Diabetes mellitus is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications. Diabetes care is complex and requires that many issues, beyond glycemic control, be addressed. A large body of evidence exists that supports a range of interventions to improve diabetes outcomes.
These standards of care are intended to provide clinicians, patients, researchers, payers, and other interested individuals with the components of diabetes care, general treatment goals, and tools to evaluate the quality of care. While individual preferences, comorbidities, and other patient factors may require modification of goals, targets that are desirable for most patients with diabetes are provided. Specifically titled sections of the standards address children with diabetes, pregnant women, and people with prediabetes. These standards are not intended to preclude clinical judgment or more extensive evaluation and management of the patient by other specialists as needed. For more detailed information about management of diabetes, refer to references 1–3.
The recommendations included are screening, diagnostic, and therapeutic actions that are known or believed to favorably affect health outcomes of patients with diabetes. A large number of these interventions have been shown to be cost-effective (4). A grading system (Table 1), developed by the American Diabetes Association (ADA) and modeled after existing methods, was utilized to clarify and codify the evidence that forms the basis for the recommendations. The level of evidence that supports each recommendation is listed after each recommendation using the letters A, B, C, or E.
Table 1.
ADA evidence grading system for clinical practice recommendations
| Level of evidence | Description |
| A | Clear evidence from well-conducted, generalizable, RCTs that are adequately powered, including:
|
Supportive evidence from well-conducted randomized controlled trials that are adequately powered, including:
| |
| B | Supportive evidence from well-conducted cohort studies
|
| Supportive evidence from a well-conducted case-control study | |
| C | Supportive evidence from poorly controlled or uncontrolled studies
|
| Conflicting evidence with the weight of evidence supporting the recommendation | |
| E | Expert consensus or clinical experience |
These standards of care are revised annually by the ADA's multidisciplinary Professional Practice Committee, incorporating new evidence. For the current revision, committee members systematically searched Medline for human studies related to each subsection and published since 1 January 2010. Recommendations (bulleted at the beginning of each subsection and also listed in the “Executive Summary: Standards of Medical Care in Diabetes—2012”) were revised based on new evidence or, in some cases, to clarify the prior recommendation or match the strength of the wording to the strength of the evidence. A table linking the changes in recommendations to new evidence can be reviewed at http://professional.diabetes.org/CPR_Search.aspx. Subsequently, as is the case for all Position Statements, the standards of care were reviewed and approved by the Executive Committee of ADA's Board of Directors, which includes health care professionals, scientists, and lay people.
Feedback from the larger clinical community was valuable for the 2012 revision of the standards. Readers who wish to comment on the “Standards of Medical Care in Diabetes—2012” are invited to do so at http://professional.diabetes.org/CPR_Search.aspx.
Members of the Professional Practice Committee disclose all potential financial conflicts of interest with industry. These disclosures were discussed at the onset of the standards revision meeting. Members of the committee, their employer, and their disclosed conflicts of interest are listed in the “Professional Practice Committee Members” table (see pg. S109). The American Diabetes Association funds development of the standards and all its position statements out of its general revenues and does not utilize industry support for these purposes.
I. CLASSIFICATION AND DIAGNOSIS
A. Classification
The classification of diabetes includes four clinical classes:
Type 1 diabetes (results from β-cell destruction, usually leading to absolute insulin deficiency)
Type 2 diabetes (results from a progressive insulin secretory defect on the background of insulin resistance)
Other specific types of diabetes due to other causes, e.g., genetic defects in β-cell function, genetic defects in insulin action, diseases of the exocrine pancreas (such as cystic fibrosis), and drug- or chemical-induced (such as in the treatment of HIV/AIDS or after organ transplantation)
Gestational diabetes mellitus (GDM) (diabetes diagnosed during pregnancy that is not clearly overt diabetes)
Some patients cannot be clearly classified as having type 1 or type 2 diabetes. Clinical presentation and disease progression vary considerably in both types of diabetes. Occasionally, patients who otherwise have type 2 diabetes may present with ketoacidosis. Similarly, patients with type 1 may have a late onset and slow (but relentless) progression of disease despite having features of autoimmune disease. Such difficulties in diagnosis may occur in children, adolescents, and adults. The true diagnosis may become more obvious over time.
B. Diagnosis of diabetes
Recommendations.
For decades, the diagnosis of diabetes was based on plasma glucose criteria, either the fasting plasma glucose (FPG) or the 2-h value in the 75-g oral glucose tolerance test (OGTT) (5).
In 2009, an International Expert Committee that included representatives of the American Diabetes Association (ADA), the International Diabetes Federation (IDF), and the European Association for the Study of Diabetes (EASD) recommended the use of the A1C test to diagnose diabetes, with a threshold of ≥6.5% (6), and ADA adopted this criterion in 2010 (5). The diagnostic test should be performed using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized or traceable to the Diabetes Control and Complications Trial (DCCT) reference assay. Point-of-care A1C assays, for which proficiency testing is not mandated, are not sufficiently accurate at this time to use for diagnostic purposes.
Epidemiologic datasets show a similar relationship between A1C and risk of retinopathy as has been shown for the corresponding FPG and 2-h PG thresholds. The A1C has several advantages to the FPG and OGTT, including greater convenience (since fasting is not required), evidence to suggest greater preanalytical stability, and less day-to-day perturbations during periods of stress and illness. These advantages must be balanced by greater cost, the limited availability of A1C testing in certain regions of the developing world, and the incomplete correlation between A1C and average glucose in certain individuals. In addition, HbA1c levels may vary with patients’ race/ethnicity (7,8). Some have posited that glycation rates differ by race (with, for example, African Americans having higher rates of glycation), but this is controversial. A recent epidemiologic study found that, when matched for FPG, African Americans (with and without diabetes) indeed had higher A1C than whites, but also had higher levels of fructosamine and glycated albumin and lower levels of 1,5-anhydroglucitol, suggesting that their glycemic burden (particularly postprandially) may be higher (9). Epidemiologic studies forming the framework for recommending use of the A1C to diagnose diabetes have all been in adult populations. Whether the cut point would be the same to diagnose children with type 2 diabetes is an area of uncertainty (10). A1C inaccurately reflects glycemia with certain anemias and hemoglobinopathies. For patients with an abnormal hemoglobin but normal red cell turnover, such as sickle cell trait, an A1C assay without interference from abnormal hemoglobins should be used (an updated list is available at www.ngsp.org/npsp.org/interf.asp). For conditions with abnormal red cell turnover, such as pregnancy, recent blood loss or transfusion, or some anemias, the diagnosis of diabetes must employ glucose criteria exclusively.
The established glucose criteria for the diagnosis of diabetes (FPG and 2-h PG) remain valid as well (Table 2). Just as there is less than 100% concordance between the FPG and 2-h PG tests, there is not perfect concordance between A1C and either glucose-based test. Analyses of National Health and Nutrition Examination Survey (NHANES) data indicate that, assuming universal screening of the undiagnosed, the A1C cut point of ≥6.5% identifies one-third fewer cases of undiagnosed diabetes than a fasting glucose cut point of ≥126 mg/dL (7.0 mmol/L) (11). However, in practice, a large portion of the diabetic population remains unaware of their condition. Thus, the lower sensitivity of A1C at the designated cut point may well be offset by the test's greater practicality, and wider application of a more convenient test (A1C) may actually increase the number of diagnoses made.
Table 2.
Criteria for the diagnosis of diabetes
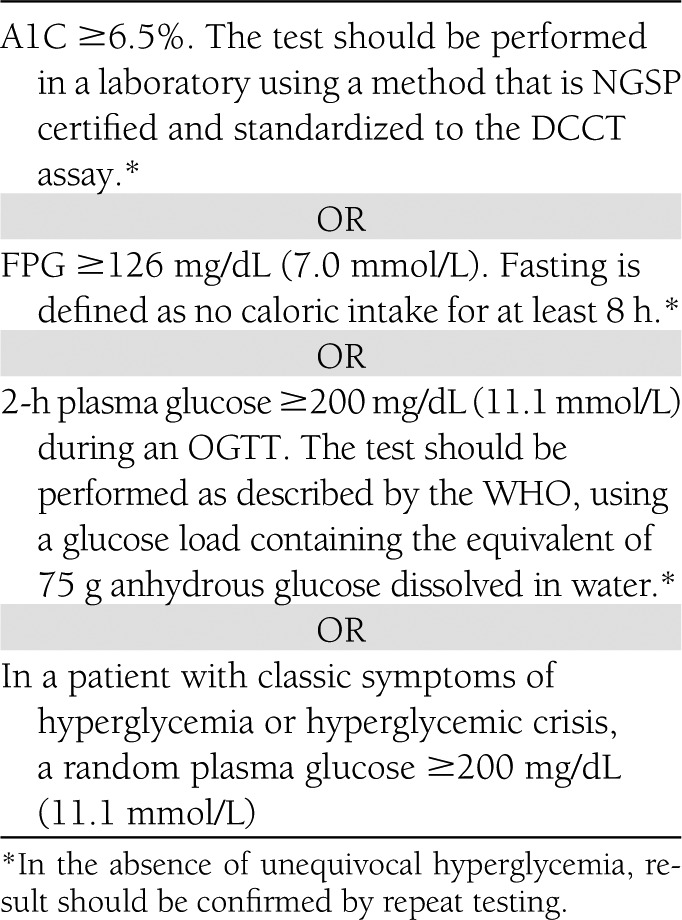
As with most diagnostic tests, a test result diagnostic of diabetes should be repeated to rule out laboratory error, unless the diagnosis is clear on clinical grounds, such as a patient with a hyperglycemic crisis or classic symptoms of hyperglycemia and a random plasma glucose ≥200 mg/dL. It is preferable that the same test be repeated for confirmation, since there will be a greater likelihood of concurrence in this case. For example, if the A1C is 7.0% and a repeat result is 6.8%, the diagnosis of diabetes is confirmed. However, if two different tests (such as A1C and FPG) are both above the diagnostic thresholds, the diagnosis of diabetes is also confirmed.
On the other hand, if two different tests are available in an individual and the results are discordant, the test whose result is above the diagnostic cut point should be repeated, and the diagnosis is made on the basis of the confirmed test. That is, if a patient meets the diabetes criterion of the A1C (two results ≥6.5%) but not the FPG (<126 mg/dL or 7.0 mmol/L), or vice versa, that person should be considered to have diabetes.
Since there is preanalytic and analytic variability of all the tests, it is also possible that when a test whose result was above the diagnostic threshold is repeated, the second value will be below the diagnostic cut point. This is least likely for A1C, somewhat more likely for FPG, and most likely for the 2-h PG. Barring a laboratory error, such patients are likely to have test results near the margins of the threshold for a diagnosis. The health care professional might opt to follow the patient closely and repeat the testing in 3–6 months. The current diagnostic criteria for diabetes are summarized in Table 2.
C. Categories of increased risk for diabetes (prediabetes)
In 1997 and 2003, The Expert Committee on Diagnosis and Classification of Diabetes Mellitus (12,13) recognized an intermediate group of individuals whose glucose levels, although not meeting criteria for diabetes, are nevertheless too high to be considered normal. These persons were defined as having impaired fasting glucose (IFG) (FPG levels 100 mg/dL [5.6 mmol/L] to 125 mg/dL [6.9 mmol/L]), or impaired glucose tolerance (IGT) (2-h values in the OGTT of 140 mg/dL [7.8 mmol/L] to 199 mg/dL [11.0 mmol/L]). It should be noted that the World Health Organization (WHO) and a number of other diabetes organizations define the cutoff for IFG at 110 mg/dL (6.1 mmol/L).
Individuals with IFG and/or IGT have been referred to as having prediabetes, indicating the relatively high risk for the future development of diabetes. IFG and IGT should not be viewed as clinical entities in their own right but rather risk factors for diabetes as well as cardiovascular disease (CVD). IFG and IGT are associated with obesity (especially abdominal or visceral obesity), dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension.
As is the case with the glucose measures, several prospective studies that used A1C to predict the progression to diabetes demonstrated a strong, continuous association between A1C and subsequent diabetes. In a systematic review of 44,203 individuals from 16 cohort studies with a follow-up interval averaging 5.6 years (range 2.8-12 years), those with an A1C between 5.5 and 6.0% had a substantially increased risk of diabetes with 5-year incidences ranging from 9–25%. An A1C range of 6.0 to 6.5% had a 5-year risk of developing diabetes between 25 to 50% and relative risk 20 times higher compared with an A1C of 5.0% (14). In a community-based study of black and white adults without diabetes, baseline A1C was a stronger predictor of subsequent diabetes and cardiovascular events than fasting glucose (15). Other analyses suggest that an A1C of 5.7% is associated with diabetes risk similar to that of the high-risk participants in the Diabetes Prevention Program (DPP).
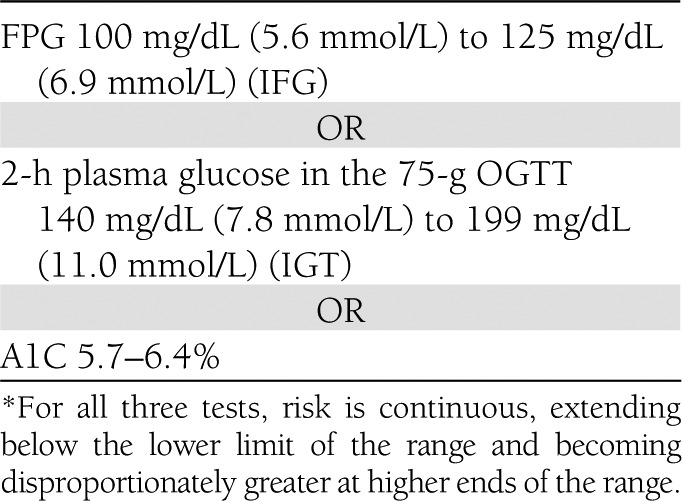
Hence, it is reasonable to consider an A1C range of 5.7 to 6.4% as identifying individuals with high risk for future diabetes, a state that may be referred to as prediabetes (5). As is the case for individuals found to have IFG and IGT, individuals with an A1C of 5.7–6.4% should be informed of their increased risk for diabetes as well as CVD and counseled about effective strategies to lower their risks (see section IV. PREVENTION/DELAY OF TYPE 2 DIABETES). As with glucose measurements, the continuum of risk is curvilinear, so that as A1C rises the risk of diabetes rises disproportionately (14). Accordingly, interventions should be most intensive and follow-up should be particularly vigilant for those with A1Cs >6.0%, who should be considered to be at very high risk. Table 3 summarizes the categories of increased risk for diabetes.
Table 3.
Categories of increased risk for diabetes (prediabetes)*
II. TESTING FOR DIABETES IN ASYMPTOMATIC PATIENTS
Recommendations.
Testing to detect type 2 diabetes and assess risk for future diabetes in asymptomatic people should be considered in adults of any age who are overweight or obese (BMI ≥25 kg/m2) and who have one or more additional risk factors for diabetes (Table 4). In those without these risk factors, testing should begin at age 45 years. (B)
If tests are normal, repeat testing at least at 3-year intervals is reasonable. (E)
To test for diabetes or to assess risk of future diabetes, the A1C, FPG, or 2-h 75-g OGTT are appropriate. (B)
In those identified with increased risk for future diabetes, identify and, if appropriate, treat other CVD risk factors. (B)
Table 4.
Criteria for testing for diabetes in asymptomatic adult individuals
1. Testing should be considered in all adults who are overweight (BMI ≥25 kg/m2*) and who have one or more additional risk factors:
|
| 2. In the absence of the above criteria, testing for diabetes should begin at age 45 years |
| 3. If results are normal, testing should be repeated at least at 3-year intervals, with consideration of more-frequent testing depending on initial results (e.g., those with prediabetes should be tested yearly) and risk status. |
At-risk BMI may be lower in some ethnic groups. PCOS, polycystic ovary syndrome.
For many illnesses, there is a major distinction between screening and diagnostic testing. However, for diabetes, the same tests would be used for “screening” as for diagnosis. Diabetes may be identified anywhere along a spectrum of clinical scenarios ranging from a seemingly low-risk individual who happens to have glucose testing, to a higher-risk individual whom the provider tests because of high suspicion of diabetes, to the symptomatic patient. The discussion herein is primarily framed as testing for diabetes in those without symptoms. The same assays used for testing for diabetes will also detect individuals with prediabetes.
A. Testing for type 2 diabetes and risk of future diabetes in adults
Prediabetes and diabetes meet established criteria for conditions in which early detection is appropriate. Both conditions are common, increasing in prevalence, and impose significant public health burdens. There is a long presymptomatic phase before the diagnosis of type 2 diabetes is usually made. Relatively simple tests are available to detect preclinical disease. Additionally, the duration of glycemic burden is a strong predictor of adverse outcomes, and effective interventions exist to prevent progression of prediabetes to diabetes (see section IV. PREVENTION/DELAY OF TYPE 2 DIABETES) and to reduce risk of complications of diabetes (see section V.I. PREVENTION AND MANAGEMENT OF DIABETES COMPLICATIONS).
Type 2 diabetes is frequently not diagnosed until complications appear, and approximately one-fourth of all people with diabetes in the U.S. may be undiagnosed. The effectiveness of early identification of prediabetes and diabetes through mass testing of asymptomatic individuals has not been proven definitively, and rigorous trials to provide such proof are unlikely to occur. In a large randomized controlled trial (RCT) in Europe, general practice patients between the ages of 40 and 69 years were screened for diabetes and then randomized by practice to routine care of diabetes or intensive treatment of multiple risk factors. After 5.3 years of follow-up, CVD risk factors were modestly but significantly more improved with intensive treatment. Incidence of first CVD event and mortality rates were not significantly different between groups (16). This study would seem to add support for early treatment of screen-detected diabetes, as risk factor control was excellent even in the routine treatment arm and both groups had lower event rates than predicted. The absence of a control unscreened arm limits the ability to definitely prove that screening impacts outcomes. Mathematical modeling studies suggest that screening independent of risk factors beginning at age 30 or age 45 years is highly cost-effective (<$11,000 per quality-adjusted life-year gained) (17).
Recommendations for testing for diabetes in asymptomatic, undiagnosed adults are listed in Table 4. Testing should be considered in adults of any age with BMI ≥25 kg/m2 and one or more of the known risk factors for diabetes. There is compelling evidence that lower BMI cut points suggest diabetes risk in some racial and ethnic groups. In a large multiethnic cohort study, for an equivalent incidence rate of diabetes conferred by a BMI of 30 kg/m2 in whites, the BMI cutoff value was 24 kg/m2 in South Asians, 25 kg/m2 in Chinese, and 26 kg/m2 African Americans (18).Disparities in screening rates, not explainable by insurance status, are highlighted by evidence that despite much higher prevalence of type 2 diabetes, non-Caucasians in an insured population are no more likely than Caucasians to be screened for diabetes (19). Because age is a major risk factor for diabetes, testing of those without other risk factors should begin no later than age 45 years.
Either A1C, FPG, or the 2-h OGTT is appropriate for testing. It should be noted that the tests do not necessarily detect diabetes in the same individuals. The efficacy of interventions for primary prevention of type 2 diabetes (20–26) has primarily been demonstrated among individuals with IGT, not for individuals with isolated IFG or for individuals with specific A1C levels.
The appropriate interval between tests is not known (27). The rationale for the 3-year interval is that false negatives will be repeated before substantial time elapses, and there is little likelihood that an individual will develop significant complications of diabetes within 3 years of a negative test result. In the modeling study, repeat screening every 3 or 5 years was cost-effective (17).
Because of the need for follow-up and discussion of abnormal results, testing should be carried out within the health care setting. Community screening outside a health care setting is not recommended because people with positive tests may not seek, or have access to, appropriate follow-up testing and care. Conversely, there may be failure to ensure appropriate repeat testing for individuals who test negative. Community screening may also be poorly targeted, i.e., it may fail to reach the groups most at risk and inappropriately test those at low risk (the worried well) or even those already diagnosed.
B. Testing for type 2 diabetes in children
The incidence of type 2 diabetes in adolescents has increased dramatically in the last decade, especially in minority populations (28), although the disease remains rare in the general pediatric population (29). Consistent with recommendations for adults, children and youth at increased risk for the presence or the development of type 2 diabetes should be tested within the healthcare setting (30). The recommendations of the ADA consensus statement on Type 2 Diabetes in Children and Youth, with some modifications, are summarized in Table 5 (30).
Table 5.
Testing for type 2 diabetes in asymptomatic children
| Criteria |
|
Plus any two of the following risk factors:
|
| Age of initiation: 10 years or at onset of puberty, if puberty occurs at a younger age |
| Frequency: every 3 years |
PCOS, polycystic ovary syndrome
C. Screening for type 1 diabetes
Generally, people with type 1 diabetes present with acute symptoms of diabetes and markedly elevated blood glucose levels, and most cases are diagnosed soon after the onset of hyperglycemia. However, evidence from type 1 prevention studies suggests that measurement of islet autoantibodies identifies individuals who are at risk for developing type 1 diabetes. Such testing may be appropriate in high-risk individuals, such as those with prior transient hyperglycemia or those who have relatives with type 1 diabetes, in the context of clinical research studies (see, e.g., http://www2.diabetestrialnet.org). Widespread clinical testing of asymptomatic low-risk individuals cannot currently be recommended, as it would identify very few individuals in the general population who are at risk. Individuals who screen positive should be counseled about their risk of developing diabetes. Clinical studies are being conducted to test various methods of preventing type 1 diabetes, or reversing early type 1 diabetes, in those with evidence of autoimmunity.
III. DETECTION AND DIAGNOSIS OF GESTATIONAL DIABETES MELLITUS (GDM)
Recommendations.
Screen for undiagnosed type 2 diabetes at the first prenatal visit in those with risk factors, using standard diagnostic criteria. (B)
In pregnant women not previously known to have diabetes, screen for GDM at 24–28 weeks’ gestation, using a 75-g 2-h OGTT and the diagnostic cut points in Table 6. (B)
Screen women with GDM for persistent diabetes at 6–12 weeks’ postpartum, using a test other than A1C. (E)
Women with a history of GDM should have lifelong screening for the development of diabetes or prediabetes at least every 3 years. (B)
Women with a history of GDM found to have prediabetes should receive lifestyle interventions or metformin to prevent diabetes. (A)
Table 6.
Screening for and diagnosis of GDM
| Perform a 75-g OGTT, with plasma glucose measurement fasting and at 1 and 2 h, at 24–28 weeks’ gestation in women not previously diagnosed with overt diabetes. |
| The OGTT should be performed in the morning after an overnight fast of at least 8 h. |
The diagnosis of GDM is made when any of the following plasma glucose values are exceeded:
|
For many years, GDM was defined as any degree of glucose intolerance with onset or first recognition during pregnancy (12), whether or not the condition persisted after pregnancy, and not excluding the possibility that unrecognized glucose intolerance may have antedated or begun concomitantly with the pregnancy. This definition facilitated a uniform strategy for detection and classification of GDM, but its limitations were recognized for many years. As the ongoing epidemic of obesity and diabetes has led to more type 2 diabetes in women of childbearing age, the number of pregnant women with undiagnosed type 2 diabetes has increased (31). Because of this, it is reasonable to screen women with risk factors for type 2 diabetes (Table 4) for diabetes at their initial prenatal visit, using standard diagnostic criteria (Table 2). Women found to have diabetes at this visit should receive a diagnosis of overt, not gestational, diabetes.
GDM carries risks for the mother and neonate. The Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study (32), a large-scale (∼25,000 pregnant women) multinational epidemiologic study, demonstrated that risk of adverse maternal, fetal, and neonatal outcomes continuously increased as a function of maternal glycemia at 24–28 weeks, even within ranges previously considered normal for pregnancy. For most complications, there was no threshold for risk. These results have led to careful reconsideration of the diagnostic criteria for GDM. After deliberations in 2008–2009, the International Association of Diabetes and Pregnancy Study Groups (IADPSG), an international consensus group with representatives from multiple obstetrical and diabetes organizations, including ADA, developed revised recommendations for diagnosing GDM. The group recommended that all women not known to have prior diabetes undergo a 75-g OGTT at 24–28 weeks of gestation. Additionally, the group developed diagnostic cut points for the fasting, 1-h, and 2-h plasma glucose measurements that conveyed an odds ratio for adverse outcomes of at least 1.75 compared with women with the mean glucose levels in the HAPO study. Current screening and diagnostic strategies, based on the IADPSG statement (33), are outlined in Table 6.
These new criteria will significantly increase the prevalence of GDM, primarily because only one abnormal value, not two, is sufficient to make the diagnosis. ADA recognizes the anticipated significant increase in the incidence of GDM diagnosed by these criteria and is sensitive to concerns about the “medicalization” of pregnancies previously categorized as normal. These diagnostic criteria changes are being made in the context of worrisome worldwide increases in obesity and diabetes rates, with the intent of optimizing gestational outcomes for women and their babies.
Admittedly, there are few data from randomized clinical trials regarding therapeutic interventions in women who will now be diagnosed with GDM based on only one blood glucose value above the specified cut points (in contrast to the older criteria that stipulated at least two abnormal values). However, there is emerging observational and retrospective evidence that women diagnosed with the new criteria (even if they would not have been diagnosed with older criteria) have increased rates of poor pregnancy outcomes similar to those of women with GDM by prior criteria (34,35). Expected benefits to these pregnancies and offspring is inferred from intervention trials that focused on women with more mild hyperglycemia than identified using older GDM diagnostic criteria and that found modest benefits (36,37). The frequency of follow-up and blood glucose monitoring for these women is not yet clear but likely to be less intensive than for women diagnosed by the older criteria. It is important to note that 80–90% of women in both of the mild GDM studies (whose glucose values overlapped with the thresholds recommended herein) could be managed with lifestyle therapy alone.
The American College of Obstetrics and Gynecology announced in 2011 that they continue to recommend use of prior diagnostic criteria for GDM (38). Several other countries have adopted the new criteria, and a report from the WHO on this topic is pending at the time of the publication of these standards.
Because some cases of GDM may represent preexisting undiagnosed type 2 diabetes, women with a history of GDM should be screened for diabetes 6–12 weeks’ postpartum, using nonpregnant OGTT criteria. Because of their prepartum treatment for hyperglycemia, use of the A1C for diagnosis of persistent diabetes at the postpartum visit is not recommended (39). Women with a history of GDM have a greatly increased subsequent risk for diabetes (40) and should be followed up with subsequent screening for the development of diabetes or prediabetes, as outlined in section II. TESTING FOR DIABETES IN ASYMPTOMATIC PATIENTS.
Lifestyle interventions or metformin should be offered to women with a history of GDM who develop prediabetes, as discussed in section IV. PREVENTION/DELAY OF TYPE 2 DIABETES.
IV. PREVENTION/DELAY OF TYPE 2 DIABETES
Recommendations.
Patients with IGT (A), IFG (E), or an A1C of 5.7–6.4% (E) should be referred to an effective ongoing support program targeting weight loss of 7% of body weight and increasing physical activity to at least 150 min per week of moderate activity such as walking.
Follow-up counseling appears to be important for success. (B)
Based on the cost-effectiveness of diabetes prevention, such programs should be covered by third-party payers. (B)
Metformin therapy for prevention of type 2 diabetes may be considered in those with IGT (A), IFG (E), or an A1C of 5.7–6.4% (E), especially for those with BMI >35 kg/m2, age <60 years, and women with prior GDM. (A)
At least annual monitoring for the development of diabetes in those with prediabetes is suggested. (E)
RCTs have shown that individuals at high risk for developing type 2 diabetes (those with IFG, IGT, or both) can significantly decrease the rate of onset of diabetes with particular interventions (20–26). These include intensive lifestyle modification programs that have been shown to be very effective (∼58% reduction after 3 years) and use of the pharmacologic agents metformin, α glucosidase inhibitors, orlistat, and thiazolidinediones, each of which has been shown to decrease incident diabetes to various degrees. Follow-up of three large studies of lifestyle intervention has shown sustained reduction in the rate of conversion to type 2 diabetes, with 43% reduction at 20 years in the Da Qing study (41), 43% reduction at 7 years in the Finnish Diabetes Prevention Study (DPS) (42), and 34% reduction at 10 years in the U.S. Diabetes Prevention Program Outcome Study (DPPOS) (43). A cost-effectiveness model suggested that lifestyle interventions as delivered in the DPP are cost-effective (44), and actual cost data from the DPP and DPPOS confirm that lifestyle interventions are highly cost-effective (45). Group delivery of the DPP intervention in community settings has the potential to be significantly less expensive while still achieving similar weight loss (46).
Based on the results of clinical trials and the known risks of progression of prediabetes to diabetes, persons with an A1C of 5.7–6.4%, IGT, or IFG should be counseled on lifestyle changes with goals similar to those of the DPP (7% weight loss and moderate physical activity of at least 150 min per week). Regarding drug therapy for diabetes prevention, a consensus panel felt that metformin should be the only drug considered (47). For other drugs, issues of cost, side effects, and lack of persistence of effect in some studies (48) require consideration. Metformin was less effective than lifestyle intervention in the DPP and DPPOS but may be cost-saving over a 10-year period (45). It was as effective as lifestyle in participants with a BMI of at least 35 kg/m2 (20), and in women with a history of GDM, metformin and intensive lifestyle led to an equivalent 50% reduction in the risk of diabetes (49). Metformin therefore might reasonably be recommended for very-high-risk individuals (those with a history of GDM, the very obese, and/or those with more severe or progressive hyperglycemia). Of note in the DPP, metformin was not significantly better than placebo in those over age 60 years.
V. DIABETES CARE
A. Initial evaluation
A complete medical evaluation should be performed to classify the diabetes, detect the presence of diabetes complications, review previous treatment and glycemic control in patients with established diabetes, assist in formulating a management plan, and provide a basis for continuing care. Laboratory tests appropriate to the evaluation of each patient's medical condition should be performed. A focus on the components of comprehensive care (Table 7) will assist the health care team to ensure optimal management of the patient with diabetes.
Table 7.
Components of the comprehensive diabetes evaluation
Medical history
|
Physical examination
|
Laboratory evaluation
|
Referrals
|
See appropriate referrals for these categories.
B. Management
People with diabetes should receive medical care from a physician-coordinated team. Such teams may include, but are not limited to, physicians, nurse practitioners, physician's assistants, nurses, dietitians, pharmacists, and mental health professionals with expertise and a special interest in diabetes. It is essential in this collaborative and integrated team approach that individuals with diabetes assume an active role in their care.
The management plan should be formulated as a collaborative therapeutic alliance among the patient and family, the physician, and other members of the health care team. A variety of strategies and techniques should be used to provide adequate education and development of problem-solving skills in the various aspects of diabetes management. Implementation of the management plan requires that each aspect is understood and agreed to by the patient and the care providers and that the goals and treatment plan are reasonable. Any plan should recognize diabetes self-management education (DSME) and on-going diabetes support as an integral component of care. In developing the plan, consideration should be given to the patient's age, school or work schedule and conditions, physical activity, eating patterns, social situation and cultural factors, and presence of complications of diabetes or other medical conditions.
C. Glycemic control
1. Assessment of glycemic control.
Two primary techniques are available for health providers and patients to assess the effectiveness of the management plan on glycemic control: patient self-monitoring of blood glucose (SMBG) or interstitial glucose, and A1C.
a. Glucose monitoring
Recommendations.
SMBG should be carried out three or more times daily for patients using multiple insulin injections or insulin pump therapy. (B)
For patients using less-frequent insulin injections, noninsulin therapies, or medical nutrition therapy (MNT) alone, SMBG may be useful as a guide to management. (E)
To achieve postprandial glucose targets, postprandial SMBG may be appropriate. (E)
When prescribing SMBG, ensure that patients receive initial instruction in, and routine follow-up evaluation of, SMBG technique and their ability to use data to adjust therapy. (E)
Continuous glucose monitoring (CGM) in conjunction with intensive insulin regimens can be a useful tool to lower A1C in selected adults (age ≥25 years) with type 1 diabetes. (A)
Although the evidence for A1C-lowering is less strong in children, teens, and younger adults, CGM may be helpful in these groups. Success correlates with adherence to ongoing use of the device. (C)
CGM may be a supplemental tool to SMBG in those with hypoglycemia unawareness and/or frequent hypoglycemic episodes. (E)
Major clinical trials of insulin-treated patients that demonstrated the benefits of intensive glycemic control on diabetes complications have included SMBG as part of multifactorial interventions, suggesting that SMBG is a component of effective therapy. SMBG allows patients to evaluate their individual response to therapy and assess whether glycemic targets are being achieved. Results of SMBG can be useful in preventing hypoglycemia and adjusting medications (particularly prandial insulin doses), MNT, and physical activity.
The frequency and timing of SMBG should be dictated by the particular needs and goals of the patient. SMBG is especially important for patients treated with insulin to monitor for and prevent asymptomatic hypoglycemia and hyperglycemia. For most patients with type 1 diabetes and pregnant women taking insulin, SMBG is recommended three or more times daily. For these populations, significantly more frequent testing may be required to reach A1C targets safely without hypoglycemia and for hypoglycemia detection prior to critical tasks such as driving. In a large database study of almost 27,000 children and adolescents with type 1 diabetes, after adjustment for multiple confounders, increased daily frequency of SMBG was significantly associated with lower A1C (−0.2% per additional test per day, leveling off at 5 tests per day) and with fewer acute complications (50). The optimal frequency and timing of SMBG for patients with type 2 diabetes on noninsulin therapy is unclear. A meta-analysis of SMBG in non–insulin-treated patients with type 2 diabetes concluded that some regimens of SMBG were associated with a reduction in A1C of −0.4%. However, many of the studies in this analysis also included patient education with diet and exercise counseling and, in some cases, pharmacologic intervention, making it difficult to assess the contribution of SMBG alone to improved control (51). Several randomized trials have called into question the clinical utility and cost-effectiveness of routine SMBG in non–insulin-treated patients (52–54).
Because the accuracy of SMBG is instrument and user dependent (55), it is important to evaluate each patient's monitoring technique, both initially and at regular intervals thereafter. In addition, optimal use of SMBG requires proper interpretation of the data. Patients should be taught how to use the data to adjust food intake, exercise, or pharmacological therapy to achieve specific glycemic goals, and these skills should be reevaluated periodically.
Real-time CGM through the measurement of interstitial glucose (which correlates well with plasma glucose) is available. These sensors require calibration with SMBG, and the latter are still recommended for making acute treatment decisions. CGM devices have alarms for hypo- and hyperglycemic excursions. Small studies in selected patients with type 1 diabetes have suggested that CGM use reduces the time spent in hypo- and hyperglycemic ranges and may modestly improve glycemic control. A 26-week randomized trial of 322 type 1 patients showed that adults age 25 years and older using intensive insulin therapy and CGM experienced a 0.5% reduction in A1C (from ∼7.6–7.1%) compared with usual intensive insulin therapy with SMBG (56). Sensor use in children, teens, and adults to age 24 years did not result in significant A1C lowering, and there was no significant difference in hypoglycemia in any group. Importantly, the greatest predictor of A1C lowering in this study for all age-groups was frequency of sensor use, which was lower in younger age-groups. In a smaller RCT of 129 adults and children with baseline A1C <7.0%, outcomes combining A1C and hypoglycemia favored the group utilizing CGM, suggesting that CGM is also beneficial for individuals with type 1 diabetes who have already achieved excellent control (57).
A recent RCT of 120 children and adults with type 1 diabetes with baseline A1C <7.5% showed that real-time CGM was associated with reduced time spent in hypoglycemia and a small but significant decrease in A1C compared with blinded CGM (58). A trial comparing CGM plus insulin pump to SMBG plus multiple injections of insulin in adults and children with type 1 diabetes showed significantly greater improvements in A1C with “sensor augmented pump” therapy (59,60), but this trial did not isolate the effect of CGM itself. Although CGM is an evolving technology, these data suggest that, in appropriately selected patients who are motivated to wear it most of the time, it may offer benefit. CGM may be particularly useful in those with hypoglycemia unawareness and/or frequent episodes of hypoglycemia, and studies in this area are ongoing. CGM forms the underpinning for the development of pumps that suspend insulin delivery when hypoglycemia is developing as well as for the burgeoning work on “artificial pancreas” systems.
b. A1C
Recommendations.
