Abstract
Background:
Acquired immune deficiency syndrome (AIDS) is now considered as a manageable chronic illness. There has been a dramatic reduction in human immunodeficiency virus (HIV) related morbidity and mortality due to antiretroviral therapy. A high level of adherence (>95%) is required for antiretroviral therapy to be effective. There are many barriers to adherence in both developed and developing countries.
Aim:
The aim of our study was to determine adherence levels and factors influencing adherence to antiretroviral therapy among people living with HIV.
Materials and Methods:
Using a cross-sectional study design, 116 HIV positive patients receiving antiretroviral therapy for at least 1 year were interviewed using a semi structured questionnaire. The collected data was analyzed using Statistical Product and Service Solutions (SPSS) version 11.5. Chi-square test was done. A P value of < 0.05 was considered statistically significant.
Results:
Of 116 participants, 63.7% reported adherence ≥ 95%. Mean adherence index was 91.25%. Financial constraints, forgetting to take medication, lack of family care, depression, alcohol use, social stigma and side effects to antiretroviral therapy were barriers for adherence in our study.
Conclusion:
Adherence to antiretroviral therapy in south India is suboptimal. Intensive adherence counseling should be provided to all patients before initiation ofantiretroviral therapy. Health care providers must identify possible barriers to adherence at the earliest and provide appropriate solutions.
Keywords: Adherence, Adherence index, Antiretroviral therapy, Depression, Human immunodeficiency virus, Stigma
Introduction
Anti-Retroviral Therapy (ART) has improved the quality of life of Human immunodeficiency virus (HIV) patients worldwide. A reduction in HIV-related morbidity and mortality has been recognized in countries where ART has been made widely available. Acquired immune deficiency syndrome (AIDS) is now a manageable chronic illness. To achieve optimal results from ART, high levels of patient adherence to ART is essential. High levels of adherence to ART (at least 95%) is needed to ensure optimal benefits.[1]
Adherence is defined as a patient's ability to follow a treatment plan, take medications at prescribed times and frequencies, and follow restrictions regarding food and other medications.[2] Adherence is a problem in any chronic disease and an average non-adherence rate of 24.8% have been reported.[3] Suboptimal adherence to ART may ultimately lead to failure of primary regimen. The national guidelines in India stipulates >95% adherence to ART.
There are many barriers to adherence in both developed and developing countries. It is important to identify factors that lead to non-adherence and develop strategies to improve long-term adherence. This study was designed to identify the levels of adherence and the factors influencing adherence to ART at a tertiary care institution in southern India.
Materials and Methods
Ethical clearance was obtained from the Institutional Ethics committee of Kasturba Medical College, Mangalore.
Study population, design and setting
A facility based cross-sectional study was carried out among 116 People Living with HIV (PLHIV) on ART.The sample size was calculated based on expected proportion of adherence to ART among PLHIV based on previous studies,[4] with a relative precision of 10% and a confidence interval (CI) of 95%.The study subjects were adult patients (aged 18 years or above) on First line Anti-Retroviral treatment (Two Nucleoside Reverse Transcriptase Inhibitor and one Non-Nucleoside Reverse Transcriptase Inhibitor) for more than 1 year and who gave written informed consent. During our study period of 2 months, 288 HIV positive patients on ART visited the HIV clinic of our hospital. Out of 288 patients, 134 patients were on ART for more than 1 year. Out of 134 patients, 116 consecutive patients who gave consent participated in the study. The study was carried out at Kasturba Medical College hospital (tertiary health care centre) in Mangalore (South India). Patients who agreed to participate were interviewed by the investigators for 25 to 30 minutes. The interview was guided by a pretested semistructured questionnaire that covered sociodemographic characteristics of the study population, duration of use of ART, distance traveled to procure ART, and whether they got government sponsored free ART.
Measurement of adherence
Adherence was assessed retrospectively based on a 4-day recall as used in Adult AIDS Clinical Trials Group (AACTG) follow up questionnaire.[5] Adherence index was calculated by the formula:
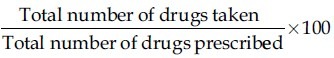
Patients with more than 95% of adherence were considered as having high adherence and those with less than 95% were considered as having low adherence.
