Abstract
Background:
Carotid artery intima media thickness reflects the ongoing process of atherosclerosis in the body. The pathologic process occurring in the obese patients in the vascular system is atherosclerosis which is an important cause of ischemic stroke. Body mass index is an indirect measure of obesity in general population.
Aim:
The study was to assess the role of carotid artery intima media thickness as a marker of atherosclerosis and its relation with body mass index in ischemic stroke patients.
Materials and Methods:
Body mass index of the all stroke patients was calculated by using formula body mass in kilograms divided by the square of height in meters. The patients were classified in four groups of body mass index according to Indian standards. Carotid sonography was done to assess the common carotid artery intima media thickness in millimeters by using high resolution 7.5 MHz sonography technique.
Results:
The average Carotid intima media thickness in this study was 9.23mm. There was a significant association found between increasing carotid artery intima media thickness and groups of body mass index (P- <0.05) in ischemic stroke patients.
Conclusions:
Body mass index as an indicator of obesity and carotid intima media thickness both are very important risk factors for ischemic stroke and are associated with each other.
Keywords: Body mass index, Carotid intima media thickness, Cerebrovascular diseases, Diabetes mellitus, Lipoproteins, Obesity, Sonography
Introduction
Stroke is defined as an “abrupt onset of neurologic deficit that is attributable to a focal vascular cause”. Approximately 80% cases of stroke are due to cerebral ischemia. Ischemic stroke may be thrombotic or embolic. Atherosclerosis is a systemic disease that is responsible for most cardiovascular events and stroke. Atherosclerosis of the arteries supplying the central nervous system frequently provokes strokes and transient cerebral ischemia.
Carotid intima-media thickness (CIMT) is a non-invasive alternative marker and intermediate phenotype of atherosclerotic disease that has been used extensively since 1986 beginning with the initial description by Pignoli, et al.[1] B-mode sonography is a noninvasive method for examining the walls of peripheral arteries and provides a measure of intima-media thickness and the presence of stenosis and plaques. The intima-media thickness corresponds to the intima-media complex, which comprises endothelial cells, connective tissue and smooth muscle and is the site of lipid deposition and plaque formation. The intima-media thickness of the carotid artery is an established sonographic marker for early atherosclerosis, and thickening of the intima-media complex reflects generalized atherosclerosis.[2]
Several studies have shown an association between increased carotid intima-media thickness and stroke in elderly and middle-aged subjects.[3] A positive association exists between carotid intima-media thickness and the risk of subsequent cardiovascular events including stroke, in general populations, independent of all major risk factors.[4] This relation has promoted the use of carotid intima-media thickness in pathophysiological studies and clinical trials, in which the perception of carotid intima-media thickness has shifted from a secondary end point to a surrogate risk factor of cerebrovascular event. Increased common carotid artery intima-media thickness has been reported under various conditions, including hypertension, dyslipidemia, obesity, diabetes, smoking, and cardiovascular disease, including ischemic stroke.[5] Also increased CIMT was found in patients of chronic renal failure on hemodialysis suggesting hemodialysis as an independent risk factor for atherosclerosis.[6]
Body Mass Index (BMI) is a measure of the body weight relative to height that is associated with body fat and health risk. It was developed in the mid 1800's by a Belgian mathematician named Adolphe Quetelet. It is equal to the weight, divided by the square of the height. Obesity is being recognized as potential threat to health and must be treated at the right time. With obesity increasing, the risk for developing several diseases like hypertension, diabetes, heart ailments, stroke, osteoarthritis, etc., also increases. Increased body mass index is tightly related to an increased risk of coronary heart disease,[7] but its association with stroke is less well recognized because of conflicting results reported in the literature. Some cohort studies have found a positive association between BMI and the risk of stroke,[7–13] whereas others have shown no apparent association[14–17] or have even reported an inverse or a U-shaped association[18–21] Recently it has been found that BMI indirectly is a spectrum of process of atherosclerosis and its relation with other markers of atherosclerosis is to be evaluated.
In the present article, we investigated the association between BMI and the CIMT in ischemic stroke patients in study conducted on north Indian population, taking other known risk factors into account.
Materials and Methods
Informed consent is taken from all the patients or their relatives before inclusion in this observational study. Ethical information from local review board was not needed as no clinical trial was done and neither any drug nor its effect was evaluated during this study.
Study population
The study was conducted in patients admitted to the Medicine Department of our Medical University over a period of 1 year from August 2011 to August 2012. The study comprised of 92 consecutive (more than 30 years of age) patients of ischemic stroke admitted in our wards. Informed consent is taken from all the patients or their relatives before inclusion in this observational study.
