Although multiple bee stings are of rare incidence, they can cause many harmful reactions in humans. Massive inoculation of bee venom is reported to cause skin necrosis, shock hypertension, bleeding, hemolysis, thrombocytopenia, pancreatitis, (adult) respiratory distress syndrome, rhabdomyolysis, and acute renal failure (ARF).[1–12] Generally, three major reactions occur after bee inoculation as 1) local swelling and irritation, 2) generalized anaphylactic responses, and 3) serum sickness like symptoms, which include hemolysis, disseminated intravascular coagulation, rhabdomyolysis, and ARF.[13,14] In India, existences of honey combs are general in rural as well as urban areas but there are sparse data available in the literature on bee sting toxicity. To the best of our knowledge, there are no epidemiological studies reported until now on multiple bee sting-induced ARF and/or rhabdomyolysis in the Indian population. Hence, we performed a retrospective study for multiple bee sting-induced ARF and/or rhabdomyolysis.
The cases under International Classification of Diseases 2010 (Code T63.4) i.e., “venom of other arthropods” were screened retrospectively from January 2009 to December 2011 after Institutional Ethics Committee (IEC) approval. A total 32 cases were found. The inclusion criteria were the adult cases diagnosed to have multiple bee sting-induced rhabdomyolysis, ARF and/or other complication. Nine cases were selected in the study [Table 1, Figure 1 and 2], out of which six were diagnosed with acute kidney injury (AKI) and rhabdomyolysis, two with AKI only, and one with rhabdomyolysis only. The following type of information was collected from the patient records: Age, sex, complaints on admission, diagnosis, medical, medication, social and family history, days between bee stings and hospital admission, number of hemodialysis given, length of stay in the hospital; laboratory results like serum urea, serum creatinine, aspartate (AST), and alanine (ALT) aminotransferases, alkaline phosphatase (ALP), creatine kinase (CK), lactate dehydrogenase (LDH), total leukocyte count (TLC), hemoglobin (Hb), presence of myoglobin in urine, and other relevant data as per the case were obtained. All the patients had no significant abnormalities in serum potassium and sodium. The distribution of the AKI cases as per the risk, injury, failure, loss, end-stage (RIFLE) criteria was 1-‘Risk’, 6-‘Failure’, 1-‘Loss’.
Table 1.
Details of the patients
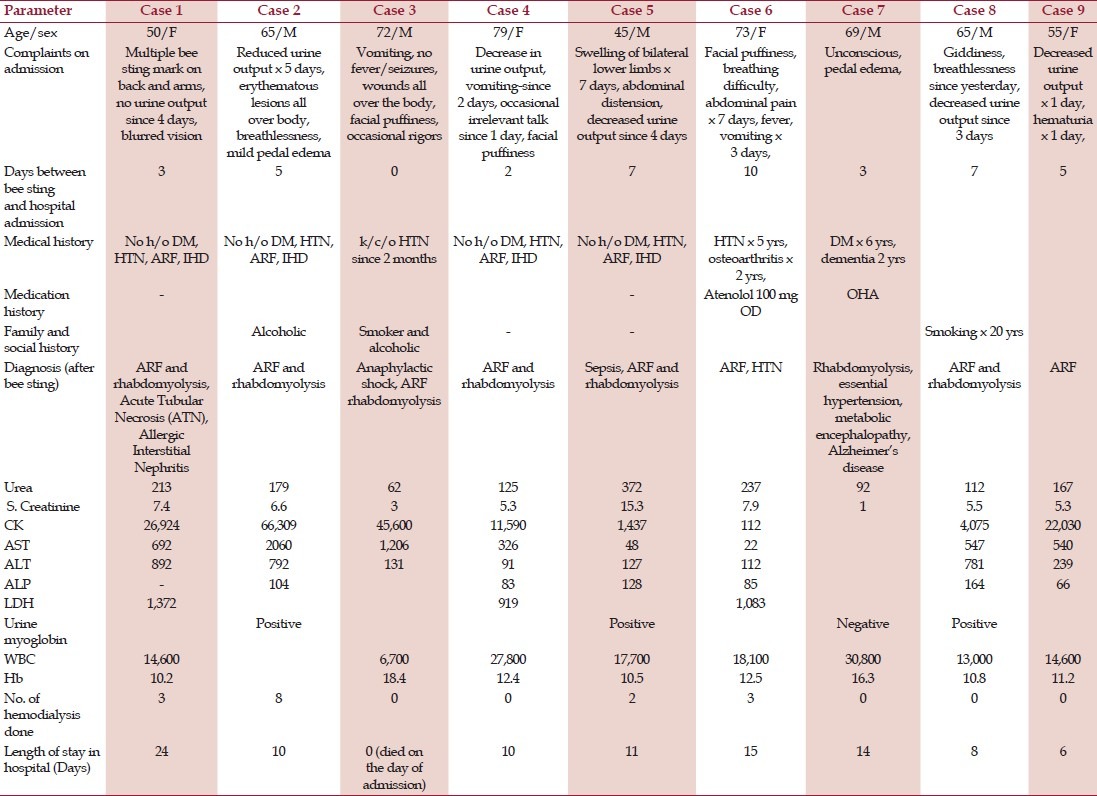
Figure 1.
