Abstract
Inflammatory bowel disease (IBD) is regarded as one of the risk factors for colorectal cancer, and early detection of cancer in these patients may be difficult, especially in pediatric patients. Prognosis of pediatric colorectal cancer is known to be poor, because of delayed diagnosis and unfavorable differentiation. We report a case of a pediatric patient with a 10-year history of ulcerative colitis who was diagnosed with sigmoid colon cancer when he was 15 years old. He underwent proctocolectomy with ileal pouch anal anastomosis. Postoperative pathological examination of the tumor revealed adenocarcinoma. The pericolic tissue layer was infiltrated, but metastases were not found in either of the two lymph nodes. Children with a long history of predisposing factors such as IBD need particular attention to the possibility of colorectal cancer. Early diagnosis through regular screening with colonoscopy is one of the most important critical factors for a good prognosis.
Keywords: Colon, Rectum, Cancer, Ulcerative colitis, Pediatric
Core tip: Inflammatory bowel disease (IBD) is regarded as one of the important risk factors of colorectal cancer. Several cases of colorectal cancer with pediatric IBD have been reported. However, this case is noticeable in that the onset of disease in the patient was at a relatively young age and the duration of illness was rather short, even though the patient was given continuous medication and regular follow-ups. Therefore, this case highlights the importance the early diagnosis of the disease with a high level of awareness in children with a history of predisposing factors.
INTRODUCTION
Pediatric colorectal cancer has a poor prognosis compared with adult colorectal cancer because of delayed diagnoses at an advanced stage. Thus, early diagnosis based on a high degree of suspicion could be the most important factor in a more favorable prognosis, especially in patients with predisposing factors. Here, we report a 15-year-old boy with a 10-year history of ulcerative colitis (UC) who developed sigmoid colon cancer.
Pediatric colorectal cancer is very rare. The reported incidence is 0.3 to 2 cases per million, accounting for 0.4% of all fatal malignancies in patients younger than 15 years of age[1-6]. According to some studies, most cases occur in the second decade of life[1,7,8]. The sex distribution is equal in adults, whereas in children, a notable preponderance of boys has been reported[2,7].
Although colorectal cancer has a relatively good prognosis in adults, the overall reported survival of pediatric colorectal cancer is poorer than in adults[5,9,10]. The most likely reason is delayed diagnoses with advanced stages of colorectal cancer and high potential for dissemination[2,8,11]. The other reason for the poor prognosis of pediatric colorectal cancer is a high proportion of mucinous histology, accounting for more than 50% of the cases[2,7,12].
CASE REPORT
A 15-year-old boy was transferred from another hospital because of abnormal computed tomography (CT) findings. He presented with abdominal pain, vomiting and poor oral intake for 1 wk before admission.
He had a very long and complicated past medical history. When he was 3 years old, he was treated for an anal fissure. Additionally, when he was 5 years old, he had bilateral knee joint pain with swelling, and a laboratory test was positive for antinuclear cytoplasmic antibody. Through a colon study and colonoscopic biopsy, he was finally diagnosed with UC. After the diagnosis, he was maintained on the combined medications of mesalazine, azathioprine and prednisolone for 5 years.
When he was 10 years old, he moved to another hospital which was in his home town. He had follow-ups through the hospital for 5 years. Then, he was admitted to that hospital for abdominal pain and vomiting, and his CT scan showed suspected cancer lesions. Therefore, he was referred back to our institute for further evaluation.
Several clinical tests were performed after admission to evaluate the patient. The esophagogastroscopy did not show any abnormal findings. The abdominal CT showed a segmental polypoid mass at the sigmoid colon, which was consistent with cancer (Figure 1A). The finding of diffuse colonic wall thickening with a loss of haustra, called “lead pipe appearance”, which was consistent with UC, was also observed (Figure 1B).
Figure 1.
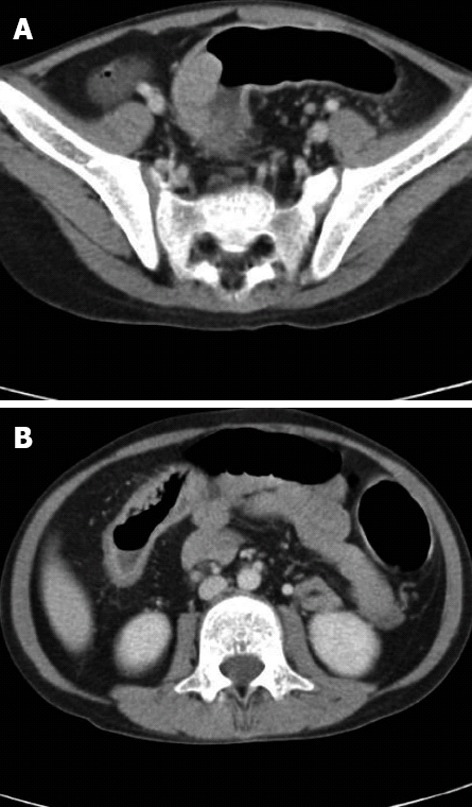
Preoperative computed tomography. A: Enhanced protruding polypoid mass at the sigmoid colon; B: diffuse colonic wall thickening with loss of haustra (“lead pipe appearance”).