Identification of ischemic stroke patient is difficult as it is confused with few other congener cerebrovascular diseases. So both imaging modalities and clinical assessment is used to select patients for this study. This included full detailed clinical current and past history as well as inclusion of imaging modalities also to rule out other diseases. Following patients have been excluded from the study: isolated transient ischemic attack, stroke as a result of apparent cardio-embolic origin, history of previous stroke, and subarachnoid or intracerebral hemorrhage.
Clinical evaluation
Height was measured on a clinic stadiometer. The body weight was assessed using a calibrated scale, with participants using light clothes and no shoes. The body mass index (BMI) was calculated as body weight (kilograms-kg) divided by square height (metersquare-m2).
The Indian Health Ministry reduced the diagnostic cut-offs for BMI to 23 kg/m2 and the standard waist circumference to fight the battle against obesity. The standards have been set for the first time in the Ministry's consensus guidelines for the Prevention and Management of Obesity and Metabolic Syndrome for the country as released on October 2008. The guidelines were released jointly by the Health Ministry, the Diabetes Foundation of India (DFI), the All-India Institute of Medical Science (AIIMS), Indian Council of Medical Research (ICMR), the National Institute of Nutrition (NIN) and 20 other health organizations.
India's new diagnostic cut-off for the body mass index is 23 kg/m2 as opposed to 25 kg/m2 globally. A person with a body mass index of 23 kg/m2 will now be considered overweight and below 23 kg/m2 as one with normal BMI, unlike the cut-off limit of 25 kg/m2 earlier. Now, those with BMI of 25 kg/m2 will be clinically termed obese (as opposed to 30 kg/m2 at the international level), and those with BMI of 32.5 kg/m2 will require bariatric surgery to eliminate excess flab.
The BMI limit for Indians now is less than 18.49–underweight, 18.5 0-22.99–normal, 23.00-24.99–overweight, and more than 25.00–obese. According to the guidelines, the cut-offs for waist circumstances will now be 90 cm for Indian men (as opposed to 102 cm globally) and 80 cm for Indian women (as opposed to 88 cm at the international level).
Researches over the last several years have shown that Indian bodies and genetics are different from their western counterparts as Indians suffer from abdominal obesity compared to people in the West whose bodies are uniformly obese. This body composition puts Indian in the high risk zone for diabetes and hypertension. Standardized questionnaires were used to obtain information about physical activity, smoking history, medication use, family history of cardiovascular disease, and duration of hypertension. Systolic and diastolic blood pressures were measured three times after a 5-minute rest, in a seated position, using an electronic device.
Biochemical assay
Patients were considered as Diabetic if Fasting serum glucose was >126mg/dl and Random serum glucose was >200mg/dl, whether they were a known case of diabetes mellitus or diagnosed during hospital admission. Blood glucose was determined by the glucose oxidase method using Eco-pak glucose reagent.
Venous blood samples were taken after the subject had fasted for 12 h. The serum lipids (total cholesterol, High density lipoprotein (HDL)-cholesterol, and triglycerides) were analyzed by colorimetry (Bioclin). The Low density lipoprotein (LDL)-cholesterol was calculated using the Friedewald formula when triglyceride value was less than 400mg/dL. Hemoglobin A1c (HbA1c) was measured by ion exchange resin method using Erba kit.
Fibrinogen is a high molecular weight glycoprotein, which plays a major role in haemostsis and an important determinant of vascular atherogenicity. Levels of fibrinogen from 2.33-4.96 g/L are taken as normal. Levels higher then this indicate an increased atherogenicity of the blood. Other biochemical parameters are measured by kits available in our pathology.
Carotid ultrasound
The patient was supine with slight hyperextension and rotation of the neck in the direction opposite the probe. A linear array transducer with a multiple frequency (7 to 12MHz) attached to a high-resolution B mode ultrasound system was used to acquire images by a single-sonographer blind to clinical data of subjects Manual measurement of IMT was performed in the common carotid artery, at both sides, in a region free of plaque located approximately 20mm from bulb. At least three values were obtained in different sites of this segment and the mean value of six measurements (three from each side) was used for analysis. The protocol we followed was according to Mannheim Carotid Intima-Media Thickness Consensus (2004–2006).[22] [Figure 1]
Figure 1.
