Abstract
We used data from a 2003 survey of US physicians to examine differences between Jewish and other religiously affiliated physicians on 4-D of physicians' beliefs and practices regarding religion and spirituality (R/S) in the clinical encounter. On each dimension, Jewish physicians ascribed less importance to the effect of R/S on health and a lesser role for physicians in addressing R/S issues. These effects were partially mediated by lower levels of religiosity among Jewish physicians and by differences in demographic and practice-level characteristics. The study provides a salient example of how religious affiliation can be an important independent predictor of physicians' clinically-relevant beliefs and practices.
Keywords: Religion, Spirituality, Judaism, Physician, Clinical encounter
Introduction
Recent research has demonstrated that physicians commonly link religion and health. A large national survey found that US physicians who were more religious by any of several validated measures are also more likely to believe that religion/spirituality (R/S) has a strong and positive impact on health and to endorse and report practices of addressing R/S in the clinical encounter (Curlin et al. 2006, 2007). In most cases, having some religious affiliation was also associated with ascribing greater clinical importance and salience to R/S. However, this was not true for those physicians with a Jewish affiliation. As seen in Fig. 1, physicians who identified their religious affiliation as Jewish tended to be closer in their responses to those who indicated they had no religion than to those with a religious affiliation of Protestant, Catholic, or other. With respect to some questions, the differences were striking; for example, only 29% of Jewish physicians believe that R/S influences health much or very much, compared to 69% of Protestant physicians, 58% of Catholic physicians, and 68% of those with other religious affiliation (Curlin et al. 2007). Similarly, in contrast to 53% of Protestant physicians and 46% of other religiously affiliated physicians, only 13% of Jewish physicians report sharing their own R/S ideas and experiences with patients (Curlin et al. 2006).
Fig. 1.
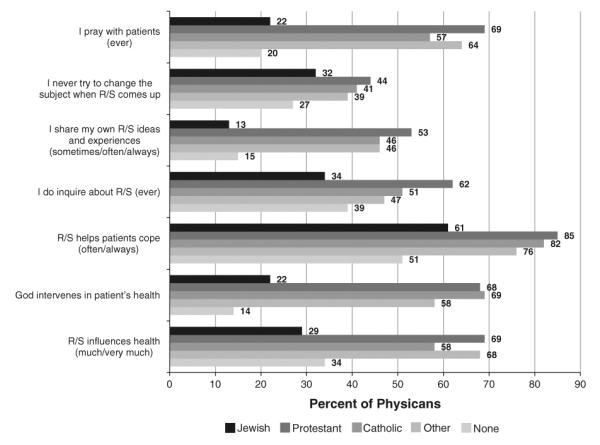
Selected survey results, previously published, showing the divergence of Jewish physicians in beliefs and practices related to religion/spirituality in the clinical encounter. The data presented are adapted from (Curlin et al. 2005, 2006)
There is little in the medical literature to explain this pattern. A growing body of research examines the impact of physician religiosity and spirituality on clinical decision-making, but few studies focus on the impact of religious affiliation generally or of Jewish affiliation specifically. Wenger and Carmel (2004) sought to understand how physicians' identification with Judaism affected their approaches to and practices concerning end-of-life care. However, their study was conducted with Israeli rather than American physicians. Christakis and Asch (1995) found that Jewish and Catholic doctors practicing at one academic medical center treated gravely ill patients in a more active manner than did Protestant doctors. Curlin et al. (2005) discovered that Jewish, Muslim, and Hindu physicians in the US were significantly less likely than physicians of a Christian affiliation to state that they carry their religious beliefs over into other aspects of their life. In addition, they found that, on average, Jewish physicians were less religious than physicians with other religious affiliations. Nevertheless, religious affiliation was not the primary focus of the latter paper, and it receives limited attention in the discussion.
To further examine the observed differences between Jewish and religiously affiliated non-Jewish physicians and to expand the literature on the clinical impact of specific religious affiliations, we reanalyzed data from a 2003 national survey of US physicians. Our purpose was to examine the association between Jewish affiliation and multiple dimensions of R/S and medicine. Among those who report a Jewish affiliation, some do so to indicate an ethnic or cultural identity rather than to indicate their religious beliefs and practices. For that reason, we hypothesized that differences between Jewish and religiously affiliated non-Jewish physicians on these measures would be accounted for by lower levels of religiosity among Jewish physicians and by differences in other demographic and practice characteristics between the two groups.