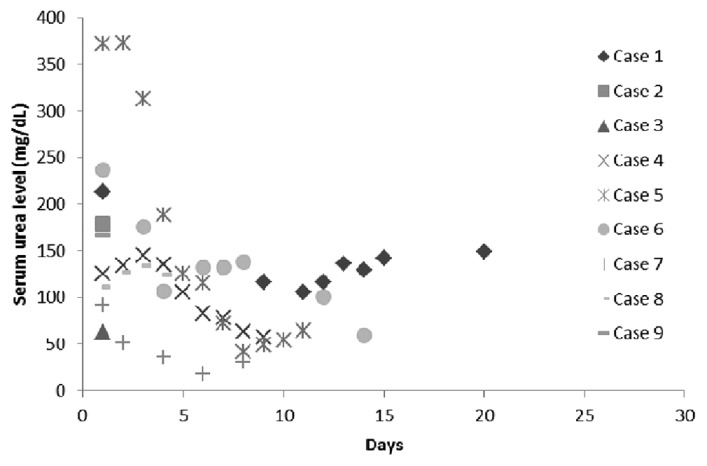
Serum urea levels of the patients
Figure 2.
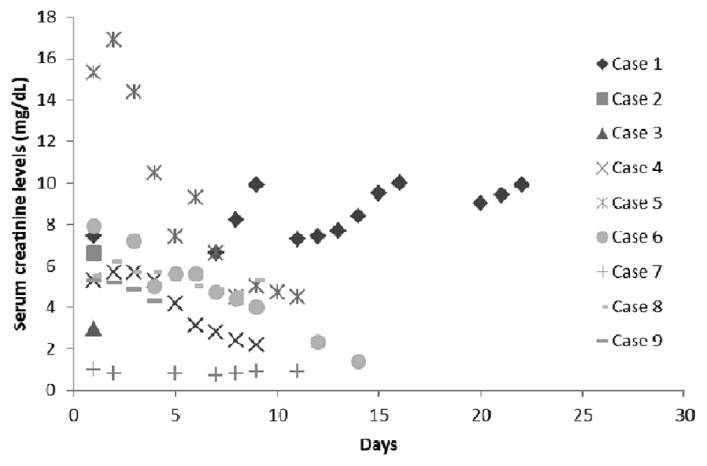
Serum creatinine of the patients
The unique points in each case are discussed below. In all the cases, for anaphylaxis standard treatment was given.
Case 1
The patient had mild pedal edema at the time of admission. She was unmarried, nulliparous, and had attained menopause 5 years back. She was hypertensive at the time of admission (blood pressure (BP) 160/90 mm Hg) and during the hospital stay she received regular anti-hypertensive treatment. Her creatine kinase levels on the day of admission was 26924 IU/L and decreased as follows 90, 53, and 22 IU/L on 7th, 9th, and 24th day of admission, respectively. Renal biopsy done was suggestive of acute tubular necrosis (ATN) eosinophils in the interstitium. In view of possibility of interstitial nephritis, intravenous pulse dose of methyl prednisone was given followed by oral steroids. Patient was better and was discharged.