Patients who reported missed doses were asked to provide reasons for missing their medications. Investigators asked leading questions to assess stigma and family support and then it was categorized as present or absent. The 20-item AACTG signs and symptoms questionnaire was used to assess side effects. Alcohol consumption during last 1 month was assessed. The Beck Depression Inventory was used to assess depression.[6]
Statistical analysis
The collected data was analyzed using SPSS version 11.5. Chi-square test was done. A P value of < 0.05 was considered statistically significant.
Results
Of the 116 subjects, 80 (69%) were males and 36 (31%) were females. Majority (51.72%) of study population was in the age group of 21-40 years. Eighty six percent of the study population was literate. 72.41% of the patients in our study received free ART provided by the government, and 27.58% of the patients paid from their pocket [Table 1].
Table 1.
Baseline characteristics of study population (N=116)
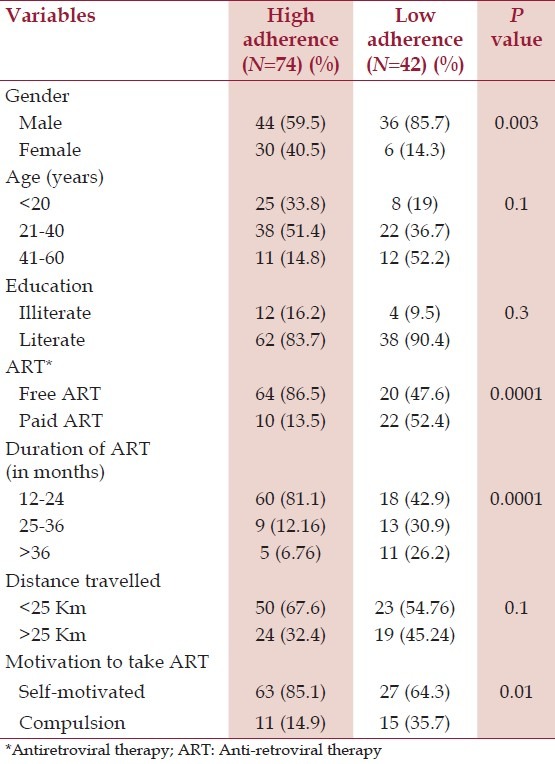
Among 116 participants, 74 (63.7%) reported adherence > 95%. Mean adherence index was 91.25%. Hundred percent adherence was reported by 54.3% of patients. Among patients who received free ART, 64 (76.2%) of them had high adherence, whereas, only 10 (31.3%) patients who paid for ART had high adherence. Among patients who were self-motivated to take ART, 63 (70%) of them had high adherence.
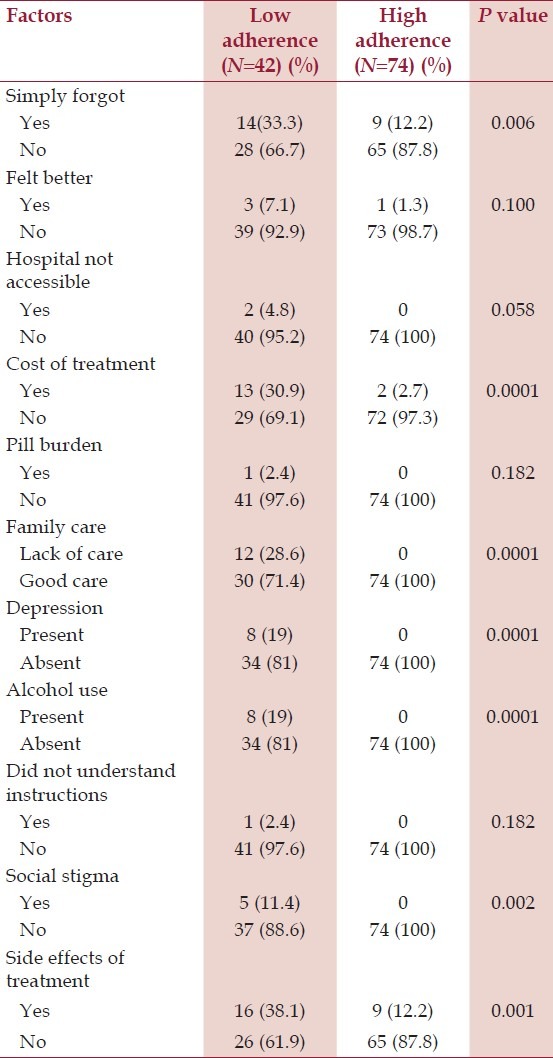
Among patients with low adherence, 14 (33%) simply forgot to take tablets and 13 (30%) patients reported that cost of treatment was responsible for low adherence. All patients who lacked family care, patients who had depression and patients who consumed alcohol had low adherence which was statistically significant. Social stigma and side effects to treatment also contributed to low adherence which was statistically significant [Table 2].