Methods
Design and Participants
The Religion and Spirituality in Medicine: Physicians' Perspectives study from which these data came has been described in prior publications (Curlin et al. 2006, 2007). In 2003, a 12-page confidential, self-administered questionnaire was mailed to a stratified random sample of 2,000 practicing US physicians. The physicians, who were all 65 years of age or younger, were chosen from the American Medical Association Physician Master file, a database intended to include all US physicians. The questionnaire was mailed to physicians up to three times, and the third mailing offered $20 for participation. To minimize error, all data was double-keyed, cross-compared, and corrected against the original questionnaires. The University of Chicago Institutional Review Board approved the study.
Measures
The criterion variables for the present study were scales created from responses to multiple survey items, each of which assessed some aspect of physicians' beliefs and self-reported behaviors concerning religion and spirituality in the clinical encounter. Survey items were developed after a thorough evaluation of the literature on religion, spirituality, and medicine and after a series of qualitative pilot interviews. They were then iteratively revised through expert panel review (Presser and Blair 1994). The terms religion and spirituality were not defined in the survey. Since they are used in overlapping ways in the medical literature, the terms were presented together as derivations of “religion/spirituality” in the items from which the criterion variables were constructed.
Because we had a number of potential outcome variables that appeared to address similar issues, we used empirical methods to reduce these outcome variables into distinct constructs that could be combined into scales (Table 1). This served two purposes. First, it reduced the number of criterion measures to a set of dimensions that more reliably represented constructs of interest. Second, by creating scales, which have greater variability than the items from which they are composed, that allowed us to use linear regression methods.
Table 1.
Questionnaire items used to assess 4-D of physicians' beliefs and practices regarding religion/spirituality in the clinical encounter
| Dimension 1: God actively intervenes in patient's health | α = 0.62 |
| 1. Do you think God or another supernatural being ever intervenes in patients' health? | |
| 2. Considering your experience, how often do you think religion/spirituality helps to prevent “hard” medical outcomes like heart attacks, infections, or even death? | |
| 3. When religious/spiritual issues come up in discussions with patients, how often do you pray with the patient? | |
| Dimension 2: R/S is beneficial for a patient's mental health | α = 0.79 |
| 1. Considering your experience, how often do you think religion/spirituality: | |
| a. Helps patients to cope with and endure illness and suffering? | |
| b. Gives patients a positive, hopeful state of mind? | |
| Dimension 3: physician inquires about R/S in the clinical encounter | α = 0.91 |
| 1. In general, is it appropriate or inappropriate for a physician to inquire about a patient's religion/spirituality? | |
| 2. I enjoy discussing religious/spiritual issues with patients | |
| 3. In the following clinical situations, how often do you inquire about religious/spiritual issues with a patient: | |
| a. Presents with a minor injury or illness? | |
| b. Faces a frightening diagnosis or crisis? | |
| c. Faces the end of life? | |
| d. Suffers from anxiety or depression? | |
| e. Comes for a history and physical? | |
| f. Faces an ethical quandary? | |
| Dimension 4: physician discusses R/S in the clinical encounter | α = 0.78 |
| 1. In general, is it appropriate or inappropriate for a physician to discuss religious/spiritual issues when a patient brings them up? | |
| 2. When, if ever, is it appropriate for a physician to talk about his or her own religious beliefs or experiences with a patient? | |
| 3. When, if ever, is it appropriate for a physician to pray with a patient? | |
| 4. I would feel comfortable discussing a patient's religious/spiritual concerns if the patient brought them up | |
| 5. When religious/spiritual issues come up in discussions with patients, how often do you respond in the following ways? | |
| a. I listen carefully and empathetically | |
| b. I try to change the subject in a tactful way | |
| c. I encourage patients in their own religious/spiritual beliefs and practices | |
| d. I respectfully share my own religious ideas and experiences |
All responses have been scaled from 0 to 4 (0 low, 4 high)
We initially grouped questionnaire items into three domains based upon their prima facie content. Exploratory factor analysis suggested that the third domain would best be subdivided into two, a division that seemed fitting on closer analysis of the respective items. The internal validity of the resulting 4-D was confirmed by calculation of alpha coefficients. The 4-D assess the extent to which a physician: (1) believes that God actively intervenes in patients' health (α = 0.62), (2) believes religion and spirituality are good for patients' psychological health (α = 0.79), (3) inquires about R/S with patients (α = 0.91), and (4) discusses R/S with patients (α = 0.78). To create the scores for each dimension, we first standardized each physician's responses (using a 0–4 scale, with 0 = low and 4 = high), and then took the average of each physician's responses to items in a given dimension. Respondents were excluded from a dimension if more than half of their answers were missing or marked “does not apply.”