Case 2
The CK levels of the patient decreased as follows 58,536, 15,374, 4,114, and 127 IU/L on 2nd, 3rd, 4th, and 8th day of admission, respectively. He was anuric throughout his hospital stay. His endotracheal culture grew pan drug resistant Acinetobacter. He developed altered sensorium he was not willing for further treatment and chose to get discharged.
Case 3
The patient got admitted on the same day of multiple bee sting inoculation. The pulse rate was 100 beats/min and blood pressure was 160/110 mm Hg. Other parameters were as follows- CK- 45600, chest x-ray-normal, electrocardiogram- normal. He expired following a cardiac event.
Cases 4 and 5
No significant unique points were observed.
Case 6
Her other laboratory results were as follows- lipase- 165 IU/L, amylase 150 IU/L. Before coming to the hospital she was admitted in other hospital was treated for viral fever for 5 days during which she did not take any anti hypertensive medication.
Case 7
Patient was unconscious for initial 8 days after admission. He had doll's eye during admission. His neutrophil count was 80% out of total leukocytes and toxic changes were found in it. His cerebrospinal fluid was normal and did not show any pathology.
Case 8
On the day of admission the patient had severe bradycardia and breathlessness. He had no chest pain. Other systemic examinations were normal. He was started on antihypertensive in view of persistently high blood pressure. The patient was symptomatically better at the time of discharge. His CK value on 3rd day was 504 IU/L.
Case 9
The patient complained of throat pain and changed voice on 3rd day of admission in view of that nasal endoscopy was performed and three honey bees (two from right part and one from left part) were suctioned out. Serum urea levels were not determined after first day of admission. CK values on 2nd and 5th day of admission were7,776 and 736 IU/L, respectively.
Anatomically, sting is a part of abdomen of female bees and is situated posteriorly. It can be used as ovipositor (egg lying) organ. Bees use it as a self-protective weapon against broad diversity of predators to inject venom into the tissues of victim. After envenomation, honey bees leave the stings at the site of inoculation. The sting is generally taken back into the abdomen when not in use. Medicinally, bee venom has anti-arthritic, anti-inflammatory, and anti-bacterial properties (without side effects).[15–20]
Bee venom, also known as apitoxin, contains many poisonous substances as-mellitin (hemolytic, vasoactive, contractile, and cellular anti-membrane properties), phospholipase A and B (cell membrane lysis action), apamine (a neurotoxin), mastocytolytic peptide (cytolytic and can cause histamine release), hyaluronidase (causes cell membrane lysis), histamine (causes increased vascular permeability), dopamine (causes hemodynamic effect), and minimine (causes cell membrane lysis). Among the poisonous substances, mellitin is the major (~50% by weight), most lethal, and primary pain-inducing component of bee venom.[21–24] The mechanism and pathogenesis of bee sting-induced kidney injury is still in dilemma. The possible factors associated with kidney insult are hemolysis, shock, direct tubular nephrotoxicity, and rhabdomyolysis.[9,21,25] As per study by Grisotto et al., the mechanisms of bee sting-induced ARF in clinically relevant model were found to be severe vasoconstriction, intense direct tubular toxicity, and rhabdomyolysis.[22] The relation between rhabdomyolysis and ARF is well-known. As no anti-venom exists, the appropriate management of non-allergic honey bee inoculation relies on aggressive supportive care.