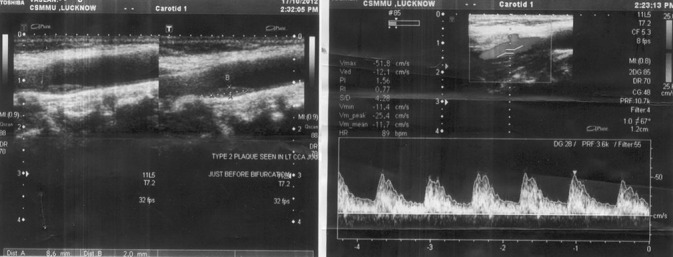
Carotid sonographic imaging showing increased carotid intima media thickness with Plaque
Statistical analysis
The results are presented in mean ± SD (standard deviation) and percentage. Chi-square test was used to compare the dichotomous/categorical variables. The analysis of variance (ANOVA) was used to compare more than two means. The unpaired t-test used to compare two means. The paired t-test was used to compare continuous variables from 0 day to follow-ups. The P < 0.05 was considered as significant. All the analysis was carried out by using SPSS (Statistical Product and Service Solutions) 15.0 versions.
Results
Characteristics of the study subjects
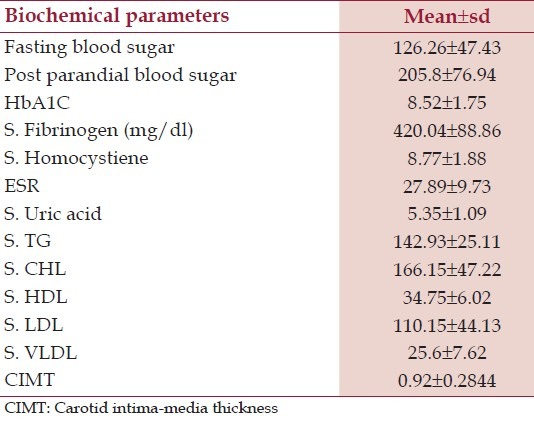
The study was conducted over one hundred four cases out of which twelve were withdrawn due to various reasons (including death and leaving against medical advice); hence only ninety-two were finally included in the study. About one third of the patients were >70 years (33.7%) and between age group 61-70 years (32.6%). 25% of the patients were between 50-60 years and 8.7% were <50 years. More than half (60.9%) of the patients were males. In our study hemiparesis was seen in 88% of the patients and cranial nerve involvement in 18.5%. Aphasia was present in 26.1% patients. Of all the patients of ischemic stroke in our study, previous history of hypertension was present in 22.8% and diabetes in 32.6%. More than one third (38%) were tobacco chewers, 21.7% were smokers and about 20.7% were alcoholic. The fasting and post-prandial blood sugar values as well as HbA1C, on an average, were higher than normal population standards. The average values of the risk factor indicator parameters in our study were greater in stroke patients as compared to the normal population, the following risk factor indicators like serum fibrinogen, homocystiene, ESR (erythrocyte sedimentation rate), triglycerides, total cholesterol, LDL and VLDL (Very low density lipoprotein) cholesterol are found to be raised [Table 1].
Table 1.
Distribution of patients by biochemical parameters
Impact of BMI and other risk factors on stroke
On average, participants were overweight, and their blood pressure, glucose, cholesterol levels and other biochemical risk parameters were greater than target ranges for primary disease prevention, and most patients were of intermediate to high risk. Anthropometric index of obesity i.e. BMI, as well as other major traditional risk factors exhibited significant high levels in our study group of ischemic stroke patients. The mean BMI was 30.25 ± 2.74kg/m2 and 72.9% had BMI level >25 which indicates that most of the stroke patients in our study were obese [Figure 2].
Figure 2.
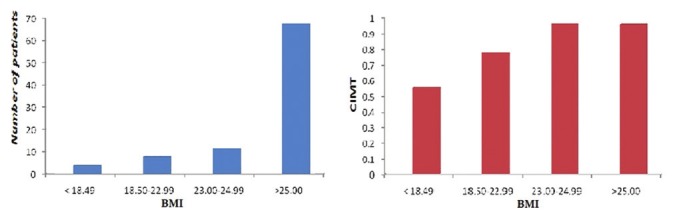
Bar diagrams showing high values of BMI in most of ischemic stroke patients and association of high CIMT values with various groups of BMI
Association of BMI with CIMT in stroke patients
Average mean CIMT of all stroke patients in our study was 0.92±0.2844. The cut-off for normal CIMT was taken as 0.8mm in Indian population as in different studies this cut-off was found to correlate with vascular risks. Prevalence of increased CIMT (>0.8mm) in patients enrolled in our study was 73. The CIMT was significantly associated with On analyzing anthropometric parameter like BMI and biochemical parameters and mean CIMT a strong association was found between different groups of BMI and CIMT (P < 0.05) [Table 2, Figures 2 and 3].
Table 2.