Perform the A1C test at least two times a year in patients who are meeting treatment goals (and who have stable glycemic control). (E)
Perform the A1C test quarterly in patients whose therapy has changed or who are not meeting glycemic goals. (E)
Use of point-of-care (POC) testing for A1C provides the opportunity for more timely treatment changes. (E)
Because A1C is thought to reflect average glycemia over several months (55), and has strong predictive value for diabetes complications (61,62), A1C testing should be performed routinely in all patients with diabetes, at initial assessment and then as part of continuing care. Measurement approximately every 3 months determines whether a patient's glycemic targets have been reached and maintained. For any individual patient, the frequency of A1C testing should be dependent on the clinical situation, the treatment regimen used, and the judgment of the clinician. Some patients with stable glycemia well within target may do well with testing only twice per year, while unstable or highly intensively managed patients (e.g., pregnant type 1 women) may be tested more frequently than every 3 months. The availability of the A1C result at the time that the patient is seen (POC testing) has been reported in small studies to result in increased intensification of therapy and improvement in glycemic control (63,64). However, two recent systematic reviews and meta-analyses found no significant difference in A1C between POC and laboratory A1C usage (65,66).
The A1C test is subject to certain limitations. Conditions that affect erythrocyte turnover (hemolysis, blood loss) and hemoglobin variants must be considered, particularly when the A1C result does not correlate with the patient's clinical situation (55). In addition, A1C does not provide a measure of glycemic variability or hypoglycemia. For patients prone to glycemic variability (especially type 1 patients, or type 2 patients with severe insulin deficiency), glycemic control is best judged by the combination of results of SMBG testing and the A1C. The A1C may also serve as a check on the accuracy of the patient's meter (or the patient's reported SMBG results) and the adequacy of the SMBG testing schedule.
Table 8 contains the correlation between A1C levels and mean plasma glucose levels based on data from the international A1C-Derived Average Glucose (ADAG) trial utilizing frequent SMBG and CGM in 507 adults (83% Caucasian) with type 1, type 2, and no diabetes (67). ADA and the American Association of Clinical Chemists have determined that the correlation (r = 0.92) is strong enough to justify reporting both an A1C result and an estimated average glucose (eAG) result when a clinician orders the A1C test. The table in pre-2009 versions of the “Standards of Medical Care in Diabetes” describing the correlation between A1C and mean glucose was derived from relatively sparse data (one 7-point profile over 1 day per A1C reading) in the primarily Caucasian type 1 participants in the DCCT (68). Clinicians should note that the numbers in the table are now different, as they are based on ∼2,800 readings per A1C in the ADAG trial.
Table 8.
Correlation of A1C with average glucose
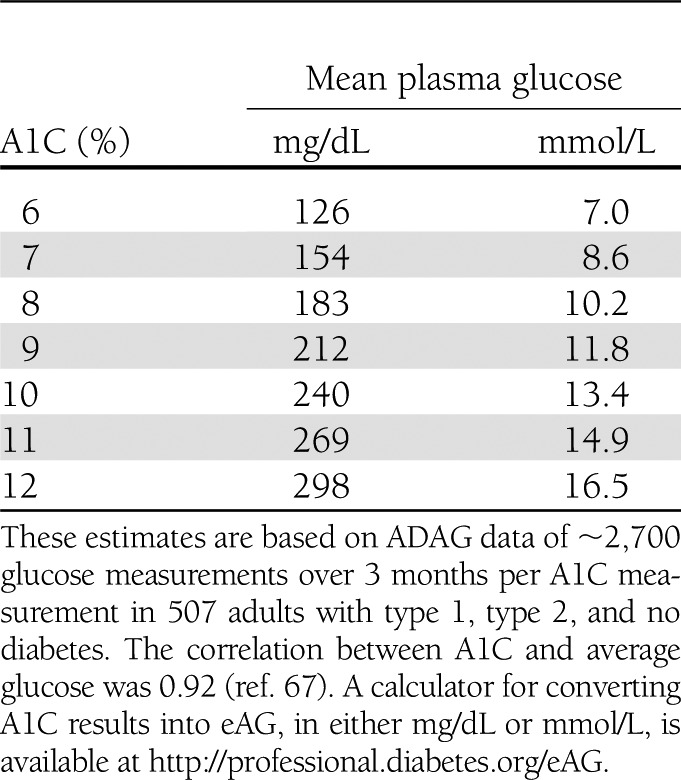
In the ADAG study, there were no significant differences among racial and ethnic groups in the regression lines between A1C and mean glucose, although there was a trend toward a difference between African/African American and Caucasian participants. A small study comparing A1C to CGM data in type 1 children found a highly statistically significant correlation between A1C and mean blood glucose, although the correlation (r = 0.7) was significantly lower than in the ADAG trial (69). Whether there are significant differences in how A1C relates to average glucose in children or in African American patients is an area for further study. For the time being, the question has not led to different recommendations about testing A1C or to different interpretations of the clinical meaning of given levels of A1C in those populations.
For patients in whom A1C/eAG and measured blood glucose appear discrepant, clinicians should consider the possibilities of hemoglobinopathy or altered red cell turnover, and the options of more frequent and/or different timing of SMBG or use of CGM. Other measures of chronic glycemia such as fructosamine are available, but their linkage to average glucose and their prognostic significance are not as clear as for A1C.
2. Glycemic goals in adults.
Recommendations.
Lowering A1C to below or around 7% has been shown to reduce microvascular complications of diabetes, and if implemented soon after the diagnosis of diabetes is associated with long-term reduction in macrovascular disease. Therefore, a reasonable A1C goal for many nonpregnant adults is <7%. (B)
Providers might reasonably suggest more stringent A1C goals (such as <6.5%) for selected individual patients, if this can be achieved without significant hypoglycemia or other adverse effects of treatment. Appropriate patients might include those with short duration of diabetes, long life expectancy, and no significant CVD. (C)
Less-stringent A1C goals (such as <8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, extensive comorbid conditions, and those with longstanding diabetes in whom the general goal is difficult to attain despite DSME, appropriate glucose monitoring, and effective doses of multiple glucose-lowering agents including insulin. (B)
Hyperglycemia defines diabetes, and glycemic control is fundamental to the management of diabetes. The DCCT study (61), a prospective RCT of intensive versus standard glycemic control in patients with relatively recently diagnosed type 1 diabetes, showed definitively that improved glycemic control is associated with significantly decreased rates of microvascular (retinopathy and nephropathy) and neuropathic complications. Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications (EDIC) study (70,71) demonstrated persistence of these microvascular benefits in previously intensively treated subjects, even though their glycemic control approximated that of previous standard arm subjects during follow-up.
The Kumamoto Study (72) and U.K. Prospective Diabetes Study (UKPDS) (73,74) confirmed that intensive glycemic control was associated with significantly decreased rates of microvascular and neuropathic complications in patients with type 2 diabetes. Long-term follow-up of the UKPDS cohorts showed persistence of the effect of early glycemic control on most microvascular complications (75).
Subsequent trials in patients with more-long-standing type 2 diabetes, designed primarily to look at the role of intensive glycemic control on cardiovascular outcomes, also confirmed a benefit, although more modest, on onset or progression of microvascular complications. The Veterans Affairs Diabetes Trial (VADT) showed significant reductions in albuminuria with intensive (achieved median A1C 6.9%) compared with standard glycemic control but no difference in retinopathy and neuropathy (76,77). The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) study of intensive versus standard glycemic control in type 2 diabetes found a statistically significant reduction in albuminuria, but not neuropathy or retinopathy, with an A1C target of <6.5% (achieved median A1C 6.3%) compared with standard therapy achieving a median A1C of 7.0% (78). Recent analyses from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial have shown lower rates of onset or progression of early-stage microvascular complications in the intensive glycemic control arm compared with the standard arm (79,80).
Epidemiological analyses of the DCCT and UKPDS (61,62) demonstrate a curvilinear relationship between A1C and microvascular complications. Such analyses suggest that, on a population level, the greatest number of complications will be averted by taking patients from very poor control to fair or good control. These analyses also suggest that further lowering of A1C from 7 to 6% is associated with further reduction in the risk of microvascular complications, albeit the absolute risk reductions become much smaller. Given the substantially increased risk of hypoglycemia (particularly in those with type 1 diabetes, but also in the recent type 2 trials), the concerning mortality findings in the ACCORD trial (81), and the relatively much greater effort required to achieve near-normoglycemia, the risks of lower glycemic targets may outweigh the potential benefits on microvascular complications on a population level. However, selected individual patients, especially those with little comorbidity and long life expectancy (who may reap the benefits of further lowering of glycemia below 7%) may, based on provider judgment and patient preferences, adopt more-intensive glycemic targets (for example, an A1C target <6.5%) as long as significant hypoglycemia does not become a barrier.
CVD, a more common cause of death in populations with diabetes than microvascular complications, is less clearly impacted by levels of hyperglycemia or intensity of glycemic control. In the DCCT, there was a trend toward lower risk of CVD events with intensive control, and in 9-year post-DCCT follow-up of the EDIC cohort participants previously randomized to the intensive arm had a significant 42% reduction in CVD outcomes and a significant 57% reduction in the risk of nonfatal myocardial infarction (MI), stroke, or CVD death compared with those previously in the standard arm (82). The benefit of intensive glycemic control in this type 1 cohort has recently been shown to persist for several decades (83).
In type 2 diabetes, there is evidence that more-intensive treatment of glycemia in newly diagnosed patients may reduce long-term CVD rates. During the UKPDS trial, there was a 16% reduction in cardiovascular events (combined fatal or nonfatal MI and sudden death) in the intensive glycemic control arm, although this difference was not statistically significant (P = 0.052), and there was no suggestion of benefit on other CVD outcomes such as stroke. However, after 10 years of follow-up, those originally randomized to intensive glycemic control had significant long-term reductions in MI (15% with sulfonylurea or insulin as initial pharmacotherapy, 33% with metformin as initial pharmacotherapy) and in all-cause mortality (13 and 27%, respectively) (75).
However, results of three more-recent large trials (ACCORD, ADVANCE, and VADT) suggest no significant reduction in CVD outcomes with intensive glycemic control in these populations, who had more advanced diabetes than UKPDS participants. All three of these trials were conducted in participants with more-long-standing diabetes (mean duration 8–11 years) and either known CVD or multiple cardiovascular risk factors. Details of these three studies are reviewed extensively in an ADA position statement (84).
The ACCORD study enrolled participants with either known CVD or two or more major CV risk factors and randomized them to intensive glycemic control (goal A1C <6%) or standard glycemic control (goal A1C 7–8%). The glycemic control arm of ACCORD was halted early due to the finding of an increased rate of mortality in the intensive arm compared with the standard arm (1.41 vs. 1.14% per year; HR 1.22, 95% CI 1.01–1.46), with a similar increase in cardiovascular deaths. This increase in mortality in the intensive glycemic control arm was seen in all prespecified patient subgroups. The primary outcome of ACCORD (MI, stroke, or cardiovascular death) was nonsignificantly lower in the intensive glycemic control group, due to a reduction in nonfatal MI, both when the glycemic control intervention was halted (81) and at completion of the planned follow-up (85).
Exploratory analyses of the mortality findings of ACCORD (evaluating variables including weight gain, use of any specific drug or drug combination, and hypoglycemia) were reportedly unable to identify a clear explanation for the excess mortality in the intensive arm (81). The ACCORD investigators subsequently published additional epidemiologic analyses showing no increase in mortality in either the intensive arm participants who achieved A1C levels <7% or those who lowered their A1C quickly after trial enrollment. In fact, although there was no A1C level at which intensive arm participants had significantly lower mortality than standard arm participants, the highest risk for mortality was observed in intensive arm participants with the highest A1C levels (86).
The role of hypoglycemia in the excess mortality findings was also complex. Severe hypoglycemia was significantly more likely in participants randomized to the intensive glycemic control arm. However, excess mortality in the intensive versus standard arms was only significant for participants with no severe hypoglycemia, and not for those with one or more episodes. Severe hypoglycemia was associated with excess mortality in either arm, but the association was stronger in those randomized to the standard glycemic control arm (87). Unlike the case with the DCCT, where lower achieved A1C levels were related to significantly increased rates of severe hypoglycemia, in ACCORD every 1% decline in A1C from baseline to 4 months into the trial was associated with a significant decrease in the rate of severe hypoglycemia in both arms (86).
The primary outcome of ADVANCE was a combination of microvascular events (nephropathy and retinopathy) and major adverse cardiovascular events (MI, stroke, and cardiovascular death). Intensive glycemic control (to a goal A1C <6.5% vs. treatment to local standards) significantly reduced the primary end point. However, this was due to a significant reduction in the microvascular outcome, primarily development of macroalbuminuria, with no significant reduction in the macrovascular outcome. There was no difference in overall or cardiovascular mortality between the intensive compared with the standard glycemic control arms (78).
VADT randomized participants with type 2 diabetes who were uncontrolled on insulin or maximal-dose oral agents (median entry A1C 9.4%) to a strategy of intensive glycemic control (goal A1C <6.0%) or standard glycemic control, with a planned A1C separation of at least 1.5%. The primary outcome of VADT was a composite of CVD events. The cumulative primary outcome was nonsignificantly lower in the intensive arm (76). An ancillary study of VADT demonstrated that intensive glycemic control was quite effective in reducing CVD events in individuals with less atherosclerosis at baseline (assessed by coronary calcium) but not in those with more extensive baseline atherosclerosis (88).
The evidence for a cardiovascular benefit of intensive glycemic control primarily rests on long-term follow-up of study cohorts treated early in the course of type 1 and type 2 diabetes and subset analyses of ACCORD, ADVANCE, and VADT. A recent group-level meta-analysis of the latter three trials suggests that glucose lowering has a modest (9%) but statistically significant reduction in major CVD outcomes, primarily nonfatal MI, with no significant effect on mortality. However, heterogeneity of the mortality effects across studies was noted, precluding firm summary measures of the mortality effects. A prespecified subgroup analysis suggested that major CVD outcome reduction occurred in patients without known CVD at baseline (HR 0.84, 95% CI 0.74–0.94) (89). Conversely, the mortality findings in ACCORD and subgroup analyses of VADT suggest that the potential risks of very intensive glycemic control may outweigh its benefits in some patients, such as those with very long duration of diabetes, known history of severe hypoglycemia, advanced atherosclerosis, and advanced age/ frailty. Certainly, providers should be vigilant in preventing severe hypoglycemia in patients with advanced disease and should not aggressively attempt to achieve near-normal A1C levels in patients in whom such a target cannot be reasonably easily and safely achieved. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals. Many factors, including patient preferences, should be taken into account when developing a patient's individualized goals (89a).
Recommended glycemic goals for many nonpregnant adults are shown in Table 9. The recommendations are based on those for A1C values, with listed blood glucose levels that appear to correlate with achievement of an A1C of <7%. The issue of pre- versus postprandial SMBG targets is complex (90). Elevated postchallenge (2-h OGTT) glucose values have been associated with increased cardiovascular risk independent of FPG in some epidemiological studies. In diabetic subjects, some surrogate measures of vascular pathology, such as endothelial dysfunction, are negatively affected by postprandial hyperglycemia (91). It is clear that postprandial hyperglycemia, like preprandial hyperglycemia, contributes to elevated A1C levels, with its relative contribution being higher at A1C levels that are closer to 7%. However, outcome studies have clearly shown A1C to be the primary predictor of complications, and landmark glycemic control trials such as the DCCT and UKPDS relied overwhelmingly on preprandial SMBG. Additionally, an RCT in patients with known CVD found no CVD benefit of insulin regimens targeting postprandial glucose compared with those targeting preprandial glucose (92). For individuals who have premeal glucose values within target but who have A1C values above target, monitoring postprandial plasma glucose (PPG) 1–2 h after the start of the meal and treatment aimed at reducing PPG values to <180 mg/dL may help lower A1C and is a reasonable recommendation for postprandial testing and targets. Glycemic goals for children are provided in section VII.A.1.a. Glycemic Control.
Table 9.
Summary of glycemic recommendations for many nonpregnant adults with diabetes
| A1C | <7.0%* |
| Preprandial capillary plasma glucose | 70–130 mg/dL* (3.9–7.2 mmol/L) |
Peak postprandial capillary plasma glucose†
|
<180 mg/dL* (<10.0 mmol/L) |
†Postprandial glucose measurements should be made 1–2 h after the beginning of the meal, generally peak levels in patients with diabetes.
As regards goals for glycemic control for women with GDM, recommendations from the Fifth International Workshop-Conference on Gestational Diabetes (93) are to target maternal capillary glucose concentrations of:
preprandial: ≤95 mg/dL (5.3 mmol/L), and either:
1-h postmeal: ≤140 mg/dL (7.8 mmol/L) or
2-h postmeal: ≤120 mg/dL (6.7 mmol/L)
For women with preexisting type 1 or type 2 diabetes who become pregnant, a recent consensus statement (94) recommended the following as optimal glycemic goals, if they can be achieved without excessive hypoglycemia:
premeal, bedtime, and overnight glucose 60–99 mg/dL (3.3–5.4 mmol/L)
peak postprandial glucose 100–129 mg/dL (5.4–7.1 mmol/L)
A1C <6.0%
D. Pharmacologic and overall approaches to treatment
1. Therapy for type 1 diabetes.
The DCCT clearly showed that intensive insulin therapy (three or more injections per day of insulin, continuous subcutaneous insulin infusion [CSII], or insulin pump therapy) was a key part of improved glycemia and better outcomes (61,82). At the time of the study, therapy was carried out with short- and intermediate-acting human insulins. Despite better microvascular outcomes, intensive insulin therapy was associated with a high rate in severe hypoglycemia (62 episodes per 100 patient-years of therapy). Since the time of the DCCT, a number of rapid-acting and long-acting insulin analogs have been developed. These analogs are associated with less hypoglycemia with equal A1C-lowering in type 1 diabetes (95,96).
Therefore, recommended therapy for type 1 diabetes consists of the following components: 1) use of multiple-dose insulin injections (three to four injections per day of basal and prandial insulin) or CSII therapy; 2) matching prandial insulin to carbohydrate intake, premeal blood glucose, and anticipated activity; and 3) for many patients (especially if hypoglycemia is a problem), use of insulin analogs. There are excellent reviews available that guide the initiation and management of insulin therapy to achieve desired glycemic goals (3,95,97).
Because of the increased frequency of other autoimmune diseases in type 1 diabetes, screening for thyroid dysfunction, vitamin B12 deficiency, or celiac disease should be considered based on signs and symptoms. Periodic screening in absence of symptoms has been recommended, but the effectiveness and optimal frequency are unclear.
2. Therapy for type 2 diabetes.
Recommendations.
At the time of type 2 diabetes diagnosis, initiate metformin therapy along with lifestyle interventions, unless metformin is contraindicated. (A)
In newly diagnosed type 2 diabetic patients with markedly symptomatic and/or elevated blood glucose levels or A1C, consider insulin therapy, with or without additional agents, from the outset. (E)
If noninsulin monotherapy at maximal tolerated dose does not achieve or maintain the A1C target over 3–6 months, add a second oral agent, a GLP-1 receptor agonist, or insulin. (E)
Prior expert consensus statements have suggested approaches to management of hyperglycemia in individuals with type 2 diabetes (98). Highlights include intervention at the time of diagnosis with metformin in combination with lifestyle changes (MNT and exercise) and continuing timely augmentation of therapy with additional agents (including early initiation of insulin therapy) as a means of achieving and maintaining recommended levels of glycemic control (i.e., A1C <7% for most patients). As A1C targets are not achieved, treatment intensification is based on the addition of another agent from a different class. Meta-analyses (98a) suggest that overall, each new class of noninsulin agents added to initial therapy lowers A1C around 0.9–1.1%. The overall objective is to safely achieve and maintain glycemic control and to change interventions when therapeutic goals are not being met.
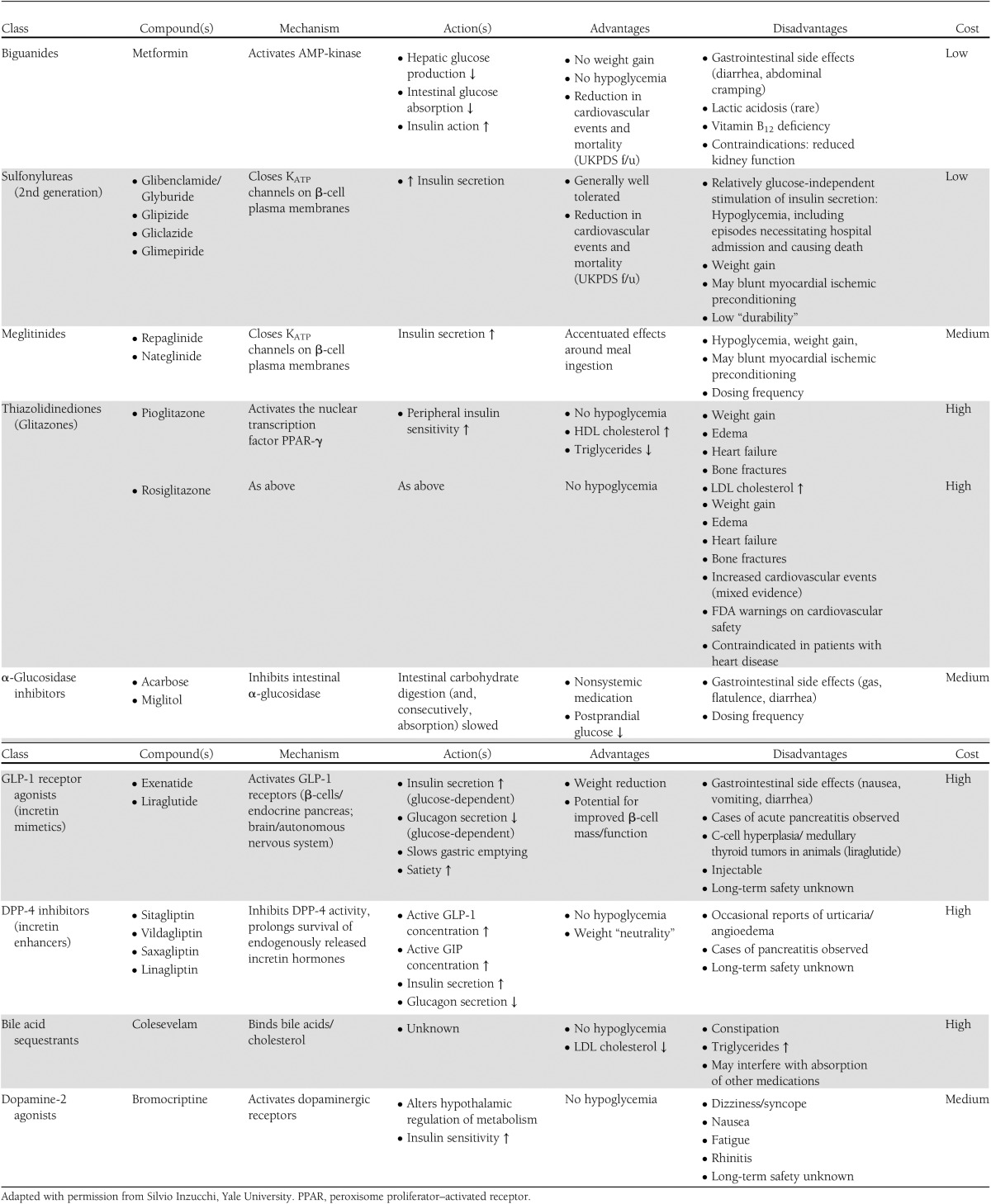
ADA and EASD have partnered on new guidance for individualization of use of medication classes and combinations in patients with type 2 diabetes. These guidelines, to be published in early 2012, will be less prescriptive than prior algorithms, and will discuss advantages and disadvantages of the available medication classes as well as considerations for their use. For information about currently approved classes of medications for treating hyperglycemia in type 2 diabetes, see Table 10.
Table 10.
Noninsulin therapies for hyperglycemia in type 2 diabetes: properties of selected glucose-lowering drugs that may guide individualization of therapy
E. Medical nutrition therapy (MNT)
General recommendations.
Individuals who have prediabetes or diabetes should receive individualized MNT as needed to achieve treatment goals, preferably provided by a registered dietitian familiar with the components of diabetes MNT. (A)
Because MNT can result in cost-savings and improved outcomes (B), MNT should be adequately covered by insurance and other payers. (E)
Energy balance, overweight, and obesity.
Weight loss is recommended for all overweight or obese individuals who have or are at risk for diabetes. (A)
For weight loss, either low-carbohydrate, low-fat calorie-restricted, or Mediterranean diets may be effective in the short-term (up to 2 years). (A)
For patients on low-carbohydrate diets, monitor lipid profiles, renal function, and protein intake (in those with nephropathy), and adjust hypoglycemic therapy as needed. (E)
Physical activity and behavior modification are important components of weight loss programs and are most helpful in maintenance of weight loss. (B)
Recommendations for primary prevention of diabetes.
Among individuals at high risk for developing type 2 diabetes, structured programs that emphasize lifestyle changes that include moderate weight loss (7% body weight) and regular physical activity (150 min/week), with dietary strategies including reduced calories and reduced intake of dietary fat, can reduce the risk for developing diabetes and are therefore recommended. (A)
Individuals at risk for type 2 diabetes should be encouraged to achieve the U.S. Department of Agriculture (USDA) recommendation for dietary fiber (14 g fiber/1,000 kcal) and foods containing whole grains (one-half of grain intake). (B)
Individuals at risk for type 2 diabetes should be encouraged to limit their intake of sugar-sweetened beverages. (B)
Recommendations for management of diabetes
Macronutrients in diabetes management.
The mix of carbohydrate, protein, and fat may be adjusted to meet the metabolic goals and individual preferences of the person with diabetes. (C)
Monitoring carbohydrate, whether by carbohydrate counting, choices, or experience-based estimation, remains a key strategy in achieving glycemic control. (B)
Saturated fat intake should be <7% of total calories. (B)
Reducing intake of trans fat lowers LDL cholesterol and increases HDL cholesterol (A), therefore intake of trans fat should be minimized. (E)
Other nutrition recommendations.
If adults with diabetes choose to use alcohol, they should limit intake to a moderate amount (one drink per day or less for adult women and two drinks per day or less for adult men) and should take extra precautions to prevent hypoglycemia. (E)
Routine supplementation with antioxidants, such as vitamins E and C and carotene, is not advised because of lack of evidence of efficacy and concern related to long-term safety. (A)
It is recommended that individualized meal planning include optimization of food choices to meet recommended daily allowance (RDA)/dietary reference intake (DRI) for all micronutrients. (E)
MNT is an integral component of diabetes prevention, management, and self-management education. In addition to its role in preventing and controlling diabetes, ADA recognizes the importance of nutrition as an essential component of an overall healthy lifestyle. A full review of the evidence regarding nutrition in preventing and controlling diabetes and its complications and additional nutrition-related recommendations can be found in the ADA position statement “Nutrition Recommendations and Interventions for Diabetes,” published in 2007 and updated in 2008 (100). Achieving nutrition-related goals requires a coordinated team effort that includes the active involvement of the person with prediabetes or diabetes. Because of the complexity of nutrition issues, it is recommended that a registered dietitian who is knowledgeable and skilled in implementing nutrition therapy into diabetes management and education be the team member who provides MNT.
Clinical trials/outcome studies of MNT have reported decreases in A1C at 3–6 months ranging from 0.25 to 2.9% with higher reductions seen in type 2 diabetes of shorter duration. Multiple studies have demonstrated sustained improvements in A1C at 12 months and longer when an registered dietitian provided follow-up visits ranging from monthly to three sessions per year (101–108). Studies in nondiabetic suggest that MNT reduces LDL cholesterol by 15–25 mg/dL up to 16% (109) and support a role for lifestyle modification in treating hypertension (109,110).
While the importance of weight loss for overweight and obese individuals is well documented, an optimal macronutrient distribution and dietary pattern of weight loss diets has not been established. A systematic review of 80 weight loss studies of ≥1 year duration demonstrated that moderate weight loss achieved through diet alone, diet and exercise, and meal replacements can be achieved and maintained (4.8–8% weight loss at 12 months) (111). Both low-fat low-carbohydrate and Mediterranean style eating patterns have been shown to promote weight loss with similar results after 1 to 2 years of follow-up (112–115). A meta-analysis showed that at 6 months, low-carbohydrate diets were associated with greater improvements in triglyceride and HDL cholesterol concentrations than low-fat diets; however, LDL cholesterol was significantly higher on the low-carbohydrate diets (116).
Because of the effects of obesity on insulin resistance, weight loss is an important therapeutic objective for overweight or obese individuals who are at risk for diabetes (117). The multifactorial intensive lifestyle intervention employed in the DPP, which included reduced intake of fat and calories, led to weight loss averaging 7% at 6 months and maintenance of 5% weight loss at 3 years, associated with a 58% reduction in incidence of type 2 diabetes (20). A RCT looking at high-risk individuals in Spain showed the Mediterranean dietary pattern reduced the incidence of diabetes in the absence of weight loss by 52% compared with the low-fat diet control group (118).
Although our society abounds with examples of high-calorie nutrient-poor foods, large increases in the consumption of sugar-sweetened beverages have coincided with the epidemics of obesity and type 2 diabetes. In a meta-analysis of eight prospective cohort studies (N = 310,819), a diet high in consumption of sugar-sweetened beverages was associated with the development of type 2 diabetes (n = 15,043). Individuals in the highest versus the lowest quantile of sugar-sweetened beverage intake had a 26% greater risk of developing diabetes (119).
For individuals with type 2 diabetes, studies have demonstrated that moderate weight loss (5% of body weight) is associated with decreased insulin resistance, improved measures of glycemia and lipemia, and reduced blood pressure (120); longer-term studies (≥52 weeks) showed mixed effects on A1C in adults with type 2 diabetes (121–123), and in some studies results were confounded by pharmacologic weight loss therapy. Look AHEAD (Action for Health in Diabetes) is a large clinical trial designed to determine whether long-term weight loss will improve glycemia and prevent cardiovascular events in subjects with type 2 diabetes. One-year results of the intensive lifestyle intervention in this trial show an average 8.6% weight loss, significant reduction of A1C, and reduction in several CVD risk factors (124), with benefits sustained at 4 years (125). When completed, the Look AHEAD trial should provide insight into the effects of long-term weight loss on important clinical outcomes.
Although numerous studies have attempted to identify the optimal mix of macronutrients for meal plans of people with diabetes, it is unlikely that one such combination of macronutrients exists. The best mix of carbohydrate, protein, and fat appears to vary depending on individual circumstances. It must be clearly recognized that regardless of the macronutrient mix, total caloric intake must be appropriate to weight management goal. Further, individualization of the macronutrient composition will depend on the metabolic status of the patient (e.g., lipid profile, renal function) and/or food preferences. A variety of dietary meal patterns are likely effective in managing diabetes including Mediterranean-style, plant-based (vegan or vegetarian), low-fat and lower-carbohydrate eating patterns (113,126–128).
It should be noted that the RDA for digestible carbohydrate is 130 g/day and is based on providing adequate glucose as the required fuel for the central nervous system without reliance on glucose production from ingested protein or fat. Although brain fuel needs can be met on lower-carbohydrate diets, long-term metabolic effects of very-low-carbohydrate diets are unclear, and such diets eliminate many foods that are important sources of energy, fiber, vitamins, and minerals and that are important in dietary palatability (129).
Saturated and trans fatty acids are the principal dietary determinants of plasma LDL cholesterol. There is a lack of evidence on the effects of specific fatty acids on people with diabetes; the recommended goals are therefore consistent with those for individuals with CVD (109,130).
Reimbursement for MNT
MNT, when delivered by a registered dietitian according to nutrition practice guidelines, is reimbursed as part of the Medicare program as overseen by the Centers for Medicare and Medicaid Services (CMS) (www.cms.gov).
F. Diabetes self-management education (DSME)
Recommendations.
People with diabetes should receive DSME according to national standards and diabetes self-management support when their diabetes is diagnosed and as needed thereafter. (B)
Effective self-management and quality of life are the key outcomes of DSME and should be measured and monitored as part of care. (C)
DSME should address psychosocial issues, since emotional well-being is associated with positive diabetes outcomes. (C)
Because DSME can result in cost-savings and improved outcomes (B), DSME should be adequately reimbursed by third-party payers. (E)
DSME is an essential element of diabetes care (131–136), and national standards for DSME (137) are based on evidence for its benefits. Education helps people with diabetes initiate effective self-management and cope with diabetes when they are first diagnosed. Ongoing DSME and diabetes self-management support (DSMS) also help people with diabetes maintain effective self-management throughout a lifetime of diabetes as they face new challenges and as treatment advances become available. DSME helps patients optimize metabolic control, prevent and manage complications, and maximize quality of life in a cost-effective manner (138).
DSME and DSMS are the on-going processes of facilitating the knowledge, skill, and ability necessary for diabetes self-care. This process incorporates the needs, goals, and life experiences of the person with diabetes. The overall objectives of DSME and DSMS are to support informed decision-making, self-care behaviors, problem-solving, and active collaboration with the health care team to improve clinical outcomes, health status, and quality of life in a cost-effective manner (137).
Current best practice for DSME is a skills-based approach that focuses on helping those with diabetes make informed self-management choices. DSME has changed from a didactic approach focusing on providing information to more theoretically based empowerment models that focus on helping those with diabetes make informed self-management decisions. Care of diabetes has shifted to an approach that is more patient centered and places the person with diabetes and his or her family at the center of the care model working in collaboration with health care professionals. Patient-centered care is respectful of and responsive to individual patient preferences, needs, and values and ensures that patient's values guide all decision making (139).
Evidence for the benefits of DSME.
Multiple studies have found that DSME is associated with improved diabetes knowledge and self-care behavior (131), improved clinical outcomes such as lower A1C (132,133,135,136,140,141), lower self-reported weight (131), improved quality of life (134,141,142), healthy coping (143), and lower costs (144). Better outcomes were reported for DSME interventions that were longer and included follow-up support (DSMS) (131,145–149) (150), that were culturally (151,152) and age appropriate (153,154), that were tailored to individual needs and preferences, and that addressed psychosocial issues and incorporated behavioral strategies (131,135,155–157). Both individual and group approaches have been found effective (158–161). There is growing evidence for the role of community health workers and peer (162,163) and lay leaders (164) in delivering DSME and support in addition to the core team (165).
Diabetes education is associated with increased use of primary and preventive services and lower use of acute, inpatient hospital services (144). Patients who participate in diabetes education are more likely to follow best practice treatment recommendations, particularly among the Medicare population, and have lower Medicare and commercial claim costs (166,167).
National standards for DSME.
The national standards for DSME are designed to define quality DSME and to assist diabetes educators in a variety of settings to provide evidence-based education (137). The standards, currently being updated, are reviewed and updated every 5 years by a task force representing key organizations involved in the field of diabetes education and care.
Reimbursement for DSME.
DSME, when provided by a program that meets national standards for DSME and is recognized by ADA or other approval bodies, is reimbursed as part of the Medicare program as overseen by the Centers for Medicare and Medicaid Services (CMS) (www.cms.gov). DSME is also covered by most health insurance plans.
G. Physical activity
Recommendations.