Out of total ARF cases, six patients had decreased or no urine output after bee sting attack. A patient (Case 1) also complained of blurred vision after multiple bee inoculation, which subsided on 7th day of admission; interestingly, she had no bee sting inoculation in eyes. To our knowledge, this was also not reported in literature previously. Two of the patients in our study (Case 5 and 6) had abdominal distension and abdominal pain as complaints on admission as a complaint on admission. Occasional rigors and irrelevant talk were the complaints on admission by Case 3 and 4, respectively. Case 6 had fever and Case 7 had unconsciousness, while Case 2 and 6 had breathlessness on admission. After mass envenomation of bee stings, direct acting nephrotoxic components of honey bee venom and hemolysis have been anticipated as mechanisms for ATN.[1,5,26] Allergic interstitial nephritis (AIN) induced by wasp and hornet are common in literature. Here we have reported a case (Case 1) of bee sting-induced AIN and ATN which is first to the best of our knowledge. Recently, a case of nephritic syndrome induced by single bee sting in a child was reported.[27] Bee-sting is also reported to cause cavernous sinus thrombosis.[28] Death resulted from bee sting is uncommon. Here we have reported a case (Case 3) where the patient died because of anaphylactic shock after multiple bee sting attack. The patient died on the same day of multiple bee sting attack and hospital admission. The death in this case was probably due to anaphylaxis rather than venom toxicity. Acute pancreatitis is reported with single wasp and multiple hornet stings.[29,30] In our study, one patient (Case 6) had abdominal pain from last 7 days and her amylase and lipase levels were 165 IU/L (normal 30-100 U/L) and 150 IU/L (normal 145-216 U/L), respectively, which was 10 days after bee sting inoculation to the patient. No information on previous reports of serum amylase and lipase levels was found. Hence, amylase and lipase levels of the patient were normal or came to normal after 10 days of bee sting attack remains unanswered here. Multiple bee sting inoculation to a patient with Alzheimer's disease is not reported in the literature, but interestingly, our study has one case (Case 7) that had the both. As per some recent studies, bee venom could be a potential therapeutic agent for anti-neuro-inflammatory effects and may be helpful in reducing glutamatergic cell toxicity in neurodegenerative diseases.[31,32] When bee inoculation on the floor of nose, it is observed to cause floor of the nose lysis and lip abscess.[33] Here in our study, we had a case (Case 9) where the patient had throat pain and change in voice. Her vocal cords were normal but she had bilateral arytenoids congestion.
Though we conducted the study, we had certain limitations. For the complete presentation of all the cases, more clinical data is required but we were able to access limited data from the case records. As the study was retrospective, we could not counsel the patient regarding history of bee sting envenomation. There is no information about number bee stings inoculated to the patient/s to determine the quantity of the poison for toxicokinetic study. India has various different climatic zones and types of bee stings are also different in different geographical parts of India. There is no clear-cut data available on number of types/species of honey bees in India in literature but the commonly found species are Apis mellifera, Apis cerana, Apis dorsata, Apis laboriosa, Apis florea.[34] We could not retrieve any specific information about type/species and number of bees responsible for envenomation to each patient. In literature, we could not find the information on the exact morbidity of the patients because of bee sting injury. Our study was based on retrospective data from only one hospital and that too in southern zone of India. Various case reports have been reported in the literature on the health problems because of bee stings from India, but we could not get the literature having information on epidemiology of such incidences.