Association of body mass index values of ischemic stroke patients with mean CIMT
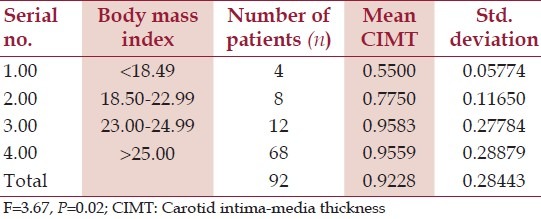
Figure 3.
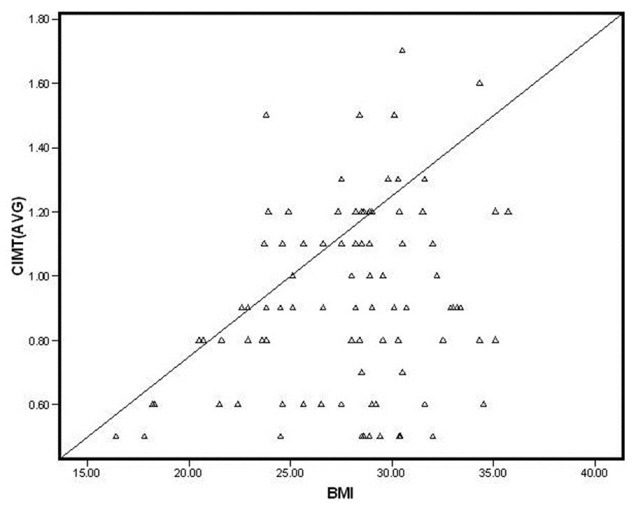
Scatter diagram showing correlation between BMI and CIMT
Association of CIMT with various cerebrovascular risk parameters in stroke patients
There are various cerebrovascular risk parameters in the study, some were significantly associated with marker of atherosclerosis i.e., CIMT but others are not as shown in table [Table 3]. Out of total 72 smokers in this cohort 53 had high CIMT (p -0.9) and out of 19 alcoholic in whole cohort of 92 stroke patients 17 had high CIMT (p -0.08) but both smoking and alcoholism were not significantly associated with high CIMT [Table 3]
Table 3.
Association of CIMT with various cerebrovascular risk parameters in stroke patients
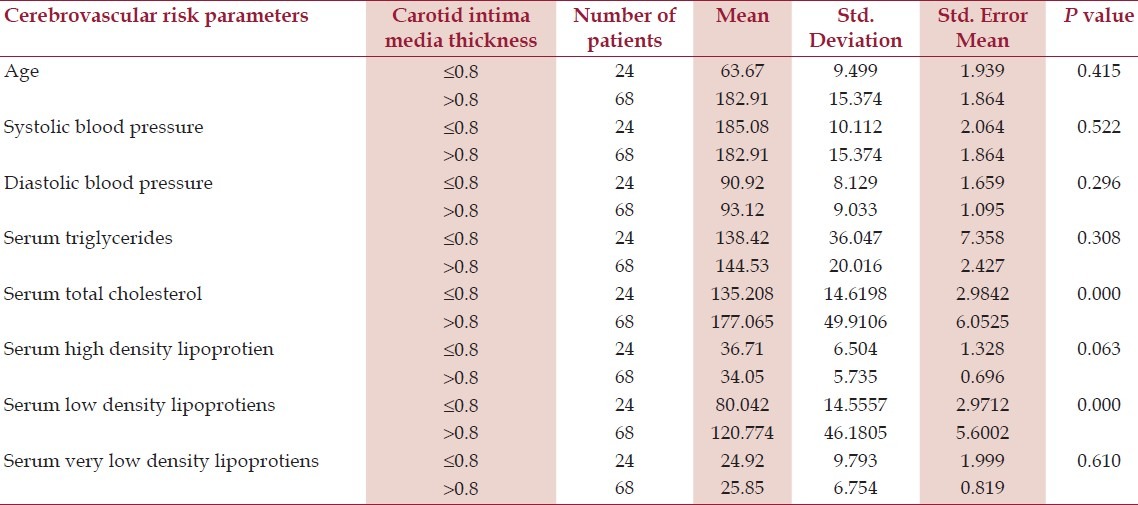
Table 3: Association of CIMT with various cerebrovascular risk parameters in stroke patients
Discussion
In our study on ischemic stroke patients, the demographic characteristics of the study sample were typical as for any hospital based study and the patterns followed had similarity to previous studies in the field.