The colonoscopy showed diffuse granular lesions in the ascending colon, multiple ulcerations from the transverse colon to rectum, and two polypoid masses without ulcerations in the descending and sigmoid colon (Figure 2).
Figure 2.

Colonoscopy findings. A: Diffuse granular lesions; B: Multiple ulcerations from the transverse colon to the rectum; C: A polypoid mass at the sigmoid colon.
The patient underwent surgery. In a digital rectal examination, we found a 6 cm nodular lesion at the level of the anal verge which was not found in colonoscopy. At the level of the sigmoid colon, a 3 cm-sized mass involving one-third of the lumen was found. Based on these findings, a total proctocolectomy with ileal pouch anal anastomosis was performed.
Grossly, there were two lesions suspicious of malignancy. A 4.0 cm × 2.0 cm × 1.0 cm-sized ulceroinfiltrative mass was located at the ascending colon. The other lesion, a 5.0 cm × 3.0 cm × 1.1 cm-sized polypoid mass, was located at the sigmoid colon (Figure 3). Microscopically, the tumors were adenocarcinomas and were T3 and T1 stage, respectively. Of the 127 lymph nodes, none were positive for metastatic carcinoma. Postoperative pathological examination of the tumor revealed adenocarcinoma. The pericolic tissue layer was infiltrated, but metastases were not found in either of the two lymph nodes.
Figure 3.
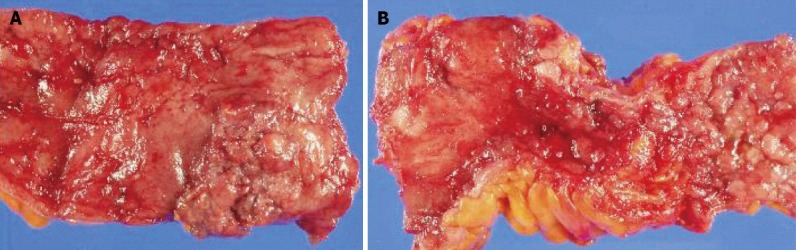
Gross appearance of the colon. A: There was a 5 cm × 3 cm-sized polypoid mass at the sigmoid colon; B: There was severe nodularity with fibrosis in the whole colon.
DISCUSSION
Many studies have reported risk factors for colorectal cancer. Known genetic factors that can increase the risk of colorectal cancer are familial polyposis of the colon, Gardner’s syndrome, Turcot’s syndrome, Peutz-Jegher’s syndrome, UC, familial occurrence of colorectal cancer, and Bloom’s syndrome[9,13,14]. According to most studies, 10% of pediatric colorectal cancers have predisposing factors[9,13].
The rate of adenocarcinoma in childhood-onset UC patients is higher than that in adult-onset UC patients[15,16]. Eaden et al[16] investigated the long-term incidence of colorectal cancer among patients with childhood-onset UC through a meta-analysis. They reported that the cumulative probabilities of developing colorectal cancer were 5.5% at 10 years after onset of UC, 10.8% at 20 years and 15.7% at 3 years.
Diagnosis of inflammatory bowel disease at a young age is a well-known factor for an increased risk of colorectal cancer[15]. Ekbom et al[17] reported that the average incidence of colorectal cancer among patients with UC between the ages of 0 and 14 was 118.3 times that of the control population.
Considering the relatively high incidence of colorectal cancer and the poor prognosis in patients with childhood-onset UC, early diagnosis through regular screening with colonoscopy can increase the resectability and improve the prognosis.
In summary, pediatric surgeons always have to keep in mind the possibility of colorectal cancer in children with a long history of predisposing factors such as UC. Early diagnosis through regular screening with colonoscopy is one of the most important critical factors for a good prognosis.