The primary predictor variable was Jewish affiliation. We asked physicians, “What is your religious affiliation?” Response categories were Jewish, Catholic, Protestant, Buddhist, Hindu, Mormon, Muslim, Eastern Orthodox, Agnostic, Atheist, none or other. For the purposes of this study, physicians who identified as no religion (agnostic, atheist, or none) were excluded from analysis. As noted in previous publications (Curlin et al. 2006, 2007) and shown in Fig. 1, physicians' responses to items regarding R/S and medicine were similar across the affiliations Catholic, Protestant, Buddhist, Hindu, Mormon, Muslim, Eastern Orthodox, and other. We therefore collapsed these into a single category, religiously affiliated non-Jewish.
We also examined measures of physician religiosity. Intrinsic religiosity is a construct intended to measure the extent to which an individual makes his or her religion the “master motive” that guides and gives meaning to life (Fetzer Institute/National Institute on Aging Working Group 1999; Hill and Hood 1999; Allport and Ross 1967). It was measured by agreement or disagreement with two questions derived from the longer Hoge's Intrinsic Religious Motivation Scale (Hoge 1972): “I try hard to carry my religious beliefs over into all my other dealings in life,” and “My whole approach to life is based on my religion.” Intrinsic religiosity was classified as low if physicians disagreed with both statements, moderate if they agreed with one but not the other, and high if they agreed with both. Religious attendance was measured by how often respondents attend religious services (never, once a month or less, and twice a month or more), and physicians were asked whether they believe in God (Yes vs. No/Undecided). Control variables include physician age, sex, geographic region, primary specialty, board certification, and US versus non-US medical school graduation.
Statistical Analysis
Case weights were assigned and included in the analyses to account for sampling strategy and small differences in response rates by sex and foreign medical graduation (Groves et al. 2004). We first used Pearson chi-square tests to examine differences between Jewish and non-Jewish physicians on each of the demographic variables. We then divided Jewish and non-Jewish physicians according to each of the measures of religiosity, and used t tests to assess differences in mean scores between the subdivided Jewish and non-Jewish physician groups on each criterion measure. Next, three models of multivariable linear regressions were developed to test scores on each dimension against potential predictors. Predictors included: religious affiliation in the first model, religious affiliation plus demographic factors in the second model, and religious affiliation plus demographic factors plus other religious characteristics in the third model. We also tested a model in which we included interaction effects for all of the religious characteristics, in order to see whether the effect of Jewish affiliation differed at different levels of religiosity. All analyses take into account survey design and case weights by using the survey commands of Stata/SE 11.0 (Stata Corp; College Station, Tex 2005).
Results
Survey Response
Of the 2,000 potential respondents, an estimated 9% were ineligible because their addresses were incorrect or they were deceased. Among eligible physicians, 63% (1,144/1,820) responded. Foreign medical graduates were less likely to respond than US medical graduates (54% vs. 65%, P < 0.001), and men were less likely to respond than women (61% vs. 67%, P = 0.03). These differences were accounted for by assigning case weights. Response rates did not differ significantly by age, region, or board certification. The present study focuses on the 1,030 physicians who reported having some religious affiliation.
Demographic and Religious Characteristics of Jewish and Non-Jewish Physicians
Table 2 lists the characteristics of Jewish and religiously affiliated non-Jewish respondents. Jewish physicians were more likely to be older, to be male, and to have graduated from a US medical school. They tended to reside in the Northeast rather than the South or Midwest and were more represented in psychiatry and internal medicine subspecialties (less likely to practice general internal medicine or family practice).
Table 2.
