definitive colostomy on the other hand.
Keywords: Colorectal surgery, Complications, Postoperative care, Anastomotic leakage, Prevention
Core tip: This editorial covers the past achievements and future challenges in the field of colorectal anastomotic leakage. New anastomotic techniques and risk scores should improve incidence numbers and early detection, whereas future research could focus on preservation of the anastomosis in case of leakage.
INTRODUCTION
Anastomotic leakage after colorectal resection (CAL) is a dreaded complication and is reported to have a significant mortality (6%-22%)[1]. Morbidity is dramatically increased opposed to patients without CAL and leads to reoperations, radiological interventions and permanent stoma in 56%[2]. CAL is the leading cause of postoperative death after colorectal surgery, increases the risk of a permanent stoma significantly. Although available data on the effect of CAL on long-term oncologic outcome is not univocal, most papers on this topic report worse oncologic outcome in terms of increased local recurrence and negative association with survival[3]. Despite great numbers of studies investigating risk factors, surgical techniques and prevention of CAL, over the last three decades incidence has not reduced. In a recent publication by the Dutch Surgical Colorectal Audit incidence of CAL after restorative colon and rectum resections in 9192 registered patients in The Netherlands over 2010 was 8.7% (Table 1). Additionally, with patients expected to become older and to have more co morbidities, every patient but also every colorectal surgeon will increasingly be exposed to CAL and forthcoming difficulties in diagnosis and treatment. Incidence should be reduced and outcome must improve. Understanding current developments and its omissions will lead to design of relevant future research.
Table 1.
Number of colon and rectum resections in The Netherlands in 2011 and percentage anastomotic leakage n (%)
| Colon | Rectum | |||
| < 75 yr | ≥ 75 yr | < 75 yr | ≥ 75 yr | |
| Resections | 10249 (59.0) | 7246 (41.0) | 5076 (72.0) | 1933 (28.0) |
| Anastomotic leakage | 666 (7.4) | 449 (7.3) | 310 (11.4) | 55 (8.1) |
RISK FACTORS
Extensive literature is available on the topic of risk factors for anastomotic leakage. Among other factors are male gender, smoking, obesity, alcohol abuse, preoperative steroid and non-steroidal anti-inflammatory drugs use, longer duration of operation, preoperative transfusion, contamination of the operative field and timing during duty hour[4-7]. Increasingly, aspects of case volume for rectal surgery are discussed in respect to postoperative complications. Asteria et al[8] described case volume per centre < 20 is correlated to CAL. In line with this finding, Biondo et al[9] described in their study over 1046 emergency colorectal resection that CAL occurred less frequent in patients who were treated by specialized colorectal surgeons. Recently, risk factor studies have also been undertaken for laparoscopic colorectal surgery, identifying body mass index, tumour distance from the anal verge, tumour depth, and pelvic outlet as independent predictors for increased operative time and morbidity after laparoscopic total mesorectal excision[10]. Furthermore, American Society of Anesthesiologists III/IV patients and operative time longer itself are risk factors for CAL after laparoscopic colorectal surgery[11]. It is debatable whether leakage rates might have been lower if preoperative radio-chemotherapy is not applied as widely as is done nowadays, since neo-adjuvant therapy is one of the strongest risk factors amongst the above mentioned. This great abundance of literature does not provide colorectal surgeons with clear guidance in the decision of when to renounce from restorative surgery. To provide an objective assessment of the risk of anastomotic leakage, Dekker et al[12] developed and tested the Colon Leakage Score (CLS). In this score multiple risk factors were taken up and points were attributed to the patients per risk factor. As a predictor, CLS had an excellent area under the curve of the receiver-operating characteristics curve (AUC 0.95, 95%CI: 0.89-1.00), and an odds ratio of 1.74 (95%CI: 1.32-2.28). To our knowledge this tool is unique in its ability to detect high-risk patients preoperatively and objectively assesses the necessity for diverting ileostomy or non-restorative surgery.
SURGICAL TECHNIQUE
A recent review from our group addresses all the important steps that surgeons need to take into mind when creating a colorectal anastomosis[13]. Although some prerequisites should be present as adequate blood flow, without any tension in the absence of peritonitis, no clear value can be given for these aspects. When the little evidence that is available for the hand-sewn anastomosis is evaluated, it can be concluded that an inverting single layer continuous suture technique with slowly absorbable monofilament material seems preferable. Strong evidence lacks for other important aspects as distance from the suture to the edge of the anastomosis, distance between the sutures, layers included in the suture, suture tension and the optimal configuration. The highest level of evidence exists for the equality regarding to CAL of stapling vs hand sewn anastomosis, without evidence for one technique being superior to the other[14]. Following the above mentioned statements, currently stapling techniques might be of preference since the technique is uniform and easy to learn, making it ideal for comparing results between hospitals and surgeons and for teaching young surgeons.