People with diabetes should be advised to perform at least 150 min/week of moderate-intensity aerobic physical activity (50–70% of maximum heart rate), spread over at least 3 days per week with no more than 2 consecutive days without exercise. (A)
In the absence of contraindications, people with type 2 diabetes should be encouraged to perform resistance training at least twice per week. (A)
Exercise is an important part of the diabetes management plan. Regular exercise has been shown to improve blood glucose control, reduce cardiovascular risk factors, contribute to weight loss, and improve well-being. Furthermore, regular exercise may prevent type 2 diabetes in high-risk individuals (20–22). Structured exercise interventions of at least 8-week duration have been shown to lower A1C by an average of 0.66% in people with type 2 diabetes, even with no significant change in BMI (168). Higher levels of exercise intensity are associated with greater improvements in A1C and in fitness (169). A joint position statement by ADA and the American College of Sports Medicine summarizes the evidence for benefits of exercise in people with type 2 diabetes (170).
Frequency and type of exercise.
The U.S. Department of Health and Human Services’ “Physical Activity Guidelines for Americans” (171) suggests that adults over age 18 years perform 150 min per week of moderate-intensity or 75 min per week of vigorous aerobic physical activity or an equivalent combination of the two. In addition, the guidelines suggest that adults also perform muscle-strengthening activities that involve all major muscle groups 2 or more days per week. The guidelines suggest that adults over age 65 years, or those with disabilities, follow the adult guidelines if possible or (if this is not possible) be as physically active as they are able. Studies included in a meta-analysis of the effects of exercise interventions on glycemic control (168) had a mean number of sessions per week of 3.4, with a mean duration of 49 min per session. The DPP lifestyle intervention, which included 150 min per week of moderate-intensity exercise, had a beneficial effect on glycemia in those with prediabetes. Therefore, it seems reasonable to recommend that people with diabetes try to follow the physical activity guidelines for the general population.
Progressive resistance exercise improves insulin sensitivity in older men with type 2 diabetes to the same or even a greater extent as aerobic exercise (172). Clinical trials have provided strong evidence for the A1C lowering value of resistance training in older adults with type 2 diabetes (173,174), and for an additive benefit of combined aerobic and resistance exercise in adults with type 2 diabetes (175,176). In the absence of contraindications, patients with type 2 diabetes should be encouraged to do at least two weekly sessions of resistance exercise (exercise with free weights or weight machines), with each session consisting of at least one set of five or more different resistance exercises involving the large muscle groups (170).
Evaluation of the diabetic patient before recommending an exercise program.
Prior guidelines suggested that before recommending a program of physical activity, the provider should assess patients with multiple cardiovascular risk factors for coronary artery disease (CAD). As discussed more fully in section VI.A.5. CHD Screening and Treatment, the area of screening asymptomatic diabetic patients for CAD remains unclear, and a recent ADA consensus statement on this issue concluded that routine screening is not recommended (177). Providers should use clinical judgment in this area. Certainly, high-risk patients should be encouraged to start with short periods of low-intensity exercise and increase the intensity and duration slowly.
Providers should assess patients for conditions that might contraindicate certain types of exercise or predispose to injury, such as uncontrolled hypertension, severe autonomic neuropathy, severe peripheral neuropathy or history of foot lesions, and unstable proliferative retinopathy. The patient's age and previous physical activity level should be considered.
Exercise in the presence of nonoptimal glycemic control hyperglycemia.
When people with type 1 diabetes are deprived of insulin for 12–48 h and are ketotic, exercise can worsen hyperglycemia and ketosis (178); therefore, vigorous activity should be avoided in the presence of ketosis. However, it is not necessary to postpone exercise based simply on hyperglycemia, provided the patient feels well and urine and/or blood ketones are negative.
Hypoglycemia.
In individuals taking insulin and/or insulin secretagogues, physical activity can cause hypoglycemia if medication dose or carbohydrate consumption is not altered. For individuals on these therapies, added carbohydrate should be ingested if preexercise glucose levels are <100 mg/dL (5.6 mmol/L). Hypoglycemia is rare in diabetic individuals who are not treated with insulin or insulin secretagogues, and no preventive measures for hypoglycemia are usually advised in these cases.
Exercise in the presence of specific long-term complications of diabetes retinopathy.
In the presence of proliferative diabetic retinopathy (PDR) or severe nonproliferative diabetic retinopathy (NPDR), vigorous aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment (179).
Peripheral neuropathy.
Decreased pain sensation in the extremities results in increased risk of skin breakdown and infection and of Charcot joint destruction. Prior recommendations have advised non–weight-bearing exercise for patients with severe peripheral neuropathy. However, studies have shown that moderate-intensity walking may not lead to increased risk of foot ulcers or reulceration in those with peripheral neuropathy (180). All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early. Anyone with a foot injury or open sore should be restricted to non–weight-bearing activities.
Autonomic neuropathy.
Autonomic neuropathy can increase the risk of exercise-induced injury or adverse event through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and unpredictable carbohydrate delivery from gastroparesis predisposing to hypoglycemia (181). Autonomic neuropathy is also strongly associated with CVD in people with diabetes (182,183). People with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity that is more intense than that to which they are accustomed.
Albuminuria and nephropathy.
Physical activity can acutely increase urinary protein excretion. However, there is no evidence that vigorous exercise increases the rate of progression of diabetic kidney disease, and there is likely no need for any specific exercise restrictions for people with diabetic kidney disease (184).
H. Psychosocial assessment and care
Recommendations.
It is reasonable to include assessment of the patient's psychological and social situation as an ongoing part of the medical management of diabetes. (E)
Psychosocial screening and follow-up may include, but is not limited to, attitudes about the illness, expectations for medical management and outcomes, affect/mood, general and diabetes-related quality of life, resources (financial, social, and emotional), and psychiatric history. (E)
Consider screening for psychosocial problems such as depression and diabetes-related distress, anxiety, eating disorders, and cognitive impairment when self-management is poor. (C)
Psychological and social problems can impair the individual's (185–188) or family's ability to carry out diabetes care tasks and therefore compromise health status. There are opportunities for the clinician to assess psychosocial status in a timely and efficient manner so that referral for appropriate services can be accomplished. A systematic review and meta-analysis showed that psychosocial interventions modestly but significantly improved A1C (standardized mean difference −0.29%) and mental health outcomes. However, a limited association between the effects on A1C and mental health, and no intervention characteristics predicted benefit on both outcomes, was shown (189).
Key opportunities for screening of psychosocial status occur at diagnosis, during regularly scheduled management visits, during hospitalizations, at discovery of complications, or when problems with glucose control, quality of life, or adherence are identified. Patients are likely to exhibit psychological vulnerability at diagnosis and when their medical status changes, e.g., the end of the honeymoon period, when the need for intensified treatment is evident, and when complications are discovered (187).
Issues known to impact self-management and health outcomes include but are not limited to attitudes about the illness, expectations for medical management and outcomes, affect/mood, general and diabetes-related quality of life, diabetes-related distress (190,191), resources (financial, social, and emotional) (192), and psychiatric history (193–195). Screening tools are available for a number of these areas (156). Indications for referral to a mental health specialist familiar with diabetes management may include gross noncompliance with medical regimen (by self or others) (195), depression with the possibility of self-harm, debilitating anxiety (alone or with depression), indications of an eating disorder (196), or cognitive functioning that significantly impairs judgment. It is preferable to incorporate psychological assessment and treatment into routine care rather than waiting for identification of a specific problem or deterioration in psychological status (156). Although the clinician may not feel qualified to treat psychological problems, utilizing the patient-provider relationship as a foundation for further treatment can increase the likelihood that the patient will accept referral for other services. It is important to establish that emotional well-being is part of diabetes management.
I. When treatment goals are not met
For a variety of reasons, some people with diabetes and their health care providers do not achieve the desired goals of treatment (Table 9). Rethinking the treatment regimen may require assessment of barriers including income, health literacy, diabetes distress, depression, and competing demands, including those related to family responsibilities and dynamics. Other strategies may include culturally appropriate and enhanced DSME, co-management with a diabetes team, referral to a medical social worker for assistance with insurance coverage, or change in pharmacological therapy. Initiation of or increase in SMBG, utilization of continuous glucose monitoring, frequent contact with the patient, or referral to a mental health professional or physician with special expertise in diabetes may be useful. Providing patients with an algorithm for self-titration of insulin doses based on SMBG results may be helpful for type 2 patients who take insulin (197).
J. Intercurrent illness
The stress of illness, trauma, and/or surgery frequently aggravates glycemic control and may precipitate diabetic ketoacidosis (DKA) or nonketotic hyperosmolar state—life-threatening conditions that require immediate medical care to prevent complications and death. Any condition leading to deterioration in glycemic control necessitates more frequent monitoring of blood glucose and (in ketosis-prone patients) urine or blood ketones. Marked hyperglycemia requires temporary adjustment of the treatment program and, if accompanied by ketosis, vomiting, or alteration in level of consciousness, immediate interaction with the diabetes care team. The patient treated with noninsulin therapies or MNT alone may temporarily require insulin. Adequate fluid and caloric intake must be assured. Infection or dehydration are more likely to necessitate hospitalization of the person with diabetes than the person without diabetes.
The hospitalized patient should be treated by a physician with expertise in the management of diabetes. For further information on management of patients with hyperglycemia in the hospital, see section IX.A. Diabetes Care in the Hospital. For further information on management of DKA or nonketotic hyperosmolar state, refer to the ADA consensus statement on hyperglycemic crises (198).
K. Hypoglycemia
Recommendations.
Glucose (15–20 g) is the preferred treatment for the conscious individual with hypoglycemia, although any form of carbohydrate that contains glucose may be used. If SMBG 15 min after treatment shows continued hypoglycemia, the treatment should be repeated. Once SMBG glucose returns to normal, the individual should consume a meal or snack to prevent recurrence of hypoglycemia. (E)
Glucagon should be prescribed for all individuals at significant risk of severe hypoglycemia, and caregivers or family members of these individuals instructed in its administration. Glucagon administration is not limited to health care professionals. (E)
Individuals with hypoglycemia unawareness or one or more episodes of severe hypoglycemia should be advised to raise their glycemic targets to strictly avoid further hypoglycemia for at least several weeks, to partially reverse hypoglycemia unawareness and reduce risk of future episodes. (B)
Hypoglycemia is the leading limiting factor in the glycemic management of type 1 and insulin-treated type 2 diabetes (199). Mild hypoglycemia may be inconvenient or frightening to patients with diabetes, and more severe hypoglycemia can cause acute harm to the person with diabetes or others, if it causes falls, motor vehicle accidents, or other injury. A large cohort study suggested that among older adults with type 2 diabetes, a history of severe hypoglycemia was associated with greater risk of dementia (200). Conversely, evidence from the DCCT/EDIC study, which involved younger type 1 patients, suggested no association of frequency of severe hypoglycemia with cognitive decline (201). Treatment of hypoglycemia (plasma glucose <70 mg/dL) requires ingestion of glucose- or carbohydrate-containing foods. The acute glycemic response correlates better with the glucose content than with the carbohydrate content of the food. Although pure glucose is the preferred treatment, any form of carbohydrate that contains glucose will raise blood glucose. Added fat may retard and then prolong the acute glycemic response. Ongoing activity of insulin or insulin secretagogues may lead to recurrence of hypoglycemia unless further food is ingested after recovery.
Severe hypoglycemia (where the individual requires the assistance of another person and cannot be treated with oral carbohydrate due to confusion or unconsciousness) should be treated using emergency glucagon kits, which require a prescription. Those in close contact with, or having custodial care of, people with hypoglycemia-prone diabetes (family members, roommates, school personnel, child care providers, correctional institution staff, or coworkers), should be instructed in use of such kits. An individual does not need to be a health care professional to safely administer glucagon. Care should be taken to ensure that unexpired glucagon kits are available.
Prevention of hypoglycemia is a critical component of diabetes management. Patients should understand situations that increase their risk of hypoglycemia, such as when fasting for tests or procedures, during or after intense exercise, and during sleep; and that increase the risk of harm to self or others from hypoglycemia, such as with driving. Teaching people with diabetes to balance insulin use, carbohydrate intake, and exercise is a necessary but not always sufficient strategy for prevention. In type 1 diabetes and severely insulin-deficient type 2 diabetes, the syndrome of hypoglycemia unawareness, or hypoglycemia-associated autonomic failure, can severely compromise stringent diabetes control and quality of life. The deficient counter-regulatory hormone release and autonomic responses in this syndrome are both risk factors for, and caused by, hypoglycemia. A corollary to this “vicious cycle” is that several weeks of avoidance of hypoglycemia has been demonstrated to improve counterregulation and awareness to some extent in many patients (202). Hence, patients with one or more episodes of severe hypoglycemia may benefit from at least short-term relaxation of glycemic targets.
L. Bariatric surgery
Recommendations.
Bariatric surgery may be considered for adults with BMI >35 kg/m2 and type 2 diabetes, especially if the diabetes or associated comorbidities are difficult to control with lifestyle and pharmacologic therapy. (B)
Patients with type 2 diabetes who have undergone bariatric surgery need life-long lifestyle support and medical monitoring. (B)
Although small trials have shown glycemic benefit of bariatric surgery in patients with type 2 diabetes and BMI of 30–35 kg/m2, there is currently insufficient evidence to generally recommend surgery in patients with BMI <35 kg/m2 outside of a research protocol. (E)
The long-term benefits, cost-effectiveness, and risks of bariatric surgery in individuals with type 2 diabetes should be studied in well-designed controlled trials with optimal medical and lifestyle therapy as the comparator. (E)
Gastric reduction surgery, either gastric banding or procedures that involve bypassing, transposing, or resecting sections of the small intestine, when part of a comprehensive team approach, can be an effective weight loss treatment for severe obesity, and national guidelines support its consideration for people with type 2 diabetes who have BMI >35 kg/m2. Bariatric surgery has been shown to lead to near- or complete normalization of glycemia in ∼55–95% of patients with type 2 diabetes, depending on the surgical procedure. A meta-analysis of studies of bariatric surgery involving 3,188 patients with diabetes reported that 78% had remission of diabetes (normalization of blood glucose levels in the absence of medications), and that the remission rates were sustained in studies that had follow-up exceeding 2 years (203). Remission rates tend to be lower with procedures that only constrict the stomach and higher with those that bypass portions of the small intestine. Additionally, there is a suggestion that intestinal bypass procedures may have glycemic effects that are independent of their effects on weight, perhaps involving the incretin axis.
One RCT compared adjustable gastric banding to “best available” medical and lifestyle therapy in subjects with type 2 diabetes diagnosed less than 2 years before randomization and with BMI 30–40 kg/m2 (204). In this trial, 73% of surgically treated patients achieved “remission” of their diabetes, compared with 13% of those treated medically. The latter group lost only 1.7% of body weight, suggesting that their therapy was not optimal. Overall the trial had 60 subjects, and only 13 had a BMI <35 kg/m2, making it difficult to generalize these results widely to diabetic patients who are less severely obese or with longer duration of diabetes. In a more recent study involving 110 patients with type 2 diabetes and a mean BMI of 47 kg/m2, Roux-en-Y gastric bypass resulted in a mean loss of excess weight of 63% at 1 year and 84% at 2 years (205).
Bariatric surgery is costly in the short term and has some risks. Rates of morbidity and mortality directly related to the surgery have been reduced considerably in recent years, with 30-day mortality rates now 0.28%, similar to those of laparoscopic cholecystectomy (206). Longer-term concerns include vitamin and mineral deficiencies, osteoporosis, and rare but often severe hypoglycemia from insulin hypersecretion. Cohort studies attempting to match subjects suggest that the procedure may reduce longer-term mortality rates (207). Recent retrospective analyses and modeling studies suggest that these procedures may be cost-effective, when one considers reduction in subsequent health care costs (208–210).
Some caution about the benefits of bariatric surgery might come from recent studies. A propensity score–adjusted analyses of older severely obese patients with high baseline mortality in Veterans Affairs Medical Centers found that the use of bariatric surgery was not associated with decreased mortality compared with usual care during a mean 6.7 years of follow-up (211). A study that followed patients who had undergone laparoscopic adjustable gastric banding (LAGB) for 12 years found that 60% were satisfied with the procedure. Nearly one of three patients experienced band erosion, and almost half had required removal of their bands. The authors’ conclusion was that, “LAGB appears to result in relatively poor long-term outcomes” (212). Studies of the mechanisms of glycemic improvement and long-term benefits and risks of bariatric surgery in individuals with type 2 diabetes, especially those who are not severely obese, will require well-designed clinical trials, with optimal medical and lifestyle therapy of diabetes and cardiovascular risk factors as the comparator.
M. Immunization
Recommendations.
Annually provide an influenza vaccine to all diabetic patients ≥6 months of age. (C)
Administer pneumococcal polysaccharide vaccine to all diabetic patients ≥2 years of age. A one-time revaccination is recommended for individuals >64 years of age previously immunized when they were <65 years of age if the vaccine was administered >5 years ago. Other indications for repeat vaccination include nephrotic syndrome, chronic renal disease, and other immunocompromised states, such as after transplantation. (C)
Administer hepatitis B vaccination to adults with diabetes as per Centers for Disease Control and Prevention (CDC) recommendations. (C)
Influenza and pneumonia are common, preventable infectious diseases associated with high mortality and morbidity in the elderly and in people with chronic diseases. Though there are limited studies reporting the morbidity and mortality of influenza and pneumococcal pneumonia specifically in people with diabetes, observational studies of patients with a variety of chronic illnesses, including diabetes, show that these conditions are associated with an increase in hospitalizations for influenza and its complications. People with diabetes may be at increased risk of the bacteremic form of pneumococcal infection and have been reported to have a high risk of nosocomial bacteremia, which has a mortality rate as high as 50% (213).
Safe and effective vaccines are available that can greatly reduce the risk of serious complications from these diseases (214,215). In a case-control series, influenza vaccine was shown to reduce diabetes-related hospital admission by as much as 79% during flu epidemics (214). There is sufficient evidence to support that people with diabetes have appropriate serologic and clinical responses to these vaccinations. The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices recommends influenza and pneumococcal vaccines for all individuals with diabetes (http://www.cdc.gov/vaccines/recs/).
At the time these standards went to press, the CDC was considering recommendations to immunize all or some adults with diabetes for hepatitis B. ADA awaits the final recommendations and will support them when they are released in 2012.
VI. PREVENTION AND MANAGEMENT OF DIABETES COMPLICATIONS
A. CVD
CVD is the major cause of morbidity and mortality for individuals with diabetes and the largest contributor to the direct and indirect costs of diabetes. The common conditions coexisting with type 2 diabetes (e.g., hypertension and dyslipidemia) are clear risk factors for CVD, and diabetes itself confers independent risk. Numerous studies have shown the efficacy of controlling individual cardiovascular risk factors in preventing or slowing CVD in people with diabetes. Large benefits are seen when multiple risk factors are addressed globally (216,217). There is evidence that measures of 10-year coronary heart disease (CHD) risk among U.S. adults with diabetes have improved significantly over the past decade (218).
1. Hypertension/blood pressure control.
Recommendations.
Screening and diagnosis
Blood pressure should be measured at every routine diabetes visit. Patients found to have systolic blood pressure (SBP) ≥ 130mmHg or diastolic blood pressure (DBP) ≥80 mmHg should have blood pressure confirmed on a separate day. Repeat SBP ≥130 mmHg or DBP ≥80 mmHg confirms a diagnosis of hypertension. (C)
Goals
A goal SBP <130 mmHg is appropriate for most patients with diabetes. (C)
Based on patient characteristics and response to therapy, higher or lower SBP targets may be appropriate. (B)
Patients with diabetes should be treated to a DBP <80 mmHg. (B)
Treatment
Patients with a SBP of 130–139 mmHg or a DBP of 80–89 mmHg may be given lifestyle therapy alone for a maximum of 3 months and then, if targets are not achieved, be treated with addition of pharmacological agents. (E)
Patients with more severe hypertension (SBP ≥140 or DBP ≥90 mmHg) at diagnosis or follow-up should receive pharmacologic therapy in addition to lifestyle therapy. (A)
Lifestyle therapy for hypertension consists of weight loss, if overweight; Dietary Approaches to Stop Hypertension (DASH)-style dietary pattern, including reducing sodium and increasing potassium intake; moderation of alcohol intake; and increased physical activity. (B)
Pharmacologic therapy for patients with diabetes and hypertension should be with a regimen that includes either an ACE inhibitor or an ARB. If one class is not tolerated, the other should be substituted. (C)
Multiple drug therapy (two or more agents at maximal doses) is generally required to achieve blood pressure targets. (B)
Administer one or more antihypertensive medications at bedtime. (A)
If ACE inhibitors, ARBs, or diuretics are used, kidney function and serum potassium levels should be monitored. (E)
In pregnant patients with diabetes and chronic hypertension, blood pressure target goals of 110–129/65–79 mmHg are suggested in the interest of long-term maternal health and minimizing impaired fetal growth. ACE inhibitors and ARBs are contraindicated during pregnancy. (E)
Hypertension is a common comorbidity of diabetes, affecting the majority of patients, with prevalence depending on type of diabetes, age, obesity, and ethnicity. Hypertension is a major risk factor for both CVD and microvascular complications. In type 1 diabetes, hypertension is often the result of underlying nephropathy, while in type 2 diabetes it usually coexists with other cardiometabolic risk factors.
Screening and diagnosis.
Measurement of blood pressure in the office should be done by a trained individual and follow the guidelines established for nondiabetic individuals: measurement in the seated position, with feet on the floor and arm supported at heart level, after 5 min of rest. Cuff size should be appropriate for the upper arm circumference. Elevated values should be confirmed on a separate day. Because of the clear synergistic risks of hypertension and diabetes, the diagnostic cutoff for a diagnosis of hypertension is lower in people with diabetes (blood pressure ≥130/80 mmHg) than those without diabetes (blood pressure ≥140/90 mmHg) (219).
Home blood pressure self-monitoring and 24-h ambulatory blood pressure monitoring may provide additional evidence of “white coat” and masked hypertension and other discrepancies between office and “true” blood pressure, and studies in nondiabetic populations found that home measurements may better correlate with CVD risk than office measurements (220,221). However, the preponderance of the clear evidence of benefits of treatment of hypertension in people with diabetes is based on office measurements.
Treatment goals.
Epidemiologic analyses show that blood pressure >115/75 mmHg is associated with increased cardiovascular event rates and mortality in individuals with diabetes (219,222,223). Randomized clinical trials have demonstrated the benefit (reduction of CHD events, stroke, and nephropathy) of lowering blood pressure to <140 mmHg systolic and <80 mmHg diastolic in individuals with diabetes (219,224–226). The ACCORD trial examined whether blood pressure lowering to systolic blood pressure (SBP) <120 mmHg provides greater cardiovascular protection than an SBP of 130–140 mmHg in patients with type 2 diabetes at high risk for CVD (227). The blood pressure achieved in the intensive group was 119/64 mmHg and in the standard group was 133/70 mmHg; the difference achieved was attained with an average of 3.4 medications per participant in the intensive group and 2.1 in the standard therapy group. The primary outcome was a composite of nonfatal MI, nonfatal stroke, and CVD death; the hazard ratio for the primary end point in the intensive group was 0.88 (95% CI 0.73–1.06; P = 0.20). Of the prespecified secondary end points, only stroke and nonfatal stroke were statistically significantly reduced by intensive blood pressure treatment, with hazard ratios of 0.59 (95% CI 0.39–0.89, P = 0.01) and 0.63 (95% CI 0.41–0.96, P = 0.03), respectively. If this finding is real, the number needed to treat to prevent one stroke over the course of 5 years with intensive blood pressure management is 89.
In predefined subgroup analyses, there was a suggestion of heterogeneity (P = 0.08) based on whether participants were randomized to standard or intensive glycemia intervention. In those randomized to standard glycemic control, the event rate for the primary end point was 1.89 per year in the intensive blood pressure arm and 2.47 in the standard blood pressure arm, while the respective rates in the intensive glycemia arm were 1.85 and 1.73. If this observation is true, it suggests that intensive management to a SBP target of <120 mmHg may be of benefit in those who are not targeting an A1C of <6% and/or that the benefit of intensive blood pressure management is diminished by more intensive glycemia management targeting an A1C of <6%.
Other recent randomized trial data include those of the ADVANCE trial in which treatment with an ACE inhibitor and a thiazide-type diuretic reduced the rate of death but not the composite macrovascular outcome. However, the ADVANCE trial had no specified targets for the randomized comparison, and the mean SBP in the intensive group (135 mmHg) was not as low as the mean SBP in the ACCORD standard-therapy group (228). A post hoc analysis of blood pressure control in 6,400 patients with diabetes and CAD enrolled in the International Verapamil/Trandolapril Study (INVEST) demonstrated that “tight control” (<130 mmHg) was not associated with improved cardiovascular outcomes compared with “usual care” (130–140 mmHg) (229).
It is possible that lowering SBP from the low-130s to <120 mmHg does not further reduce coronary events or death, and that most of the benefit from lowering blood pressure is achieved by targeting a goal <140 mmHg. However, this has not been formally assessed. Only the ACCORD blood pressure trial has formally examined treatment targets significantly <130 mmHg in diabetes. The absence of significant harms, the trends toward benefit in stroke, and the potential heterogeneity with respect to intensive glycemia management suggests that previously recommended targets are reasonable pending further analyses and results. SBP targets more or less stringent than <130 mmHg may be appropriate for individual patients, based on response to therapy, medication tolerance, and individual characteristics, keeping in mind that most analyses have suggested that outcomes are worse if the SBP is >140 mmHg.
Treatment strategies.
Although there are no well-controlled studies of diet and exercise in the treatment of hypertension in individuals with diabetes, the Dietary Approaches to Stop Hypertension (DASH) study in nondiabetic individuals has shown antihypertensive effects similar to pharmacologic monotherapy. Lifestyle therapy consists of reducing sodium intake (to <1,500 mg per day) and excess body weight; increasing consumption of fruits, vegetables (8–10 servings per day), and low-fat dairy products (2–3 servings per day); avoiding excessive alcohol consumption (no more than two servings per day in men and no more than one serving per day in women) (230); and increasing activity levels (219). These nonpharmacological strategies may also positively affect glycemia and lipid control. Their effects on cardiovascular events have not been established. An initial trial of nonpharmacologic therapy may be reasonable in diabetic individuals with mild hypertension (SBP 130–139 mmHg or DBP 80–89 mmHg). If the blood pressure is ≥140 mmHg systolic and/or ≥90 mmHg diastolic at the time of diagnosis, pharmacologic therapy should be initiated along with nonpharmacologic therapy (219).
Lowering of blood pressure with regimens based on a variety of antihypertensive drugs, including ACE inhibitors, ARBs, β-blockers, diuretics, and calcium channel blockers, has been shown to be effective in reducing cardiovascular events. Several studies suggested that ACE inhibitors may be superior to dihydropyridine calcium channel blockers in reducing cardiovascular events (231–233). However, a variety of other studies have shown no specific advantage to ACE inhibitors as initial treatment of hypertension in the general hypertensive population, but rather an advantage on cardiovascular outcomes of initial therapy with low-dose thiazide diuretics (219,234,235).
In people with diabetes, inhibitors of the renin-angiotensin system (RAS) may have unique advantages for initial or early therapy of hypertension. In a nonhypertension trial of high-risk individuals, including a large subset with diabetes, an ACE inhibitor reduced CVD outcomes (236). In patients with congestive heart failure (CHF), including diabetic subgroups, ARBs have been shown to reduce major CVD outcomes (237–240), and in type 2 patients with significant nephropathy, ARBs were superior to calcium channel blockers for reducing heart failure (241). Though evidence for distinct advantages of RAS inhibitors on CVD outcomes in diabetes remains conflicting (224,235), the high CVD risks associated with diabetes, and the high prevalence of undiagnosed CVD, may still favor recommendations for their use as first-line hypertension therapy in people with diabetes (219).
Recently, the blood pressure arm of the ADVANCE trial demonstrated that routine administration of a fixed combination of the ACE inhibitor perindopril and the diuretic indapamide significantly reduced combined microvascular and macrovascular outcomes, as well as CVD and total mortality. The improved outcomes could also have been due to lower achieved blood pressure in the perindopril-indapamide arm (228). In addition the ACCOMPLISH trial showed a decrease in morbidity and mortality in those receiving benazapril and amlodipine versus benazapril and hydrochlorothiazide. The compelling benefits of RAS inhibitors in diabetic patients with albuminuria or renal insufficiency provide additional rationale for use of these agents (see section VI.B. Nephropathy Screening and Treatment). If needed to achieve blood pressure targets, amlodipine, HCTZ, or chlorthalidone can be added. If estimated glomerular filtration rate (GFR) is <30 ml/min/m2, a loop diuretic, rather than HCTZ or chlorthatlidone should be prescribed. Titration of and/or addition of further blood pressure medications should be made in timely fashion to overcome clinical inertia in achieving blood pressure targets.
Evidence is emerging that health information technology can be used safely and effectively as a tool to enable attainment of blood pressure goals. Using a telemonitoring intervention to direct titrations of antihypertensive medications between medical office visits has been demonstrated to have a profound impact on SBP control (242).
An important caveat is that most patients with hypertension require multidrug therapy to reach treatment goals, especially diabetic patients whose targets are lower (219). If blood pressure is refractory to optimal doses of at least 3 antihypertensive agents of different classifications, one of which should be a diuretic, clinicians should consider an evaluation for secondary forms of hypertension. Growing evidence suggests that there is an association between increase in sleep-time blood pressure and incidence of CVD events. A recent RCT of 448 participants with type 2 diabetes and hypertension demonstrated reduced cardiovascular events and mortality with median follow-up of 5.4 years if at least one antihypertensive medication was given at bedtime (243).
During pregnancy in diabetic women with chronic hypertension, target blood pressure goals of SBP 110–129 mmHg and DBP 65–79 mmHg are reasonable, as they contribute to long-term maternal health. Lower blood pressure levels may be associated with impaired fetal growth. During pregnancy, treatment with ACE inhibitors and ARBs is contraindicated, since they can cause fetal damage. Antihypertensive drugs known to be effective and safe in pregnancy include methyldopa, labetalol, diltiazem, clonidine, and prazosin. Chronic diuretic use during pregnancy has been associated with restricted maternal plasma volume, which might reduce uteroplacental perfusion (244).
2. Dyslipidemia/lipid management.
Recommendations
Screening
In most adult patients, measure fasting lipid profile at least annually. In adults with low-risk lipid values (LDL cholesterol <100 mg/dL, HDL cholesterol >50 mg/dL, and triglycerides <150 mg/dL), lipid assessments may be repeated every 2 years. (E)
Treatment recommendations and goals
Lifestyle modification focusing on the reduction of saturated fat, trans fat, and cholesterol intake; increase of n-3 fatty acids, viscous fiber and plant stanols/sterols; weight loss (if indicated); and increased physical activity should be recommended to improve the lipid profile in patients with diabetes. (A)
- Statin therapy should be added to lifestyle therapy, regardless of baseline lipid levels, for diabetic patients:
- ○ with overt CVD. (A)
- ○ without CVD who are over the age of 40 years and who have one or more other CVD risk factors. (A)
For patients at lower risk than those above (e.g., those without overt CVD and under the age of 40 years), statin therapy should be considered in addition to lifestyle therapy if LDL cholesterol remains >100 mg/dL or in those with multiple CVD risk factors. (E)
In individuals without overt CVD, the primary goal is an LDL cholesterol <100 mg/dL (2.6 mmol/L). (A)
In individuals with overt CVD, a lower LDL cholesterol goal of <70 mg/dL (1.8 mmol/L), using a high dose of a statin, is an option. (B)
If drug-treated patients do not reach the above targets on maximal tolerated statin therapy, a reduction in LDL cholesterol of ∼30–40% from baseline is an alternative therapeutic goal. (A)
Triglycerides levels <150 mg/dL (1.7 mmol/L) and HDL cholesterol >40 mg/dL (1.0 mmol/L) in men and >50 mg/dL (1.3 mmol/L) in women, are desirable. However, LDL cholesterol–targeted statin therapy remains the preferred strategy. (C)
If targets are not reached on maximally tolerated doses of statins, combination therapy using statins and other lipid-lowering agents may be considered to achieve lipid targets but has not been evaluated in outcome studies for either CVD outcomes or safety. (E)
Statin therapy is contraindicated in pregnancy. (B)
Evidence for benefits of lipid-lowering therapy.
Patients with type 2 diabetes have an increased prevalence of lipid abnormalities, contributing to their high risk of CVD. For the past decade or more, multiple clinical trials demonstrated significant effects of pharmacologic (primarily statin) therapy on CVD outcomes in subjects with CHD and for primary CVD prevention (245). Subanalyses of diabetic subgroups of larger trials (246–250) and trials specifically in subjects with diabetes (251,252) showed significant primary and secondary prevention of CVD events +/− CHD deaths in diabetic populations. Similar to findings in nondiabetic subjects, reduction in “hard” CVD outcomes (CHD death and nonfatal MI) can be more clearly seen in diabetic subjects with high baseline CVD risk (known CVD and/or very high LDL cholesterol levels), but overall the benefits of statin therapy in people with diabetes at moderate or high risk for CVD are convincing.
Low levels of HDL cholesterol, often associated with elevated triglyceride levels, are the most prevalent pattern of dyslipidemia in persons with type 2 diabetes. However, the evidence base for drugs that target these lipid fractions is significantly less robust than that for statin therapy (253). Nicotinic acid has been shown to reduce CVD outcomes (254), although the study was done in a nondiabetic cohort. Gemfibrozil has been shown to decrease rates of CVD events in subjects without diabetes (255,256) and in the diabetic subgroup of one of the larger trials (255). However, in a large trial specific to diabetic patients, fenofibrate failed to reduce overall cardiovascular outcomes (257).
Dyslipidemia treatment and target lipid levels.
For most patients with diabetes, the first priority of dyslipidemia therapy (unless severe hypertriglyceridemia is the immediate issue) is to lower LDL cholesterol to a target goal of <100 mg/dL (2.60 mmol/L) (258). Lifestyle intervention, including MNT, increased physical activity, weight loss, and smoking cessation, may allow some patients to reach lipid goals. Nutrition intervention should be tailored according to each patient's age, type of diabetes, pharmacological treatment, lipid levels, and other medical conditions and should focus on the reduction of saturated fat, cholesterol, and trans unsaturated fat intake and increases in n-3 fatty acids, viscous fiber (such as in oats, legumes, citrus), and plant stanols/sterols. Glycemic control can also beneficially modify plasma lipid levels, particularly in patients with very high triglycerides and poor glycemic control.
In those with clinical CVD or who are over 40 years of age with other CVD risk factors, pharmacological treatment should be added to lifestyle therapy regardless of baseline lipid levels. Statins are the drugs of choice for lowering LDL cholesterol.
In patients other than those described above, statin treatment should be considered if there is an inadequate LDL cholesterol response to lifestyle modifications and improved glucose control, or if the patient has increased cardiovascular risk (e.g., multiple cardiovascular risk factors or long duration of diabetes). Very little clinical trial evidence exists for type 2 patients under the age of 40 years or for type 1 patients of any age. In the Heart Protection Study (lower age limit: 40 years), the subgroup of ∼600 patients with type 1 diabetes had a reduction in risk proportionately similar to that of patients with type 2 diabetes, although not statistically significant (247). Although the data are not definitive, consideration should be given to lipid-lowering goals in type 1 diabetic patients similar to those in type 2 diabetic patients, particularly if they have other cardiovascular risk factors.
Alternative LDL cholesterol goals.