Respondent characteristics (N = 1,030)
| Characteristic | Jewish (N = 181) | Religiously affiliated non-Jewish (N = 849) | P |
|---|---|---|---|
| N (%) | N (%) | ||
| Age (M, SD) | 50.1, 8.4 | 48.6, 8.3 | 0.03 |
| Women | 30 (17) | 240 (28) | 0.01 |
| Geographic region | <0.0005 | ||
| South | 43 (24) | 313 (37) | |
| Midwest | 32 (18) | 223 (26) | |
| Northeast | 73 (40) | 164 (19) | |
| West | 33 (18) | 147 (17) | |
| Non-US med school graduate | 24 (13) | 186 (22) | 0.02 |
| Board certification | 162 (90) | 722 (85) | 0.12 |
| Primary specialty | 0.02 | ||
| Family practice | 8 (4) | 136 (16) | |
| General internal medicine | 18 (10) | 100 (12) | |
| Internal medicine subspecialties | 43 (24) | 168 (20) | |
| Obstetrics and gynecology | 14 (8) | 56 (7) | |
| Pediatrics and subspecialties | 23 (13) | 111 (13) | |
| Psychiatry | 29 (16) | 54 (6) | |
| Surgical subspecialties | 15 (8) | 73 (9) | |
| Other | 31 (17) | 149 (18) | |
| Intrinsic religiosity | <0.0005 | ||
| Low | 113 (64) | 214 (26) | |
| Moderate | 37 (21) | 243 (30) | |
| High | 26 (15) | 366 (45) | |
| Religious attendance | <0.0005 | ||
| Never | 17 (9) | 38 (5) | |
| Once a month or less | 138 (76) | 308 (37) | |
| Twice a month or more | 26 (14) | 487 (59) | |
| Belief in God | <0.0005 | ||
| Yes | 105 (59) | 728 (87) | |
| No/undecided | 74 (41) | 106 (13) |
N values, mean values, and standard deviations are unweighted. Percent values and chi-square statistics are adjusted for survey design
This study excludes respondents with no religious affiliation
As measured by intrinsic religiosity, religious service attendance, and belief in God, Jewish respondents were significantly less religious than religiously affiliated non-Jewish respondents. In comparison to only 26% of religiously affiliated non-Jewish physicians, 64% of Jewish physicians scored low on the intrinsic religiosity scale (P < 0.001). Moreover, when compared to the religiously affiliated non-Jewish physicians, Jewish physicians were more likely to report attending religious services never or once a month or less (87% vs. 42%, P < 0.001) and to answer no/undecided when asked whether they believe in God (41% vs. 13%, P < 0.001).
Jewish Affiliation and R/S in Medicine
Figure 2 displays the mean scores of Jewish and non-Jewish physicians for dimension 3 (inquires about R/S in the clinical encounter), with scores stratified by responses to the three measures of religiosity. As seen there, among both Jewish and non-Jewish physicians, higher religiosity is associated with more inquiry about R/S. Yet, at each level of religiosity, Jewish physicians are less likely to inquire about R/S than their religiously affiliated non-Jewish colleagues. Patterns for the other 3-D (not shown) were similar, although the differences between Jewish physicians and religiously affiliated non-Jewish physicians were more pronounced in dimension 2 and less pronounced in dimensions 1 and 4.
Fig. 2.