BMI is an important parameter showing recent trends pertaining to a sedentary lifestyle and its relation with stroke denotes that body composition is important parameter in today's life. In this study, we have shown that carotid intima-media thickness is positively associated with BMI in ischemic stroke patients. In fact, our valuation showed that excess body weight that is prevalent in Indian population having various risks of stroke was associated with carotid intima-media thickening.
The novelty of our study is that our data support the hypothesis that the anthropometric parameters like BMI has their own importance as a risk factor for ischemic stroke which affects the changes occurring in arterial wall as a generalized process of atherosclerosis implicated by increased CIMT. Likewise, we might state that overweight and obesity are related to subclinical stages of premature atherosclerosis. Some studies have reported associations between BMI and stroke subtypes.[23–26] For ischemic stroke, our findings are in accord with previous Western and Japanese studies.[27–30] To our knowledge, this is also the first study conducted in an Indian population showing such relationship.
The clinical implications and contribution of abdominal adiposity to global cardio metabolic risk have been extensively reviewed[31] and[32] few studies have reported the relationship between different bedside anthropometric obesity indices and subclinical vascular disease, an early manifestation of atherosclerosis. Several such studies have evaluated associations between indices of adiposity and Carotid intima-media thickness (CIMT).[23–26]
CIMT is an intermediate phenotype for early atherosclerosis, and because it can be measured relatively simply and noninvasively, it is well suited for use in large-scale population studies. It also allows risk stratification in individuals.[33] In the last decades, it became widely used in adults and the first studies in children and adolescents emerged, mainly in pediatric populations of higher cardiovascular risk.[34,35]
Though few prior longitudinal studies of older subjects have often failed to find a relation between measures of central adiposity and coronary heart disease[36–38] or stroke,[39] particularly after adjustment for general adiposity our study is novel and extends such observations by demonstrating that these indices and particularly BMI are more closely linked to subclinical atherosclerotic vascular disease leading to catastrophic cerebrovascular events. Besides anthropometric indices like BMI cutaneous manifestations of generalized obesity like xanthelasma could also be associated with atherosclerosis and further risks of cerebrovascular diseases.[40] But anthropetric indices provide better and direct measure of obesity and hyperlipidemia.
The increased CIMT accompanied by further cardiovascular risk factors in overweight and obese persons and the correlation of risk factors with BMI strongly suggests that overweight and obesity represent powerful determinants of early manifestations of atherosclerosis which affects structural and mechanical properties of major vessels leading to ischemic stroke. In various trials, it has been shown that atherosclerosis is a multifactorial process which is accelerated by metabolic disorders, high blood pressure and low-grade inflammation. It seems that lipid disorders and elevated levels of blood lipid parameters, blood glucose, glycated proteins, advanced glycation end-products (AGE), elevated concentrations of pro-inflammatory cytokines, acute phase proteins, and enhanced activation of pro-inflammatory signals are key players in the development of vascular disorders.[41–43] Our study also supports this as there was a significant association found between different lipid profile parameters like total cholesterol and serum LDL, with markers of carotid atherosclerosis though few of known risk factors like smoking and alcoholism were not found to be associated. This indicates cumulative effects of various parameters involved in process of generalized atherosclerosis which is reflected physiologically as raised BMI or biochemically as raised levels of biochemical parameters. Additionally, in overweight and obese subjects there is often an accumulation of macrophages in the adipose tissue. The macrophage accumulation in adipose tissue has been positively correlated with adipocyte size and contributes to a further expression of pro-inflammatory mediators, such as TNF (tumor necrosis factor)-α, IL (interleukin)-6 and inducible nitric oxide synthase.[44–50] It appears that the co-existence of various risk factors and an underlying chronic inflammatory process may well explain an increased mortality risk and risk for cerebrovascular events in overweight and obese subjects.
This study has various strengths, including its focus on older adults through age 80 years; its inclusion of both women and men; exclusion of cardio embolic stroke; standardized measurement, and not self-reports, of baseline anthropometry parameters; evaluation of directly measured body composition along with institutionalized measurements of carotid vessel wall thickness.
There are likewise several limitations. First, because prevalent cardiovascular disease and co morbidities can confound the association of BMI with outcome the present findings are generalizable only to healthier older adults free of clinically overt cardiovascular disease. Second, the number of ischemic stroke patients was not adequate to represent whole population. Third, there was no comparison group formulated to assess the association in general population. Fourth, formal assessment of reproducibility of anthropometric measurements was not undertaken.