Virtually all trials of statins and CVD outcomes tested specific doses of statins against placebo, other doses of statin, or other statins, rather than aiming for specific LDL cholesterol goals (259). Placebo-controlled trials generally achieved LDL cholesterol reductions of 30–40% from baseline. Hence, LDL cholesterol lowering of this magnitude is an acceptable outcome for patients who cannot reach LDL cholesterol goals due to severe baseline elevations in LDL cholesterol and/or intolerance of maximal, or any, statin doses. Additionally for those with baseline LDL cholesterol minimally >100 mg/dL, prescribing statin therapy to lower LDL cholesterol ∼30–40% from baseline is probably more effective than prescribing just enough to get LDL cholesterol slightly <100 mg/dL.
Recent clinical trials in high-risk patients, such as those with acute coronary syndromes or previous cardiovascular events (260–262), have demonstrated that more aggressive therapy with high doses of statins to achieve an LDL cholesterol of <70 mg/dL led to a significant reduction in further events. Therefore, a reduction in LDL cholesterol to a goal of <70 mg/dL is an option in very-high-risk diabetic patients with overt CVD (263).
In individual patients, LDL cholesterol lowering with statins is highly variable and this variable response is poorly understood (264). Reduction of CVD events with statins correlates very closely with LDL cholesterol lowering (245). When maximally tolerated doses of statins fail to significantly lower LDL cholesterol (<30% reduction from patients baseline), the primary aim of combination therapy should be to achieve additional LDL cholesterol lowering. Niacin, fenofibrate, ezetimibe, and bile acid sequestrants all offer additional LDL cholesterol lowering. The evidence that combination therapy for LDL cholesterol lowering provides a significant increment in CVD risk reduction over statin therapy alone is still elusive. Some experts recommend a greater focus on non–HDL cholesterol and apolipoprotein B (apoB) in patients who are likely to have small LDL particles, such as people with diabetes (265).
Treatment of other lipoprotein fractions or targets.
Severe hypertriglyceridemia may warrant immediate therapy of this abnormality with lifestyle and usually pharmacologic therapy (fibric acid derivative, niacin, or fish oil) to reduce the risk of acute pancreatitis. In the absence of severe hypertriglyceridemia, therapy targeting HDL cholesterol or triglycerides has intuitive appeal but lacks the evidence base of statin therapy. If the HDL cholesterol is <40 mg/dL and the LDL cholesterol 100–129 mg/dL, gemfibrozil or niacin might be used, especially if a patient is intolerant to statins. Niacin is the most effective drug for raising HDL cholesterol. It can significantly increase blood glucose at high doses, but recent studies demonstrate that at modest doses (750–2,000 mg/day), significant improvements in LDL cholesterol, HDL cholesterol, and triglyceride levels are accompanied by only modest changes in glucose that are generally amenable to adjustment of diabetes therapy (266,267).
Combination therapy.
Combination therapy, with a statin and a fibrate or statin and niacin, may be efficacious for treatment for all three lipid fractions, but this combination is associated with an increased risk for abnormal transaminase levels, myositis, or rhabdomyolysis. The risk of rhabdomyolysis is higher with higher doses of statins and with renal insufficiency and seems to be lower when statins are combined with fenofibrate than gemfibrozil (268). In the recent ACCORD study, the combination of fenofibrate and simvastatin did not reduce the rate of fatal cardiovascular events, nonfatal MI, or nonfatal stroke, as compared with simvastatin alone, in patients with type 2 diabetes who were at high risk for CVD. However, prespecified subgroup analyses suggested heterogeneity in treatment effects according to sex, with a benefit of combination therapy for men and possible harm for women, and a possible benefit for patients with both triglyceride level ≥204 mg/dL and HDL cholesterol level ≤34 mg/dL (269). The AIM-HIGH trial randomized over 3,000 patients (about one-third with diabetes) to statin therapy plus or minus addition of extended release niacin. The trial was halted early due to no difference in the primary CVD outcome and a possible increase in ischemic stroke in those on combination therapy (270). Table 11 summarizes common treatment goals for A1C, blood pressure, and LDL cholesterol.
Table 11.
Summary of recommendations for glycemic, blood pressure, and lipid control for most adults with diabetes
| A1C | <7.0%* |
| Blood pressure | <130/80 mmHg† |
| Lipids | |
| LDL cholesterol | <100 mg/dL (<2.6 mmol/L)‡ |
*More or less stringent glycemic goals may be appropriate for individual patients. Goals should be individualized based on duration of diabetes, age/life expectancy, comorbid conditions, known CVD or advanced microvascular complications, hypoglycemia unawareness, individual and patient considerations.
†Based on patient characteristics and response to therapy, higher or lower SBP targets may be appropriate.
‡In individuals with overt CVD, a lower LDL cholesterol goal of <70 mg/dL (1.8 mmol/L), using a high dose of a statin, is an option.
3. Antiplatelet agents.
Recommendations
Consider aspirin therapy (75–162 mg/day) as a primary prevention strategy in those with type 1 or type 2 diabetes at increased cardiovascular risk (10-year risk >10%). This includes most men >50 years of age or women >60 years of age who have at least one additional major risk factor (family history of CVD, hypertension, smoking, dyslipidemia, or albuminuria). (C)
Aspirin should not be recommended for CVD prevention for adults with diabetes at low CVD risk (10-year CVD risk <5%, such as in men <50 years and women <60 years with no major additional CVD risk factors), since the potential adverse effects from bleeding likely offset the potential benefits. (C)
In patients in these age-groups with multiple other risk factors (e.g., 10-year risk 5–10%), clinical judgment is required. (E)
Use aspirin therapy (75–162 mg/day) as a secondary prevention strategy in those with diabetes with a history of CVD. (A)
For patients with CVD and documented aspirin allergy, clopidogrel (75 mg/day) should be used. (B)
Combination therapy with ASA (75–162 mg/day) and clopidogrel (75 mg/day) is reasonable for up to a year after an acute coronary syndrome. (B)
Aspirin has been shown to be effective in reducing cardiovascular morbidity and mortality in high-risk patients with previous MI or stroke (secondary prevention). Its net benefit in primary prevention among patients with no previous cardiovascular events is more controversial, both for patients with and without a history of diabetes (271). Two recent RCTs of aspirin specifically in patients with diabetes failed to show a significant reduction in CVD end points, raising further questions about the efficacy of aspirin for primary prevention in people with diabetes (272,273).
The Antithrombotic Trialist (ATT) collaborators recently published an individual patient-level meta-analysis of the six large trials of aspirin for primary prevention in the general population. These trials collectively enrolled over 95,000 participants, including almost 4,000 with diabetes. Overall, they found that aspirin reduced the risk of vascular events by 12% (relative risk [RR] 0.88, 95% CI 0.82–0.94). The largest reduction was for nonfatal MI with little effect on CHD death (RR 0.95, 95% CI 0.78–1.15) or total stroke. There was some evidence of a difference in aspirin effect by gender. Aspirin significantly reduced CHD events in men but not in women. Conversely, aspirin had no effect on stroke in men but significantly reduced stroke in women. Notably, differences between sexes in aspirin's effects have not been observed in studies of secondary prevention (271). In the six trials examined by the ATT collaborators, the effects of aspirin on major vascular events were similar for patients with or without diabetes (RR 0.88, 95% CI 0.67–1.15, and 0.87, 0.79–0.96), respectively. The confidence interval was wider for those with diabetes because of their smaller number.
Based on the currently available evidence, aspirin appears to have a modest effect on ischemic vascular events, with the absolute decrease in events depending on the underlying CVD risk. The main adverse effects appear to be an increased risk of gastrointestinal bleeding. The excess risk may be as high as 1–5 per 1,000 per year in real-world settings. In adults with CVD risk >1% per year, the number of CVD events prevented will be similar to or greater than the number of episodes of bleeding induced, although these complications do not have equal effects on long-term health (274).
In 2010, a position statement of the ADA, AHA, and the American College of Cardiology Foundation (ACCF) updated prior joint recommendations for primary prevention (275). Low-dose (75–162 mg/day) aspirin use for primary prevention is reasonable for adults with diabetes and no previous history of vascular disease who are at increased CVD risk (10-year risk of CVD events >10%) and who are not at increased risk for bleeding. This generally includes most men over age 50 years and women over age 60 years who also have one or more of the following major risk factors: smoking, hypertension, dyslipidemia,) family history of premature CVD, or albuminuria.
However, aspirin is no longer recommended for those at low CVD risk (women under age 60 years and men under age 50 years with no major CVD risk factors; 10-year CVD risk <5%), as the low benefit is likely to be outweighed by the risks of significant bleeding. Clinical judgment should be used for those at intermediate risk (younger patients with one or risk factors, or older patients with no risk factors; those with 10-year CVD risk of 5–10%) until further research is available. Use of aspirin in patients under the age of 21 years is contraindicated due to the associated risk of Reye's syndrome.
Average daily dosages used in most clinical trials involving patients with diabetes ranged from 50 to 650 mg but were mostly in the range of 100 to 325 mg/day. There is little evidence to support any specific dose, but using the lowest possible dosage may help reduce side-effects (276). Although platelets from patients with diabetes have altered function, it is unclear what, if any, impact that finding has on the required dose of aspirin for cardioprotective effects in the patient with diabetes. There are many alternate pathways for platelet activation that are independent of thromboxane A2 and thus not sensitive to the effects of aspirin (277). Therefore, while “aspirin resistance” appears higher in the diabetic patients when measured by a variety of ex vivo and in vitro methods (platelet aggrenometry, measurement of thromboxane B2), these observations alone are insufficient to empirically recommend higher doses of aspirin be used in the diabetic patient at this time.
Clopidogrel has been demonstrated to reduce CVD events in diabetic individuals (278). It is recommended as adjunctive therapy in the first year after an acute coronary syndrome or as alternative therapy in aspirin-intolerant patients.
4. Smoking cessation.
Recommendations
Advise all patients not to smoke. (A)
Include smoking cessation counseling and other forms of treatment as a routine component of diabetes care. (B)
A large body of evidence from epidemiological, case-control, and cohort studies provides convincing documentation of the causal link between cigarette smoking and health risks. Much of the work documenting the impact of smoking on health does not separately discuss results on subsets of individuals with diabetes, but suggests that the identified risks are at least equivalent to those found in the general population. Other studies of individuals with diabetes consistently demonstrate that smokers have a heightened risk of CVD and premature death and increased rate of microvascular complications of diabetes. Smoking may have a role in the development of type 2 diabetes.
The routine and thorough assessment of tobacco use is important as a means of preventing smoking or encouraging cessation. A number of large randomized clinical trials have demonstrated the efficacy and cost-effectiveness of brief counseling in smoking cessation, including the use of quit lines, in the reduction of tobacco use. For the patient motivated to quit, the addition of pharmacological therapy to counseling is more effective than either treatment alone. Special considerations should include assessment of the level of nicotine dependence, which is associated with difficulty in quitting and relapse (279).
5. CHD screening and treatment.
Recommendations
Screening
In asymptomatic patients, routine screening for CAD is not recommended, as it does not improve outcomes as long as CVD risk factors are treated. (A)
Treatment
In patients with known CVD, consider ACE inhibitor therapy (C) and use aspirin and statin therapy (A) (if not contraindicated) to reduce the risk of cardiovascular events. In patients with a prior MI, β-blockers should be continued for at least 2 years after the event. (B)
Longer-term use of β-blockers in the absence of hypertension is reasonable if well tolerated, but data are lacking. (E)
Avoid TZD treatment in patients with symptomatic heart failure. (C)
Metformin may be used in patients with stable CHF if renal function is normal. It should be avoided in unstable or hospitalized patients with CHF. (C)
Screening for CAD is reviewed in a recently updated consensus statement (177). To identify the presence of CAD in diabetic patients without clear or suggestive symptoms, a risk factor–based approach to the initial diagnostic evaluation and subsequent follow-up has intuitive appeal. However, recent studies concluded that using this approach fails to identify which patients with type 2 diabetes will have silent ischemia on screening tests (182,280).
Candidates for cardiac testing include those with 1) typical or atypical cardiac symptoms and 2) an abnormal resting ECG. The screening of asymptomatic patients remains controversial. Intensive medical therapy, which would be indicated anyway for diabetic patients at high risk for CVD, seems to provide equal outcomes to invasive revascularization, which raises questions of how screening results would change management. (281,282). There is also some evidence that silent myocardial ischemia may reverse over time, adding to the controversy concerning aggressive screening strategies (283). Finally, a recent randomized observational trial demonstrated no clinical benefit to routine screening of asymptomatic patients with type 2 diabetes and normal ECGs (284). Despite abnormal myocardial perfusion imaging in more than one in five patients, cardiac outcomes were essentially equal (and very low) in screened versus unscreened patients. Accordingly, the overall effectiveness, especially the cost-effectiveness, of such an indiscriminate screening strategy is now questioned.
Newer noninvasive CAD screening methods, such as computed tomography (CT) and CT angiography have gained in popularity. These tests infer the presence of coronary atherosclerosis by measuring the amount of calcium in coronary arteries and, in some circumstances, by direct visualization of luminal stenoses. Although asymptomatic diabetic patients found to have a higher coronary disease burden have more future cardiac events (285–287), the role of these tests beyond risk stratification is not clear. Their routine use leads to radiation exposure and may result in unnecessary invasive testing such as coronary angiography and revascularization procedures. The ultimate balance of benefit, cost, and risks of such an approach in asymptomatic patients remains controversial, particularly in the modern setting of aggressive CVD risk factor control.
In all patients with diabetes, cardiovascular risk factors should be assessed at least annually. These risk factors include dyslipidemia, hypertension, smoking, a positive family history of premature coronary disease, and the presence of micro- or macroalbuminuria. Abnormal risk factors should be treated as described elsewhere in these guidelines. Patients at increased CHD risk should receive aspirin and a statin, and ACE inhibitor or ARB therapy if hypertensive, unless there are contraindications to a particular drug class. While clear benefit exists for ACE inhibitor and ARB therapy in patients with nephropathy or hypertension, the benefits in patients with CVD in the absence of these conditions is less clear, especially when LDL cholesterol is concomitantly controlled (288,289).
B. Nephropathy screening and treatment
Recommendations
General recommendations
To reduce the risk or slow the progression of nephropathy, optimize glucose control. (A)
To reduce the risk or slow the progression of nephropathy, optimize blood pressure control. (A)
Screening
Perform an annual test to assess urine albumin excretion in type 1 diabetic patients with diabetes duration of ≥5 years and in all type 2 diabetic patients starting at diagnosis. (B)
Measure serum creatinine at least annually in all adults with diabetes regardless of the degree of urine albumin excretion. The serum creatinine should be used to estimate GFR and stage the level of chronic kidney disease (CKD), if present. (E)
Treatment
In the treatment of the nonpregnant patient with micro- or macroalbuminuria, either ACE inhibitors or ARBs should be used. (A)
If one class is not tolerated, the other should be substituted. (E)
Reduction of protein intake to 0.8–1.0 g · kg body wt−1 · day−1 in individuals with diabetes and the earlier stages of CKD and to 0.8 g · kg body wt−1 · day−1 in the later stages of CKD may improve measures of renal function (urine albumin excretion rate, GFR) and is recommended. (B)
When ACE inhibitors, ARBs, or diuretics are used, monitor serum creatinine and potassium levels for the development of increased creatinine and hyperkalemia. (E)
Continued monitoring of urine albumin excretion to assess both response to therapy and progression of disease is reasonable. (E)
When estimated GFR is <60 ml · min/1.73 m2, evaluate and manage potential complications of CKD. (E)
Consider referral to a physician experienced in the care of kidney disease for uncertainty about the etiology of kidney disease, difficult management issues, or advanced kidney disease. (B)
Diabetic nephropathy occurs in 20–40% of patients with diabetes and is the single leading cause of end-stage renal disease (ESRD). Persistent albuminuria in the range of 30–299 mg/24 h (microalbuminuria) has been shown to be the earliest stage of diabetic nephropathy in type 1 diabetes and a marker for development of nephropathy in type 2 diabetes. Microalbuminuria is also a well-established marker of increased CVD risk (290,291). Patients with microalbuminuria who progress to macroalbuminuria (≥300 mg/24 h) are likely to progress to ESRD (292,293). However, a number of interventions have been demonstrated to reduce the risk and slow the progression of renal disease.
Intensive diabetes management with the goal of achieving near-normoglycemia has been shown in large prospective randomized studies to delay the onset of microalbuminuria and the progression of micro- to macroalbuminuria in patients with type 1 (294,295) and type 2 (73,74,78,79) diabetes. The UKPDS provided strong evidence that control of blood pressure can reduce the development of nephropathy (224). In addition, large prospective randomized studies in patients with type 1 diabetes have demonstrated that achievement of lower levels of SBP (<140 mmHg) resulting from treatment using ACE inhibitors provides a selective benefit over other antihypertensive drug classes in delaying the progression from micro- to macroalbuminuria and can slow the decline in GFR in patients with macroalbuminuria (296–298). In type 2 diabetes with hypertension and normoalbuminuria, RAS inhibition has been demonstrated to delay onset of microalbuminuria in two studies (299,300). In the latter study, there was an unexpected higher rate of fatal cardiovascular events with olmesartan among patients with preexisting CHD.
ACE inhibitors have been shown to reduce major CVD outcomes (i.e., MI, stroke, death) in patients with diabetes (236), thus further supporting the use of these agents in patients with microalbuminuria, a CVD risk factor. ARBs do not prevent microalbuminuria in normotensive patients with type 1 or type 2 diabetes (301,302); however, ARBs have been shown to reduce the rate of progression from micro- to macroalbuminuria as well as ESRD in patients with type 2 diabetes (303–305). Some evidence suggests that ARBs have a smaller magnitude of rise in potassium compared with ACE inhibitors in people with nephropathy (306,307). Combinations of drugs that block the rennin-angiotensin-aldosterone system (e.g., an ACE inhibitor plus an ARB, a mineralocorticoid antagonist, or a direct renin inhibitor) have been shown to provide additional lowering of albuminuria (308–311). However, the long-term effects of such combinations on renal or cardiovascular outcomes have not yet been evaluated in clinical trials and they are associated with increased risk for hyperkalemia.
Other drugs, such as diuretics, calcium channel blockers, and β-blockers, should be used as additional therapy to further lower blood pressure in patients already treated with ACE inhibitors or ARBs (241), or as alternate therapy in the rare individual unable to tolerate ACE inhibitors or ARBs.
Studies in patients with varying stages of nephropathy have shown that protein restriction of dietary protein helps slow the progression of albuminuria, GFR decline, and occurrence of ESRD (312–315). Dietary protein restriction should be considered particularly in patients whose nephropathy seems to be progressing despite optimal glucose and blood pressure control and use of ACE inhibitor and/or ARBs (315).
Assessment of albuminuria status and renal function.
Screening for microalbuminuria can be performed by measurement of the albumin-to-creatinine ratio in a random spot collection; 24-h or timed collections are more burdensome and add little to prediction or accuracy (316,317). Measurement of a spot urine for albumin only, whether by immunoassay or by using a dipstick test specific for microalbumin, without simultaneously measuring urine creatinine, is somewhat less expensive but susceptible to false-negative and false-positive determinations as a result of variation in urine concentration due to hydration and other factors.
Abnormalities of albumin excretion are defined in Table 12. Because of variability in urinary albumin excretion (UAE), two of three specimens collected within a 3- to 6-month period should be abnormal before considering a patient to have crossed one of these diagnostic thresholds. Exercise within 24 h, infection, fever, CHF, marked hyperglycemia, and marked hypertension may elevate UAE over baseline values.
Table 12.
Definitions of abnormalities in albumin excretion
| Category | Spot collection (μg/mg creatinine) |
| Normal | <30 |
| Microalbuminuria | 30–299 |
| Macro (clinical)-albuminuria | ≥300 |
Information on presence of abnormal UAE in addition to level of GFR may be used to stage CKD. The National Kidney Foundation classification (Table 13) is primarily based on GFR levels and therefore differs from other systems in which staging is based primarily on UAE (318). Studies have found decreased GFR in the absence of increased UAE in a substantial percentage of adults with diabetes (319). Serum creatinine should therefore be measured at least annually in all adults with diabetes, regardless of the degree of UAE.
Table 13.
Stages of CKD
| Stage | Description | GFR (ml/min per 1.73 m2 body surface area) |
| 1 | Kidney damage* with normal or increased GFR | ≥90 |
| 2 | Kidney damage* with mildly decreased GFR | 60–89 |
| 3 | Moderately decreased GFR | 30–59 |
| 4 | Severely decreased GFR | 15–29 |
| 5 | Kidney failure | <15 or dialysis |
Kidney damage defined as abnormalities on pathologic, urine, blood, or imaging tests. Adapted from ref. 317.
Serum creatinine should be used to estimate GFR and to stage the level of CKD, if present. Estimated GFR (eGFR) is commonly co-reported by laboratories, or can be estimated using formulae such as the Modification of Diet in Renal Disease (MDRD) study equation (320). Recent reports have indicated that the MDRD is more accurate for the diagnosis and stratification of CKD in patients with diabetes than the Cockcroft-Gault equation (321). GFR calculators are available at http://www.nkdep.nih.gov.
The role of continued annual quantitative assessment of albumin excretion after diagnosis of microalbuminuria and institution of ACE inhibitor or ARB therapy and blood pressure control is unclear. Continued surveillance can assess both response to therapy and progression of disease. Some suggest that reducing abnormal albuminuria (>30 mg/g) to the normal or near-normal range may improve renal and cardiovascular prognosis, but this approach has not been formally evaluated in prospective trials.
Complications of kidney disease correlate with level of kidney function. When the eGFR is <60 mL/min/1.73 m2, screening for complications of CKD is indicated (Table 14). Early vaccination against hepatitis B is indicated in patients likely to progress to end-stage kidney disease.
Table 14.
Management of CKD in diabetes
| GFR | Recommended |
| All patients | Yearly measurement of creatinine, UAE, potassium |
| 45-60 | Referral to nephrology if possibility for nondiabetic kidney disease exists (duration type 1 diabetes <10 years, heavy proteinuria, abnormal findings on renal ultrasound, resistant hypertension, rapid fall in GFR, or active urinary sediment on ultrasound) |
| Consider need for dose adjustment of medications | |
| Monitor eGFR every 6 months | |
| Monitor electrolytes, bicarbonate, hemoglobin, calcium, phosphorus, parathyroid hormone at least yearly | |
| Assure vitamin D sufficiency | |
| Consider bone density testing | |
| Referral for dietary counseling | |
| 30–44 | Monitor eGFR every 3 months |
| Monitor electrolytes, bicarbonate, calcium, phosphorus, parathyroid hormone, hemoglobin, albumin, weight every 3–6 months | |
| Consider need for dose adjustment of medications | |
| <30 | Referral to nephrologists |
Adapted from National Kidney Foundation guidelines (available at http://www.kidney.org/professionals/KDOQI/guideline_diabetes/).
Consider referral to a physician experienced in the care of kidney disease when there is uncertainty about the etiology of kidney disease (heavy proteinuria, active urine sediment, absence of retinopathy, rapid decline in GFR, resistant hypertension). Other triggers for referral may include difficult management issues (anemia, secondary hyperparathyroidism, metabolic bone disease, or electrolyte disturbance), or advanced kidney disease. The threshold for referral may vary depending on the frequency with which a provider encounters diabetic patients with significant kidney disease. Consultation with a nephrologist when Stage 4 CKD develops has been found to reduce cost, improve quality of care, and keep people off dialysis longer (322). However, nonrenal specialists should not delay educating their patients about the progressive nature of diabetic kidney disease; the renal preservation benefits of aggressive treatment of blood pressure, blood glucose, and hyperlipidemia; and the potential need for renal replacement therapy.
C. Retinopathy screening and treatment
Recommendations
General recommendations
To reduce the risk or slow the progression of retinopathy, optimize glycemic control. (A)
To reduce the risk or slow the progression of retinopathy, optimize blood pressure control. (A)
Screening
Adults and children aged 10 years or older with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the onset of diabetes. (B)
Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist shortly after the diagnosis of diabetes. (B)
Subsequent examinations for type 1 and type 2 diabetic patients should be repeated annually by an ophthalmologist or optometrist. Less-frequent exams (every 2–3 years) may be considered following one or more normal eye exams. Examinations will be required more frequently if retinopathy is progressing. (B)
High-quality fundus photographs can detect most clinically significant diabetic retinopathy. Interpretation of the images should be performed by a trained eye care provider. While retinal photography may serve as a screening tool for retinopathy, it is not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional. (E)
Women with preexisting diabetes who are planning pregnancy or who have become pregnant should have a comprehensive eye examination and be counseled on the risk of development and/or progression of diabetic retinopathy. Eye examination should occur in the first trimester with close follow-up throughout pregnancy and for 1 year postpartum. (B)
Treatment
Promptly refer patients with any level of macular edema, severe NPDR, or any PDR to an ophthalmologist who is knowledgeable and experienced in the management and treatment of diabetic retinopathy. (A)
Laser photocoagulation therapy is indicated to reduce the risk of vision loss in patients with high-risk PDR, clinically significant macular edema, and in cases of severe NPDR. (A)
The presence of retinopathy is not a contraindication to aspirin therapy for cardioprotection, as this therapy does not increase the risk of retinal hemorrhage. (A)
Diabetic retinopathy is a highly specific vascular complication of both type 1 and type 2 diabetes, with prevalence strongly related to the duration of diabetes. Diabetic retinopathy is the most frequent cause of new cases of blindness among adults aged 20–74 years. Glaucoma, cataracts, and other disorders of the eye occur earlier and more frequently in people with diabetes.
In addition to duration of diabetes, other factors that increase the risk of, or are associated with, retinopathy include chronic hyperglycemia (323), nephropathy (324), and hypertension (325). Intensive diabetes management with the goal of achieving near normoglycemia has been shown in large prospective randomized studies to prevent and/or delay the onset and progression of diabetic retinopathy (61,73,74,80). Lowering blood pressure has been shown to decrease the progression of retinopathy (224), although tight targets (systolic <120 mmHg) do not impart additional benefit (80). Several case series and a controlled prospective study suggest that pregnancy in type 1 diabetic patients may aggravate retinopathy (326,327); laser photocoagulation surgery can minimize this risk (327).
One of the main motivations for screening for diabetic retinopathy is the established efficacy of laser photocoagulation surgery in preventing visual loss. Two large trials, the Diabetic Retinopathy Study (DRS) in patients with PDR and the Early Treatment Diabetic Retinopathy Study (ETDRS) in patients with macular edema, provide the strongest support for the therapeutic benefits of photocoagulation surgery. The DRS (328) showed that panretinal photocoagulation surgery reduced the risk of severe vision loss from PDR from 15.9% in untreated eyes to 6.4% in treated eyes, with greatest risk-to-benefit ratio in those with baseline disease (disc neovascularization or vitreous hemorrhage).
The ETDRS (329) established the benefit of focal laser photocoagulation surgery in eyes with macular edema, particularly those with clinically significant macular edema, with reduction of doubling of the visual angle (e.g., 20/50 to 20/100) from 20% in untreated eyes to 8% in treated eyes. The ETDRS also verified the benefits of panretinal photocoagulation for high-risk PDR, and in older-onset patients with severe NPDR or less-than-high-risk PDR.
Laser photocoagulation surgery in both trials was beneficial in reducing the risk of further visual loss, but generally not beneficial in reversing already diminished acuity. Recombinant monoclonal antibody to vascular endothelial growth factor is an emerging therapy that seems to halt progression of macular edema and may in fact improve vision in some patients (330).
The preventive effects of therapy and the fact that patients with PDR or macular edema may be asymptomatic provide strong support for a screening program to detect diabetic retinopathy. As retinopathy is estimated to take at least 5 years to develop after the onset of hyperglycemia, patients with type 1 diabetes should have an initial dilated and comprehensive eye examination within 5 years after the onset of diabetes. Patients with type 2 diabetes, who generally have had years of undiagnosed diabetes and who have a significant risk of prevalent diabetic retinopathy at the time of diabetes diagnosis, should have an initial dilated and comprehensive eye examination soon after diagnosis. Examinations should be performed by an ophthalmologist or optometrist who is knowledgeable and experienced in diagnosing the presence of diabetic retinopathy and is aware of its management. Subsequent examinations for type 1 and type 2 diabetic patients are generally repeated annually. Less-frequent exams (every 2–3 years) may be cost-effective after one or more normal eye exams, and in a population with well-controlled type 2 diabetes there was essentially no risk of development of significant retinopathy with a 3-year interval after a normal examination (331). Examinations will be required more frequently if retinopathy is progressing (332).
The use of retinal photography with remote reading by experts has great potential in areas where qualified eye care professionals are not available and may also enhance efficiency and reduce costs when the expertise of ophthalmologists can be utilized for more complex examinations and for therapy (333). In-person exams are still necessary when the photos are unacceptable and for follow-up of detected abnormalities. Photos are not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional. Results of eye examinations should be documented and transmitted to the referring health care professional.
D. Neuropathy screening and treatment
Recommendations
All patients should be screened for distal symmetric polyneuropathy (DPN) starting at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes and at least annually thereafter, using simple clinical tests. (B)
Electrophysiological testing is rarely needed, except in situations where the clinical features are atypical. (E)
Screening for signs and symptoms of cardiovascular autonomic neuropathy should be instituted at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes. Special testing is rarely needed and may not affect management or outcomes. (E)
Medications for the relief of specific symptoms related to painful DPN and autonomic neuropathy are recommended, as they improve the quality of life of the patient. (E)
The diabetic neuropathies are heterogeneous with diverse clinical manifestations. They may be focal or diffuse. Most common among the neuropathies are chronic sensorimotor DPN and autonomic neuropathy. Although DPN is a diagnosis of exclusion, complex investigations to exclude other conditions are rarely needed.
The early recognition and appropriate management of neuropathy in the patient with diabetes is important for a number of reasons: 1) nondiabetic neuropathies may be present in patients with diabetes and may be treatable; 2) a number of treatment options exist for symptomatic diabetic neuropathy; 3) up to 50% of DPN may be asymptomatic and patients are at risk for insensate injury to their feet; 4) autonomic neuropathy and particularly cardiovascular autonomic neuropathy is associated with substantial morbidity and even mortality. Specific treatment for the underlying nerve damage is currently not available, other than improved glycemic control, which may modestly slow progression (79) but not reverse neuronal loss. Effective symptomatic treatments are available for some manifestations of DPN (334) and autonomic neuropathy.
Diagnosis of neuropathy.
Distal symmetric polyneuropathy
Patients with diabetes should be screened annually for DPN using tests such as pinprick sensation, vibration perception (using a 128-Hz tuning fork), 10-g monofilament pressure sensation at the distal plantar aspect of both great toes and metatarsal joints, and assessment of ankle reflexes. Combinations of more than one test have >87% sensitivity in detecting DPN. Loss of 10-g monofilament perception and reduced vibration perception predict foot ulcers (335). Importantly, in patients with neuropathy, particularly when severe, causes other than diabetes should always be considered, such as neurotoxic mediations, heavy metal poisoning, alcohol abuse, vitamin B12 deficiency (especially in those taking metformin for prolonged periods (336), renal disease, chronic inflammatory demyelinating neuropathy, inherited neuropathies, and vasculitis (337).
Diabetic autonomic neuropathy (338)
The symptoms and signs of autonomic dysfunction should be elicited carefully during the history and physical examination. Major clinical manifestations of diabetic autonomic neuropathy include resting tachycardia, exercise intolerance, orthostatic hypotension, constipation, gastroparesis, erectile dysfunction, sudomotor dysfunction, impaired neurovascular function, and potentially autonomic failure in response to hypoglycemia.
Cardiovascular autonomic neuropathy (CAN), a CVD risk factor (93), is the most studied and clinically important form of diabetic autonomic neuropathy. CAN may be indicated by resting tachycardia (>100 bpm) or orthostasis (a fall in SBP >20 mmHg upon standing without an appropriate heart rate response); it is also associated with increased cardiac event rates. Although some societies have developed guidelines for screening for CAN, the benefits of sophisticated testing beyond risk stratification are not clear (339).
Gastrointestinal neuropathies (e.g., esophageal enteropathy, gastroparesis, constipation, diarrhea, fecal incontinence) are common, and any section of the gastrointestinal tract may be affected. Gastroparesis should be suspected in individuals with erratic glucose control or with upper gastrointestinal symptoms without other identified cause. Evaluation of solid-phase gastric emptying using double-isotope scintigraphy may be done if symptoms are suggestive, but test results often correlate poorly with symptoms. Constipation is the most common lower-gastrointestinal symptom but can alternate with episodes of diarrhea.
Diabetic autonomic neuropathy is also associated with genitourinary tract disturbances. In men, diabetic autonomic neuropathy may cause erectile dysfunction and/or retrograde ejaculation. Evaluation of bladder dysfunction should be performed for individuals with diabetes who have recurrent urinary tract infections, pyelonephritis, incontinence, or a palpable bladder.
Symptomatic treatments.
DPN
The first step in management of patients with DPN should be to aim for stable and optimal glycemic control. Although controlled trial evidence is lacking, several observational studies suggest that neuropathic symptoms improve not only with optimization of control, but also with the avoidance of extreme blood glucose fluctuations. Patients with painful DPN may benefit from pharmacological treatment of their symptoms; many agents have confirmed or probable efficacy confirmed in systematic reviews of RCTs (334), with several U.S. Food and Drug Administration (FDA)-approved for the management of painful DPN.
Autonomic neuropathy
Gastroparesis symptoms may improve with dietary changes and prokinetic agents such as metoclopramide or erythromycin. Treatments for erectile dysfunction may include phosphodiesterase type 5 inhibitors, intracorporeal or intraurethral prostaglandins, vacuum devices, or penile prostheses. Interventions for other manifestations of autonomic neuropathy are described in an ADA statement on neuropathy (335). As with DPN treatments, these interventions do not change the underlying pathology and natural history of the disease process, but may have a positive impact on the quality of life of the patient.
E. Foot care
Recommendations
For all patients with diabetes, perform an annual comprehensive foot examination to identify risk factors predictive of ulcers and amputations. The foot examination should include inspection, assessment of foot pulses, and testing for loss of protective sensation (10-g monofilament plus testing any one of the following: vibration using 128-Hz tuning fork, pinprick sensation, ankle reflexes, or vibration perception threshold). (B)
Provide general foot self-care education to all patients with diabetes. (B)
A multidisciplinary approach is recommended for individuals with foot ulcers and high-risk feet, especially those with a history of prior ulcer or amputation. (B)
Refer patients who smoke, have loss of protective sensation and structural abnormalities, or have history of prior lower-extremity complications to foot care specialists for ongoing preventive care and life-long surveillance. (C)
Initial screening for peripheral arterial disease (PAD) should include a history for claudication and an assessment of the pedal pulses. Consider obtaining an ankle-brachial index (ABI), as many patients with PAD are asymptomatic. (C)
Refer patients with significant claudication or a positive ABI for further vascular assessment and consider exercise, medications, and surgical options. (C)
Amputation and foot ulceration, consequences of diabetic neuropathy and/or PAD, are common and major causes of morbidity and disability in people with diabetes. Early recognition and management of risk factors can prevent or delay adverse outcomes.
The risk of ulcers or amputations is increased in people who have the following risk factors:
Previous amputation
Past foot ulcer history
Peripheral neuropathy
Foot deformity
Peripheral vascular disease
Visual impairment
Diabetic nephropathy (especially patients on dialysis)
Poor glycemic control
Cigarette smoking
Many studies have been published proposing a range of tests that might usefully identify patients at risk for foot ulceration, creating confusion among practitioners as to which screening tests should be adopted in clinical practice. An ADA task force was therefore assembled in 2008 to concisely summarize recent literature in this area and then recommend what should be included in the comprehensive foot exam for adult patients with diabetes. Their recommendations are summarized below, but clinicians should refer to the task force report (340) for further details and practical descriptions of how to perform components of the comprehensive foot examination.