There is a need for development of new techniques since all previous research has not lead to radically decreased leakage rates. Many experimental techniques have been investigated and some have shown at least equal result in comparison to hand-sewn techniques. Not many techniques tested in animal experiments have been translated to the human setting. Reasons for this could be that no standard models and robust translatable outcome measures exist for colorectal experiments. In humans, the so-called compression anastomosis is shown to have similar leakage rates compared to hand-sewn anastomosis[14,15]. Extra-luminal sealing using fibrin glue or acrylates have been reported mostly in animal studies, few reports on their use in human colorectal anastomosis have not shown beneficial effects on CAL[16]. Endo-luminal sealing by means of a biodegradable barrier has shown to be successfully applied in humans and a multicentre randomised clinical trial is currently being undertaken (Figure 1)[17].
Figure 1.
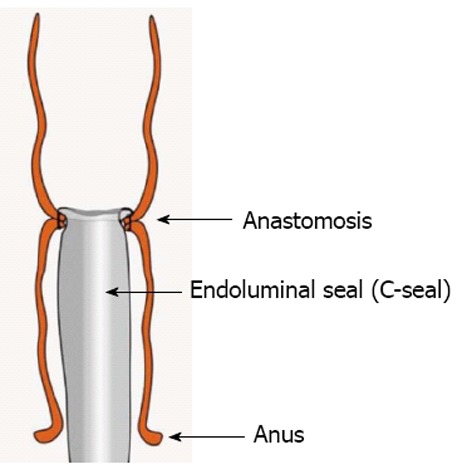
C-seal. Endoluminal biodegradable anastomotic cover. Printing with permission from Bakker et al[17].
Future studies should in our opinion focus on techniques that are easy to learn and have high reproducibility. To enhance reproducibility, animal studies should use the same animal models that are currently available or under construction.
EARLY DETECTION
Anastomotic leakage typically becomes clinically apparent between the 5th and the 8th postoperative day, but many exceptions exist, with one study even reporting a mean of the 12th postoperative day for the diagnosis of CAL[18]. Clinical signs of systemic inflammatory response syndrome, fever, ileus and pain are frequent but have low positive predictive value for CAL, when observed separately. In a study by den Dulk et al[19] these clinical features were combined into a clinical scoring system (Dutch Leakage Score), with which patients were scored daily in a systematical and uniform way. Points are attributed to certain clinical symptoms (i.e., fever, heart rate), nutritional status (signs of ileus, gastric retention, type of intake) and laboratory findings [i.e., C-reactive protein (CRP) level, leucocytes, kidney function]. After applying the score system retrospectively on a historical cohort, the score was used prospectively. It was shown that patients with a higher score were prone to CAL requiring intensive clinical observation or radiological evaluation (Figure 2). This scoring system reduced delay in diagnosis of anastomotic leak from 4 to 1.5 d, decreasing false negative diagnostic imaging representing a major factor of delay in diagnosis[20]. Although it is not known if the application of the score leads to an increase of negative imaging, the score could be especially beneficial in daily clinical practise where young doctors and nursing staff could identify high risk patients very easily and in a standardised manner. Furthermore, it could improve comparability of studies when applied more universally.
Figure 2.
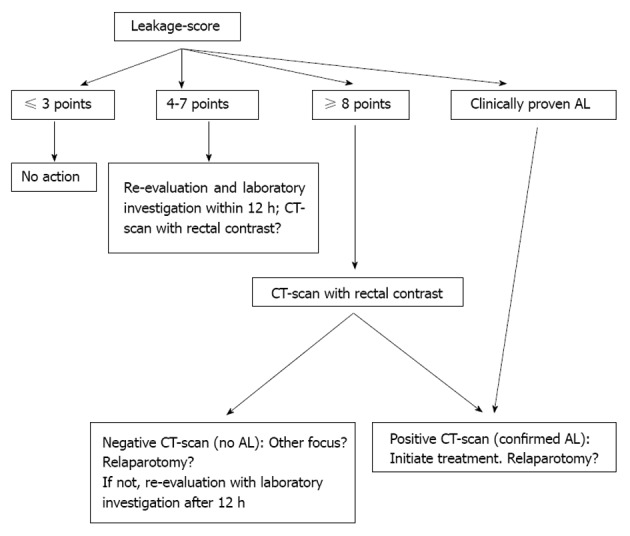
The Dutch Leakage Score. According to the points attributed to the patients on the basis of clinical symptoms, treating doctors can follow this diagnostic flowchart. Reprinted from den Dulk et al[19]. CT: Computed tomography; AL: Anastomotic leak.