Table 2.
Factors influencing adherence
Discussion
Of the 116 participants in our study, 42 (36%) patients reported adherence of <95%. Financial constraints, forgetting to take medication, lack of family care, depression, alcohol use, social stigma, and side effects to ART were associated with low adherence in our study.
Adherence is a major issue in management of chronic diseases. In a meta-analysis of 569 studies, 24.8% of subjects were non-adherent.[3] In HIV, studies indicate that high levels of adherence are necessary for viral suppression, prevention of resistance, and disease progression.[7] A meta-analysis of studies on ART adherence found that 77% of patients in Africa achieved adequate adherence of 95% compared to just 55% of patients in North America.[8] Studies from India have reported adherence rates of 76-93%.[4,9,10]
Studies from India have shown that financial problems, lack of family care, substance abuse, depression, social stigma, and side effects are barriers to adherence to ART. Majority of patients (78%) report more than one barrier to ART adherence.[11]
Batavia et al.,[12] have concluded that providing free ART improves adherence. Wanchu et al.,[13] have shown that the major reasons for non-adherence was financial constraints, forgetting to take the medication, drug toxicity, lack of access to drug, fear of getting immune to the benefit of the drug, and to avoid side effects. Not having money to travel to ART centre and forgetting to take the medication were the major reasons for non-adherence in the African setting.[14]
A meta-analysis reported that adherence is 1.74 times higher in patients from cohesive families.[15] Depression has been shown to be an independent predictor for poor adherence.[10] Depression was found to be strongly associated with lower adherence in our study. Depression is common among HIV infected persons.[16] Early identification and management of depression is essential to improve adherence. A meta-analysis has shown that individuals who consumed alcohol had reduced adherence to ART.[17]
There is concern that patients on ART would become less adherent once they feel better. Our study did not find any such evidence. Educated people show better adherence.[18] Education may impact adherence in several ways including facilitating communication with health care providers.[19] In our study, majority of patients who had low adherence were literate.
Self-reporting is the most commonly used measure of adherence in resource limited settings because it is easy to include in routine clinical practice. There are some objective measures of adherence. Medication event monitoring system (MEMS),[20] pharmacy refill data,[21] and directly observed therapy (DOT) are other methods to monitor adherence.
Our study had some limitations. Adherence was assessed through a self-reporting adherence questionnaire and other objective tools such as electronic pill caps, viral load and CD4 count were not used. Stigma was assessed in our study using a single interview question. We did not use a validated questionnaire to assess stigma. Our study group was predominantly urban so our results do not necessarily reflect practices in other settings. Finally, the cross sectional study design has its own limitations.
Conclusion
Adherence to ART in Southern India is sub-optimal. Alcohol use, drug side effects, depression, stigma and lack of family support are factors associated with reduced adherence. Priorities should be given to improving adherence otherwise our ART programme will fail. Busy medical practitioners must find sufficient time for counseling, which is very essential for the success of ART program in our country.
Acknowledgment
Indian Council of Medical Research
Footnotes
Source of Support: Indian Council of Medical Research.
Conflict of Interest: None declared.