At least annually, all adults with diabetes should undergo a comprehensive foot examination to identify high risk conditions. Clinicians should ask about history of previous foot ulceration or amputation, neuropathic or peripheral vascular symptoms, impaired vision, tobacco use, and foot care practices. A general inspection of skin integrity and musculoskeletal deformities should be done in a well-lit room. Vascular assessment would include inspection and assessment of pedal pulses.
The neurologic exam recommended is designed to identify loss of protective sensation (LOPS) rather than early neuropathy. The clinical examination to identify LOPS is simple and requires no expensive equipment. Five simple clinical tests (use of a 10-g monofilament, vibration testing using a 128-Hz tuning fork, tests of pinprick sensation, ankle reflex assessment, and testing vibration perception threshold with a biothesiometer), each with evidence from well-conducted prospective clinical cohort studies, are considered useful in the diagnosis of LOPS in the diabetic foot. The task force agrees that any of the five tests listed could be used by clinicians to identify LOPS, although ideally two of these should be regularly performed during the screening exam—normally the 10-g monofilament and one other test. One or more abnormal tests would suggest LOPS, while at least two normal tests (and no abnormal test) would rule out LOPS. The last test listed, vibration assessment using a biothesiometer or similar instrument, is widely used in the U.S.; however, identification of the patient with LOPS can easily be carried out without this or other expensive equipment.
Initial screening for PAD should include a history for claudication and an assessment of the pedal pulses. A diagnostic ABI should be performed in any patient with symptoms of PAD. Due to the high estimated prevalence of PAD in patients with diabetes and the fact that many patients with PAD are asymptomatic, an ADA consensus statement on PAD (341) suggested that a screening ABI be performed in patients over 50 years of age and be considered in patients under 50 years of age who have other PAD risk factors (e.g., smoking, hypertension, hyperlipidemia, or duration of diabetes >10 years). Refer patients with significant symptoms or a positive ABI for further vascular assessment and consider exercise, medications, and surgical options (341).
Patients with diabetes and high-risk foot conditions should be educated regarding their risk factors and appropriate management. Patients at risk should understand the implications of the loss of protective sensation, the importance of foot monitoring on a daily basis, the proper care of the foot, including nail and skin care, and the selection of appropriate footwear. Patients with loss of protective sensation should be educated on ways to substitute other sensory modalities (hand palpation, visual inspection) for surveillance of early foot problems. The patients’ understanding of these issues and their physical ability to conduct proper foot surveillance and care should be assessed. Patients with visual difficulties, physical constraints preventing movement, or cognitive problems that impair their ability to assess the condition of the foot and to institute appropriate responses will need other people, such as family members, to assist in their care.
People with neuropathy or evidence of increased plantar pressure (e.g., erythema, warmth, callus, or measured pressure) may be adequately managed with well-fitted walking shoes or athletic shoes that cushion the feet and redistribute pressure. Callus can be debrided with a scalpel by a foot care specialist or other health professional with experience and training in foot care. People with bony deformities (e.g., hammertoes, prominent metatarsal heads, bunions) may need extra-wide or -depth shoes. People with extreme bony deformities (e.g., Charcot foot) who cannot be accommodated with commercial therapeutic footwear may need custom-molded shoes.
Foot ulcers and wound care may require care by a podiatrist, orthopedic or vascular surgeon, or rehabilitation specialist experienced in the management of individuals with diabetes.
VII. ASSESSMENT OF COMMON COMORBID CONDITIONS
Recommendations
For patients with risk factors, signs or symptoms, consider assessment and treatment for common diabetes-associated conditions (see Table 15). (B)
Table 15.
Common comorbidities for which increased risk is associated with diabetes
| Hearing impairment |
| Obstructive sleep apnea |
| Fatty liver disease |
| Low testosterone in men |
| Periodontal disease |
| Certain cancers |
| Fractures |
| Cognitive impairment |
In addition to the commonly appreciated comorbidities of obesity, hypertension, and dyslipidemia, diabetes is also associated with other diseases or conditions at rates higher than those of age-matched people without diabetes. A few of the more common comorbidities are described herein, and listed in Table 15.
Hearing impairment
Hearing impairment, both high frequency and low/mid frequency, is more common in people with diabetes, perhaps due to neuropathy and/or vascular disease. In an NHANES analysis, hearing impairment was about twice as great in people with diabetes than in those without diabetes, after adjusting for age and other risk factors for hearing impairment (342). Controlling for age, race, and other demographic factors, high-frequency loss in those with diabetes was significantly associated with history of CHD and with peripheral neuropathy, while low/mid frequency loss was associated with low HDL cholesterol and with poor reported health status (343).
Obstructive sleep apnea
Age-adjusted rates of obstructive sleep apnea, a risk factor for CVD, are significantly higher (4- to 10-fold) with obesity, especially with central obesity, in men and women (344). The prevalence in general populations with type 2 diabetes may be up to 23% (345) and in obese participants enrolled in the Look AHEAD trial exceeded 80% (346). Treatment of sleep apnea significantly improves quality of life and blood pressure control. The evidence for a treatment effect on glycemic control is mixed (347).
Fatty liver disease
Unexplained elevation of hepatic transaminase concentrations are significantly associated with higher BMI, waist circumference, triglycerides, and fasting insulin and with lower HDL cholesterol. Type 2 diabetes and hypertension are independently associated with transaminase elevations in women (348). In a prospective analysis, diabetes was significantly associated with incident nonalcoholic chronic liver disease and with hepatocellular carcinoma (349). Interventions that improve metabolic abnormalities in patients with diabetes (weight loss, glycemic control, treatment with specific drugs for hyperglycemia or dyslipidemia) are also beneficial for fatty liver disease (350).
Low testosterone in men
Mean levels of testosterone are lower in men with diabetes compared with age-matched men without diabetes, but obesity is a major confounder (351). The issue of treatment in asymptomatic men is controversial. The evidence for effects of testosterone replacement on outcomes is mixed, and recent guidelines suggest that screening and treatment of men without symptoms is not recommended (352).
Periodontal disease
Periodontal disease is more severe, but not necessarily more prevalent, in patients with diabetes than those without (353). Numerous studies have suggested associations with poor glycemic control, nephropathy, and CVD, but most studies are highly confounded. A comprehensive assessment, and treatment of identified disease, is indicated in patients with diabetes, but the evidence that periodontal disease treatment improves glycemic control is mixed. A meta-analysis reported a significant 0.47% improvement in A1C, but noted multiple problems with the quality of the published studies included in the analysis (354). Several high-quality RCTs have not shown a significant effect (355).
Cancer
Diabetes (possibly only type 2 diabetes) is associated with increased risk of cancers of the liver, pancreas, endometrium, colon/ rectum, breast, and bladder (356). The association may result from shared risk factors between type 2 diabetes and cancer (obesity, age, physical inactivity) but may also be due to hyperinsulinemia or hyperglycemia (356a). Patients with diabetes should be encouraged to undergo recommended age- and sex-appropriate cancer screenings and to reduce their modifiable cancer risk factors (obesity, smoking, physical inactivity).
Fractures
Age-matched hip fracture risk is significantly increased in both type 1 (summary RR 6.3) and type 2 diabetes (summary RR 1.7) in both sexes (357). Type 1 diabetes is associated with osteoporosis, but in type 2 diabetes an increased risk of hip fracture is seen despite higher bone mineral density (BMD) (358). One study showed that prevalent vertebral fractures were significantly more common in men and women with type 2 diabetes, but were not associated with BMD (359). In three large observational studies of older adults, femoral neck BMD T-score and the World Health Organization Fracture Risk Algorithm (FRAX) score were associated with hip and nonspine fracture, although fracture risk was higher in diabetic participants compared with participants without diabetes for a given T-score and age or for a given FRAX score risk (360). It is appropriate to assess fracture history and risk factors in older patients with diabetes and to recommend BMD testing if appropriate for the patient's age and sex. For at-risk patients, it is reasonable to consider standard primary or secondary prevention strategies (reduce risk factors for falls, ensure adequate calcium and vitamin D intake, and avoid use of medications that lower BMD, such as glucocorticoids) and to consider pharmacotherapy for high-risk patients. For patients with type 2 diabetes with fracture risk factors, avoidance of TZDs is warranted.
Cognitive impairment
Diabetes is associated with significantly increased risk of cognitive decline, a greater rate of cognitive decline, and increased risk of dementia (361,362). In a 15-year prospective study of a community-dwelling people over the age of 60 years, the presence of diabetes at baseline significantly increased the age- and sex-adjusted incidence of all-cause dementia, Alzheimer disease, and vascular dementia compared with rates in those with normal glucose tolerance (363). In a substudy of the ACCORD study, there were no differences in cognitive outcomes between intensive and standard glycemic control, although there was significantly less of a decrement in total brain volume by MRI in participants in the intensive arm (364). The effects of hyperglycemia and insulin on the brain are areas of intense research interest.
VIII. DIABETES CARE IN SPECIFIC POPULATIONS
A. Children and adolescents
1. Type 1 diabetes.
Three-quarters of all cases of type 1 diabetes are diagnosed in individuals <18 years of age. It is appropriate to consider the unique aspects of care and management of children and adolescents with type 1 diabetes. Children with diabetes differ from adults in many respects, including changes in insulin sensitivity related to sexual maturity and physical growth, ability to provide self-care, supervision in child care and school, and unique neurologic vulnerability to hypoglycemia and DKA. Attention to such issues as family dynamics, developmental stages, and physiological differences related to sexual maturity are all essential in developing and implementing an optimal diabetes regimen. Although recommendations for children and adolescents are less likely to be based on clinical trial evidence, expert opinion and a review of available and relevant experimental data are summarized in the ADA statement on care of children and adolescents with type 1 diabetes (365).
Ideally, the care of a child or adolescent with type 1 diabetes should be provided by a multidisciplinary team of specialists trained in the care of children with pediatric diabetes. At the very least, education of the child and family should be provided by health care providers trained and experienced in childhood diabetes and sensitive to the challenges posed by diabetes in this age-group. At the time of initial diagnosis, it is essential that diabetes education be provided in a timely fashion, with the expectation that the balance between adult supervision and self-care should be defined by, and will evolve according to, physical, psychological, and emotional maturity. MNT and psychological support should be provided at diagnosis, and regularly thereafter, by individuals experienced with the nutritional and behavioral needs of the growing child and family.
a. Glycemic control
Recommendations
Consider age when setting glycemic goals in children and adolescents with type 1 diabetes. (E)
While current standards for diabetes management reflect the need to maintain glucose control as near to normal as safely possible, special consideration should be given to the unique risks of hypoglycemia in young children. Glycemic goals may need to be modified to take into account the fact that most children <6 or 7 years of age have a form of “hypoglycemic unawareness,” including immaturity of and a relative inability to recognize and respond to hypoglycemic symptoms, placing them at greater risk for severe hypoglycemia and its sequelae. In addition, and unlike the case in adults, young children below the age of 5 years may be at risk for permanent cognitive impairment after episodes of severe hypoglycemia (366–368). Furthermore, findings from the DCCT demonstrated that near-normalization of blood glucose levels was more difficult to achieve in adolescents than adults. Nevertheless, the increased frequency of use of basal-bolus regimens and insulin pumps in youth from infancy through adolescence has been associated with more children reaching ADA blood glucose targets (369,370) in those families in which both parents and the child with diabetes participate jointly to perform the required diabetes-related tasks. Furthermore, recent studies documenting neurocognitive sequelae of hyperglycemia in children provide another compelling motivation for achieving glycemic targets (371,372).
In selecting glycemic goals, the benefits on long-term health outcomes of achieving a lower A1C should be balanced against the risks of hypoglycemia and the developmental burdens of intensive regimens in children and youth. Age-specific glycemic and A1C goals are presented in Table 16.
Table 16.
Plasma blood glucose and A1C goals for type 1 diabetes by age-group
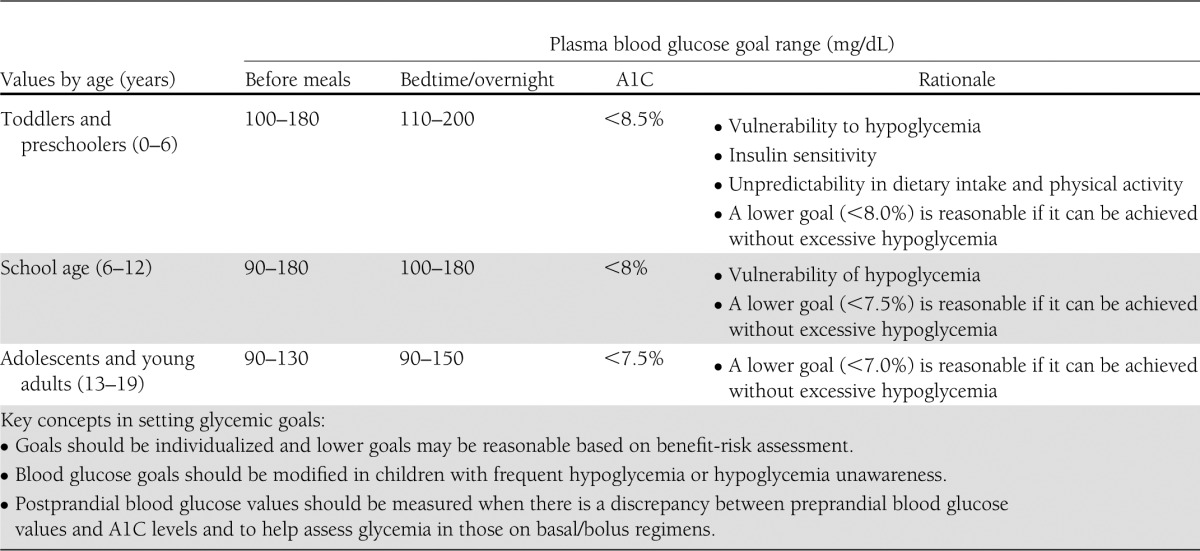
b. Screening and management of chronic complications in children and adolescents with type 1 diabetes
i. Nephropathy
Recommendations
Annual screening for microalbuminuria, with a random spot urine sample for albumin-to-creatinine ratio (ACR), should be considered once the child is 10 years of age and has had diabetes for 5 years. (B)
Treatment with an ACE inhibitor, titrated to normalization of albumin excretion, should be considered when elevated ACR is subsequently confirmed on two additional specimens from different days. (E)
ii. Hypertension
Recommendations
Initial treatment of high-normal blood pressure (systolic or diastolic blood pressure consistently above the 90th percentile for age, sex, and height) includes dietary intervention and exercise, aimed at weight control and increased physical activity, if appropriate. If target blood pressure is not reached with 3–6 months of lifestyle intervention, pharmacologic treatment should be considered. (E)
Pharmacologic treatment of hypertension (systolic or diastolic blood pressure consistently above the 95th percentile for age, sex, and height or consistently >130/80 mmHg, if 95% exceeds that value) should be considered as soon as the diagnosis is confirmed. (E)
ACE inhibitors should be considered for the initial treatment of hypertension, following appropriate reproductive counseling due to its potential teratogenic effects. (E)
The goal of treatment is a blood pressure consistently <130/80 mmHg or below the 90th percentile for age, sex, and height, whichever is lower. (E)
It is important that blood pressure measurements are determined correctly, using the appropriate size cuff, and with the child seated and relaxed. Hypertension should be confirmed on at least 3 separate days. Normal blood pressure levels for age, sex, and height and appropriate methods for determinations are available online at www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf.
iii. Dyslipidemia
Recommendations
Screening
If there is a family history of hypercholesterolemia or a cardiovascular event before age 55 years, or if family history is unknown, then consider obtaining a fasting lipid profile on children >2 years of age soon after diagnosis (after glucose control has been established). If family history is not of concern, then consider the first lipid screening at puberty (≥10 years of age). For children diagnosed with diabetes at or after puberty, consider obtaining a fasting lipid profile soon after diagnosis (after glucose control has been established). (E)
For both age-groups, if lipids are abnormal, annual monitoring is reasonable. If LDL cholesterol values are within the accepted risk levels (<100 mg/dL [2.6 mmol/L]), a lipid profile repeated every 5 years is reasonable. (E)
Treatment
Initial therapy may consist of optimization of glucose control and MNT using a Step 2 American Heart Association diet aimed at a decrease in the amount of saturated fat in the diet. (E)
After the age of 10, the addition of a statin in patients who, after MNT and lifestyle changes, have LDL cholesterol >160 mg/dL (4.1 mmol/L), or LDL cholesterol >130 mg/dL (3.4 mmol/L) and one or more CVD risk factors, is reasonable. (E)
The goal of therapy is an LDL cholesterol value <100 mg/dL (2.6 mmol/L). (E)
People diagnosed with type 1 diabetes in childhood have a high risk of early subclinical (373–375) and clinical (376) CVD. Although intervention data are lacking, the American Heart Association (AHA) categorizes children with type 1 diabetes in the highest tier for cardiovascular risk and recommends both lifestyle and pharmacologic treatment for those with elevated LDL cholesterol levels (377,378). Initial therapy should be with a Step 2 AHA diet, which restricts saturated fat to 7% of total calories and restricts dietary cholesterol to 200 mg per day. Data from randomized clinical trials in children as young as 7 months of age indicate that this diet is safe and does not interfere with normal growth and development (379,380).
Neither long-term safety nor cardiovascular outcome efficacy of statin therapy has been established for children. However, recent studies have shown short-term safety equivalent to that seen in adults, and efficacy in lowering LDL cholesterol levels, improving endothelial function, and causing regression of carotid intimal thickening (381–383). No statin is approved for use under the age of 10 years, and statin treatment should generally not be used in children with type 1 diabetes prior to this age. For postpubertal girls, issues of pregnancy prevention are paramount, since statins are category X in pregnancy. For more information, see section VIII.B. Preconception care.
iv. Retinopathy
Recommendations
The first ophthalmologic examination should be obtained once the child is ≥10 years of age and has had diabetes for 3–5 years. (B)
After the initial examination, annual routine follow-up is generally recommended. Less-frequent examinations may be acceptable on the advice of an eye care professional. (E)
Although retinopathy (like albuminuria) most commonly occurs after the onset of puberty and after 5–10 years of diabetes duration (384), it has been reported in prepubertal children and with diabetes duration of only 1–2 years. Referrals should be made to eye care professionals with expertise in diabetic retinopathy, an understanding of the risk for retinopathy in the pediatric population, and experience in counseling the pediatric patient and family on the importance of early prevention/intervention.
v. Celiac disease
Recommendations
Consider screening children with type 1 diabetes for celiac disease by measuring tissue transglutaminase or anti-endomysial antibodies, with documentation of normal total serum IgA levels, soon after the diagnosis of diabetes. (E)
Testing should be considered in children with growth failure, failure to gain weight, weight loss, diarrhea, flatulence, abdominal pain, or signs of malabsorption, or in children with frequent unexplained hypoglycemia or deterioration in glycemic control. (E)
Consider referral to a gastroenterologist for evaluation with endoscopy and biopsy for confirmation of celiac disease in asymptomatic children with positive antibodies. (E)
Children with biopsy-confirmed celiac disease should be placed on a gluten-free diet and have consultation with a dietitian experienced in managing both diabetes and celiac disease. (B)
Celiac disease is an immune-mediated disorder that occurs with increased frequency in patients with type 1 diabetes (1–16% of individuals compared with 0.3–1% in the general population) (385,386). Symptoms of celiac disease include diarrhea, weight loss or poor weight gain, growth failure, abdominal pain, chronic fatigue, malnutrition due to malabsorption, and other gastrointestinal problems, and unexplained hypoglycemia or erratic blood glucose concentrations.
Screening for celiac disease includes measuring serum levels of tissue transglutaminase or anti-endomysial antibodies, then small bowel biopsy in antibody-positive children. One small study that included children with and without type 1 diabetes suggested that antibody-positive but biopsy-negative children were similar clinically to those who were biopsy positive, and that biopsy-negative children had benefits from a gluten-free diet but worsening on a usual diet (387). Because this study was small, and because children with type 1 diabetes already need to follow a careful diet, it is difficult to advocate for not confirming the diagnosis by biopsy before recommending a gluten-free diet, especially in asymptomatic children. In symptomatic children with type 1 diabetes and celiac disease, gluten-free diets reduce symptoms and rates of hypoglycemia (388).
vi. Hypothyroidism
Recommendations
Consider screening children with type 1 diabetes for thyroid peroxidase and thyroglobulin antibodies soon after diagnosis. (E)
Measuring TSH concentrations soon after diagnosis of type 1 diabetes, after metabolic control has been established, is reasonable. If normal, consider rechecking every 1–2 years, especially if the patient develops symptoms of thyroid dysfunction, thyromegaly, or an abnormal growth rate. (E)
Autoimmune thyroid disease is the most common autoimmune disorder associated with diabetes, occurring in 17–30% of patients with type 1 diabetes (389). About one-quarter of type 1 children have thyroid autoantibodies at the time of diagnosis of their diabetes (390), and the presence of thyroid autoantibodies is predictive of thyroid dysfunction, generally hypothyroidism but less commonly hyperthyroidism (391). Subclinical hypothyroidism may be associated with increased risk of symptomatic hypoglycemia (392) and with reduced linear growth (393). Hyperthyroidism alters glucose metabolism, potentially resulting in deterioration of metabolic control.
c. Self-management
No matter how sound the medical regimen, it can only be as good as the ability of the family and/or individual to implement it. Family involvement in diabetes remains an important component of optimal diabetes management throughout childhood and into adolescence. Health care providers who care for children and adolescents, therefore, must be capable of evaluating the behavioral, emotional, and psychosocial factors that interfere with implementation and then must work with the individual and family to resolve problems that occur and/or to modify goals as appropriate.
d. School and day care
Since a sizable portion of a child's day is spent in school, close communication with and cooperation of school or day care personnel is essential for optimal diabetes management, safety, and maximal academic opportunities. See the ADA position statement on diabetes care in the school and day care setting (394) for further discussion.
e. Transition from pediatric to adult care
Recommendations
As teens transition into emerging adulthood, health care providers and families must recognize their many vulnerabilities (B) and prepare the developing teen, beginning in early to mid adolescence and at least 1 year prior to the transition. (E)
Both pediatricians and adult health care providers should assist in providing support and links to resources for the teen and emerging adult. (B)
Care and close supervision of diabetes management is increasingly shifted from parents and other older adults throughout childhood and adolescence; however, the shift from pediatric to adult health care providers often occurs very abruptly as the older teen enters the next developmental stage, referred to as emerging adulthood (395, 397), a critical period for young people who have diabetes. During this period of major life transitions, youth begin to move out of their parents’ home and must become more fully responsible for their diabetes care including the many aspects of self management, making medical appointments, and financing health care once they are no longer covered under their parents health insurance (396,397). In addition to lapses in health care, this is also a period of deterioration in glycemic control, increased occurrence of acute complications, psychosocial and emotional behavioral issues, and emergence of chronic complications (396–399).
Though scientific evidence continues to be limited, it is clear that early and ongoing attention be given to comprehensive and coordinated planning for seamless transition of all youth from pediatric to adult health care (396,397). A comprehensive discussion regarding the challenges faced during this period, including specific recommendations is found in the ADA position statement “Diabetes Care for Emerging Adults: Recommendations for the Transition from Pediatric to Adult Diabetes Care Systems” (397).
The National Diabetes Education Program (NDEP) has materials available to facilitate the transition process (http://ndep.nih.gov/transitions/).
2. Type 2 diabetes.
The incidence of type 2 diabetes in adolescents is increasing, especially in ethnic minority populations (28). Distinction between type 1 and type 2 diabetes in children can be difficult, since the prevalence of overweight in children continues to rise and since autoantigens and ketosis may be present in a substantial number of patients with features of type 2 diabetes (including obesity and acanthosis nigricans). Such a distinction at the time of diagnosis is critical since treatment regimens, educational approaches, and dietary counsel will differ markedly between the two diagnoses.
Type 2 diabetes has a significant incidence of comorbidities already present at the time of diagnosis (400). It is recommended that blood pressure measurement, a fasting lipid profile, microalbuminuria assessment, and dilated eye examination be performed at the time of diagnosis. Thereafter, screening guidelines and treatment recommendations for hypertension, dyslipidemia, microalbuminuria and retinopathy in youth with type 2 diabetes are similar to those for youth with type 1. Additional problems that may need to be addressed include polycystic ovarian disease and the various comorbidities associated with pediatric obesity such as sleep apnea, hepatic steatosis, orthopedic complications, and psychosocial concerns. An ADA consensus statement on this subject (30) provides guidance on the prevention, screening, and treatment of type 2 diabetes and its comorbidities in young people.
3. Monogenic diabetes syndromes.
Monogenic forms of diabetes (neonatal diabetes or maturity-onset diabetes of youth) represent a small fraction of children with diabetes (<5%), but the ready availability of commercial genetic testing is now enabling a true genetic diagnosis with increasing frequency. It is important to correctly diagnose one of the monogenic forms of diabetes, as these children may be incorrectly diagnosed with type 1 or type 2 diabetes, leading to nonoptimal treatment regimens and delays in diagnosing other family members.
The diagnosis of monogenic diabetes should be considered in the following settings: diabetes diagnosed within the first 6 months of life; in children with strong family history of diabetes but without typical features of type 2 diabetes (nonobese, low-risk ethnic group); in children with mild fasting hyperglycemia (100–150 mg/dL [5.5–8.5 mmol]), especially if young and nonobese; and in children with diabetes but with negative autoantibodies without signs of obesity or insulin resistance. A recent international consensus document discusses further in detail the diagnosis and management of children with monogenic forms of diabetes (401).
B. Preconception care
Recommendations
A1C levels should be as close to normal as possible (<7%) in an individual patient before conception is attempted. (B)
Starting at puberty, preconception counseling should be incorporated in the routine diabetes clinic visit for all women of childbearing potential. (C)
Women with diabetes who are contemplating pregnancy should be evaluated and, if indicated, treated for diabetic retinopathy, nephropathy, neuropathy, and CVD. (B)
Medications used by such women should be evaluated prior to conception, since drugs commonly used to treat diabetes and its complications may be contraindicated or not recommended in pregnancy, including statins, ACE inhibitors, ARBs, and most noninsulin therapies. (E)
Since many pregnancies are unplanned, consider the potential risks and benefits of medications that are contraindicated in pregnancy in all women of childbearing potential, and counsel women using such medications accordingly. (E)
Major congenital malformations remain the leading cause of mortality and serious morbidity in infants of mothers with type 1 and type 2 diabetes. Observational studies indicate that the risk of malformations increases continuously with increasing maternal glycemia during the first 6–8 weeks of gestation, as defined by first-trimester A1C concentrations. There is no threshold for A1C values below which risk disappears entirely. However, malformation rates above the 1–2% background rate of nondiabetic pregnancies appear to be limited to pregnancies in which first-trimester A1C concentrations are >1% above the normal range for a nondiabetic pregnant woman.
Preconception care of diabetes appears to reduce the risk of congenital malformations. Five nonrandomized studies compared rates of major malformations in infants between women who participated in preconception diabetes care programs and women who initiated intensive diabetes management after they were already pregnant. The preconception care programs were multidisciplinary and designed to train patients in diabetes self-management with diet, intensified insulin therapy, and SMBG. Goals were set to achieve normal blood glucose concentrations, and >80% of subjects achieved normal A1C concentrations before they became pregnant. In all five studies, the incidence of major congenital malformations in women who participated in preconception care (range 1.0–1.7% of infants) was much lower than the incidence in women who did not participate (range 1.4–10.9% of infants) (94). One limitation of these studies is that participation in preconception care was self-selected rather than randomized. Thus, it is impossible to be certain that the lower malformation rates resulted fully from improved diabetes care. Nonetheless, the evidence supports the concept that malformations can be reduced or prevented by careful management of diabetes before pregnancy.
Planned pregnancies greatly facilitate preconception diabetes care. Unfortunately, nearly two-thirds of pregnancies in women with diabetes are unplanned, leading to a persistent excess of malformations in infants of diabetic mothers. To minimize the occurrence of these devastating malformations, standard care for all women with diabetes who have child-bearing potential, beginning at the onset of puberty or at diagnosis, should include 1) education about the risk of malformations associated with unplanned pregnancies and poor metabolic control; and 2) use of effective contraception at all times, unless the patient has good metabolic control and is actively trying to conceive.
Women contemplating pregnancy need to be seen frequently by a multidisciplinary team experienced in the management of diabetes before and during pregnancy. The goals of preconception care are to 1) involve and empower the patient in the management of her diabetes, 2) achieve the lowest A1C test results possible without excessive hypoglycemia, 3) assure effective contraception until stable and acceptable glycemia is achieved, and 4) identify, evaluate, and treat long-term diabetes complications such as retinopathy, nephropathy, neuropathy, hypertension, and CHD (94).
Among the drugs commonly used in the treatment of patients with diabetes, a number may be relatively or absolutely contraindicated during pregnancy. Statins are category X (contraindicated for use in pregnancy) and should be discontinued before conception, as should ACE inhibitors (402). ARBs are category C (risk cannot be ruled out) in the first trimester, but category D (positive evidence of risk) in later pregnancy, and should generally be discontinued before pregnancy. Since many pregnancies are unplanned, health care professionals caring for any woman of childbearing potential should consider the potential risks and benefits of medications that are contraindicated in pregnancy. Women using medications such as statins or ACE inhibitors need ongoing family planning counseling. Among the oral antidiabetic agents, metformin and acarbose are classified as category B (no evidence of risk in humans) and all others as category C. Potential risks and benefits of oral antidiabetic agents in the preconception period must be carefully weighed, recognizing that data are insufficient to establish the safety of these agents in pregnancy.
For further discussion of preconception care, see the ADA consensus statement on preexisting diabetes and pregnancy (94) and also the position statement (403) on this subject.
C. Older adults
Recommendations
Older adults who are functional, cognitively intact, and have significant life expectancy should receive diabetes care using goals developed for younger adults. (E)
Glycemic goals for older adults not meeting the above criteria may be relaxed using individual criteria, but hyperglycemia leading to symptoms or risk of acute hyperglycemic complications should be avoided in all patients. (E)
Other cardiovascular risk factors should be treated in older adults with consideration of the time frame of benefit and the individual patient. Treatment of hypertension is indicated in virtually all older adults, and lipid and aspirin therapy may benefit those with life expectancy at least equal to the time frame of primary or secondary prevention trials. (E)
Screening for diabetes complications should be individualized in older adults, but particular attention should be paid to complications that would lead to functional impairment. (E)
Diabetes is an important health condition for the aging population; at least 20% of patients over the age of 65 years have diabetes, and this number can be expected to grow rapidly in the coming decades. Older individuals with diabetes have higher rates of premature death, functional disability, and coexisting illnesses such as hypertension, CHD, and stroke than those without diabetes. Older adults with diabetes are also at greater risk than other older adults for several common geriatric syndromes, such as polypharmacy, depression, cognitive impairment, urinary incontinence, injurious falls, and persistent pain.
The American Geriatric Society's guidelines for improving the care of the older person with diabetes (404) have influenced the following discussion and recommendations. The care of older adults with diabetes is complicated by their clinical and functional heterogeneity. Some older individuals developed diabetes years earlier and may have significant complications; others who are newly diagnosed may have had years of undiagnosed diabetes with resultant complications or may have few complications from the disease. Some older adults with diabetes are frail and have other underlying chronic conditions, substantial diabetes-related comorbidity, or limited physical or cognitive functioning. Other older individuals with diabetes have little comorbidity and are active. Life expectancies are highly variable for this population, but often longer than clinicians realize. Providers caring for older adults with diabetes must take this heterogeneity into consideration when setting and prioritizing treatment goals.
There are few long-term studies in older adults demonstrating the benefits of intensive glycemic, blood pressure, and lipid control. Patients who can be expected to live long enough to reap the benefits of long-term intensive diabetes management and who are active, have good cognitive function, and are willing should be provided with the needed education and skills to do so and be treated using the goals for younger adults with diabetes.
For patients with advanced diabetes complications, life-limiting comorbid illness, or substantial cognitive or functional impairment, it is reasonable to set less intensive glycemic target goals. These patients are less likely to benefit from reducing the risk of microvascular complications and more likely to suffer serious adverse effects from hypoglycemia. However, patients with poorly controlled diabetes may be subject to acute complications of diabetes, including dehydration, poor wound healing, and hyperglycemic hyperosmolar coma. Glycemic goals at a minimum should avoid these consequences.
Although control of hyperglycemia may be important in older individuals with diabetes, greater reductions in morbidity and mortality may result from control of other cardiovascular risk factors rather than from tight glycemic control alone. There is strong evidence from clinical trials of the value of treating hypertension in the elderly (405,406). There is less evidence for lipid-lowering and aspirin therapy, although the benefits of these interventions for primary and secondary prevention are likely to apply to older adults whose life expectancies equal or exceed the time frames seen in clinical trials.
Special care is required in prescribing and monitoring pharmacologic therapy in older adults. Metformin is often contraindicated because of renal insufficiency or significant heart failure. TZDs can cause fluid retention, which may exacerbate or lead to heart failure. They are contraindicated in patients with CHF (New York Heart Association Class III and IV), and if used at all should be used very cautiously in those with, or at risk for, milder degrees of CHF. Sulfonylureas, other insulin secretagogues, and insulin can cause hypoglycemia. Insulin use requires that patients or caregivers have good visual and motor skills and cognitive ability. Drugs should be started at the lowest dose and titrated up gradually until targets are reached or side effects develop.
Screening for diabetes complications in older adults also should be individualized. Particular attention should be paid to complications that can develop over short periods of time and/or that would significantly impair functional status, such as visual and lower extremity complications.
D. Cystic fibrosis–related diabetes (CFRD)
Recommendations
Annual screening for CFRD with OGTT should begin by age 10 years in all patients with cystic fibrosis who do not have CFRD (B). Use of A1C as a screening test for CFRD is not recommended. (B)
During a period of stable health the diagnosis of CFRD can be made in cystic fibrosis patients according to usual diagnostic criteria. (E)
Patients with CFRD should be treated with insulin to attain individualized glycemic goals. (A)
Annual monitoring for complications of diabetes is recommended, beginning 5 years after the diagnosis of CFRD. (E)
CFRD is the most common comorbidity in persons with cystic fibrosis, occurring in about 20% of adolescents and 40–50% of adults. The additional diagnosis of diabetes in this population is associated with worse nutritional status, more severe inflammatory lung disease, and greater mortality from respiratory failure. Insulin insufficiency related to partial fibrotic destruction of the islet mass is the primary defect in CFRD. Genetically determined function of the remaining β-cells and insulin resistance associated with infection and inflammation may also play a role. Encouraging new data suggest that early detection and aggressive insulin therapy have narrowed the gap in mortality between cystic fibrosis patients with and without diabetes, and have eliminated the difference in mortality between the sexes (407).
Recommendations for the clinical management of CFRD can be found in a recent ADA position statement on this topic (408).
IX. DIABETES CARE IN SPECIFIC SETTINGS
A. Diabetes care in the hospital
Recommendations
All patients with diabetes admitted to the hospital should have their diabetes clearly identified in the medical record. (E)
All patients with diabetes should have an order for blood glucose monitoring, with results available to all members of the health care team. (E)
- Goals for blood glucose levels:
- ○ Critically ill patients: Insulin therapy should be initiated for treatment of persistent hyperglycemia starting at a threshold of no greater than 180 mg/dL (10 mmol/L). Once insulin therapy is started, a glucose range of 140–180 mg/dL (7.8 to 10 mmol/L) is recommended for the majority of critically ill patients. (A)
- ○ More stringent goals, such as 110–140 mg/dL (6.1–7.8 mmol/L) may be appropriate for selected patients, as long as this can be achieved without significant hypoglycemia. (C)
- ○ Critically ill patients require an intravenous insulin protocol that has demonstrated efficacy and safety in achieving the desired glucose range without increasing risk for severe hypoglycemia. (E)
- ○ Non–critically ill patients: There is no clear evidence for specific blood glucose goals. If treated with insulin, premeal blood glucose targets generally <140 mg/dL (7.8 mmol/L) with random blood glucose <180 mg/dL (10.0 mmol/L) are reasonable, provided these targets can be safely achieved. More stringent targets may be appropriate in stable patients with previous tight glycemic control. Less stringent targets may be appropriate in those with severe comorbidities. (E)
Scheduled subcutaneous insulin with basal, nutritional, and correction components is the preferred method for achieving and maintaining glucose control in noncritically ill patients.