This interval between surgery and clinical onset suggests a preclinical phase in which non-clinical methods could be used to predict CAL. Consequently, routine postoperative measurement of serum level CRP is studied for infectious complications after colorectal surgery in general and CAL in particular. In a meta-analysis by Warschkow et al[21] including six studies, a cut-off of 135 mg/L on postoperative day 4 resulted in a negative predictive value of 89% for infectious complications. CRP and other biochemical parameters detect systemic reactions, while other techniques are recently applied to detect local, juxta-anastomotical changes in metabolism and ischemia. Microdialysis of the peritoneal cavity is such a technique using an indwelling two-lumen catheter that detects changes in oxygenation locally at the site of anastomosis. Few studies have shown the ability to distinct patients with CAL after rectum resection from patients with an uncomplicated course, although these have insufficient samples to provide predictive values[22,23]. Future studies should focus on preclinical detection of CAL, since patients that are reoperated in an early phase could be protected from septic sequellae of clinical CAL.
TREATMENT
When facing and treating patients with CAL, surgeons have to take into account many different aspects, i.e., age, health status and current clinical condition of the patient, extent of dehiscence, time between operation and reoperation, indication of primary resection, presence of diverting stoma and localisation of the anastomosis. These variables lead to individualisation of treatment strategies and incomparable outcome. However, few studies, showing that surgeons believe that the anastomosis can be repaired rather than dismantled, have paved the way for a trial in which next to mortality and morbidity, preservation of the anastomosis could be one of the endpoints[24,25]. Difficulties in designing such a trial are the aforementioned large variety of clinical course, the unpredictability of CAL and the relatively low incidence of CAL per centre.
CONCLUSION
Colorectal anastomotic leakage is a serious complication that has great clinical impact on patients, putting surgeons in dilemmas of prevention, diagnosis and treatment. Many aspects of colorectal anastomotic leakage like etiology remain unclear. Current practise however should comprise intra-operative risk assessment and subsequent adaptation of operative technique when necessary. Current optimal suture technique appears to be using slowly absorbable monofilament sutures applied in a continuous, inverting, single layer manner or stapling. Postoperatively, early detection plays a key role and a leakage score system and routine laboratory tests (CRP at postoperative day 3-4) contribute strongly to it. When reoperating, sparing the anastomosis should be kept in mind as a valid treatment option, although more research is needed on which clinical state allows this option.
Footnotes
P- Reviewers Rege RV, Mayol J S- Editor Gou SX L- Editor A E- Editor Li JY
References
- 1.Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg. 1998;85:355–358. doi: 10.1046/j.1365-2168.1998.00615.x. [DOI] [PubMed] [Google Scholar]
- 2.Lindgren R, Hallböök O, Rutegård J, Sjödahl R, Matthiessen P. What is the risk for a permanent stoma after low anterior resection of the rectum for cancer? A six-year follow-up of a multicenter trial. Dis Colon Rectum. 2011;54:41–47. doi: 10.1007/DCR.0b013e3181fd2948. [DOI] [PubMed] [Google Scholar]
- 3.Walker KG, Bell SW, Rickard MJ, Mehanna D, Dent OF, Chapuis PH, Bokey EL. Anastomotic leakage is predictive of diminished survival after potentially curative resection for colorectal cancer. Ann Surg. 2004;240:255–259. doi: 10.1097/01.sla.0000133186.81222.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006;76:579–585. doi: 10.1111/j.1445-2197.2006.03780.x. [DOI] [PubMed] [Google Scholar]
- 5.Konishi T, Watanabe T, Kishimoto J, Nagawa H. Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg. 2006;202:439–444. doi: 10.1016/j.jamcollsurg.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 6.Buckley JE. Credibility and drug education: a critique and reformulation. Int J Addict. 1989;24:489–497. doi: 10.3109/10826088909081831. [DOI] [PubMed] [Google Scholar]
- 7.Gorissen KJ, Benning D, Berghmans T, Snoeijs MG, Sosef MN, Hulsewe KW, Luyer MD. Risk of anastomotic leakage with non-steroidal anti-inflammatory drugs in colorectal surgery. Br J Surg. 2012;99:721–727. doi: 10.1002/bjs.8691. [DOI] [PubMed] [Google Scholar]