Conclusion
The identification of risk factors associated with early atherogenesis is important to stratify the individual risk and to predict cardiovascular events. It has been formerly shown in few studies a close relationship between carotid IMT and traditional cardiovascular risk factors such as ageing, hypertension, obesity, dyslipidemia, and diabetes. Our study was an effort to confirm the importance of BMI as a risk factor for ischemic stroke. This result supports the hypotheses that metabolic changes occurring in overweight person ultimately lead to events in the body that lead to acceleration of process of atherosclerosis culminating in to catastrophic cerebrovascular events. Finally, there is a strong need to reduce the trend toward growing obesity in ours like developing country to overcome such life threatening events in future.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: A direct measurement with ultrasound imaging. Circulation. 1986;74:1399–406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 2.Cupini LM, Pasqualetti P, Diomedi M, Vernieri F, Silvestrini M, Rizzato B, et al. Carotid artery intima-media thickness and lacunar versus nonlacunar infarcts. Stroke. 2002;33:689–94. doi: 10.1161/hs0302.103661. [DOI] [PubMed] [Google Scholar]
- 3.Touboul PJ, Elbaz A, Koller C, Lucas C, Adraï V, Chédru F, et al. Common carotid artery intima-media thickness and brain infarction: The Etude du Profile Genetique delInfarctus Cerebral (GENIC) case-control study: The GENIC Investigators. Circulation. 2000;102:313–8. doi: 10.1161/01.cir.102.3.313. [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto K, Sera Y, Nakamura H, Ueki Y, Miyake S. Correlation between common carotid arterial wall thickness and ischemic stroke in patients with type 2 diabetes mellitus. Metabolism. 2002;51:244–7. doi: 10.1053/meta.2002.28971. [DOI] [PubMed] [Google Scholar]
- 5.Vemmos KN, Tsivgoulis G, Spengos K, Papamichael CM, Zakopoulos N, Daffertshofer M, et al. Common carotid artery intima-media thickness in patients with brain infarction and intracerebral hemorrhage. Cerebrovasc Dis. 2004;17:280–6. doi: 10.1159/000077338. [DOI] [PubMed] [Google Scholar]
- 6.Paul J, Dasgupta S, Ghosh MK. Carotid artery intima media thickness as a surrogate marker of atherosclerosis in patient with chronic renal failure on hemodialysis. N Am J Med Sci. 2012;4:77–80. doi: 10.4103/1947-2714.93379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ni Mhurchu C, Rodgers A, Pan WH, Gu DF, Woodward M. Body mass index and cardiovascular disease in the Asia-Pacific Region: An overview of 33 cohorts involving 310 000 participants. Int J Epidemiol. 2004;33:751–8. doi: 10.1093/ije/dyh163. [DOI] [PubMed] [Google Scholar]
- 8.Kurth T, Gaziano JM, Rexrode KM, Kase CS, Cook NR, Manson JE, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111:1992–8. doi: 10.1161/01.CIR.0000161822.83163.B6. [DOI] [PubMed] [Google Scholar]
- 9.Wilson PW, Bozeman SR, Burton TM, Hoaglin DC, Ben-Joseph R, Pashos CL. Prediction of first events of coronary heart disease and stroke with consideration of adiposity. Circulation. 2008;118:124–30. doi: 10.1161/CIRCULATIONAHA.108.772962. [DOI] [PubMed] [Google Scholar]
- 10.Zhou M, Offer A, Yang G, Smith M, Hui G, Whitlock G, et al. Body mass index, blood pressure, and mortality from stroke: A nationally representative prospective study of 212000 Chinese men. Stroke. 2008;39:753–9. doi: 10.1161/STROKEAHA.107.495374. [DOI] [PubMed] [Google Scholar]
- 11.Song YM, Sung J, Smith GD, Ebrahim S. Body mass index and ischemic and hemorrhagic stroke: a prospective study in Korean men. Stroke. 2004;35:831–6. doi: 10.1161/01.STR.0000119386.22691.1C. [DOI] [PubMed] [Google Scholar]
- 12.Rexrode KM, Hennekens CH, Wellett WC, Colditz GA, Stampfer MJ, Rich-Edwards JW, et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA. 1997;277:1539–45. doi: 10.1001/jama.1997.03540430051032. [DOI] [PubMed] [Google Scholar]
- 13.Bazzano LA, Gu D, Whelton MR, Wu X, Chen CS, Duan X, et al. Body mass index and risk of stroke among Chinese men and women. Ann Neurol. 2010;67:11–20. doi: 10.1002/ana.21950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart CL, Hole DJ, Smith GD. Risk factors and 20-year stroke mortality in men and women in the Renfrew/Paisley Study in Scotland. Stroke. 1999;30:1999–2007. doi: 10.1161/01.str.30.10.1999. [DOI] [PubMed] [Google Scholar]