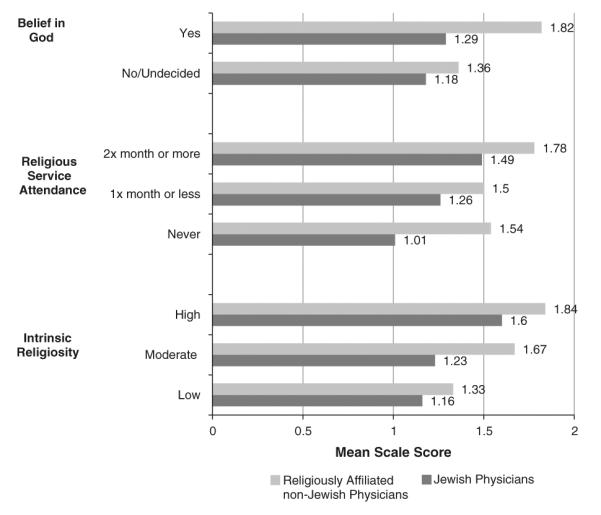
Physician inquires about R/S in the clinical encounter: mean dimension scores for Jewish versus religiously affiliated non-Jewish physicians, stratified by three religious characteristics. All differences between Jewish and religiously affiliated non-Jewish physicians presented in the table are statistically significant at P < 0.05
Table 3 presents the results of multivariable linear regression analysis for each of the 4-D represented by the scales. With respect to the first dimension, in the unadjusted model, Jewish physicians were less likely than religiously affiliated non-Jewish physicians to believe that God actively intervenes in patient health (b = −0.92, P < 0.005). When the model was expanded to include demographic and practice characteristics, the coefficient for Jewish affiliation decreased but remained statistically significant (b = −0.79, P < 0.005). This decrease was primarily the result of adding to the model residing in the Northeast (b = −0.31, P < 0.005) and the primary specialties of family practice (b = 0.41, P < 0.005), general internal medicine (b = 0.24, P = 0.032), and obstetrics and gynecology (P = 0.44, P = 0.001). The coefficient on Jewish affiliation was further attenuated but remained statistically significant (full model: b = −0.29, P < 0.005; R2 = 0.49, P < 0.005) after adding religious characteristics to the model.
Table 3.
Regression analysis of 4 d of physicians' beliefs and practices regarding religion and spirituality in the clinical encounter on physician identification with Judaism
| Model 1a Coefficient (95% CI) | Model 2b Coefficient (95% CI) | Model 3c Coefficient (95% CI) | |
|---|---|---|---|
| Scale 1: god actively intervenes in patient's health | −0.92 (−1.07, −0.77) R2 = 0.14 | −0.79 (−0.95, −0.63) R2 = 0.14 | −0.29 (−0.44, −0.14) R2 = 0.49 |
| Scale 2: R/S is beneficial for a patient's mental health | −0.40 (−0.51, −0.30) R2 = 0.07 | −0.32 (−0.42, −0.22) R2 = 0.12 | −0.14 (−0.26, −0.03) R2 = 0.23 |
| Scale 3: physician inquires about R/S in the clinical encounter | −0.58 (−0.72, −0.44) R2 = 0.06 | −0.57 (−0.70, −0.43) R2 = 0.19 | −0.30 (−0.45, −0.16) R2 = 0.31 |
| Scale 4: physician discusses R/S in the clinical encounter | −0.54 (−0.66, −0.43) R2 = 0.10 | −0.52 (−0.64, −0.4) R2 = 0.15 | −0.31 (−0.45, −0.18) R2 = 0.30 |
Table 3 presents unstandardized partial regression coefficients and 95% confidence intervals (with R2 for each model) for identification with Judaism on each of 4-D of physician's beliefs and practices regarding religion/spirituality in the clinical encounter
All values presented are statistically significant at P < 0.05
Model 1 includes identification with Judaism as the predictor variable
Model 2 includes identification with Judaism plus demographics (age, gender, geographic region) and practice characteristics (non-US medical school graduation, board certification, primary specialty) as the predictor variables
Model 3 includes identification with Judaism plus demographics, practice characteristics, and religious characteristics (intrinsic religiosity, religious service attendance, belief in God) as the predictor variables
With respect to the second dimension, in the unadjusted model, Jewish physicians were less likely than religiously affiliated non-Jewish physicians to believe that religion and spirituality are good for patients' psychological health (b = −0.40, P < 0.005). The effect of Jewish affiliation was attenuated but remained statistically significant after the addition of demographic and practice characteristics (b = −0.32, P < 0.005), as well as religious characteristics (full model: b = −0.14, P < 0.005; R2 = 0.23, P < 0.005). The reduction in the coefficient on Jewish affiliation in the second model resulted primarily from the effect of residing in the Northeast (b = −0.28, P < 0.005), foreign medical school graduation (b = 0.1, P = 0.061), and board certification (b = −0.14, P = 0.015).