There are few studies available in literature on bee sting envenomation from south-Asian region. Out of the studies available in the literature, majority are case reports. Hence, there is need of regular and further reporting of the cases emphasizing the effects of bee venom for better understanding and management of the toxic effects of bee venom.
References
- 1.Mejia G, Arbelaez M, Henao JE, Sus AA, Arango JL. Acute renal failure due to multiple stings by Africanized bees. Ann Intern Med. 1986;104:210–1. doi: 10.7326/0003-4819-104-2-210. [DOI] [PubMed] [Google Scholar]
- 2.Mendes RP, Meira DA, Teixeira UA, Molinari H, Rodrigues PS, Coelho KY. Acidentepormultiplaspicadas de abelhas. Arq Bras Med. 1990;64:81–8. [Google Scholar]
- 3.Muñoz-Arizpe R, Valencia-Espinoza L, Velásquez-Jones L, Abarca-Franco C, Gamboa-Marrufo J, Valencia-Mayoral P. Africanized bee stings and pathogenesis of acute renal failure. Nephron. 1992;61:478. doi: 10.1159/000186975. [DOI] [PubMed] [Google Scholar]
- 4.Sert M, Tetiker T, Paydas S. Rhabdomyolysis and acute renal failure due to honeybee stings as an uncommon cause. Nephron. 1993;65:647. doi: 10.1159/000187584. [DOI] [PubMed] [Google Scholar]
- 5.Tumwine JK, Nkrumah FK. Acute renal failure and dermal necrosis due to bee stings: Report of a case in a child. Cent Afr J Med. 1990;36:202–4. [PubMed] [Google Scholar]
- 6.Daher Ede F, da Silva GB, Júnior, Bezerra GP, Pontes LB, Martins AM, Guimarães JA. Acute renal failure after massive honeybee stings. Rev Inst Med Trop Sao Paulo. 2003;45:45–50. doi: 10.1590/s0036-46652003000100010. [DOI] [PubMed] [Google Scholar]
- 7.Daisley H. Acute haemorrhagic pancreatitis following multiple stings by Africanized bees in Trinidad. Trans R Soc Trop Med Hyg. 1998;92:71–2. doi: 10.1016/s0035-9203(98)90960-9. [DOI] [PubMed] [Google Scholar]
- 8.Diaz-Sanchez CL, Lifshitz-Guinzberg A, Ignacio-Ibarra G, Halabe-Cherem J, Quinones-Galvan A. Survival after massive (42000) Africanized honeybee stings. Arch Intern Med. 1998;158:925–7. doi: 10.1001/archinte.158.8.925. [DOI] [PubMed] [Google Scholar]
- 9.Franca FO, Benvenuti LA, Fan HW, Dos Santos DR, Hain SH, Picchi-Martins FR, et al. Severe and fatal mass attacks by ‘killer’ bees (Africanized honey bees–Apis mellifera scutellata) in Brazil: Clinicopathological studies with measurement of serum venom concentrations. Q J Med. 1994;87:269–82. [PubMed] [Google Scholar]
- 10.Gabriel DP, Rodrigues AG, Jr, Barsante RC, dos Santos Silva V, Caramori JT, Martim LC, et al. Severe acute renal failure after massive attack of Africanized bees. Nephrol Dial Transplant. 2004;19:2680. doi: 10.1093/ndt/gfh440. [DOI] [PubMed] [Google Scholar]
- 11.Bresolin NL, Carvalho LC, Goes EC, Fernandes R, Barotto AM. Acute renal failure following massive attack by Africanized bee stings. Pediatr Nephrol. 2002;17:625–7. doi: 10.1007/s00467-002-0888-0. [DOI] [PubMed] [Google Scholar]
- 12.Kolecki P. Delayed toxic reaction following massive bee envenomation. Ann Emerg Med. 1999;33:114–6. doi: 10.1016/s0196-0644(99)70428-2. [DOI] [PubMed] [Google Scholar]
- 13.Golden DBK, Valentine MD. Insect sting allergy. In: Franklin EC, editor. Clinical immunology update. Edinburgh: Churchill Livingstone; 1981. pp. 169–96. [Google Scholar]
- 14.Light WC, Reisman RE, Shimizu M, Arbesman CE. Unusual reactions following insect stings.Clinical features and immunologic analysis. J Allergy Clin Immunol. 1977;59:391–7. doi: 10.1016/0091-6749(77)90024-0. [DOI] [PubMed] [Google Scholar]
- 15.Suh SJ, Kim KS, Kim MJ, Chang YC, Lee SD, Kim MS, et al. Effects of bee venom on protease activities and free radical damages in synovial fluid from type II collagen-induced rheumatoid arthritis rats. Toxicol In Vitro. 2006;20:1465–71. doi: 10.1016/j.tiv.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Lariviere WR, Melzack R. The bee venom test: A new tonic-pain test. Pain. 1996;66:271–7. doi: 10.1016/0304-3959(96)03075-8. [DOI] [PubMed] [Google Scholar]