Footnotes
P- Reviewers Yang SF, Fang BL S- Editor Huang XZ L- Editor Cant MR E- Editor Li JY
References
- 1.Jain AK, Motil KJ, Olutoye OO, Cope-Yokoyama S, Egler RA, Tatevian N. Colon cancer in a 16-year-old girl: signet-ring cell carcinoma without microsatellite instability--an unusual suspect. J Pediatr Gastroenterol Nutr. 2009;48:110–114. doi: 10.1097/MPG.0b013e31815dda8c. [DOI] [PubMed] [Google Scholar]
- 2.Kravarusic D, Feigin E, Dlugy E, Steinberg R, Baazov A, Erez I, Lazar L, Kapuller V, Grunspan M, Ash S, et al. Colorectal carcinoma in childhood: a retrospective multicenter study. J Pediatr Gastroenterol Nutr. 2007;44:209–211. doi: 10.1097/01.mpg.0000252195.84084.52. [DOI] [PubMed] [Google Scholar]
- 3.Angelini C, Crippa S, Uggeri F, Bonardi C, Sartori P, Uggeri F. Colorectal cancer with neuroendocrine differentiation in a child. Pediatr Surg Int. 2005;21:839–840. doi: 10.1007/s00383-005-1525-3. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto K, Tanaka T, Kuno K, Amoh Y, Takahashi Y, Murakami H. Carcinoma of the colon in children: case report and review of the Japanese literature. J Gastroenterol. 1994;29:647–652. doi: 10.1007/BF02365450. [DOI] [PubMed] [Google Scholar]
- 5.Durno C, Aronson M, Bapat B, Cohen Z, Gallinger S. Family history and molecular features of children, adolescents, and young adults with colorectal carcinoma. Gut. 2005;54:1146–1150. doi: 10.1136/gut.2005.066092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chantada GL, Perelli VB, Lombardi MG, Amaral D, Cascallar D, Scopinaro M, Deza EG, Gercovich FG. Colorectal carcinoma in children, adolescents, and young adults. J Pediatr Hematol Oncol. 2005;27:39–41. doi: 10.1097/01.mph.0000149251.68562.8e. [DOI] [PubMed] [Google Scholar]
- 7.Rao BN, Pratt CB, Fleming ID, Dilawari RA, Green AA, Austin BA. Colon carcinoma in children and adolescents. A review of 30 cases. Cancer. 1985;55:1322–1326. doi: 10.1002/1097-0142(19850315)55:6<1322::aid-cncr2820550627>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 8.Steinberg JB, Tuggle DW, Postier RG. Adenocarcinoma of the colon in adolescents. Am J Surg. 1988;156:460–462. doi: 10.1016/s0002-9610(88)80528-2. [DOI] [PubMed] [Google Scholar]
- 9.Salas-Valverde S, Lizano A, Gamboa Y, Vega S, Barrantes M, Santamaría S, Zamora JB. Colon carcinoma in children and adolescents: prognostic factors and outcome-a review of 11 cases. Pediatr Surg Int. 2009;25:1073–1076. doi: 10.1007/s00383-009-2491-y. [DOI] [PubMed] [Google Scholar]
- 10.Brown RA, Rode H, Millar AJ, Sinclair-Smith C, Cywes S. Colorectal carcinoma in children. J Pediatr Surg. 1992;27:919–921. doi: 10.1016/0022-3468(92)90399-r. [DOI] [PubMed] [Google Scholar]
- 11.Vastyan AM, Walker J, Pintér AB, Gerrard M, Kajtar P. Colorectal carcinoma in children and adolescents--a report of seven cases. Eur J Pediatr Surg. 2001;11:338–341. doi: 10.1055/s-2001-18548. [DOI] [PubMed] [Google Scholar]
- 12.Goldthorn JF, Powars D, Hays DM. Adenocarcinoma of the colon and rectum in the adolescent. Surgery. 1983;93:409–414. [PubMed] [Google Scholar]
- 13.Karnak I, Ciftci AO, Senocak ME, Büyükpamukçu N. Colorectal carcinoma in children. J Pediatr Surg. 1999;34:1499–1504. doi: 10.1016/s0022-3468(99)90112-4. [DOI] [PubMed] [Google Scholar]
- 14.Heiss KF, Schaffner D, Ricketts RR, Winn K. Malignant risk in juvenile polyposis coli: increasing documentation in the pediatric age group. J Pediatr Surg. 1993;28:1188–1193. doi: 10.1016/0022-3468(93)90162-e. [DOI] [PubMed] [Google Scholar]
- 15.Kayton ML. Cancer and pediatric inflammatory bowel disease. Semin Pediatr Surg. 2007;16:205–213. doi: 10.1053/j.sempedsurg.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–535. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ekbom A, Helmick C, Zack M, Adami HO. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med. 1990;323:1228–1233. doi: 10.1056/NEJM199011013231802. [DOI] [PubMed] [Google Scholar]