Glucose monitoring should be initiated in any patient not known to be diabetic who receives therapy associated with high-risk for hyperglycemia, including high-dose glucocorticoid therapy, initiation of enteral or parenteral nutrition, or other medications such as octreotide or immunosuppressive medications. (B) If hyperglycemia is documented and persistent, consider treating such patients to the same glycemic goals as patients with known diabetes. (E)
A hypoglycemia management protocol should be adopted and implemented by each hospital or hospital system. A plan for preventing and treating hypoglycemia should be established for each patient. Episodes of hypoglycemia in the hospital should be documented in the medial record and tracked. (E)
Consider obtaining an A1C on patients with diabetes admitted to the hospital if the result of testing in the previous 2–3 months is not available. (E)
Patients with hyperglycemia in the hospital who do not have a prior diagnosis of diabetes should have appropriate plans for follow-up testing and care documented at discharge. (E)
Hyperglycemia in the hospital can represent previously known diabetes, previously undiagnosed diabetes, or hospital-related hyperglycemia (fasting blood glucose ≥126 mg/dL or random blood glucose ≥200 mg/dL occurring during the hospitalization that reverts to normal after hospital discharge). Hyperglycemia in the hospital is extensively reviewed in an ADA technical review (409). An updated consensus statement by the American Association of Clinical Endocrinologists (AACE) and ADA (410) forms the basis for the discussion and guidelines in this section.
The management of hyperglycemia in the hospital has often been considered secondary in importance to the condition that prompted admission (409). However, a body of literature now supports targeted glucose control in the hospital setting for potential improved clinical outcomes. Hyperglycemia in the hospital may result from stress, decompensation of type 1 or type 2 or other forms of diabetes, and/or may be iatrogenic due to withholding of antihyperglycemic medications or administration of hyperglycemia-provoking agents such as glucocorticoids or vasopressors.
There is substantial observational evidence linking hyperglycemia in hospitalized patients (with or without diabetes) to poor outcomes. Cohort studies as well as a few early RCTs suggested that intensive treatment of hyperglycemia improved hospital outcomes (409,411,412). In general, these studies were heterogeneous in terms of patient population, blood glucose targets and insulin protocols used, provision of nutritional support, and the proportion of patients receiving insulin, which limits the ability to make meaningful comparisons among them. Recent trials in critically ill patients have failed to show a significant improvement in mortality with intensive glycemic control (413,414) or have even shown increased mortality risk (415). Moreover, these recent RCTs have highlighted the risk of severe hypoglycemia resulting from such efforts (413–418).
The largest study to date, NICE-SUGAR, a multicenter, multinational RCT, compared the effect of intensive glycemic control (target 81–108 mg/dL, mean blood glucose attained 115 mg/dL) to standard glycemic control (target 144–180 mg/dL, mean blood glucose attained 144 mg/dL) on outcomes among 6,104 critically ill participants, almost all of whom required mechanical ventilation (415). Ninety-day mortality was significantly higher in the intensive versus the conventional group in both surgical and medical patients, as was mortality from cardiovascular causes. Severe hypoglycemia was also more common in the intensively treated group (6.8% vs. 0.5%; P < 0.001). The precise reason for the increased mortality in the tightly controlled group is unknown. The results of this study lie in stark contrast to a famous 2001 single-center study which reported a 42% relative reduction in ICU mortality in critically ill surgical patients treated to a target blood glucose of 80–110 mg/dL (411). Importantly, the control group in NICE-SUGAR had reasonably good blood glucose management, maintained at a mean glucose of 144 mg/dL, only 29 mg/dL above the intensively managed patients. Accordingly, this study's findings do not disprove the notion that glycemic control in the ICU is important. However they do strongly suggest that it may not be necessary to target blood glucose values <140 mg/dL, and that a highly stringent target of <110 mg/dL may actually be dangerous.
In a recent meta-analysis of 26 trials (N = 13,567), which included the NICE-SUGAR data, the pooled relative risk (RR) of death with intensive insulin therapy was 0.93 as compared with conventional therapy (95% CI 0.83–1.04) (418). Approximately half of these trials reported hypoglycemia, with a pooled RR of intensive therapy of 6.0 (95% CI 4.5–8.0). The specific ICU setting influenced the findings, with patients in surgical ICUs appearing to benefit from intensive insulin therapy (RR 0.63, 95% CI 0.44–0.91), while those in other medical and mixed critical care settings did not. It was concluded that, overall, intensive insulin therapy increased the risk of hypoglycemia but provided no overall benefit on mortality in the critically ill, although a possible mortality benefit to patients admitted to the surgical ICU was suggested.
1. Glycemic targets in hospitalized patients.
Definition of glucose abnormalities in the hospital setting.
Hyperglycemia in the hospital has been defined as any blood glucose >140 mg/dL (7.8 mmol/L). Levels that are significantly and persistently above this may require treatment in hospitalized patients. A1C values >6.5% suggest, in undiagnosed patients, that diabetes preceded hospitalization (419). Hypoglycemia has been defined as any blood glucose <70 mg/dL (3.9 mmol/L). This is the standard definition in outpatients and correlates with the initial threshold for the release of counterregulatory hormones. Severe hypoglycemia in hospitalized patients has been defined by many as <40 mg/dL (2.2 mmol/L), although this is lower than the ∼50 mg/dL (2.8 mmol/L) level at which cognitive impairment begins in normal individuals (420). As with hyperglycemia, hypoglycemia among inpatients is also associated with adverse short- and long-term outcomes. Early recognition and treatment of mild-to-moderate hypoglycemia (40–69 mg/dL (2.2–3.8 mmol/L) can prevent deterioration to a more severe episode with potential adverse sequelae (410).
Critically ill patients.
Based on the weight of the available evidence, for the majority of critically ill patients in the ICU setting, insulin infusion should be used to control hyperglycemia, with a starting threshold of no higher than 180 mg/dL (10.0 mmol/L). Once intravenous insulin is started, the glucose level should be maintained between 140 and 180 mg/dL (7.8–10.0 mmol/L). Greater benefit maybe realized at the lower end of this range. Although strong evidence is lacking, somewhat lower glucose targets may be appropriate in selected patients. However, targets <110 mg/dL (6.1 mmol/L) are not recommended. Use of insulin infusion protocols with demonstrated safety and efficacy, resulting in low rates of hypoglycemia, are highly recommended (410).
Noncritically ill patients.
With no prospective RCT data to inform specific glycemic targets in noncritically ill patients, recommendations are based on clinical experience and judgment. For the majority of noncritically ill patients treated with insulin, premeal glucose targets should generally be <140 mg/dL (7.8 mmol/L) with random blood glucose <180 mg/dL (10.0 mmol/L), as long as these targets can be safely achieved. To avoid hypoglycemia, consideration should be given to reassessing the insulin regimen if blood glucose levels fall <100 mg/dL (5.6 mmol/L). Modification of the regimen is required when blood glucose values are <70 mg/dL (3.9 mmol/L), unless the event is easily explained by other factors (such as a missed meal). There is some evidence that systematic attention to hyperglycemia in the emergency room leads to better glycemic control in the hospital for those subsequently admitted (421).
Occasional patients with a prior history of successful tight glycemic control in the outpatient setting who are clinically stable may be maintained with a glucose range below the above cut points. Conversely, higher glucose ranges may be acceptable in terminally ill patients or in patients with severe comorbidities, as well as in those in patient-care settings where frequent glucose monitoring or close nursing supervision is not feasible.
Clinical judgment, combined with ongoing assessment of the patient's clinical status, including changes in the trajectory of glucose measures, the severity of illness, nutritional status, or concurrent use of medications that might affect glucose levels (e.g., steroids, octreotide), must be incorporated into the day-to-day decisions regarding insulin dosing (410).
2. Antihyperglycemic agents in hospitalized patients.
In the hospital setting, insulin therapy is the preferred method of glycemic control in majority of clinical situations (410). In the ICU, intravenous infusion is the preferred route of insulin administration. When the patient is transitioned off intravenous insulin to subcutaneous therapy, precautions should be taken to prevent hyperglycemia escape (422,423). Outside of critical care units, scheduled subcutaneous insulin that delivers basal, nutritional, and correction (supplemental) components is preferred. Prolonged therapy with sliding scale insulin (SSI) as the sole regimen is ineffective in the majority of patients, increases risk of both hypoglycemia and hyperglycemia, and has recently been shown in a randomized trial to be associated with adverse outcomes in general surgery patients with type 2 diabetes (424). SSI is potentially dangerous in type 1 diabetes (410). The reader is referred to several recent publications and reviews that describe currently available insulin preparations and protocols and provide guidance in use of insulin therapy in specific clinical settings including parenteral nutrition (425) and enteral tube feedings and with high-dose glucocorticoid therapy (410).
There are no data on the safety and efficacy of oral agents and injectable noninsulin therapies such as GLP1 analogs and pramlintide in the hospital. They are generally considered to have a limited role in the management of hyperglycemia in conjunction with acute illness. Continuation of these agents may be appropriate in selected stable patients who are expected to consume meals at regular intervals, and they may be initiated or resumed in anticipation of discharge once the patient is clinically stable. Specific caution is required with metformin due to the possibility that a contraindication may develop during the hospitalization, such as renal insufficiency, unstable hemodynamic status, or need for an imaging study that requires a radio-contrast dye.
3. Preventing hypoglycemia.
In the hospital, multiple risk factors for hypoglycemia are present. Patients with or without diabetes may experience hypoglycemia in the hospital in association with altered nutritional state, heart failure, renal or liver disease, malignancy, infection, or sepsis. Additional triggering events leading to iatrogenic hypoglycemia include sudden reduction of corticosteroid dose, altered ability of the patient to report symptoms, reduction of oral intake, emesis, new n.p.o. status, inappropriate timing of short- or rapid-acting insulin in relation to meals, reduction of rate of administration of intravenous dextrose, and unexpected interruption of enteral feedings or parenteral nutrition.
Despite the preventable nature of many inpatient episodes of hypoglycemia, institutions are more likely to have nursing protocols for the treatment of hypoglycemia than for its prevention. Tracking such episodes and analyzing their causes are important quality improvement activities (410).
4. Diabetes care providers in the hospital.
Inpatient diabetes management may be effectively championed and/or provided by primary care physicians, endocrinologists, intensivists or hospitalists. Involvement of appropriately trained specialists or specialty teams may reduce length of stay, improve glycemic control, and improve outcomes (410). In the care of diabetes, implementation of standardized order sets for scheduled and correction-dose insulin may reduce reliance on sliding-scale management. As hospitals move to comply with “meaningful use” regulations for electronic health records, as mandated by the Health Information Technology Act, efforts should be made to assure that all components of structured insulin order sets are incorporated into electronic insulin order sets (426,427).
A team approach is needed to establish hospital pathways. To achieve glycemic targets associated with improved hospital outcomes, hospitals will need multidisciplinary support to develop insulin management protocols that effectively and safely enable achievement of glycemic targets (428).
5. Self-management in the hospital.
Self-management of diabetes in the hospital may be appropriate for competent adult patients who have a stable level of consciousness, have reasonably stable daily insulin requirements, successfully conduct self-management of diabetes at home, have physical skills needed to successfully self-administer insulin and perform SMBG, have adequate oral intake, are proficient in carbohydrate counting, use multiple daily insulin injections or insulin pump therapy, and employ sick-day management. The patient and physician, in consultation with nursing staff, must agree that patient self-management is appropriate under the conditions of hospitalization.
Patients who use CSII pump therapy in the outpatient setting can be candidates for diabetes self-management in the hospital, provided that they have the mental and physical capacity to do so (410). A hospital policy and procedures delineating inpatient guidelines for CSII therapy are advisable, and availability of hospital personnel with expertise in CSII therapy is essential. It is important that nursing personnel document basal rates and bolus doses taken on a regular basis (at least daily).
6. MNT in the hospital.
The goals of MNT are to optimize glycemic control, provide adequate calories to meet metabolic demands, and create a discharge plan for follow-up care (409,429). ADA does not endorse any single meal plan or specified percentages of macronutrients, and the term “ADA diet” should no longer be used. Current nutrition recommendations advise individualization based on treatment goals, physiologic parameters, and medication usage. Consistent carbohydrate meal plans are preferred by many hospitals because they facilitate matching the prandial insulin dose to the amount of carbohydrate consumed (430). Because of the complexity of nutrition issues in the hospital, a registered dietitian, knowledgeable and skilled in MNT, should serve as an inpatient team member. The dietitian is responsible for integrating information about the patient's clinical condition, eating, and lifestyle habits and for establishing treatment goals in order to determine a realistic plan for nutrition therapy (431,432).
7. Bedside blood glucose monitoring.
Point-of-care (POC) blood glucose monitoring performed at the bedside is used to guide insulin dosing. In the patient who is receiving nutrition, the timing of glucose monitoring should match carbohydrate exposure. In the patient who is not receiving nutrition, glucose monitoring is performed every 4 to 6 h (433,434). More-frequent blood glucose testing ranging from every 30 min to every 2 h is required for patients on intravenous insulin infusions.
Safety standards should be established for blood glucose monitoring prohibiting sharing of fingerstick lancing devices, lancets, needles, and meters to reduce the risk of transmission of blood borne diseases. Shared lancing devices carry essentially the same risk as is conferred from sharing of syringes and needles (435).
Accuracy of blood glucose measurements using POC meters has limitations that must be considered. Although the FDA allows a +/− 20% error for blood glucose meters, questions about the appropriateness of these criteria have been raised (388). Glucose measures differ significantly between plasma and whole blood, terms that are often used interchangeably and can lead to misinterpretation. Most commercially available capillary blood glucose meters introduce a correction factor of ∼1.12 to report a “plasma adjusted” value (436).
Significant discrepancies between capillary, venous, and arterial plasma samples have been observed in patients with low or high hemoglobin concentrations, hypoperfusion, and the presence of interfering substances, particularly maltose, as contained in immunoglobulins (437). Analytical variability has been described with several POC meters (438). Increasingly newer generation POC blood glucose meters correct for variation in hematocrit and for interfering substances. Any glucose result that does not correlate with the patient's status should be confirmed through conventional laboratory sampling of plasma glucose. The FDA has become increasingly concerned about the use of POC blood glucose meters in the hospital and is presently reviewing matters related to their use.
8. Discharge planning and DSME.
Transition from the acute care setting is a high risk time for all patients, not just those with diabetes or new hyperglycemia. Although there is an extensive literature concerning safe transition within and from the hospital, little of it is specific to diabetes (439). It is important to remember that diabetes discharge planning is not a separate entity, but is part of an overall discharge plan. As such, discharge planning begins at admission to the hospital and is updated as projected patient needs change.
Inpatients may be discharged to varied settings, including home (with or without visiting nurse services), assisted living, rehabilitation, or skilled nursing facilities. The latter two sites are generally staffed by health professionals, so diabetes discharge planning will be limited to communication of medication and diet orders. For the patient who is discharged to assisted living or to home, the optimal program will need to consider the type and severity of diabetes, the effects of the patient's illness on blood glucose levels, and the capacities and desires of the patient. Smooth transition to outpatient care should be ensured. The Agency for Healthcare Research and Quality recommends that at a minimum, discharge plans include:
Medication reconciliation: The patient's medications must be cross-checked to ensure that no chronic medications were stopped and to ensure the safety of new prescriptions.
Whenever possible, prescriptions for new or changed medication should be filled and reviewed with the patient and family at or before discharge.
Structured discharge communication: Information on medication changes, pending tests and studies, and follow-up needs must be accurately and promptly communicated to outpatient physicians.
Discharge summaries should be transmitted to the primary physician as soon as possible after discharge.
Appointment-keeping behavior is enhanced when the inpatient team schedules outpatient medical follow up prior to discharge. Ideally the inpatient care providers or case managers/discharge planners will schedule follow-up visit(s) with the appropriate professionals, including the primary care provider, endocrinologist, and diabetes educator (99).
Teaching diabetes self-management to patients in hospitals is a challenging task. Patients are ill, under increased stress related to their hospitalization and diagnosis, and in an environment not conducive to learning. Ideally, people with diabetes should be taught at a time and place conducive to learning—as an outpatient in a recognized program of diabetes education. For the hospitalized patient, diabetes “survival skills” education is generally a feasible approach to provide sufficient information and training to enable safe care at home. Patients hospitalized because of a crisis related to diabetes management or poor care at home need education to prevent subsequent episodes of hospitalization. An assessment of the need for a home health referral or referral to an outpatient diabetes education program should be part of discharge planning for all patients.
DSME cannot wait until discharge, especially in those new to insulin therapy or in whom the diabetes regimen has been substantially altered during the hospitalization.
It is recommended that the following areas of knowledge be reviewed and addressed prior to hospital discharge:
Identification of health care provider who will provide diabetes care after discharge
Level of understanding related to the diagnosis of diabetes, SMBG, and explanation of home blood glucose goals
Definition, recognition, treatment, and prevention of hyperglycemia and hypoglycemia
Information on consistent eating patterns
When and how to take blood glucose–lowering medications including insulin administration (if going home on insulin)
Sick-day management
Proper use and disposal of needles and syringes
It is important that patients be provided with appropriate durable medical equipment, medication, supplies, and prescriptions at the time of discharge in order to avoid a potentially dangerous hiatus in care. These supplies/prescriptions should include:
Insulin (vials or pens) if needed
Syringes or pen needles (if needed)
Oral medications (if needed)
Blood glucose meter and strips
Lancets and lancing device
Urine ketone strips (type 1)
Glucagon emergency kit (insulin-treated)
Medical alert application/charm
More expanded diabetes education can be arranged in the community. An outpatient follow-up visit with the primary care provider, endocrinologist, or diabetes educator within 1 month of discharge is advised for all patients having hyperglycemia in the hospital. Clear communication with outpatient providers either directly or via hospital discharge summaries facilitates safe transitions to outpatient care. Providing information regarding the cause or the plan for determining the cause of hyperglycemia, related complications and comorbidities, and recommended treatments can assist outpatient providers as they assume ongoing care.
B. Diabetes and employment
Any person with diabetes, whether insulin-treated or noninsulin treated, should be eligible for any employment for which he/she is otherwise qualified. Employment decisions should never be based on generalizations or stereotypes regarding the effects of diabetes. When questions arise about the medical fitness of a person with diabetes for a particular job, a health care professional with expertise in treating diabetes should perform an individualized assessment. See the ADA position statement on diabetes and employment (440).
C. Diabetes and driving
A large percentage of people with diabetes in the U.S. and elsewhere seek a license to drive, either for personal or employment purposes. There has been considerable debate whether, and the extent to which, diabetes may be a relevant factor in determining the driver ability and eligibility for a license.
People with diabetes are subject to a great variety of licensing requirements applied by both state and federal jurisdictions, which may lead to loss of employment or significant restrictions on a person's license. Presence of a medical condition that can lead to significantly impaired consciousness or cognition may lead to drivers being evaluated for fitness to drive. For diabetes, this typically arises when the person has had a hypoglycemic episode behind the wheel, even if this did not lead to a motor vehicle accident.
Epidemiologic and simulator data suggest that people with insulin-treated diabetes have a small increase in risk of motor vehicle accidents, primarily due to hypoglycemia and decreased awareness of hypoglycemia. This increase (RR 1.12–1.19) is much smaller than the risks associated with teenage male drivers (RR 42), driving at night (RR 142), driving on rural roads compared with urban roads (RR 9.2), and obstructive sleep apnea (RR 2.4), all of which are accepted for unrestricted licensure.
The ADA position statement on diabetes and driving (441) recommends against blanket restrictions based on the diagnosis of diabetes and urges individual assessment by a health care professional knowledgeable in diabetes if restrictions on licensure are being considered. Patients should be evaluated for decreased awareness of hypoglycemia, hypoglycemia episodes while driving, or severe hypoglycemia. Patients with retinopathy or peripheral neuropathy require assessment to determine if those complications interfere with operation of a motor vehicle. Health care professionals should be cognizant of the potential risk of driving with diabetes and counsel their patients about detecting and avoiding hypoglycemia while driving.
D. Diabetes management in correctional institutions
People with diabetes in correctional facilities should receive care that meets national standards. Because it is estimated that nearly 80,000 inmates have diabetes, correctional institutions should have written policies and procedures for the management of diabetes and for training of medical and correctional staff in diabetes care practices. See the ADA position statement on diabetes management in correctional institutions (442) for further discussion.
X. STRATEGIES FOR IMPROVING DIABETES CARE
Recommendations
Care should be aligned with components of the Chronic Care Model to ensure productive interactions between a prepared proactive practice team and an informed activated patient. (A)
When feasible, care systems should support team-based care, community involvement, patient registries, and embedded decision support tools to meet patient needs (B).
Treatment decisions should be timely and based on evidence-based guidelines that are tailored to individual patient preferences, prognoses, and comorbidities. (B)
A patient-centered communication style should be employed that incorporates patient preferences, assesses literacy and numeracy, and addresses cultural barriers to care. (B)
There has been steady improvement in the proportion of diabetes patients achieving recommended levels of A1C, blood pressure, and LDL cholesterol in the last 10 years, both in primary care settings and in endocrinology practices. Mean A1C nationally has declined from 7.82% in 1999–2000 to 7.18% in 2004 based on NHANES data (443). This has been accompanied by improvements in lipids and blood pressure control and has led to substantial reductions in end-stage microvascular complications in those with diabetes. Nevertheless in some studies only 57.1% of adults with diagnosed diabetes achieved an A1C <7%, only 45.5% had a blood pressure <130/80 mmHg, and only 46.5% had a total cholesterol <200 mg/dL, with only 12.2% of people with diabetes achieving all three treatment goals (444). Evidence also suggests that progress in risk factor control may be slowing (445). Certain patient groups, such as those with complex comorbidities, financial or other social hardships, and/or limited English proficiency (LEP), may present particular challenges to goal-based care (446,447). Persistent variation in quality of diabetes care across providers and across practice settings even after adjusting for patient factors indicates that there remains potential for substantial further improvements in diabetes care.
While numerous interventions to improve adherence to the recommended standards have been implemented, a major barrier to optimal care is a delivery system that too often is fragmented, lacks clinical information capabilities, often duplicates services, and is poorly designed for the coordinated delivery of chronic care. The Chronic Care Model (CCM) has been shown in numerous studies to be an effective framework for improving the quality of diabetes care (448). The CCM includes six core elements for the provision of optimal care of patients with chronic disease: 1) delivery system design (moving from a reactive to a proactive care delivery system where planned visits are coordinated through a team based approach), 2) self-management support, 3) decision support (basing care on evidence-based, effective care guidelines), 4) clinical information systems (using registries that can provide patient-specific and population-based support to the care team), 5) community resources and policies (identifying or developing resources to support healthy lifestyles), and 6) health systems (to create a quality-oriented culture). Redefinition of the roles of the clinic staff and promoting self-management on the part of the patient are fundamental to the successful implementation of the CCM (449). Collaborative, multidisciplinary teams are best suited to provide such care for people with chronic conditions like diabetes and to facilitate patients’ performance of appropriate self-management (148,150,450,451).
NDEP maintains an online resource (www.betterdiabetescare.nih.gov) to help health care professionals design and implement more effective health care delivery systems for those with diabetes. Three specific objectives, with references to literature that outline practical strategies to achieve each, are below.
Objective 1: Optimize provider and team behavior
The care team should prioritize timely and appropriate intensification of lifestyle and/or pharmaceutical therapy of patients who have not achieved beneficial levels of blood pressure, lipid, or glucose control (452). Strategies such as explicit goal setting with patients (453); identifying and addressing language, numeracy, or cultural barriers to care (454–456); integrating evidence-based guidelines and clinical information tools into the process of care (457–459); and incorporating care management teams including nurses, pharmacists, and other providers (460–463) have each been shown to optimize provider and team behavior and thereby catalyze reduction in A1C, blood pressure, and LDL cholesterol.
Objective 2: Support patient behavior change
Successful diabetes care requires a systematic approach to supporting patients’ behavior change efforts, including (a) healthy lifestyle changes (physical activity, healthy eating, nonuse of tobacco, weight management, effective coping), (b) disease self-management (medication taking and management, self-monitoring of glucose and blood pressure when clinically appropriate); and (c) prevention of diabetes complications (self-monitoring of foot health, active participation in screening for eye, foot, and renal complications, and immunizations). High-quality DSME has been shown to improve patient self-management, satisfaction, and glucose control (166,464), as has delivery of on-going diabetes self-management support (DSMS) so that gains achieved during DSME are sustained (120,121,137). National DSME standards call for an integrated approach that includes clinical content and skills and behavioral strategies (goal-setting, problem solving) and addresses emotional concerns in each needed curriculum content area.
Objective 3: Change the system of care
The most successful practices have an institutional priority for providing high quality of care (465). Changes that have been shown to increase quality of diabetes care include basing care on evidence-based guidelines (466), expanding the role of teams and staff (449,467), redesigning the processes of care (468,469), implementing electronic health record tools (470,471), activating and educating patients (472,473), and identifying and/or developing and engaging community resources and public policy that support healthy lifestyles (474). Recent initiatives such as the Patient Centered Medical Home show promise to improve outcomes through coordinated primary care and offer new opportunities for team-based chronic disease care (475). Alterations in reimbursement that reward the provision of appropriate and high quality care rather than visit-based billing (476), and that can accommodate the need to personalize care goals, may provide additional incentives to improve diabetes care (477).
It is clear that optimal diabetes management requires an organized, systematic approach and involvement of a coordinated team of dedicated health care professionals working in an environment where patient-centered high quality care is a priority.