- 17.Park HJ, Lee SH, Son DJ, Oh KW, Kim KH, Song HS, et al. Antiarthritic effect of bee venom: Inhibition of inflammation mediator generation by suppression of NF-kappaB through interaction with the p50 subunit. Arthritis Rheum. 2004;50:3504–15. doi: 10.1002/art.20626. [DOI] [PubMed] [Google Scholar]
- 18.Lee JD, Kim SY, Kim TW, Lee SH, Yang HI, Lee DI, et al. Anti-inflammatory effect of bee venom on type II collagen-induced arthritis. Am J Chin Med. 2004;32:361–7. doi: 10.1142/S0192415X04002016. [DOI] [PubMed] [Google Scholar]
- 19.Jang HS, Kim SK, Han JB, Ahn HJ, Bae H, Min BI. Effects of bee venom on the pro-inflammatory responses in RAW264.7 macrophage cell line. J Ethnopharmacol. 2005;99:157–60. doi: 10.1016/j.jep.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 20.Han S, Lee K, Yeo J, Kweon H, Woo S, Lee M, et al. Effect of honey bee venom on microglial cells nitric oxide and tumor necrosis factor-alpha production stimulated by LPS. J Ethnopharmacol. 2007;111:176–81. doi: 10.1016/j.jep.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Dos Reis MA, Costa RS, Coimbra TM, Teixeira VP. Acute renal failure in experimental envenomation with Africanized bee venom. Ren Fail. 1998;20:39–51. doi: 10.3109/08860229809045088. [DOI] [PubMed] [Google Scholar]
- 22.Grisotto LS, Mendes GE, Castro I, Baptista MA, Alves VA, Yu L, et al. Mechanisms of bee venom-induced acute renal failure. Toxicon. 2006;48:44–54. doi: 10.1016/j.toxicon.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Vetter RS, Visscher PK, Camazine S. Mass envenomations by honey bees and wasps. West J Med. 1999;170:223–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Fletcher JE, Michaux K, Jiang MS. Contribution of bee venom phospholipase A2 contamination in melittin fractions to presumed activation of tissue phospholipase A2. Toxicon. 1990;28:647–56. doi: 10.1016/0041-0101(90)90253-4. [DOI] [PubMed] [Google Scholar]
- 25.Dos Reis MA, Costa RS, Coimbra TM, Dantas M, Gomes UA. Renal changes induced by envenomation with Africanized bee venom in female Wistar rats. Kidney Blood Press Res. 1997;20:271–7. doi: 10.1159/000174157. [DOI] [PubMed] [Google Scholar]
- 26.Humblet Y, Sonnet J, van Ypersele de Strihou C. Bee stings and acute tubular necrosis. Nephron. 1982;31:187–8. doi: 10.1159/000182643. [DOI] [PubMed] [Google Scholar]
- 27.Kaarthigeyan K, Sivanandam S, Jothilakshmi K, Matthai J. Nephrotic syndrome following a single bee sting in a child. Indian J Nephrol. 2012;22:57–8. doi: 10.4103/0971-4065.83742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Senthikumaran S, Balamurugan N, Sweni S, Thirumalaikolundusubramanian P. Cavernous sinus thrombosis following bee sting. Int J Crit IIIn Inj Sci. 2011;1:167–8. doi: 10.4103/2229-5151.84808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma N, Balamurugeshan PK, Sharma A. Acute pancreatitis and acute renal failure following multiple hornet stings. J Venom Anim Toxins Incl Trop Dis. 2006;12:310–4. [Google Scholar]
- 30.Azad C, Parmar VR, Jat KR. Unusual fatal multiple-organ dysfunction and pancreatitis induced by a single wasp sting. J Venom Anim Toxins Incl Trop Dis. 2011;17:108–10. [Google Scholar]
- 31.Yang EJ, Jiang JH, Lee SM, Yang SC, Hwang HS, Lee MS, et al. Bee venom attenuates neuroinflammatory events and extends survival in amyotrophic lateral sclerosis models. J Neuroinflammation. 2010;7:69. doi: 10.1186/1742-2094-7-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee SM, Yang EJ, Choi SM, Kim SH, Baek MG, Jiang JH. Effects of bee venom on glutamate-induced toxicity in neuronal and glial cells. Evid Based Complement Alternat Med. 2012;2012:368196. doi: 10.1155/2012/368196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alemán Navas RM, Martínez Mendoza MG, Herrera H, Herrera HP. Floor of the nose mucosa lysis and labial abscess caused by a bee sting. Braz Dent J. 2009;20:249–53. doi: 10.1590/s0103-64402009000300014. [DOI] [PubMed] [Google Scholar]
- 34.Beesfordevelopment.org. Information portal: Honey bee species. [Accessed December 25, 2012]. at http://www.beesfordevelopment.org/portal/topic.php?id=53 and P=38 .