With respect to the third dimension, which measures the extent to which a physician inquires about R/S with patients, Jewish affiliation was once again a statistically significant negative predictor across all models. The coefficient on Jewish affiliation hardly changed when including demographic and practice characteristics. Only a primary specialty of family practice (b = 0.48, P < 0.005) or psychiatry (b = 1.11, P < 0.005) modified the effect. The addition of religiosity measures to the model did attenuate the effect of affiliation, but it remained significant (full model: b = −0.30, P < 0.005; R2 = 0.31, P < 0.005).
The fourth dimension assessed the extent to which a physician discusses R/S in the clinical encounter. Parallel to the above findings, Jewish physicians reported less willingness to engage in discussions of R/S than religiously affiliated non-Jewish peers. The effect of Jewish affiliation remained significant across the three models (full model: b = −0.31, P < 0.005; R2 = 0.30, P < 0.005). In addition to religious characteristics, the effect of Jewish affiliation was modified by age (b = −0.05, P = 0.027), foreign medical school graduation (b = −0.12, P = 0.019), and a primary specialty of family practice (b = 0.19, P = 0.006), psychiatry (b = 0.21, P = 0.008), or “Other” (b = −0.16, P = 0.026).
We repeated the full multivariable regression models after adding in interaction terms between religious affiliation and each of intrinsic religiosity, religious service attendance, and belief in God. This analysis tested whether the effect of religious affiliation on the 4-D varied when each of the religious characteristics were stratified. When we examined whether adding the interaction terms significantly increased the variance in the dimensions explained by the models, we found that, in each case, the contribution of the interaction terms was not significant. This indicated that there was no interaction between religious affiliation and the religious characteristics and that model 3 was appropriate to use in our final analysis.
Discussion
Using data from a 2003 survey of American physicians, we found that when compared to religiously affiliated non-Jewish physicians, Jewish physicians are less likely to believe that God actively intervenes in patient health or that R/S are good for patients' psychological health, and they are less likely to inquire about or discuss R/S with patients. Multivariable linear regression analyses suggested these differences are partially accounted for by the differences in demographic, practices and religious characteristics between Jewish and non-Jewish physicians. Yet, the effect of Jewish affiliation remains significant even after adjustment for these covariates and consideration of possible interaction terms.
Because physicians who identify as Jewish are so diverse, we were surprised that Jewish affiliation was independently associated with physicians' ideas about R/S in medicine. Jewish physicians reside across all four of the geographic regions and work in all specialty categories. Moreover, although for some, Jewish affiliation indicates a system of religious beliefs and practices, for others, it primarily indicates an ethnicity or culture. Indeed, we found that Jewish physicians were more likely than other religiously affiliated physicians to indicate they rarely or never attend religious services, and they do not believe in God. Even among more religious Jews, there is a wide spectrum of beliefs. Jews may differ in such basic religious tenets as whether they ascribe divinity to Jewish law and whether they perceive Jewish law as binding. Hecht and Faulkner (2000), building on the work of political scientist Medding (1987), noted that Judaism is not a singular entity but rather a “`system of voluntary memberships and individual decision' with vague boundaries in which Jewish identity is neither as central nor as salient as in the traditional Jewish community” (p. 373). We therefore did not expect to find that Jewish physicians consistently ascribed less importance to R/S in the clinical encounter than did their religiously affiliated non-Jewish counterparts, even after adjusting for other relevant characteristics.
We can only speculate about why Jewish physicians differ from religiously affiliated non-Jewish physicians on this subject. The great majority (93%) of the Jewish physicians surveyed were raised in the 30 years following the Holocaust. Contemporary Jewish historians note that for this generation of American Jews, the Holocaust was a defining event (Sarna 2004). Katz et al. (2007) write that the death of 6 million European Jews and God's seeming absence during this event forced Jews to reconsider their traditional theology, and, in particular, the role of God in everyday human life. Many rejected the existence of God outright; for example, Alexander Donat, a Holocaust survivor and journalist in New York concludes that he cannot find any explanation to excuse the inaction of traditional Judaism's assertedly benevolent, omnipotent, historically active God during the [Holocaust]. And so, he rejects Him, i.e., His existence, outright, allowing no half-measures” (Katz et al. 2007, p. 274). Other Jews explained God's apparent absence during the Holocaust by giving up the idea that God intervenes in day–day human existence. They concluded that once God granted human beings free will, God had to respect the decisions that human beings would make. This forced God to turn His face from the suffering of the Jews during the Holocaust. The Rabbi and theologian Eliezer Berkovits, describes this as “the ultimate tragedy of existence: God's very mercy and forbearance, His very love for man, necessitates the abandonment of some men to a fate that they may well experience as divine indifference to justice and human suffering” (Katz et al. 2007, p. 470).