References
- 1.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 2.Sahay S, Reddy KS, Dhayarkar S. Optimizing adherence to antiretroviral therapy. Indian J Med Res. 2011;134:835–49. doi: 10.4103/0971-5916.92629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42:200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 4.Lal V, Kant S, Dewan R, Rai SK, Biswas A. A two-site hospital-based study on factors associated with nonadherence to highly active antiretroviral therapy. Indian J Public Health. 2010;54:179–83. doi: 10.4103/0019-557X.77256. [DOI] [PubMed] [Google Scholar]
- 5.Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. Patient Care Committee and Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 6.Beck AT, Steer RA, Garbin GM. Psychometric properties of the Beck depression inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 7.Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–3. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. JAMA. 2006;296:679–90. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 9.Safren SA, Kumarasamy N, James R, Raminani S, Solomon S, Mayer KH. ART adherence, demographic variables and CD4 outcome among HIV-positive patients on antiretroviral therapy in Chennai, India. AIDS Care. 2005;17:853–62. doi: 10.1080/09540120500038439. [DOI] [PubMed] [Google Scholar]
- 10.Sarna A, Pujari S, Sengar AK, Garg R, Gupta I, Dam JV. Adherence to antiretroviral therapy and its determinants amongst HIV patients in India. Indian J Med Res. 2008;127:28–36. [PubMed] [Google Scholar]
- 11.Joglekar N, Paranjape R, Jain R, Rahane G, Potdar R, Reddy KS, et al. Barriers to ART adherence and follow ups among patients attending ART centres in Maharashtra, India. Indian J Med Res. 2011;134:954–9. doi: 10.4103/0971-5916.92642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Batavia AS, Balaji K, Houle E, Parisaboina S, Ganesh AK, Mayer KH, et al. Adherence to antiretroviral therapy in patients participating in a graduated cost recovery program at an HIV care center in South India. AIDS Behav. 2010;14:794–8. doi: 10.1007/s10461-009-9663-6. [DOI] [PubMed] [Google Scholar]
- 13.Wanchu A, Kaur R, Bambery P, Singh S. Adherence to generic reverse transcriptase inhibitor-based antiretroviral medication at a Tertiary Center in North India. AIDS Behav. 2007;11:99–102. doi: 10.1007/s10461-006-9101-y. [DOI] [PubMed] [Google Scholar]
- 14.Kebede A, Wabe NT. Medication adherence and its determinants among patients on concomitant tuberculosis and antiretroviral therapy in south west Ethiopia. N Am J Med Sci. 2012;4:67–71. doi: 10.4103/1947-2714.93376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychol. 2004;23:207–18. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 16.Chandra PS, Desai G, Ranjan S. HIV and psychiatric disorders. Indian J Med Res. 2005;121:451–67. [PubMed] [Google Scholar]
- 17.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: Review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52:180–202. doi: 10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kleeberger CA, Phair JP, Strathdee SA, Detels R, Kingsley L, Jacobson LP. Determinants of heterogeneous adherence to HIV-antiretroviral therapies in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2001;26:82–92. doi: 10.1097/00126334-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 19.Wasti SP, Simkhada P, Randall J, Freeman JV, van Teijlingen E. Factors influencing adherence to antiretroviral treatment in Nepal: A mixed-methods study. PLoS One. 2012;7:e35547. doi: 10.1371/journal.pone.0035547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin S, Elliott-DeSorbo DK, Calabrese S, Wolters PL, Roby G, Brennan T, et al. A comparison of adherence assessment methods utilized in the United States: Perspectives of researchers, HIV-infected children, and their caregivers. AIDS Patient Care STDs. 2009;23:593–601. doi: 10.1089/apc.2009.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bisson GP, Gross R, Bellamy S, Chittams J, Hislop M, Regensberg L, et al. Pharmacy refill adherence compared with CD4 count changes for monitoring HIV-infected adults on antiretroviral therapy. PLoS Med. 2008;5:e109. doi: 10.1371/journal.pmed.0050109. [DOI] [PMC free article] [PubMed] [Google Scholar]