References
- 1.American Diabetes Asociation Medical Management of Type 1 Diabetes. Alexandria, VA, American Diabetes Association, 2008 [Google Scholar]
- 2.American Diabetes Asociation Medical Management of Type 2 Diabetes. Alexandria, VA, American Diabetes Association, 2008 [Google Scholar]
- 3.American Diabetes Association Intensive Diabetes Management. Alexandria, VA, American Diabetes Association, 2009 [Google Scholar]
- 4.Li R, Zhang P, Barker LE, Chowdhury FM, Zhang X. Cost-effectiveness of interventions to prevent and control diabetes mellitus: a systematic review. Diabetes Care 2010;33:1872–1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2012;35(Suppl 1):S64–S71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziemer DC, Kolm P, Weintraub WS, et al. Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med 2010;152:770–777 [DOI] [PubMed] [Google Scholar]
- 8.Kumar PR, Bhansali A, Ravikiran M, et al. Utility of glycated hemoglobin in diagnosing type 2 diabetes mellitus: a community-based study. J Clin Endocrinol Metab 2010;95:2832–2835 [DOI] [PubMed] [Google Scholar]
- 9.Selvin E, Steffes MW, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL. Racial differences in glycemic markers: a cross-sectional analysis of community-based data. Ann Intern Med 2011;154:303–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nowicka P, Santoro N, Liu H, et al. Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 2011;34:1306–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care 2010;33:562–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 13.Genuth S, Alberti KG, Bennett P, et al. ; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003;26:3160–3167 [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Gregg EW, Williamson DF, et al. A1C level and future risk of diabetes: a systematic review. Diabetes Care 2010;33:1665–1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Griffin SJ, Borch-Johnsen K, Davies MJ, et al. Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 2011;378:156–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahn R, Alperin P, Eddy D, et al. Age at initiation and frequency of screening to detect type 2 diabetes: a cost-effectiveness analysis. Lancet 2010;375:1365–1374 [DOI] [PubMed] [Google Scholar]
- 18.Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV. Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care 2011;34:1741–1748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheehy A, Pandhi N, Coursin DB, et al. Minority status and diabetes screening in an ambulatory population. Diabetes Care 2011;34:1289–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tuomilehto J, Lindström J, Eriksson JG, et al. ; Finnish Diabetes Prevention Study Group Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–1350 [DOI] [PubMed] [Google Scholar]
- 22.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997;20:537–544 [DOI] [PubMed] [Google Scholar]
- 23.Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic women. Diabetes 2002;51:2796–2803 [DOI] [PubMed] [Google Scholar]
- 24.Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M; STOP-NIDDM Trail Research Group Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 2002;359:2072–2077 [DOI] [PubMed] [Google Scholar]
- 25.Gerstein HC, Yusuf S, Bosch J, et al. ; DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 2006;368:1096–1105 [DOI] [PubMed] [Google Scholar]
- 26.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V; Indian Diabetes Prevention Programme (IDPP) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49:289–297 [DOI] [PubMed] [Google Scholar]
- 27.Johnson SL, Tabaei BP, Herman WH. The efficacy and cost of alternative strategies for systematic screening for type 2 diabetes in the U.S. population 45-74 years of age. Diabetes Care 2005;28:307–311 [DOI] [PubMed] [Google Scholar]
- 28.Dabelea D, D'Agostino RB, Jr, Mayer-Davis EJ, et al. ; SEARCH for Diabetes in Youth Study Group Testing the accelerator hypothesis: body size, beta-cell function, and age at onset of type 1 (autoimmune) diabetes. Diabetes Care 2006;29:290–294 [DOI] [PubMed] [Google Scholar]
- 29.Liese AD, D'Agostino RB, Jr, Hamman RF, et al. ; SEARCH for Diabetes in Youth Study Group The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics 2006;118:1510–1518 [DOI] [PubMed] [Google Scholar]
- 30.American Diabetes Association Type 2 diabetes in children and adolescents. Diabetes Care 2000;23:381–389 [DOI] [PubMed] [Google Scholar]
- 31.Lawrence JM, Contreras R, Chen W, Sacks DA. Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999-2005. Diabetes Care 2008;31:899–904 [DOI] [PubMed] [Google Scholar]
- 32.Metzger BE, Lowe LP, Dyer AR, et al. ; HAPO Study Cooperative Research Group Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:1991–2002 [DOI] [PubMed] [Google Scholar]
- 33.Metzger BE, Gabbe SG, Persson B, et al. ; International Association of Diabetes and Pregnancy Study Groups Consensus Panel International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Sullivan EP, Avalos G, O'Reilly M, Dennedy MC, Gaffney G, Dunne F; Atlantic DIP collaborators Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 2011;54:1670–1675 [DOI] [PubMed] [Google Scholar]
- 35.Lapolla A, Dalfrà MG, Ragazzi E, De Cata AP, Fedele D. New International Association of the Diabetes and Pregnancy Study Groups (IADPSG) recommendations for diagnosing gestational diabetes compared with former criteria: a retrospective study on pregnancy outcome. Diabet Med 2011;28:1074–1077 [DOI] [PubMed] [Google Scholar]
- 36.Landon MB, Spong CY, Thom E, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009;361:1339–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS; Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005;352:2477–2486 [DOI] [PubMed] [Google Scholar]
- 38.Committee on Obstetric Practice Committee opinion no. 504: screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol 2011;118:751–753 [DOI] [PubMed] [Google Scholar]
- 39.Kim C, Herman WH, Cheung NW, Gunderson EP, Richardson C. Comparison of hemoglobin A1c with fasting plasma glucose and 2-h postchallenge glucose for risk stratification among women with recent gestational diabetes mellitus. Diabetes Care 2011;34:1949–1951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 2002;25:1862–1868 [DOI] [PubMed] [Google Scholar]
- 41.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008;371:1783–1789 [DOI] [PubMed] [Google Scholar]
- 42.Lindström J, Ilanne-Parikka P, Peltonen M, et al. ; Finnish Diabetes Prevention Study Group Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–1679 [DOI] [PubMed] [Google Scholar]
- 43.Knowler WC, Fowler SE, Hamman RF, et al. ; Diabetes Prevention Program Research Group 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Herman WH, Hoerger TJ, Brandle M, et al. ; Diabetes Prevention Program Research Group The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 2005;142:323–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herman WH, Edelsrein SL, Ratner RE, et al. The 10-year cost-effectiveness of lifestyle intervention or metformin for primary prevention of type 2 diabetes mellitus; an intent-to-treat analysis of diabetes prevention. Presented at 71st Scientific Sessions of the American Diabetes Association, 28 June 2011, San Diego, California [Google Scholar]
- 46.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med 2008;35:357–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nathan DM, Davidson MB, DeFronzo RA, et al. ; American Diabetes Association Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 2007;30:753–759 [DOI] [PubMed] [Google Scholar]
- 48.DREAM Trial Investigators Incidence of diabetes following ramipril or rosiglitazone withdrawal. Diabetes Care 2011;34:1265–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ratner RE, Christophi CA, Metzger BE, et al. ; Diabetes Prevention Program Research Group Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab 2008;93:4774–4779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ziegler R, Heidtmann B, Hilgard D, Hofer S, Rosenbauer J, Holl R; DPV-Wiss-Initiative Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes 2011;12:11–17 [DOI] [PubMed] [Google Scholar]
- 51.Welschen LM, Bloemendal E, Nijpels G, et al. Self-monitoring of blood glucose in patients with type 2 diabetes who are not using insulin: a systematic review. Diabetes Care 2005;28:1510–1517 [DOI] [PubMed] [Google Scholar]
- 52.Farmer A, Wade A, Goyder E, et al. Impact of self monitoring of blood glucose in the management of patients with non-insulin treated diabetes: open parallel group randomised trial. BMJ 2007;335:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O'Kane MJ, Bunting B, Copeland M, Coates VE; ESMON study group Efficacy of self monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): randomised controlled trial. BMJ 2008;336:1174–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simon J, Gray A, Clarke P, Wade A, Neil A, Farmer A; Diabetes Glycaemic Education and Monitoring Trial Group Cost effectiveness of self monitoring of blood glucose in patients with non-insulin treated type 2 diabetes: economic evaluation of data from the DiGEM trial. BMJ 2008;336:1177–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sacks DB, Bruns DE, Goldstein DE, Maclaren NK, McDonald JM, Parrott M. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 2002;48:436–472 [PubMed] [Google Scholar]
- 56.Tamborlane WV, Beck RW, Bode BW, et al. ; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 57.Beck RW, Hirsch IB, Laffel L, et al. ; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group The effect of continuous glucose monitoring in well-controlled type 1 diabetes. Diabetes Care 2009;32:1378–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Battelino T, Phillip M, Bratina N, Nimri R, Oskarsson P, Bolinder J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care 2011;34:795–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bergenstal RM, Tamborlane WV, Ahmann A, et al. ; STAR 3 Study Group Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med 2010;363:311–320 [DOI] [PubMed] [Google Scholar]
- 60.Slover RH, Welsh JB, Criego A, Weinzimer SA, Willi SM, Wood MA, Tamborlane WV: Effectiveness of sensor-augmented pump therapy in children and adolescents with type 1 diabetes in the STAR 3 study. Pediatr Diabetes. 3 July 2011 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 61.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 62.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cagliero E, Levina EV, Nathan DM. Immediate feedback of HbA1c levels improves glycemic control in type 1 and insulin-treated type 2 diabetic patients. Diabetes Care 1999;22:1785–1789 [DOI] [PubMed] [Google Scholar]
- 64.Miller CD, Barnes CS, Phillips LS, et al. Rapid A1c availability improves clinical decision-making in an urban primary care clinic. Diabetes Care 2003;26:1158–1163 [DOI] [PubMed] [Google Scholar]
- 65.Al-Ansary L, Farmer A, Hirst J, et al. Point-of-care testing for Hb A1c in the management of diabetes: a systematic review and metaanalysis. Clin Chem 2011;57:568–576 [DOI] [PubMed] [Google Scholar]
- 66.Gialamas A, St John A, Laurence CO, Bubner TK; PoCT Management Committee Point-of-care testing for patients with diabetes, hyperlipidaemia or coagulation disorders in the general practice setting: a systematic review. Fam Pract 2010;27:17–24 [DOI] [PubMed] [Google Scholar]
- 67.Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ; A1c-Derived Average Glucose Study Group Translating the A1C assay into estimated average glucose values. Diabetes Care 2008;31:1473–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rohlfing CL, Wiedmeyer HM, Little RR, England JD, Tennill A, Goldstein DE. Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA(1c) in the Diabetes Control and Complications Trial. Diabetes Care 2002;25:275–278 [DOI] [PubMed] [Google Scholar]
- 69.Wilson DM, Kollman; Diabetes Research in Children Network (DirecNet) Study Group Relationship of A1C to glucose concentrations in children with type 1 diabetes: assessments by high-frequency glucose determinations by sensors. Diabetes Care 2008;31:381–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med 2000;342:381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martin CL, Albers J, Herman WH, et al. ; DCCT/EDIC Research Group Neuropathy among the diabetes control and complications trial cohort 8 years after trial completion. Diabetes Care 2006;29:340–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 1995;28:103–117 [DOI] [PubMed] [Google Scholar]
- 73.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865 [PubMed] [Google Scholar]
- 74.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 75.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577–1589 [DOI] [PubMed] [Google Scholar]
- 76.Duckworth W, Abraira C, Moritz T, et al. ; VADT Investigators Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 77.Moritz T, Duckworth W, Abraira C. Veterans Affairs diabetes trial—corrections. N Engl J Med 2009;361:1024–1025 [DOI] [PubMed] [Google Scholar]
- 78.Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 79.Ismail-Beigi F, Craven T, Banerji MA, et al. ; ACCORD trial group Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet 2010;376:419–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chew EY, Ambrosius WT, Davis MD, et al. ; ACCORD Study Group; ACCORD Eye Study Group Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med 2010;363:233–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gerstein HC, Miller ME, Byington RP, et al. ; Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nathan DM, Cleary PA, Backlund JY, et al. ; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nathan DM, Zinman B, Cleary PA, et al. ; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983-2005). Arch Intern Med 2009;169:1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Skyler JS, Bergenstal R, Bonow RO, et al. ; American Diabetes Association; American College of Cardiology Foundation; American Heart Association Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Diabetes Care 2009;32:187–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gerstein HC, Miller ME, Genuth S, et al. ; ACCORD Study Group Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med 2011;364:818–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Riddle MC, Ambrosius WT, Brillon DJ, et al. ; Action to Control Cardiovascular Risk in Diabetes Investigators Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care 2010;33:983–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ 2010;340:b4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reaven PD, Moritz TE, Schwenke DC, Anderson RJ, Criqui M, Detrano R, Emanuele N, Kayshap M, Marks J, Mudaliar S, Rao RH, Shah JH, Goldman S, Reda DJ, McCarren M, Abraira C, Duckworth W: Intensive glucose lowering therapy reduces cardiovascular disease events in VADT participants with lower calcified coronary atherosclerosis. Diabetes 2009;58:2642–2648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Turnbull FM, Abraira C, Anderson RJ, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 2009;52:2288–2298 [DOI] [PubMed] [Google Scholar]
- 89a.Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med 2011;154:554–559 [DOI] [PubMed] [Google Scholar]
- 90.American Diabetes Association Postprandial blood glucose. Diabetes Care 2001;24:775–778 [DOI] [PubMed] [Google Scholar]
- 91.Ceriello A, Taboga C, Tonutti L, et al. Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation 2002;106:1211–1218 [DOI] [PubMed] [Google Scholar]
- 92.Raz I, Wilson PW, Strojek K, et al. Effects of prandial versus fasting glycemia on cardiovascular outcomes in type 2 diabetes: the HEART2D trial. Diabetes Care 2009;32:381–386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 2007;30(Suppl 2):S251–S260 [DOI] [PubMed] [Google Scholar]
- 94.Kitzmiller JL, Block JM, Brown FM, et al. Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 2008;31:1060–1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA 2003;289:2254–2264 [DOI] [PubMed] [Google Scholar]
- 96.Rosenstock J, Dailey G, Massi-Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine: a meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005;28:950–955 [DOI] [PubMed] [Google Scholar]
- 97.Mooradian AD, Bernbaum M, Albert SG. Narrative review: a rational approach to starting insulin therapy. Ann Intern Med 2006;145:125–134 [DOI] [PubMed] [Google Scholar]
- 98.Nathan DM, Buse JB, Davidson MB, et al. ; American Diabetes Association; European Association for Study of Diabetes Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009;32:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98a.Bennett WL, Maruthur NM, Singh S, et al. Comparative effectiveness and safety of medications for type 2 diabetes: an update including new drugs and 2-drug combinations. Ann Intern Med 2011;154:602–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Agency for Healthcare Research and Qualtiy Adverse Events after Hospital Discharge [article online]. Available from http://psnet.ahrq.gov/primer.aspx?primerID=11. Accessed 17 August 2010
- 100.Bantle JP, Wylie-Rosett J, Albright AL, et al. ; American Diabetes Association Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 2008;31(Suppl 1):S61–S78 [DOI] [PubMed] [Google Scholar]
- 101.DAFNE Study Group Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325:746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Franz MJ, Monk A, Barry B, et al. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J Am Diet Assoc 1995;95:1009–1017 [DOI] [PubMed] [Google Scholar]
- 103.Goldhaber-Fiebert JD, Goldhaber-Fiebert SN, Tristán ML, Nathan DM. Randomized controlled community-based nutrition and exercise intervention improves glycemia and cardiovascular risk factors in type 2 diabetic patients in rural Costa Rica. Diabetes Care 2003;26:24–29 [DOI] [PubMed] [Google Scholar]
- 104.Lemon CC, Lacey K, Lohse B, Hubacher DO, Klawitter B, Palta M. Outcomes monitoring of health, behavior, and quality of life after nutrition intervention in adults with type 2 diabetes. J Am Diet Assoc 2004;104:1805–1815 [DOI] [PubMed] [Google Scholar]
- 105.Miller CK, Edwards L, Kissling G, Sanville L. Nutrition education improves metabolic outcomes among older adults with diabetes mellitus: results from a randomized controlled trial. Prev Med 2002;34:252–259 [DOI] [PubMed] [Google Scholar]
- 106.Wilson C, Brown T, Acton K, Gilliland S. Effects of clinical nutrition education and educator discipline on glycemic control outcomes in the Indian health service. Diabetes Care 2003;26:2500–2504 [DOI] [PubMed] [Google Scholar]
- 107.Graber AL, Elasy TA, Quinn D, Wolff K, Brown A. Improving glycemic control in adults with diabetes mellitus: shared responsibility in primary care practices. South Med J 2002;95:684–690 [PubMed] [Google Scholar]
- 108.Gaetke LM, Stuart MA, Truszczynska H. A single nutrition counseling session with a registered dietitian improves short-term clinical outcomes for rural Kentucky patients with chronic diseases. J Am Diet Assoc 2006;106:109–112 [DOI] [PubMed] [Google Scholar]
- 109.Van Horn L, McCoin M, Kris-Etherton PM, et al. The evidence for dietary prevention and treatment of cardiovascular disease. J Am Diet Assoc 2008;108:287–331 [DOI] [PubMed] [Google Scholar]
- 110.Appel LJ, Moore TJ, Obarzanek E, et al. ; DASH Collaborative Research Group A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–1124 [DOI] [PubMed] [Google Scholar]
- 111.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107:1755–1767 [DOI] [PubMed] [Google Scholar]
- 112.Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003;348:2082–2090 [DOI] [PubMed] [Google Scholar]
- 113.Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med 2004;140:778–785 [DOI] [PubMed] [Google Scholar]
- 114.Foster GD, Wyatt HR, Hill JO, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med 2010;153:147–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shai I, Schwarzfuchs D, Henkin Y, et al. ; Dietary Intervention Randomized Controlled Trial (DIRECT) Group Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229–241 [DOI] [PubMed] [Google Scholar]
- 116.Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:285–293 [DOI] [PubMed] [Google Scholar]
- 117.Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of weight-loss interventions in adults with pre-diabetes: a review. Am J Prev Med 2005;28:126–139 [DOI] [PubMed] [Google Scholar]
- 118.Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J, Estruch R, Covas MI, Corella D, Aros F, Ruiz-Gutierrez V, Ros E: Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus Nutrition Intervention Randomized Trial. Diabetes Care 2010;34:14-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 2010;33:2477–2483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Klein S, Sheard NF, Pi-Sunyer X, et al. ; American Diabetes Association; North American Association for the Study of Obesity; American Society for Clinical Nutrition Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Diabetes Care 2004;27:2067–2073 [DOI] [PubMed] [Google Scholar]
- 121.Norris SL, Zhang X, Avenell A, et al. Efficacy of pharmacotherapy for weight loss in adults with type 2 diabetes mellitus: a meta-analysis. Arch Intern Med 2004;164:1395–1404 [DOI] [PubMed] [Google Scholar]
- 122.Wolf AM, Conaway MR, Crowther JQ, et al. ; Improving Control with Activity and Nutrition (ICAN) Study Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study. Diabetes Care 2004;27:1570–1576 [DOI] [PubMed] [Google Scholar]
- 123.Manning RM, Jung RT, Leese GP, Newton RW. The comparison of four weight reduction strategies aimed at overweight patients with diabetes mellitus: four-year follow-up. Diabet Med 1998;15:497–502 [DOI] [PubMed] [Google Scholar]
- 124.Pi-Sunyer X, Blackburn G, Brancati FL, et al. ; Look AHEAD Research Group Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 2007;30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wing RR, Look AHEAD Research Group Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med 2010;170:1566–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Esposito K, Maiorino MI, Ciotola M, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009;151:306–314 [DOI] [PubMed] [Google Scholar]
- 127.Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care 2006;29:1777–1783 [DOI] [PubMed] [Google Scholar]
- 128.Turner-McGrievy GM, Barnard ND, Cohen J, Jenkins DJ, Gloede L, Green AA. Changes in nutrient intake and dietary quality among participants with type 2 diabetes following a low-fat vegan diet or a conventional diabetes diet for 22 weeks. J Am Diet Assoc 2008;108:1636–1645 [DOI] [PubMed] [Google Scholar]
- 129.Institute of Medicine DIetary Reference Intakes: Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, D.C., National Academies Press, 2002 [DOI] [PubMed] [Google Scholar]
- 130.Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2002;25:148–198 [DOI] [PubMed] [Google Scholar]
- 131.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care 2001;24:561–587 [DOI] [PubMed] [Google Scholar]
- 132.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159–1171 [DOI] [PubMed] [Google Scholar]
- 133.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ 2003;29:488–501 [DOI] [PubMed] [Google Scholar]
- 134.Steed L, Cooke D, Newman S. A systematic review of psychosocial outcomes following education, self-management and psychological interventions in diabetes mellitus. Patient Educ Couns 2003;51:5–15 [DOI] [PubMed] [Google Scholar]
- 135.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns 2004;52:97–105 [DOI] [PubMed] [Google Scholar]
- 136.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med 2004;164:1641–1649 [DOI] [PubMed] [Google Scholar]
- 137.Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self-management education. Diabetes Care 2007;30:1630–1637 [DOI] [PubMed] [Google Scholar]
- 138.Mulcahy K, Maryniuk M, Peeples M, Peyrot M, Tomky D, Weaver T, Yarborough P: Diabetes self-management education core outcomes measures. Diabetes Educ 2003;29:768–784 [DOI] [PubMed] [Google Scholar]
- 139.Glasgow RE, Peeples M, Skovlund SE. Where is the patient in diabetes performance measures? The case for including patient-centered and self-management measures. Diabetes Care 2008;31:1046–1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Barker JM, Goehrig SH, Barriga K, et al. ; DAISY study Clinical characteristics of children diagnosed with type 1 diabetes through intensive screening and follow-up. Diabetes Care 2004;27:1399–1404 [DOI] [PubMed] [Google Scholar]
- 141.Heinrich ESNCadVNK Self-management interventions for type 2 diabetes: a systematic review. Eur Diabetes Nurs 2010;7:71–76 [Google Scholar]
- 142.Cochran J, Conn VS. Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes Educ 2008;34:815–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ 2007;33:1080–1103; discussion 1104–1106 [DOI] [PubMed] [Google Scholar]
- 144.Robbins JM, Thatcher GE, Webb DA, Valdmanis VG. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care 2008;31:655–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Polonsky WH, Earles J, Smith S, et al. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care 2003;26:3048–3053 [DOI] [PubMed] [Google Scholar]
- 146.Anderson RM, Funnell MM, Nwankwo R, Gillard ML, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethn Dis 2005;15:671–678 [PubMed] [Google Scholar]
- 147.Brown SA, Blozis SA, Kouzekanani K, Garcia AA, Winchell M, Hanis CL. Dosage effects of diabetes self-management education for Mexican Americans: the Starr County Border Health Initiative. Diabetes Care 2005;28:527–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Piatt GA, Anderson RM, Brooks MM, et al. 3-year follow-up of clinical and behavioral improvements following a multifaceted diabetes care intervention: results of a randomized controlled trial. Diabetes Educ 2010;36:301–309 [DOI] [PubMed] [Google Scholar]
- 149.Tang TS, Funnell MM, Brown MB, Kurlander JE. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns 2010;79:178–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev 2001. (1):CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29:1675–1688 [DOI] [PubMed] [Google Scholar]
- 152.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 2008. (3):CD006424. [DOI] [PubMed] [Google Scholar]
- 153.Sarkisian CA, Brown AF, Norris KC, Wintz RL, Mangione CM. A systematic review of diabetes self-care interventions for older, African American, or Latino adults. Diabetes Educ 2003;29:467–479 [DOI] [PubMed] [Google Scholar]
- 154.Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005;143:427–438 [DOI] [PubMed] [Google Scholar]
- 155.Piette JD, Glasgow RE. Strategies for improving behavioral and health outcomes among people with diabetes: self managemnt education. In Evidence-Based Diabetes Care. Gerstein HC, Hayes RB, Eds. Ontario, Canada, BC Decker, 2000 [Google Scholar]
- 156.Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes: a conceptual review. Diabetes Care 2007;30:2433–2440 [DOI] [PubMed] [Google Scholar]
- 157.Anderson DR, Christison-Legay J, Proctor-Gray E. Self-management goal setting in a community health center: the impact of goal attainment on diabetes outcomes. Diabetes Spectrum 2010;23:97–106 [Google Scholar]
- 158.Rickheim PL, Weaver TW, Flader JL, Kendall DM. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care 2002;25:269–274 [DOI] [PubMed] [Google Scholar]
- 159.Trento M, Passera P, Borgo E, et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care 2004;27:670–675 [DOI] [PubMed] [Google Scholar]
- 160.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2005. (2):CD003417. [DOI] [PubMed] [Google Scholar]
- 161.Duke SA, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2009. (1):CD005268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med 2010;153:507–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract 2010;27(Suppl 1):i23–i32 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 164.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev 2007. (4):CD005108. [DOI] [PubMed] [Google Scholar]
- 165.Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med 2006;23:544–556 [DOI] [PubMed] [Google Scholar]
- 166.Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ 2009;35:752–760 [DOI] [PubMed] [Google Scholar]
- 167.Duncan I, Ahmed T, Li QE, et al. Assessing the value of the diabetes educator. Diabetes Educ 2011;37:638–657 [DOI] [PubMed] [Google Scholar]
- 168.Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 2001;286:1218–1227 [DOI] [PubMed] [Google Scholar]
- 169.Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in Type 2 diabetes mellitus. Diabetologia 2003;46:1071–1081 [DOI] [PubMed] [Google Scholar]
- 170.Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes. The American Collegoe of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care 2010;33:2692–2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.U.S.Department of Health and Human Services 2008 Physical Activity Guidelines for Americans [article online], 2008. Available from http://www.health.gov/paguidelines/guidelines/default.aspx. Accessed December 2010
- 172.Cauza E, Hanusch-Enserer U, Strasser B, et al. The relative benefits of endurance and strength training on the metabolic factors and muscle function of people with type 2 diabetes mellitus. Arch Phys Med Rehabil 2005;86:1527–1533 [DOI] [PubMed] [Google Scholar]
- 173.Dunstan DW, Daly RM, Owen N, et al. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care 2002;25:1729–1736 [DOI] [PubMed] [Google Scholar]
- 174.Castaneda C, Layne JE, Munoz-Orians L, et al. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care 2002;25:2335–2341 [DOI] [PubMed] [Google Scholar]
- 175.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care 2004;27:2518–2539 [DOI] [PubMed] [Google Scholar]
- 176.Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA 2010;304:2253–2262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ; ADA Screening for coronary artery disease in patients with diabetes. Diabetes Care 2007;30:2729–2736 [DOI] [PubMed] [Google Scholar]
- 178.Berger M, Berchtold P, Cüppers HJ, et al. Metabolic and hormonal effects of muscular exercise in juvenile type diabetics. Diabetologia 1977;13:355–365 [DOI] [PubMed] [Google Scholar]
- 179.Aiello LP, Wong J, Cavallerano J, Bursell SE, Aiello LM. Retinopathy. In Handbook of Exercise in Diabetes. 2nd ed Ruderman N, Devlin JT, Kriska A, Eds. Alexandria, VA, American Diabetes Association, 2002, p. 401–413 [Google Scholar]
- 180.Lemaster JW, Reiber GE, Smith DG, Heagerty PJ, Wallace C. Daily weight-bearing activity does not increase the risk of diabetic foot ulcers. Med Sci Sports Exerc 2003;35:1093–1099 [DOI] [PubMed] [Google Scholar]
- 181.Vinik A, Erbas T. Neuropathy. In Handbook of Exercise in Diabetes. 2nd ed Ruderman N, Devlin JT, Kriska A, Eds. Alexandria, VA, American Diabetes Association, 2002, p. 463–496 [Google Scholar]
- 182.Wackers FJ, Young LH, Inzucchi SE, et al. ; Detection of Ischemia in Asymptomatic Diabetics Investigators Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care 2004;27:1954–1961 [DOI] [PubMed] [Google Scholar]
- 183.Valensi P, Sachs RN, Harfouche B, et al. Predictive value of cardiac autonomic neuropathy in diabetic patients with or without silent myocardial ischemia. Diabetes Care 2001;24:339–343 [DOI] [PubMed] [Google Scholar]
- 184.Mogensen CE. Nephropathy. In Handbook of Exercise in Diabetes. 2nd ed Ruderman N, Devlin JT, Kriska A, Eds. Alexandria, VA, American Diabetes Association, 2002, p. 433–449 [Google Scholar]
- 185.Anderson RJ, Grigsby AB, Freedland KE, et al. Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med 2002;32:235–247 [DOI] [PubMed] [Google Scholar]
- 186.Delahanty LM, Grant RW, Wittenberg E, et al. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with Type 2 diabetes. Diabet Med 2007;24:48–54 [DOI] [PubMed] [Google Scholar]
- 187.American Diabetes Association Psychosocial factors affecting adherence, quality of life, and well-being: helping patients cope. In Medical Management of Type 1 Diabetes. 5th ed Kaufman FR, Alexandria, VA, American Diabetes Association, 2008, p. 173–193 [Google Scholar]
- 188.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001;24:1069–1078 [DOI] [PubMed] [Google Scholar]
- 189.Harkness E, Macdonald W, Valderas J, Coventry P, Gask L, Bower P. Identifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:926–930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care 2007;30:542–548 [DOI] [PubMed] [Google Scholar]
- 191.Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care 2010;33:1034–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Gary TL, Safford MM, Gerzoff RB, et al. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 2008;31:273–278 [DOI] [PubMed] [Google Scholar]
- 193.Katon W, Fan MY, Unützer J, Taylor J, Pincus H, Schoenbaum M. Depression and diabetes: a potentially lethal combination. J Gen Intern Med 2008;23:1571–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles G, Kahn HS. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol 2005;161:652–660 [DOI] [PubMed] [Google Scholar]
- 195.Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol 2001;57:457–478 [DOI] [PubMed] [Google Scholar]
- 196.Young-Hyman DL, Davis CL. Disordered eating behavior in individuals with diabetes: importance of context, evaluation, and classification. Diabetes Care 2010;33:683–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Blonde L, Merilainen M, Karwe V, Raskin P; TITRATE Study Group Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets - the TITRATE study. Diabetes Obes Metab 2009;11:623–631 [DOI] [PubMed] [Google Scholar]
- 198.Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 2009;32:1335–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Cryer PE. Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. Diabetologia 2002;45:937–948 [DOI] [PubMed] [Google Scholar]
- 200.Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP, Jr, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA 2009;301:1565–1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Jacobson AM, Musen G, Ryan CM, et al. ; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med 2007;356:1842–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2004;350:2272–2279 [DOI] [PubMed] [Google Scholar]
- 203.Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009;122:248–256, e5 [DOI] [PubMed] [Google Scholar]
- 204.Dixon JB, O'Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008;299:316–323 [DOI] [PubMed] [Google Scholar]
- 205.Hall TC, Pellen MG, Sedman PC, Jain PK. Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity. Obes Surg 2010;20:1245–1250 [DOI] [PubMed] [Google Scholar]
- 206.Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 2007;142:621–632; discussion 632–635 [DOI] [PubMed] [Google Scholar]
- 207.Sjöström L, Narbro K, Sjöström CD, et al. ; Swedish Obese Subjects Study Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741–752 [DOI] [PubMed] [Google Scholar]
- 208.Hoerger TJ, Zhang P, Segel JE, Kahn HS, Barker LE, Couper S. Cost-effectiveness of bariatric surgery for severely obese adults with diabetes. Diabetes Care 2010;33:1933–1939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Makary MA, Clark JM, Shore AD, et al. Medication utilization and annual health care costs in patients with type 2 diabetes mellitus before and after bariatric surgery. Arch Surg 2010;145:726–731 [DOI] [PubMed] [Google Scholar]
- 210.Keating CL, Dixon JB, Moodie ML, Peeters A, Playfair J, O'Brien PE. Cost-efficacy of surgically induced weight loss for the management of type 2 diabetes: a randomized controlled trial. Diabetes Care 2009;32:580–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Maciejewski ML, Livingston EH, Smith VA, et al. Survival among high-risk patients after bariatric surgery. JAMA 2011;305:2419–2426 [DOI] [PubMed] [Google Scholar]
- 212.Himpens J, Cadière GB, Bazi M, Vouche M, Cadière B, Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg 2011;146:802–807 [DOI] [PubMed] [Google Scholar]
- 213.Smith SA, Poland GA. Use of influenza and pneumococcal vaccines in people with diabetes. Diabetes Care 2000;23:95–108 [DOI] [PubMed] [Google Scholar]
- 214.Colquhoun AJ, Nicholson KG, Botha JL, Raymond NT. Effectiveness of influenza vaccine in reducing hospital admissions in people with diabetes. Epidemiol Infect 1997;119:335–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Bridges CB, Fukuda K, Uyeki TM, Cox NJ, Singleton JA; Centers for Disease Control and Prevention, Advisory Committee on Immunization Practices Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2002;51(RR-3):1–31 [PubMed] [Google Scholar]
- 216.Buse JB, Ginsberg HN, Bakris GL, et al. ; American Heart Association; American Diabetes Association Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2007;30:162–172 [DOI] [PubMed] [Google Scholar]
- 217.Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–591 [DOI] [PubMed] [Google Scholar]
- 218.Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999-2008. Diabetes Care 2011;34:1337–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Chobanian AV, Bakris GL, Black HR, et al. ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 220.Bobrie G, Genès N, Vaur L, et al. Is “isolated home” hypertension as opposed to “isolated office” hypertension a sign of greater cardiovascular risk? Arch Intern Med 2001;161:2205–2211 [DOI] [PubMed] [Google Scholar]
- 221.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation 2005;111:1777–1783 [DOI] [PubMed] [Google Scholar]
- 222.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–1913 [DOI] [PubMed] [Google Scholar]
- 223.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993;16:434–444 [DOI] [PubMed] [Google Scholar]
- 224.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 225.Hansson L, Zanchetti A, Carruthers SG, et al. ; HOT Study Group Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998;351:1755–1762 [DOI] [PubMed] [Google Scholar]
- 226.Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Cushman WC, Evans GW, Byington RP, et al. ; ACCORD Study Group Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 2007;370:829–840 [DOI] [PubMed] [Google Scholar]
- 229.Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010;304:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Sacks FM, Svetkey LP, Vollmer WM, et al. ; DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10 [DOI] [PubMed] [Google Scholar]
- 231.Tatti P, Pahor M, Byington RP, et al. Outcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM. Diabetes Care 1998;21:597–603 [DOI] [PubMed] [Google Scholar]
- 232.Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med 1998;338:645–652 [DOI] [PubMed] [Google Scholar]
- 233.Schrier RW, Estacio RO, Mehler PS, Hiatt WR. Appropriate blood pressure control in hypertensive and normotensive type 2 diabetes mellitus: a summary of the ABCD trial. Nat Clin Pract Nephrol 2007;3:428–438 [DOI] [PubMed] [Google Scholar]
- 234.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981–2997 [DOI] [PubMed] [Google Scholar]
- 235.Psaty BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA 1997;277:739–745 [PubMed] [Google Scholar]
- 236.Heart Outcomes Prevention Evaluation Study Investigators Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 2000;355:253–259 [PubMed] [Google Scholar]
- 237.McMurray JJ, Ostergren J, Swedberg K, et al. ; CHARM Investigators and Committees Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet 2003;362:767–771 [DOI] [PubMed] [Google Scholar]
- 238.Pfeffer MA, Swedberg K, Granger CB, et al. ; CHARM Investigators and Committees Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet 2003;362:759–766 [DOI] [PubMed] [Google Scholar]
- 239.Granger CB, McMurray JJ, Yusuf S, et al. ; CHARM Investigators and Committees Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet 2003;362:772–776 [DOI] [PubMed] [Google Scholar]
- 240.Lindholm LH, Ibsen H, Dahlöf B, et al. ; LIFE Study Group Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002;359:1004–1010 [DOI] [PubMed] [Google Scholar]
- 241.Berl T, Hunsicker LG, Lewis JB, et al. ; Irbesartan Diabetic Nephropathy Trial. Collaborative Study Group Cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial of patients with type 2 diabetes and overt nephropathy. Ann Intern Med 2003;138:542–549 [DOI] [PubMed] [Google Scholar]
- 242.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010;376:163–172 [DOI] [PubMed] [Google Scholar]
- 243.Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care 2011;34:1270–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Sibai BM. Treatment of hypertension in pregnant women. N Engl J Med 1996;335:257–265 [DOI] [PubMed] [Google Scholar]
- 245.Baigent C, Keech A, Kearney PM, et al. ; Cholesterol Treatment Trialists’ (CTT) Collaborators Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–1278 [DOI] [PubMed] [Google Scholar]
- 246.Pyŏrälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20:614–620 [DOI] [PubMed] [Google Scholar]
- 247.Collins R, Armitage J, Parish S, Sleigh P, Peto R; Heart Protection Study Collaborative Group MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003;361:2005–2016 [DOI] [PubMed] [Google Scholar]
- 248.Goldberg RB, Mellies MJ, Sacks FM, et al. ; The Care Investigators Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the cholesterol and recurrent events (CARE) trial. Circulation 1998;98:2513–2519 [DOI] [PubMed] [Google Scholar]
- 249.Shepherd J, Barter P, Carmena R, et al. Effect of lowering LDL cholesterol substantially below currently recommended levels in patients with coronary heart disease and diabetes: the Treating to New Targets (TNT) study. Diabetes Care 2006;29:1220–1226 [DOI] [PubMed] [Google Scholar]
- 250.Sever PS, Poulter NR, Dahlöf B, et al. Reduction in cardiovascular events with atorvastatin in 2,532 patients with type 2 diabetes: Anglo-Scandinavian Cardiac Outcomes Trial—lipid-lowering arm (ASCOT-LLA). Diabetes Care 2005;28:1151–1157 [DOI] [PubMed] [Google Scholar]
- 251.Knopp RH, d'Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN). Diabetes Care 2006;29:1478–1485 [DOI] [PubMed] [Google Scholar]
- 252.Colhoun HM, Betteridge DJ, Durrington PN, et al. ; CARDS investigators Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004;364:685–696 [DOI] [PubMed] [Google Scholar]
- 253.Singh IM, Shishehbor MH, Ansell BJ. High-density lipoprotein as a therapeutic target: a systematic review. JAMA 2007;298:786–798 [DOI] [PubMed] [Google Scholar]
- 254.Canner PL, Berge KG, Wenger NK, et al. Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin. J Am Coll Cardiol 1986;8:1245–1255 [DOI] [PubMed] [Google Scholar]
- 255.Rubins HB, Robins SJ, Collins D, et al. ; Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. N Engl J Med 1999;341:410–418 [DOI] [PubMed] [Google Scholar]
- 256.Frick MH, Elo O, Haapa K, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med 1987;317:1237–1245 [DOI] [PubMed] [Google Scholar]
- 257.Keech A, Simes RJ, Barter P, et al. ; FIELD study investigators Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005;366:1849–1861 [DOI] [PubMed] [Google Scholar]
- 258.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 259.Hayward RA, Hofer TP, Vijan S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med 2006;145:520–530 [DOI] [PubMed] [Google Scholar]