These theological responses may explain why many Jewish physicians maintain that God does not actively intervene in patient's health. If one rejects God outright or believes that God must turn His face from everyday human life, one might reasonably conclude that God cannot intervene in patients' health.
In a different vein, our findings regarding the discussion of R/S in the clinical encounter may highlight the Jewish physician's outsider status as a member of a religious minority. Because Jewishness is not always readily apparent, Jewish physicians can choose the extent to which they disclose or foreground their Jewish identity. Even in the United States, where Jews experience a great measure of acceptance and success, many are reluctant to call attention to their Jewish identity because of associated stigmas (Hecht and Faulkner 2000). In a qualitative analysis to determine how frequently and under what circumstances Jewish individuals are willing to share their Jewish identity, Hecht and Faulkner (2000) found that one-fourth of Jews would not disclose their Judaism when asked about their religion. They discovered that even among Jews who were willing to identify as Jewish, some were uncomfortable sharing this information in a first meeting or when there was a difference in values or customs. In addition, many of these individuals only identified as Jewish when the topic of religion was raised by others. Discussion of R/S in the clinical encounter could require that a Jewish physician shares his/her Jewish identity with the patient. Discomfort in disclosing this information may lead Jewish physicians to avoid this discussion altogether. For this reason, Jewish physicians may have indicated less willingness to inquire about R/S with the patient or to engage in a discussion of it.1
Although we can only speculate about why Jewish and religiously affiliated non-Jewish physicians differ in the importance they ascribe to R/S in the clinical encounter, these differences may be clinically important. The place of religion and spirituality in the doctor–patient relationship continues to be controversial (Curlin et al. 2006). To some physicians, the importance that patients ascribe to religion and spirituality make religion and spirituality necessary topics within the clinical encounter (Koenig 2000; Astrow et al. 2001; Pembroke 2008). To other physicians, the sensitive and potentially controversial nature of religion and spirituality place religion and spirituality outside the purview of the doctor–patient relationship (Sloan et al. 2000; Lawrence 2002). Since a physician's view on this subject may be in direct conflict with that of his/her patient, it is important to understand what characteristics account for physicians' perspectives. Identification with Judaism must now be added to the list of independent predictors, along with religiosity, spirituality, and region.
This study has significant limitations. First, the survey questions were not sufficiently detailed to explain why Jewish and religiously affiliated non-Jewish physicians differ in the importance that they indicate for R/S in the clinical encounter. Future studies should deploy more comprehensive survey questions and/or qualitative analysis to build on these findings. Second, although the study had a better than average response rate (Asch et al. 1997) and we did not find evidence to suggest substantial response bias (Curlin et al. 2005), religious affiliation or other characteristics could have systemically affected physician's willingness to respond in unmeasured ways. Third, religion and spirituality can be operationalized in different manners, using additional or different constructs. This limitation is partially mitigated by the similar relationships that we found when we operationalized religiosity by self-assessment or by self-reported frequency of attendance at religious service. Finally, we had a small number of subjects in some of our subpopulations, which limited the stability of estimates for those subpopulations.
Despite these limitations, this study shows that identification with Judaism affects the significance and role that a physician ascribes to R/S in the clinical encounter. It also demonstrates more generally that religious affiliation can be a significant predictor of a physician's beliefs or practices. Additional studies of Jewish physicians and physicians from other religious traditions are needed to explain when and why religious affiliation affects physicians' beliefs and practices in this and other clinical domains.
Acknowledgments
This work was supported by grants from the University of Chicago Summer Research Program, as well as the Greenwall Foundation, the Robert Wood Johnson Clinical Scholars Program, and the National Center for Complementary and Alternative Medicine (1 K23 AT002749). The funding agencies did not have any role in the design, conduct, analysis, and interpretation of the study, nor in the preparation of the manuscript. The authors are indebted to Michael Putman, Michael Combs, and Helen Shin for their constructive feedback on an earlier version of this paper.