- 15.Harmsen P, Rosengren A, Tsipoglanni A, Wihelmsen L. Risk factors for stroke in middle-aged men in Gothborg, Sweden. Stroke. 1990;21:223–9. doi: 10.1161/01.str.21.2.223. [DOI] [PubMed] [Google Scholar]
- 16.Shaper AG, Wannamethee SG, Walker M. Body weight: Implications for the prevention of coronary heart disease, stroke, and diabetes mellitus in a cohort study of middle aged men. BMJ. 1997;314:1311–7. doi: 10.1136/bmj.314.7090.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haheim LL, Holme I, Hjermann I, Leren P. Risk factors of stroke incidence and mortality: A 12-year follow-up of the Oslo study. Stroke. 1993;24:1484–9. doi: 10.1161/01.str.24.10.1484. [DOI] [PubMed] [Google Scholar]
- 18.Jood K, Jern C, Wilhelmsen L, Rosengren A. Body mass index in mid-life is associated with a first stroke in men: A prospective study over 28 years. Stroke. 2004;35:2764–9. doi: 10.1161/01.STR.0000147715.58886.ad. [DOI] [PubMed] [Google Scholar]
- 19.Selmer R, Tverdal A. Body mass index and cardiovascular mortality at different levels of blood pressure: A prospective study of Norwegian men and women. J Epidemiol Commun Health. 1995;49:265–70. doi: 10.1136/jech.49.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oki I, Nakamura Y, Okamura T, Okayama A, Hayakawa T, Kita Y, et al. NIPPON DATA 80 Research Group. Body mass index and risk of stroke mortality among a random sample of Japanese adults: 19-year follow-up of NIPPON DATA 80. Cerebrovasc Dis. 2006;22:409–15. doi: 10.1159/000094860. [DOI] [PubMed] [Google Scholar]
- 21.Cui R, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, et al. JACC Study Group. Body mass index and mortality from cardiovascular disease among Japanese men and women: The JACC Study. Stroke. 2005;36:1377–82. doi: 10.1161/01.STR.0000169925.57251.4e. [DOI] [PubMed] [Google Scholar]
- 22.Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim Carotid Intima-Media Thickness Consensus (2004–2006) Cerebrovasc Dis. 2007;23:75–80. doi: 10.1159/000097034. [DOI] [PubMed] [Google Scholar]
- 23.Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 24.Folsom AR, Eckfeldt JH, Weitzman S, Ma J, Chambless LE, Barnes RW, et al. Relation of carotid artery wall thickness to diabetes mellitus, fasting glucose and insulin, body size, and physical activity Atherosclerosis Risk in Communities (ARIC) Study Investigators. Stroke. 1994;25:66–73. doi: 10.1161/01.str.25.1.66. [DOI] [PubMed] [Google Scholar]
- 25.Takami R, Takeda N, Hayashi M, Sasaki A, Kawachi S, Yoshino K, et al. Body fatness and fat distribution as predictors of metabolic abnormalities and early carotid atherosclerosis. Diabetes Care. 2001;24:1248–52. doi: 10.2337/diacare.24.7.1248. [DOI] [PubMed] [Google Scholar]
- 26.De Michele M, Panico S, Iannuzzi A, Celentano E, Ciardullo AV, Galasso R, et al. Association of obesity and central fat distribution with carotid artery wall thickening in middle-aged women. Stroke. 2002;33:2923–8. doi: 10.1161/01.str.0000038989.90931.be. [DOI] [PubMed] [Google Scholar]
- 27.Benfante R, Yano K, Hwang LJ, Curb JD, Kagan A, Ross W. Elevated serum cholesterol is a risk factor for both coronary heart disease and thromboembolic stroke in Hawaiian Japanese men: Implications of shared risk. Stroke. 1994;25:814–20. doi: 10.1161/01.str.25.4.814. [DOI] [PubMed] [Google Scholar]
- 28.Rexrode KM, Henneckens CH, Willett WC, Colditz GA, Stanpfer MJ, Rich-Edwards JW, et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA. 1997;277:1539–45. doi: 10.1001/jama.1997.03540430051032. [DOI] [PubMed] [Google Scholar]
- 29.Al-Roomi K, Heller RF, Holland T, Floate D, Wlodarczyk J. The importance of hypertension in the aetiology of infarctive and haemorrhagic stroke: The Lower Hunter Stroke Study. Med J Aust. 1992;157:452–5. [PubMed] [Google Scholar]
- 30.Petitti DB, Sidney S, Bernstein A, Wolf S, Quesenberry C, Ziel HK. Stroke in users of low-dose contraceptives. N Engl J Med. 1996;335:8–15. doi: 10.1056/NEJM199607043350102. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez BL, D’Agostino R, Abbott RD, Kagan A, Burchfiel CM, Yano K, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: A comparison of incidence and risk factor effects. Stroke. 2002;33:230–6. doi: 10.1161/hs0102.101081. [DOI] [PubMed] [Google Scholar]