- 260.Cannon CP, Braunwald E, McCabe CH, et al. ; Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 Investigators Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004;350:1495–1504 [DOI] [PubMed] [Google Scholar]
- 261.de Lemos JA, Blazing MA, Wiviott SD, et al. ; A to Z Investigators Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 2004;292:1307–1316 [DOI] [PubMed] [Google Scholar]
- 262.Nissen SE, Tuzcu EM, Schoenhagen P, et al. ; REVERSAL Investigators Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 2004;291:1071–1080 [DOI] [PubMed] [Google Scholar]
- 263.Grundy SM, Cleeman JI, Merz CN, et al. ; National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004;110:227–239 [DOI] [PubMed] [Google Scholar]
- 264.Chasman DI, Posada D, Subrahmanyan L, Cook NR, Stanton VP, Jr, Ridker PM. Pharmacogenetic study of statin therapy and cholesterol reduction. JAMA 2004;291:2821–2827 [DOI] [PubMed] [Google Scholar]
- 265.Brunzell JD, Davidson M, Furberg CD, et al. ; American Diabetes Association; American College of Cardiology Foundation Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care 2008;31:811–822 [DOI] [PubMed] [Google Scholar]
- 266.Elam MB, Hunninghake DB, Davis KB, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: the ADMIT study: A randomized trial. Arterial Disease Multiple Intervention Trial. JAMA 2000;284:1263–1270 [DOI] [PubMed] [Google Scholar]
- 267.Grundy SM, Vega GL, McGovern ME, et al. ; Diabetes Multicenter Research Group Efficacy, safety, and tolerability of once-daily niacin for the treatment of dyslipidemia associated with type 2 diabetes: results of the assessment of diabetes control and evaluation of the efficacy of niaspan trial. Arch Intern Med 2002;162:1568–1576 [DOI] [PubMed] [Google Scholar]
- 268.Jones PH, Davidson MH. Reporting rate of rhabdomyolysis with fenofibrate + statin versus gemfibrozil + any statin. Am J Cardiol 2005;95:120–122 [DOI] [PubMed] [Google Scholar]
- 269.Ginsberg HN, Elam MB, Lovato LC, et al. ; ACCORD Study Group Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 2010;362:1563–1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Aim High Study Group Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med, 2011. E-pub. [DOI] [PubMed] [Google Scholar]
- 271.Baigent C, Blackwell L, Collins R, et al. ; Antithrombotic Trialists’ (ATT) Collaboration Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849–1860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Ogawa H, Nakayama M, Morimoto T, et al. ; Japanese Primary Prevention of Atherosclerosis With Aspirin for Diabetes (JPAD) Trial Investigators Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 2008;300:2134–2141 [DOI] [PubMed] [Google Scholar]
- 273.Belch J, MacCuish A, Campbell I, Cobbe S, Taylor R, Prescott R, Lee R, Bancroft J, MacEwan S, Shepherd J, Macfarlane P, Morris A, Jung R, Kelly C, Connacher A, Peden N, Jamieson A, Matthews D, Leese G, McKnight J, O'Brien I, Semple C, Petrie J, Gordon D, Pringle S, MacWalter R: The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 2008;337:a1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Pignone M, Earnshaw S, Tice JA, Pletcher MJ. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med 2006;144:326–336 [DOI] [PubMed] [Google Scholar]
- 275.Pignone M, Alberts MJ, Colwell JA, et al. ; American Diabetes Association; American Heart Association; American College of Cardiology Foundation Aspirin for primary prevention of cardiovascular events in people with diabetes: a position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Diabetes Care 2010;33:1395–1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Campbell CL, Smyth S, Montalescot G, Steinhubl SR. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA 2007;297:2018–2024 [DOI] [PubMed] [Google Scholar]
- 277.Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med 2007;357:2482–2494 [DOI] [PubMed] [Google Scholar]
- 278.Bhatt DL, Marso SP, Hirsch AT, Ringleb PA, Hacke W, Topol EJ. Amplified benefit of clopidogrel versus aspirin in patients with diabetes mellitus. Am J Cardiol 2002;90:625–628 [DOI] [PubMed] [Google Scholar]
- 279.Ranney L, Melvin C, Lux L, McClain E, Lohr KN. Systematic review: smoking cessation intervention strategies for adults and adults in special populations. Ann Intern Med 2006;145:845–856 [DOI] [PubMed] [Google Scholar]
- 280.Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol 2006;47:65–71 [DOI] [PubMed] [Google Scholar]
- 281.Boden WE, O'Rourke RA, Teo KK, et al. ; COURAGE Trial Research Group Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503–1516 [DOI] [PubMed] [Google Scholar]
- 282.Frye RL, August P, Brooks MM, et al. ; BARI 2D Study Group A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503–2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Wackers FJ, Chyun DA, Young LH, et al. ; Detection of Ischemia in Asymptomatic Diabetics (DIAD) Investigators Resolution of asymptomatic myocardial ischemia in patients with type 2 diabetes in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study. Diabetes Care 2007;30:2892–2898 [DOI] [PubMed] [Google Scholar]
- 284.Young LH, Wackers FJ, Chyun DA, et al. ; DIAD Investigators Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA 2009;301:1547–1555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Hadamitzky M, Hein F, Meyer T, et al. Prognostic value of coronary computed tomographic angiography in diabetic patients without known coronary artery disease. Diabetes Care 2010;33:1358–1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Elkeles RS, Godsland IF, Feher MD, et al. ; PREDICT Study Group Coronary calcium measurement improves prediction of cardiovascular events in asymptomatic patients with type 2 diabetes: the PREDICT study. Eur Heart J 2008;29:2244–2251 [DOI] [PubMed] [Google Scholar]
- 287.Choi EK, Chun EJ, Choi SI, et al. Assessment of subclinical coronary atherosclerosis in asymptomatic patients with type 2 diabetes mellitus with single photon emission computed tomography and coronary computed tomography angiography. Am J Cardiol 2009;104:890–896 [DOI] [PubMed] [Google Scholar]
- 288.Braunwald E, Domanski MJ, Fowler SE, et al. ; PEACE Trial Investigators Angiotensin-converting-enzyme inhibition in stable coronary artery disease. N Engl J Med 2004;351:2058–2068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Yusuf S, Teo K, Anderson C, et al. ; Telmisartan Randomised AssessmeNt Study in ACE iNtolerant subjects with cardiovascular Disease (TRANSCEND) Investigators Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomised controlled trial. Lancet 2008;372:1174–1183 [DOI] [PubMed] [Google Scholar]
- 290.Garg JP, Bakris GL. Microalbuminuria: marker of vascular dysfunction, risk factor for cardiovascular disease. Vasc Med 2002;7:35–43 [DOI] [PubMed] [Google Scholar]
- 291.Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 2004;110:32–35 [DOI] [PubMed] [Google Scholar]
- 292.Gall MA, Hougaard P, Borch-Johnsen K, Parving HH. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: prospective, observational study. BMJ 1997;314:783–788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Ravid M, Lang R, Rachmani R, Lishner M. Long-term renoprotective effect of angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus. A 7-year follow-up study. Arch Intern Med 1996;156:286–289 [PubMed] [Google Scholar]
- 294.Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med 1993;329:304–309 [DOI] [PubMed] [Google Scholar]
- 295.The Diabetes Control and Complications (DCCT) Research Group Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. Kidney Int 1995;47:1703–1720 [DOI] [PubMed] [Google Scholar]
- 296.Lewis EJ, Hunsicker LG, Bain RP, Rohde RD; The Collaborative Study Group The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med 1993;329:1456–1462 [DOI] [PubMed] [Google Scholar]
- 297.Laffel LM, McGill JB, Gans DJ; North American Microalbuminuria Study Group The beneficial effect of angiotensin-converting enzyme inhibition with captopril on diabetic nephropathy in normotensive IDDM patients with microalbuminuria. Am J Med 1995;99:497–504 [DOI] [PubMed] [Google Scholar]
- 298.Bakris GL, Williams M, Dworkin L, et al. ; National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis 2000;36:646–661 [DOI] [PubMed] [Google Scholar]
- 299.Remuzzi G, Macia M, Ruggenenti P. Prevention and treatment of diabetic renal disease in type 2 diabetes: the BENEDICT study. J Am Soc Nephrol 2006;17(Suppl 2):S90–S97 [DOI] [PubMed] [Google Scholar]
- 300.Haller H, Ito S, Izzo JL, Jr, et al. ; ROADMAP Trial Investigators Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N Engl J Med 2011;364:907–917 [DOI] [PubMed] [Google Scholar]
- 301.Bilous R, Chaturvedi N, Sjølie AK, et al. Effect of candesartan on microalbuminuria and albumin excretion rate in diabetes: three randomized trials. Ann Intern Med 2009;151:11–20, W3-4 [DOI] [PubMed] [Google Scholar]
- 302.Mauer M, Zinman B, Gardiner R, et al. Renal and retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med 2009;361:40–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Lewis EJ, Hunsicker LG, Clarke WR, et al. ; Collaborative Study Group Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001;345:851–860 [DOI] [PubMed] [Google Scholar]
- 304.Brenner BM, Cooper ME, de Zeeuw D, et al. ; RENAAL Study Investigators Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001;345:861–869 [DOI] [PubMed] [Google Scholar]
- 305.Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001;345:870–878 [DOI] [PubMed] [Google Scholar]
- 306.Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. ; INVEST Investigators A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA 2003;290:2805–2816 [DOI] [PubMed] [Google Scholar]
- 307.Bakris GL, Siomos M, Richardson D, et al. ; VAL-K Study Group ACE inhibition or angiotensin receptor blockade: impact on potassium in renal failure. Kidney Int 2000;58:2084–2092 [DOI] [PubMed] [Google Scholar]
- 308.Mogensen CE, Neldam S, Tikkanen I, et al. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ 2000;321:1440–1444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Schjoedt KJ, Jacobsen P, Rossing K, Boomsma F, Parving HH. Dual blockade of the renin-angiotensin-aldosterone system in diabetic nephropathy: the role of aldosterone. Horm Metab Res 2005;37(Suppl 1):4–8 [DOI] [PubMed] [Google Scholar]
- 310.Schjoedt KJ, Rossing K, Juhl TR, et al. Beneficial impact of spironolactone in diabetic nephropathy. Kidney Int 2005;68:2829–2836 [DOI] [PubMed] [Google Scholar]
- 311.Parving HH, Persson F, Lewis JB, Lewis EJ, Hollenberg NK; AVOID Study Investigators Aliskiren combined with losartan in type 2 diabetes and nephropathy. N Engl J Med 2008;358:2433–2446 [DOI] [PubMed] [Google Scholar]
- 312.Pijls LT, de Vries H, Donker AJ, van Eijk JT. The effect of protein restriction on albuminuria in patients with type 2 diabetes mellitus: a randomized trial. Nephrol Dial Transplant 1999;14:1445–1453 [DOI] [PubMed] [Google Scholar]
- 313.Pedrini MT, Levey AS, Lau J, Chalmers TC, Wang PH. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal diseases: a meta-analysis. Ann Intern Med 1996;124:627–632 [DOI] [PubMed] [Google Scholar]
- 314.Hansen HP, Tauber-Lassen E, Jensen BR, Parving HH. Effect of dietary protein restriction on prognosis in patients with diabetic nephropathy. Kidney Int 2002;62:220–228 [DOI] [PubMed] [Google Scholar]
- 315.Kasiske BL, Lakatua JD, Ma JZ, Louis TA. A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am J Kidney Dis 1998;31:954–961 [DOI] [PubMed] [Google Scholar]
- 316.Eknoyan G, Hostetter T, Bakris GL, et al. Proteinuria and other markers of chronic kidney disease: a position statement of the national kidney foundation (NKF) and the national institute of diabetes and digestive and kidney diseases (NIDDK). Am J Kidney Dis 2003;42:617–622 [DOI] [PubMed] [Google Scholar]
- 317.Levey AS, Coresh J, Balk E, et al. ; National Kidney Foundation National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137–147 [DOI] [PubMed] [Google Scholar]
- 318.Kramer H, Molitch ME. Screening for kidney disease in adults with diabetes. Diabetes Care 2005;28:1813–1816 [DOI] [PubMed] [Google Scholar]
- 319.Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 2003;289:3273–3277 [DOI] [PubMed] [Google Scholar]
- 320.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D; Modification of Diet in Renal Disease Study Group A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999;130:461–470 [DOI] [PubMed] [Google Scholar]
- 321.Rigalleau V, Lasseur C, Perlemoine C, et al. Estimation of glomerular filtration rate in diabetic subjects: Cockcroft formula or modification of Diet in Renal Disease study equation? Diabetes Care 2005;28:838–843 [DOI] [PubMed] [Google Scholar]
- 322.Levinsky NG. Specialist evaluation in chronic kidney disease: too little, too late. Ann Intern Med 2002;137:542–543 [DOI] [PubMed] [Google Scholar]
- 323.Klein R. Hyperglycemia and microvascular and macrovascular disease in diabetes. Diabetes Care 1995;18:258–268 [DOI] [PubMed] [Google Scholar]
- 324.Estacio RO, McFarling E, Biggerstaff S, Jeffers BW, Johnson D, Schrier RW. Overt albuminuria predicts diabetic retinopathy in Hispanics with NIDDM. Am J Kidney Dis 1998;31:947–953 [DOI] [PubMed] [Google Scholar]
- 325.Leske MC, Wu SY, Hennis A, et al. ; Barbados Eye Study Group Hyperglycemia, blood pressure, and the 9-year incidence of diabetic retinopathy: the Barbados Eye Studies. Ophthalmology 2005;112:799–805 [DOI] [PubMed] [Google Scholar]
- 326.Fong DS, Aiello LP, Ferris FL, 3rd, Klein R. Diabetic retinopathy. Diabetes Care 2004;27:2540–2553 [DOI] [PubMed] [Google Scholar]
- 327.Diabetes Control and Complications Trial Research Group Effect of pregnancy on microvascular complications in the diabetes control and complications trial. Diabetes Care 2000;23:1084–1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.The Diabetic Retinopathy Study Research Group Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol 1976;81:383–396 [DOI] [PubMed] [Google Scholar]
- 329.ETDRS Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol 1985;103:1796–1806 [PubMed] [Google Scholar]
- 330.Boyer DS. Ranibizumab (anti-VEGF) for vision loss due to diabetic macular edema: reslts of two phase III randomized trials. 2011
- 331.Agardh E, Tababat-Khani P. Adopting 3-year screening intervals for sight-threatening retinal vascular lesions in type 2 diabetic subjects without retinopathy. Diabetes Care 2011;34:1318–1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Fong DS, Aiello L, Gardner TW, et al. ; American Diabetes Association Retinopathy in diabetes. Diabetes Care 2004;27(Suppl 1):S84–S87 [DOI] [PubMed] [Google Scholar]
- 333.Ahmed J, Ward TP, Bursell SE, Aiello LM, Cavallerano JD, Vigersky RA. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Diabetes Care 2006;29:2205–2209 [DOI] [PubMed] [Google Scholar]
- 334.Bril V, England J, Franklin GM, et al. ; American Academy of Neurology; American Association of Neuromuscular and Electrodiagnostic Medicine; American Academy of Physical Medicine and Rehabilitation Evidence-based guideline: Treatment of painful diabetic neuropathy: report of the American Academy of Neurology, the American Association of Neuromuscular and Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2011;76:1758–1765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Boulton AJ, Vinik AI, Arezzo JC, et al. ; American Diabetes Association Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care 2005;28:956–962 [DOI] [PubMed] [Google Scholar]
- 336.Wile DJ, Toth C. Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 2010;33:156–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Freeman R. Not all neuropathy in diabetes is of diabetic etiology: differential diagnosis of diabetic neuropathy. Curr Diab Rep 2009;9:423–431 [DOI] [PubMed] [Google Scholar]
- 338.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care 2003;26:1553–1579 [DOI] [PubMed] [Google Scholar]
- 339.Spallone V, Bellavere F, Scionti L, et al. ; Diabetic Neuropathy Study Group of the Italian Society of Diabetology Recommendations for the use of cardiovascular tests in diagnosing diabetic autonomic neuropathy. Nutr Metab Cardiovasc Dis 2011;21:69–78 [DOI] [PubMed] [Google Scholar]
- 340.Boulton AJ, Armstrong DG, Albert SF, et al. ; American Diabetes Association; American Association of Clinical Endocrinologists Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care 2008;31:1679–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.American Diabetes Association Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26:3333–3341 [DOI] [PubMed] [Google Scholar]
- 342.Bainbridge KE, Hoffman HJ, Cowie CC. Diabetes and hearing impairment in the United States: audiometric evidence from the National Health and Nutrition Examination Survey, 1999 to 2004. Ann Intern Med 2008;149:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Bainbridge KE, Hoffman HJ, Cowie CC. Risk factors for hearing impairment among U.S. adults with diabetes: National Health and Nutrition Examination Survey 1999-2004. Diabetes Care 2011;34:1540–1545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Li C, Ford ES, Zhao G, Croft JB, Balluz LS, Mokdad AH. Prevalence of self-reported clinically diagnosed sleep apnea according to obesity status in men and women: National Health and Nutrition Examination Survey, 2005-2006. Prev Med 2010;51:18–23 [DOI] [PubMed] [Google Scholar]
- 345.West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax 2006;61:945–950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Foster GD, Sanders MH, Millman R, et al. ; Sleep AHEAD Research Group Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 2009;32:1017–1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Shaw JE, Punjabi NM, Wilding JP, Alberti KG, Zimmet PZ; International Diabetes Federation Taskforce on Epidemiology and Prevention Sleep-disordered breathing and type 2 diabetes: a report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res Clin Pract 2008;81:2–12 [DOI] [PubMed] [Google Scholar]
- 348.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol 2003;98:960–967 [DOI] [PubMed] [Google Scholar]
- 349.El-Serag HB, Tran T, Everhart JE. Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology 2004;126:460–468 [DOI] [PubMed] [Google Scholar]
- 350.American Gastroenterological Association American Gastroenterological Association medical position statement: nonalcoholic fatty liver disease. Gastroenterology 2002;123:1702–1704 [DOI] [PubMed] [Google Scholar]
- 351.Dhindsa S, Miller MG, McWhirter CL, et al. Testosterone concentrations in diabetic and nondiabetic obese men. Diabetes Care 2010;33:1186–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Bhasin S, Cunningham GR, Hayes FJ, et al. ; Task Force, Endocrine Society Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2010;95:2536–2559 [DOI] [PubMed] [Google Scholar]
- 353.Khader YS, Dauod AS, El-Qaderi SS, Alkafajei A, Batayha WQ. Periodontal status of diabetics compared with nondiabetics: a meta-analysis. J Diabetes Complications 2006;20:59–68 [DOI] [PubMed] [Google Scholar]
- 354.Darré L, Vergnes JN, Gourdy P, Sixou M. Efficacy of periodontal treatment on glycaemic control in diabetic patients: A meta-analysis of interventional studies. Diabetes Metab 2008;34:497–506 [DOI] [PubMed] [Google Scholar]
- 355.International Diabetes Federation Oral Health for People with Diabetes. Brussels, International Diabetes Federation, 2009 [Google Scholar]
- 356.Suh S, Kim KW. Diabetes and cancer: is diabetes causally related to cancer? Diabetes Metab J 2011;35:193–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356a.International Diabetes Federation. Oral Health for Patients with Diabetes. Brussels, 2009, International Diabetes Federation. [Google Scholar]
- 357.Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 2007;166:495–505 [DOI] [PubMed] [Google Scholar]
- 358.Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 2007;18:427–444 [DOI] [PubMed] [Google Scholar]
- 359.Yamamoto M, Yamaguchi T, Yamauchi M, Kaji H, Sugimoto T. Diabetic patients have an increased risk of vertebral fractures independent of BMD or diabetic complications. J Bone Miner Res 2009;24:702–709 [DOI] [PubMed] [Google Scholar]
- 360.Schwartz AV, Vittinghoff E, Bauer DC, et al. ; Study of Osteoporotic Fractures (SOF) Research Group; Osteoporotic Fractures in Men (MrOS) Research Group; Health, Aging, and Body Composition (Health ABC) Research Group Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 2011;305:2184–2192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Cukierman T, Gerstein HC, Williamson JD. Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies. Diabetologia 2005;48:2460–2469 [DOI] [PubMed] [Google Scholar]
- 362.Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol 2006;5:64–74 [DOI] [PubMed] [Google Scholar]
- 363.Ohara T, Doi Y, Ninomiya T, et al. Glucose tolerance status and risk of dementia in the community: the Hisayama study. Neurology 2011;77:1126–1134 [DOI] [PubMed] [Google Scholar]
- 364.Launer LJ, Miller ME, Williamson JD, Lazar RM, Gerstein HC, Murray AM, Sullivan M, Horowitz KR, Ding J, Marcovina S, Lovato LC, Lovato J, Margolis KL, O'Connor P, Lipkin EW, Hirsch J, Coker L, Maldjian J, Sunshine JL, Truwit C, Davatzikos C, Bryan RN: Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol 2011;10:969–977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Silverstein J, Klingensmith G, Copeland KC, et al. ; American Diabetes Association Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 2005;28:186–212 [DOI] [PubMed] [Google Scholar]
- 366.Northam EA, Anderson PJ, Werther GA, Warne GL, Adler RG, Andrewes D. Neuropsychological complications of IDDM in children 2 years after disease onset. Diabetes Care 1998;21:379–384 [DOI] [PubMed] [Google Scholar]
- 367.Rovet J, Alvarez M. Attentional functioning in children and adolescents with IDDM. Diabetes Care 1997;20:803–810 [DOI] [PubMed] [Google Scholar]
- 368.Bjørgaas M, Gimse R, Vik T, Sand T. Cognitive function in type 1 diabetic children with and without episodes of severe hypoglycaemia. Acta Paediatr 1997;86:148–153 [DOI] [PubMed] [Google Scholar]
- 369.Nimri R, Weintrob N, Benzaquen H, Ofan R, Fayman G, Phillip M. Insulin pump therapy in youth with type 1 diabetes: a retrospective paired study. Pediatrics 2006;117:2126–2131 [DOI] [PubMed] [Google Scholar]
- 370.Doyle EA, Weinzimer SA, Steffen AT, Ahern JA, Vincent M, Tamborlane WV. A randomized, prospective trial comparing the efficacy of continuous subcutaneous insulin infusion with multiple daily injections using insulin glargine. Diabetes Care 2004;27:1554–1558 [DOI] [PubMed] [Google Scholar]
- 371.Perantie DC, Wu J, Koller JM, et al. Regional brain volume differences associated with hyperglycemia and severe hypoglycemia in youth with type 1 diabetes. Diabetes Care 2007;30:2331–2337 [DOI] [PubMed] [Google Scholar]
- 372.Mäkimattila S, Malmberg-Cèder K, Häkkinen AM, et al. Brain metabolic alterations in patients with type 1 diabetes-hyperglycemia-induced injury. J Cereb Blood Flow Metab 2004;24:1393–1399 [DOI] [PubMed] [Google Scholar]
- 373.Krantz JS, Mack WJ, Hodis HN, Liu CR, Liu CH, Kaufman FR. Early onset of subclinical atherosclerosis in young persons with type 1 diabetes. J Pediatr 2004;145:452–457 [DOI] [PubMed] [Google Scholar]
- 374.Järvisalo MJ, Putto-Laurila A, Jartti L, et al. Carotid artery intima-media thickness in children with type 1 diabetes. Diabetes 2002;51:493–498 [DOI] [PubMed] [Google Scholar]
- 375.Haller MJ, Samyn M, Nichols WW, et al. Radial artery tonometry demonstrates arterial stiffness in children with type 1 diabetes. Diabetes Care 2004;27:2911–2917 [DOI] [PubMed] [Google Scholar]
- 376.Orchard TJ, Forrest KY, Kuller LH, Becker DJ; Pittsburgh Epidemiology of Diabetes Complications Study Lipid and blood pressure treatment goals for type 1 diabetes: 10-year incidence data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2001;24:1053–1059 [DOI] [PubMed] [Google Scholar]
- 377.Kavey RE, Allada V, Daniels SR, et al. ; American Heart Association Expert Panel on Population and Prevention Science; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Nutrition, Physical Activity and Metabolism; American Heart Association Council on High Blood Pressure Research; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on the Kidney in Heart Disease; Interdisciplinary Working Group on Quality of Care and Outcomes Research Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation 2006;114:2710–2738 [DOI] [PubMed] [Google Scholar]
- 378.McCrindle BW, Urbina EM, Dennison BA, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee; American Heart Association Council of Cardiovascular Disease in the Young; American Heart Association Council on Cardiovascular Nursing Drug therapy of high-risk lipid abnormalities in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee, Council of Cardiovascular Disease in the Young, with the Council on Cardiovascular Nursing. Circulation 2007;115:1948–1967 [DOI] [PubMed] [Google Scholar]
- 379.Salo P, Viikari J, Hämäläinen M, et al. Serum cholesterol ester fatty acids in 7- and 13-month-old children in a prospective randomized trial of a low-saturated fat, low-cholesterol diet: the STRIP baby project. Special Turku coronary Risk factor Intervention Project for children. Acta Paediatr 1999;88:505–512 [DOI] [PubMed] [Google Scholar]
- 380.The Dietary Intervention Study in Children (DISC). The Writing Group for the DISC Collaborative Research Group Efficacy and safety of lowering dietary intake of fat and cholesterol in children with elevated low-density lipoprotein cholesterol. JAMA 1995;273:1429–1435 [DOI] [PubMed] [Google Scholar]
- 381.McCrindle BW, Ose L, Marais AD. Efficacy and safety of atorvastatin in children and adolescents with familial hypercholesterolemia or severe hyperlipidemia: a multicenter, randomized, placebo-controlled trial. J Pediatr 2003;143:74–80 [DOI] [PubMed] [Google Scholar]
- 382.de Jongh S, Lilien MR, op't Roodt J, Stroes ES, Bakker HD, Kastelein JJ; de JS Early statin therapy restores endothelial function in children with familial hypercholesterolemia. J Am Coll Cardiol 2002;40:2117–2121 [DOI] [PubMed] [Google Scholar]
- 383.Wiegman A, Hutten BA, de Groot E, et al. Efficacy and safety of statin therapy in children with familial hypercholesterolemia: a randomized controlled trial. JAMA 2004;292:331–337 [DOI] [PubMed] [Google Scholar]
- 384.Cho YH, Craig ME, Hing S, Gallego PH, Poon M, Chan A, Donaghue KC: Microvascular complications assessment in adolescents with 2- to 5-yr duration of type 1 diabetes from 1990 to 2006. Pediatr Diabetes. 24 March 2011 [Epub ahead of print] [DOI] [PubMed]
- 385.Holmes GK. Screening for coeliac disease in type 1 diabetes. Arch Dis Child 2002;87:495–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Rewers M, Liu E, Simmons J, Redondo MJ, Hoffenberg EJ: Celiac disease associated with type 1 diabetes mellitus. Endocrinol Metab Clin North Am 2004;33:197–214 [DOI] [PubMed] [Google Scholar]
- 387.Kurppa K, Ashorn M, Iltanen S, Koskinen LL, Saavalainen P, Koskinen O, Maki M, Kaukinen K: Celiac disease without villous atrophy in children: a prospective study. J Pediatr 2010157:373–380 [DOI] [PubMed] [Google Scholar]
- 388.Abid N, McGlone O, Cardwell C, McCallion W, Carson D. Clinical and metabolic effects of gluten free diet in children with type 1 diabetes and coeliac disease. Pediatr Diabetes 2011;12:322–325 [DOI] [PubMed] [Google Scholar]
- 389.Roldán MB, Alonso M, Barrio R. Thyroid autoimmunity in children and adolescents with Type 1 diabetes mellitus. Diabetes Nutr Metab 1999;12:27–31 [PubMed] [Google Scholar]
- 390.Triolo TM, Armstrong TK, McFann K, et al. Additional autoimmune disease found in 33% of patients at type 1 diabetes onset. Diabetes Care 2011;34:1211–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Kordonouri O, Deiss D, Danne T, Dorow A, Bassir C, Grüters-Kieslich A. Predictivity of thyroid autoantibodies for the development of thyroid disorders in children and adolescents with Type 1 diabetes. Diabet Med 2002;19:518–521 [DOI] [PubMed] [Google Scholar]
- 392.Mohn A, Di Michele S, Di Luzio R, Tumini S, Chiarelli F. The effect of subclinical hypothyroidism on metabolic control in children and adolescents with Type 1 diabetes mellitus. Diabet Med 2002;19:70–73 [DOI] [PubMed] [Google Scholar]
- 393.Chase HP, Garg SK, Cockerham RS, Wilcox WD, Walravens PA. Thyroid hormone replacement and growth of children with subclinical hypothyroidism and diabetes. Diabet Med 1990;7:299–303 [DOI] [PubMed] [Google Scholar]
- 394.American Diabetes Association Diabetes care in the school and day care setting. Diabetes Care 2010;33(Suppl 1):S70–S74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55:469–480 [PubMed] [Google Scholar]
- 396.Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care 2007;30:2441–2446 [DOI] [PubMed] [Google Scholar]
- 397.American Diabetes Association Transition in care from youth to adulthood. Diabetes Care. 2011;34:2477–248522025785 [Google Scholar]
- 398.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care 2001;24:1536–1540 [DOI] [PubMed] [Google Scholar]
- 399.Laing SP, Jones ME, Swerdlow AJ, Burden AC, Gatling W. Psychosocial and socioeconomic risk factors for premature death in young people with type 1 diabetes. Diabetes Care 2005;28:1618–1623 [DOI] [PubMed] [Google Scholar]
- 400.Eppens MC, Craig ME, Cusumano J, et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care 2006;29:1300–1306 [DOI] [PubMed] [Google Scholar]
- 401.Hattersley A, Bruining J, Shield J, Njolstad P, Donaghue KC. The diagnosis and management of monogenic diabetes in children and adolescents. Pediatr Diabetes 2009;10(Suppl 12):33–42 [DOI] [PubMed] [Google Scholar]
- 402.Cooper WO, Hernandez-Diaz S, Arbogast PG, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med 2006;354:2443–2451 [DOI] [PubMed] [Google Scholar]
- 403.American Diabetes Association Preconception care of women with diabetes. Diabetes Care 2004;27(Suppl 1):S76–S78 [DOI] [PubMed] [Google Scholar]
- 404.Brown AF, Mangione CM, Saliba D, Sarkisian CA; California Healthcare Foundation/American Geriatrics Society Panel on Improving Care for Elders with Diabetes Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc 2003;51(Suppl Guidelines):S265–S280 [DOI] [PubMed] [Google Scholar]
- 405.Curb JD, Pressel SL, Cutler JA, et al. ; Systolic Hypertension in the Elderly Program Cooperative Research Group Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. JAMA 1996;276:1886–1892 [PubMed] [Google Scholar]
- 406.Beckett NS, Peters R, Fletcher AE, et al. ; HYVET Study Group Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887–1898 [DOI] [PubMed] [Google Scholar]
- 407.Moran A, Dunitz J, Nathan B, Saeed A, Holme B, Thomas W. Cystic fibrosis-related diabetes: current trends in prevalence, incidence, and mortality. Diabetes Care 2009;32:1626–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Moran A, Brunzell C, Cohen RC, et al. ; CFRD Guidelines Committee Clinical care guidelines for cystic fibrosis-related diabetes: a position statement of the American Diabetes Association and a clinical practice guideline of the Cystic Fibrosis Foundation, endorsed by the Pediatric Endocrine Society. Diabetes Care 2010;33:2697–2708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Clement S, Braithwaite SS, Magee MF, et al. ; American Diabetes Association; Diabetes in Hospitals Writing Committee Management of diabetes and hyperglycemia in hospitals. Diabetes Care 2004;27:553–591 [DOI] [PubMed] [Google Scholar]
- 410.Moghissi ES, Korytkowski MT, DiNardo M, et al. ; American Association of Clinical Endocrinologists; American Diabetes Association American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 2009;32:1119–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359–1367 [DOI] [PubMed] [Google Scholar]
- 412.Malmberg K, Norhammar A, Wedel H, Rydén L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation 1999;99:2626–2632 [DOI] [PubMed] [Google Scholar]
- 413.Wiener RS, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 2008;300:933–944 [DOI] [PubMed] [Google Scholar]
- 414.Brunkhorst FM, Engel C, Bloos F, et al. ; German Competence Network Sepsis (SepNet) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 2008;358:125–139 [DOI] [PubMed] [Google Scholar]
- 415.Finfer S, Chittock DR, Su SY, et al. ; NICE-SUGAR Study Investigators Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–1297 [DOI] [PubMed] [Google Scholar]
- 416.Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med 2007;35:2262–2267 [DOI] [PubMed] [Google Scholar]
- 417.Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006;354:449–461 [DOI] [PubMed] [Google Scholar]
- 418.Griesdale DE, de Souza RJ, van Dam RM, et al. Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. CMAJ 2009;180:821–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab 2008;93:2447–2453 [DOI] [PubMed] [Google Scholar]
- 420.Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902–1912 [DOI] [PubMed] [Google Scholar]
- 421.Bernard JB, Munoz C, Harper J, Muriello M, Rico E, Baldwin D. Treatment of inpatient hyperglycemia beginning in the emergency department: a randomized trial using insulins aspart and detemir compared with usual care. J Hosp Med 2011;6:279–284 [DOI] [PubMed] [Google Scholar]
- 422.Czosnowski QA, Swanson JM, Lobo BL, Broyles JE, Deaton PR, Finch CK. Evaluation of glycemic control following discontinuation of an intensive insulin protocol. J Hosp Med 2009;4:28–34 [DOI] [PubMed] [Google Scholar]
- 423.Shomali MI, Herr DL, Hill PC, Pehlivanova M, Sharretts JM, Magee MF. Transition to target: a prospective randomized trial comparing three formulae for determination of subcutaneous basal insulin dosing at the time of transition from intravenous insulin therapy following cardiac surgery. Diabetes Technol Ther 2011;13:121–126 [DOI] [PubMed] [Google Scholar]
- 424.Umpierrez GE, Smiley D, Jacobs S, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 2011;34:256–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Pasquel FJ, Spiegelman R, McCauley M, et al. Hyperglycemia during total parenteral nutrition: an important marker of poor outcome and mortality in hospitalized patients. Diabetes Care 2010;33:739–741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Schnipper JL, Liang CL, Ndumele CD, Pendergrass ML. Effects of a computerized order set on the inpatient management of hyperglycemia: a cluster-randomized controlled trial. Endocr Pract 2010;16:209–218 [DOI] [PubMed] [Google Scholar]
- 427.Wexler DJ, Shrader P, Burns SM, Cagliero E. Effectiveness of a computerized insulin order template in general medical inpatients with type 2 diabetes: a cluster randomized trial. Diabetes Care 2010;33:2181–2183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Furnary AP, Braithwaite SS. Effects of outcome on in-hospital transition from intravenous insulin infusion to subcutaneous therapy. Am J Cardiol 2006;98:557–564 [DOI] [PubMed] [Google Scholar]
- 429.Schafer RG, Bohannon B, Franz MJ, et al. ; American Diabetes Association Diabetes nutrition recommendations for health care institutions. Diabetes Care 2004;27(Suppl 1):S55–S57 [DOI] [PubMed] [Google Scholar]
- 430.Curll M, Dinardo M, Noschese M, Korytkowski MT. Menu selection, glycaemic control and satisfaction with standard and patient-controlled consistent carbohydrate meal plans in hospitalised patients with diabetes. Qual Saf Health Care 2010;19:355–359 [DOI] [PubMed] [Google Scholar]
- 431.Schafer RG, Bohannon B, Franz MJ, et al. ; American Diabetes Association Diabetes nutrition recommendations for health care institutions. Diabetes Care 2004;27(Suppl 1):S55–S57 [DOI] [PubMed] [Google Scholar]
- 432.Boucher JL, Swift CS, Franz MJ, et al. Inpatient management of diabetes and hyperglycemia: implications for nutrition practice and the food and nutrition professional. J Am Diet Assoc 2007;107:105–111 [DOI] [PubMed] [Google Scholar]
- 433.Korytkowski MT, Salata RJ, Koerbel GL, et al. Insulin therapy and glycemic control in hospitalized patients with diabetes during enteral nutrition therapy: a randomized controlled clinical trial. Diabetes Care 2009;32:594–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Umpierrez GE. Basal versus sliding-scale regular insulin in hospitalized patients with hyperglycemia during enteral nutrition therapy. Diabetes Care 2009;32:751–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Klonoff DC, Perz JF. Assisted monitoring of blood glucose: special safety needs for a new paradigm in testing glucose. J Diabetes Sci Tech 2010;4:1027–1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.D'Orazio P, Burnett RW, Fogh-Andersen N, et al. ; International Federation of Clinical Chemistry Scientific Division Working Group on Selective Electrodes and Point of Care Testing Approved IFCC recommendation on reporting results for blood glucose (abbreviated). Clin Chem 2005;51:1573–1576 [DOI] [PubMed] [Google Scholar]
- 437.Dungan K, Chapman J, Braithwaite SS, Buse J. Glucose measurement: confounding issues in setting targets for inpatient management. Diabetes Care 2007;30:403–409 [DOI] [PubMed] [Google Scholar]
- 438.Boyd JC, Bruns DE. Quality specifications for glucose meters: assessment by simulation modeling of errors in insulin dose. Clin Chem 2001;47:209–214 [PubMed] [Google Scholar]
- 439.Shepperd S, McClaran J, Phillips CO, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev 2010. (1):CD000313. [DOI] [PubMed] [Google Scholar]
- 440.American Diabetes Association Diabetes and employment. Diabetes Care 2011;34(Suppl 1):S82–S86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.American Diabetes Association: Diabetes and driving. Diabetes Care 2012;35(Suppl 1):S81–S86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.American Diabetes Association Diabetes management in correctional institutions. Diabetes Care 2011;34(Suppl 1):S75–S81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care 2008;31:81–86 [DOI] [PubMed] [Google Scholar]
- 444.Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med 2009;122:443–453 [DOI] [PubMed] [Google Scholar]
- 445.Wang J, Geiss LS, Cheng YJ, et al. Long-term and recent progress in blood pressure levels among U.S. adults with diagnosed diabetes, 1988-2008. Diabetes Care 2011;34:1579–1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Kerr EA, Heisler M, Krein SL, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med 2007;22:1635–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med 2011;26:170–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.The Chronic Care Model: Improving Chronic Illness Care. 2011 [Google Scholar]
- 449.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Parchman ML, Zeber JE, Romero RR, Pugh JA. Risk of coronary artery disease in type 2 diabetes and the delivery of care consistent with the chronic care model in primary care settings: a STARNet study. Med Care 2007;45:1129–1134 [DOI] [PubMed] [Google Scholar]
- 451.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med 2010;363:2611–2620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Davidson MB. How our current medical care system fails people with diabetes: lack of timely, appropriate clinical decisions. Diabetes Care 2009;32:370–372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Grant RW, Pabon-Nau L, Ross KM, Youatt EJ, Pandiscio JC, Park ER. Diabetes oral medication initiation and intensification: patient views compared with current treatment guidelines. Diabetes Educ 2011;37:78–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163:83–90 [DOI] [PubMed] [Google Scholar]
- 455.Rosal MC, Ockene IS, Restrepo A, et al. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: latinos en control. Diabetes Care 2011;34:838–844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Osborn CY, Cavanaugh K, Wallston KA, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun 2011;16(Suppl 3):268–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.O'Connor PJ, Sperl-Hillen JM, Rush WA, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med 2011;9:12–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005;293:1223–1238 [DOI] [PubMed] [Google Scholar]
- 459.Smith SA, Shah ND, Bryant SC, et al. ; Evidens Research Group Chronic care model and shared care in diabetes: randomized trial of an electronic decision support system. Mayo Clin Proc 2008;83:747–757 [DOI] [PubMed] [Google Scholar]
- 460.McLean DL, McAlister FA, Johnson JA, et al. ; SCRIP-HTN Investigators A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med 2008;168:2355–2361 [DOI] [PubMed] [Google Scholar]
- 461.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy 2008;28:421–436 [DOI] [PubMed] [Google Scholar]
- 462.Davidson MB, Ansari A, Karlan VJ. Effect of a nurse-directed diabetes disease management program on urgent care/emergency room visits and hospitalizations in a minority population. Diabetes Care 2007;30:224–227 [DOI] [PubMed] [Google Scholar]
- 463.Stone RA, Rao RH, Sevick MA, et al. Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care 2010;33:478–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Berikai P, Meyer PM, Kazlauskaite R, Savoy B, Kozik K, Fogelfeld L. Gain in patients’ knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care 2007;30:1587–1589 [DOI] [PubMed] [Google Scholar]
- 465.Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA 2006;296:427–440 [DOI] [PubMed] [Google Scholar]
- 466.O'Connor PJ, Bodkin NL, Fradkin J, et al. Diabetes performance measures: current status and future directions. Diabetes Care 2011;34:1651–1659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA 2009;301:603–618 [DOI] [PubMed] [Google Scholar]
- 468.Feifer C, Nemeth L, Nietert PJ, et al. Different paths to high-quality care: three archetypes of top-performing practice sites. Ann Fam Med 2007;5:233–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Ornstein S, Nietert PJ, Jenkins RG, et al. Improving diabetes care through a multicomponent quality improvement model in a practice-based research network. Am J Med Qual 2007;22:34–41 [DOI] [PubMed] [Google Scholar]
- 470.Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med 2011;365:825–833 [DOI] [PubMed] [Google Scholar]
- 471.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care 2009;32:234–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Battersby M, Von Korff M, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf 2010;36:561–570 [DOI] [PubMed] [Google Scholar]
- 473.Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med 2008;168:1776–1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Pullen-Smith B, Carter-Edwards L, Leathers KH. Community health ambassadors: a model for engaging community leaders to promote better health in North Carolina. J Public Health Manag Pract 2008;14(Suppl):S73–S81 [DOI] [PubMed] [Google Scholar]
- 475.Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care 2011;34:1047–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Rosenthal MB, Cutler DM, Feder J. The ACO rules—striking the balance between participation and transformative potential. N Engl J Med 2011;365:e6. [DOI] [PubMed] [Google Scholar]
- 477.Washington AE, Lipstein SH: The Patient-Centered Outcomes Research Institute: Promoting better information, decisions, and health. N Engl J Med 2011;365:e31. [DOI] [PubMed] [Google Scholar]