Footnotes
1Interestingly, the two explanations offered here may be specific to the generation of Jewish physicians surveyed. Younger Jews in the United States are less defined by an outsider status and less affected by the events of the Holocaust. It will be note-worthy whether identification with Judaism remains a significant predictor amongst the next generation of Jewish physicians.
References
- Allport G, Ross J. Personal religious orientation and prejudice. Journal of Personality and Social Psychology. 1967;5:447–457. doi: 10.1037/0022-3514.5.4.432. [DOI] [PubMed] [Google Scholar]
- Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. Journal of Clinical Epidemiology. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- Astrow AB, Puchalski CM, Sulmasy DP. Religion, spirituality, and health care: Social, ethical, and practical considerations. American Journal of Medicine. 2001;110:283–287. doi: 10.1016/s0002-9343(00)00708-7. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Asch DA. Physician characteristics association with decisions to withdraw life support. American Journal of Public Health. 1995;85(3):367–372. doi: 10.2105/ajph.85.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curlin FA, Lantos JD, Roach CJ, Sellergren SA, Chin MH. Religious characteristics of US physicians: A national survey. Journal of General Internal Medicine. 2005;20:629–634. doi: 10.1111/j.1525-1497.2005.0119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curlin FA, Chin MH, Sellergren SA, Roach CJ, Lantos JD. The association of physicians' religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical endeavor. Medical Care. 2006;44(5):446–453. doi: 10.1097/01.mlr.0000207434.12450.ef. [DOI] [PubMed] [Google Scholar]
- Curlin FA, Sellergren SA, Lantos JD, Chin MH. Physicians' observations and interpretations of the influence of religion and spirituality on health. Archives of Internal Medicine. 2007;167:649–654. doi: 10.1001/archinte.167.7.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey methodology. Wiley; Hoboken, NJ: 2004. [Google Scholar]
- Hecht ML, Faulkner SL. Sometimes Jewish, sometimes not: the closeting of Jewish American identity. Communication Studies. 2000;51(4):372–387. [Google Scholar]
- Hill PC, Hood RW. Measures of religiosity. Religious Education Press; Birmingham, Alabama: 1999. [Google Scholar]
- Hoge DR. A validated intrinsic religious motivation scale. Journal for the Scientific Study Religion. 1972;11:369–376. [Google Scholar]
- Katz ST, Biderman S, Greenberg G. Wrestling with God: Jewish theological responses during and after the holocaust. Oxford University Press; NY: 2007. [Google Scholar]
- Koenig HG. MSJAMA: Religion, spirituality, and medicine: Application to clinical practice. Journal of the American Medical Association. 2000;284:1708. [PubMed] [Google Scholar]
- Lawrence RJ. The witches' brew of spirituality and medicine. Annals of Behavioral Medicine. 2002;24:74–76. doi: 10.1207/S15324796ABM2401_09. [DOI] [PubMed] [Google Scholar]
- Medding PY. Segmented ethnicity and the new Jewish politics. Studies in Contemporary Jewry. 1987;3:26–45. [Google Scholar]
- Multidimensional measurement of religiousness. spirituality for use in health research: A report of the Fetzer Institute. National Institute on Aging Working Group [accessed July 28, 2010];1999 Available at http://www.fetzer.org.
- Pembroke NF. Appropriate spiritual care by physicians: A theological perspective. Journal of Religion and Health. 2008;47(4):549–559. doi: 10.1007/s10943-008-9183-0. [DOI] [PubMed] [Google Scholar]
- Presser S, Blair J. Survey pretesting: Do different methods produce different results? Sociological Methodology. 1994;24:73–104. [Google Scholar]
- Sarna JD. American Judaism: A history. Yale University Press; New Haven, CT: 2004. [Google Scholar]
- Sloan RP, Bagiella E, VandeCreek L, Hover M, Casalone C, Jinpu Hirsch T, et al. Should physicians prescribe religious activities? New England Journal of Medicine. 2000;342:1913–1916. doi: 10.1056/NEJM200006223422513. [DOI] [PubMed] [Google Scholar]
- Wenger NS, Carmel S. Physicians' religiosity and end-of-life care attitudes and behaviors. Mount Sinai Journal of Medicine. 2004;71(5):335–343. [PubMed] [Google Scholar]