- 32.Després JP, Cartier A, Côté M, Arsenault BJ. The concept of cardiometabolic risk: Bridging the fields of diabetology and cardiology. Ann Med. 2008;40:514–23. doi: 10.1080/07853890802004959. [DOI] [PubMed] [Google Scholar]
- 33.Lamotte C, Iliescu C, Libersa C, Gottrand F. Increased intimamedia thickness of the carotid artery in childhood: A systematic review of observational studies. Eur J Pediatr. 2011;170:719–29. doi: 10.1007/s00431-010-1328-y. [DOI] [PubMed] [Google Scholar]
- 34.Czernichow S, Bertrais S, Oppert JM, Galan P, Blacher J, Ducimetière P, et al. Body composition and fat repartition in relation to structure and function of large arteries in middle-aged adults. Int J Obes (Lond) 2005;29:826–32. doi: 10.1038/sj.ijo.0802986. [DOI] [PubMed] [Google Scholar]
- 35.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intimamedia thickness. Circulation. 2007;115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 36.Litwin M, Niermirska A. Intima-media thickness measurements in children with cardiovascular risk factors. Pediatr Nephrol. 2009;24:707–19. doi: 10.1007/s00467-008-0962-3. [DOI] [PubMed] [Google Scholar]
- 37.Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord. 2001;25:1047–56. doi: 10.1038/sj.ijo.0801615. [DOI] [PubMed] [Google Scholar]
- 38.Dey DK, Lissner L. Obesity in 70-year-old subjects as a risk factor for 15-year coronary heart disease incidence. Obes Res. 2003;11:817–27. doi: 10.1038/oby.2003.113. [DOI] [PubMed] [Google Scholar]
- 39.Nicklas BJ, Penninx BW, Cesari M, Kritchevsky SB, Newman AB, Kanaya AM, et al. Association of visceral adipose tissue with incident myocardial infarction in older men and women: The Health, Aging and Body Composition Study. Am J Epidemiol. 2004;160:741–9. doi: 10.1093/aje/kwh281. [DOI] [PubMed] [Google Scholar]
- 40.Dwivedi S, Aggarwal A, Singh S, Sharma V. Familial Xanthelasma with Dyslipidemia: Just Another Family Trait? N Am J Med Sci. 2012;4:238–40. doi: 10.4103/1947-2714.95910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dey DK, Rothenberg E, Sundh V, Bosaeus I, Steen B. Waist circumference, body mass index, and risk for stroke in older people: A 15 year longitudinal population study of 70-year-olds. J Am Geriatr Soc. 2002;50:1510–8. doi: 10.1046/j.1532-5415.2002.50406.x. [DOI] [PubMed] [Google Scholar]
- 42.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–43. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 43.Selvin E, Coresh J, Golden SH, Brancati FL, Folsom AR, Steffes MW. Glycemic control and coronary heart disease risk in persons with and without diabetes: The atherosclerosis risk in communities study. Arch Intern Med. 2005;165:1910–6. doi: 10.1001/archinte.165.16.1910. [DOI] [PubMed] [Google Scholar]
- 44.Singh R, Barden A, Mori T, Beilin L. Advanced glycation end-products: A review. Diabetologia. 2001;44:129–46. doi: 10.1007/s001250051591. [DOI] [PubMed] [Google Scholar]
- 45.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW., Jr Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White PJ, Marette A. Is omega-3 key to unlocking inflammatory in obesity? Diabetologia. 2006;49:1999–2001. doi: 10.1007/s00125-006-0346-9. [DOI] [PubMed] [Google Scholar]
- 47.Woo KS, Chook P, Yu CW, Sung RY, Qiao M, Leung SS, et al. Effects of diet and exercise on obesity-related vascular dysfunction in children. Circulation. 2004;109:1981–6. doi: 10.1161/01.CIR.0000126599.47470.BE. [DOI] [PubMed] [Google Scholar]
- 48.Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: Findings from thousand families cohort study. Br Med J. 2001;323:1280–4. doi: 10.1136/bmj.323.7324.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wunsch R, de Sousa G, Toschke AM, Reinehr T. Intimamedia thickness in obese children before and after weight loss. Pediatrics. 2006;118:2334–40. doi: 10.1542/peds.2006-0302. [DOI] [PubMed] [Google Scholar]
- 50.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–30. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]