- 8.Asteria CR, Gagliardi G, Pucciarelli S, Romano G, Infantino A, La Torre F, Tonelli F, Martin F, Pulica C, Ripetti V, et al. Anastomotic leaks after anterior resection for mid and low rectal cancer: survey of the Italian Society of Colorectal Surgery. Tech Coloproctol. 2008;12:103–110. doi: 10.1007/s10151-008-0407-9. [DOI] [PubMed] [Google Scholar]
- 9.Biondo S, Kreisler E, Millan M, Fraccalvieri D, Golda T, Frago R, Miguel B. Impact of surgical specialization on emergency colorectal surgery outcomes. Arch Surg. 2010;145:79–86. doi: 10.1001/archsurg.2009.208. [DOI] [PubMed] [Google Scholar]
- 10.Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T. Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery. 2009;146:483–489. doi: 10.1016/j.surg.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 11.Canelas A, Bun M, Laporte M, Peczan C, Rotholtz N. Laparoscopic emergency surgery for ulcerative colitis. Colorectal Dis. 2010;12:35. [Google Scholar]
- 12.Dekker JW, Liefers GJ, de Mol van Otterloo JC, Putter H, Tollenaar RA. Predicting the risk of anastomotic leakage in left-sided colorectal surgery using a colon leakage score. J Surg Res. 2011;166:e27–e34. doi: 10.1016/j.jss.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 2013;148:190–201. doi: 10.1001/2013.jamasurg.33. [DOI] [PubMed] [Google Scholar]
- 14.Lustosa SA, Matos D, Atallah AN, Castro AA. Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev. 2001;(3):CD003144. doi: 10.1002/14651858.CD003144. [DOI] [PubMed] [Google Scholar]
- 15.Påhlman L, Ejerblad S, Graf W, Kader F, Kressner U, Lindmark G, Raab Y. Randomized trial of a biofragmentable bowel anastomosis ring in high-risk colonic resection. Br J Surg. 1997;84:1291–1294. doi: 10.1046/j.1365-2168.1997.02771.x. [DOI] [PubMed] [Google Scholar]
- 16.Huh JW, Kim HR, Kim YJ. Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg. 2010;199:435–441. doi: 10.1016/j.amjsurg.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 17.Bakker IS, Morks AN, Hoedemaker HO, Burgerhof JG, Leuvenink HG, Ploeg RJ, Havenga K. The C-seal trial: colorectal anastomosis protected by a biodegradable drain fixed to the anastomosis by a circular stapler, a multi-center randomized controlled trial. BMC Surg. 2012;12:23. doi: 10.1186/1471-2482-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA. Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg. 2007;245:254–258. doi: 10.1097/01.sla.0000225083.27182.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.den Dulk M, Noter SL, Hendriks ER, Brouwers MA, van der Vlies CH, Oostenbroek RJ, Menon AG, Steup WH, van de Velde CJ. Improved diagnosis and treatment of anastomotic leakage after colorectal surgery. Eur J Surg Oncol. 2009;35:420–426. doi: 10.1016/j.ejso.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Doeksen A, Tanis PJ, Vrouenraets BC, Lanschot van JJ, Tets van WF. Factors determining delay in relaparotomy for anastomotic leakage after colorectal resection. World J Gastroenterol. 2007;13:3721–3725. doi: 10.3748/wjg.v13.i27.3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warschkow R, Beutner U, Steffen T, Müller SA, Schmied BM, Güller U, Tarantino I. Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg. 2012;256:245–250. doi: 10.1097/SLA.0b013e31825b60f0. [DOI] [PubMed] [Google Scholar]
- 22.Ellebaek Pedersen M, Qvist N, Bisgaard C, Kelly U, Bernhard A, Møller Pedersen S. Peritoneal microdialysis. Early diagnosis of anastomotic leakage after low anterior resection for rectosigmoid cancer. Scand J Surg. 2009;98:148–154. doi: 10.1177/145749690909800304. [DOI] [PubMed] [Google Scholar]
- 23.Matthiessen P, Strand I, Jansson K, Törnquist C, Andersson M, Rutegård J, Norgren L. Is early detection of anastomotic leakage possible by intraperitoneal microdialysis and intraperitoneal cytokines after anterior resection of the rectum for cancer? Dis Colon Rectum. 2007;50:1918–1927. doi: 10.1007/s10350-007-9023-4. [DOI] [PubMed] [Google Scholar]
- 24.Phitayakorn R, Delaney CP, Reynolds HL, Champagne BJ, Heriot AG, Neary P, Senagore AJ. Standardized algorithms for management of anastomotic leaks and related abdominal and pelvic abscesses after colorectal surgery. World J Surg. 2008;32:1147–1156. doi: 10.1007/s00268-008-9468-1. [DOI] [PubMed] [Google Scholar]
- 25.Daams F, Slieker JC, Tedja A, Karsten TM, Lange JF. Treatment of Colorectal Anastomotic Leakage: Results of a Questionnaire amongst Members of the Dutch Society of Gastrointestinal Surgery. Dig Surg. 2013;29:516–521. doi: 10.1159/000346348. [DOI] [PubMed] [Google Scholar]


