Abstract
Objective
To examine effects of a delivery system for evidence-based preventive interventions through 12th grade, 6.5 years past baseline.
Method
A cohort sequential design included 28 public school districts randomly assigned to the partnership delivery system or usual-programming conditions. At baseline, 11,960 students participated. Partnerships supported community teams that implemented a family-focused intervention in 6th grade and a school-based intervention in 7th grade. Outcome measures included lifetime, current misuse, and frequencies of misuse, for a range of substances. Intent-to-treat, multilevel analyses of covariance of point-in-time misuse and analyses of growth in misuse were conducted.
Results
Results showed significantly lower substance misuse in the intervention group at one or both time points for most outcomes, with relative reduction rates of up to 31.4%. There was significantly slower growth in misuse in the intervention group for 8 of 10 outcomes. In addition, risk moderation results indicated there were significantly greater intervention benefits for higher- versus lower-risk youth, for misuse of 6 of 10 substances at 11th grade, illicit substances at 12th grade, and growth in misuse of illicit substances.
Conclusion
Partnership-based delivery systems for brief universal interventions have potential for public health impact by reducing substance misuse among youth, particularly higher-risk youth.
Keywords: Evidence-based, universal preventive intervention, community-university partnership model, delivery system
Introduction
Prevalence rates of alcohol, tobacco, marijuana, and other illicit substances among adolescents continue to be high (Johnston et al., 2011) and result in adverse health effects. The long-term negative consequences of underage drinking and substance misuse are well documented (Harwood, 2000; Harwood and Bouchery, 2004; McCambridge et al., 2011; Miller and Hendrie 2008; Mathurin and Deltenre, 2009). Early substance misuse is associated with reduced levels of educational and occupational attainment, risky sexual practices, and impaired mental health (National Institute on Drug Abuse, 2009).
Recent recommendations for addressing substance misuse through universal intervention include implementation through community-based partnerships linking scientists with community practitioners (Hawkins et al., 2012; Grumbach and Mold, 2009; National Research Council and Institute of Medicine, 2009; Spoth and Greenberg, 2005). However, community health-related systems often are ill-equipped to develop and sustain the necessary partnerships and interventions (Berwick, 2003; Gold and Bailey, 2008; Grumbach and Mold, 2009; Woolf, 2008). The current study evaluates a diffusion model that addresses these problems, in order to better translate health science into practice (Berwick, 2003; Woolf, 2008). This model, called PROSPER (PROmoting School-community-university Partnerships to Enhance Resilience), was designed as a partnership-based delivery system for scientifically-proven prevention programs.
The PROSPER model leverages the existing infrastructure of land grant universities’ Cooperative Extension Systems (CES), which serve scientific outreach functions in every state. The three tiers of the PROSPER model consist of: (1) teams of community stakeholders linked with public schools and led by local CES staff, (2) Prevention Coordinators (PCs) connected with the land grant university’s CES, and (3) a team of state-level university researchers and CES faculty. Prevention Coordinators serve as liaisons between the community and university teams, providing ongoing, proactive technical assistance to community teams to optimize team functioning and program delivery.
Effectiveness of the PROSPER model’s key elements (Spoth et al., 2004; Spoth et al., 2007a) has been demonstrated through a longitudinal cluster randomized controlled trial (RCT), begun in 2001. These findings include effective participant recruitment (Spoth et al., 2007b), maintenance of implementation quality (Spoth et al., 2007c), and sustainability of intervention delivery (Greenberg et al., unpublished results). Additional results include positive effects on intervention-targeted youth and parent skills, putative mediators likely to reduce substance misuse (Redmond et al., 2009), as well as significant reductions in substance misuse at 4.5 years (10th grade) among intervention group students (Spoth et al., 2011). The current study examines longer-term effects of this partnership-based prevention program delivery model.
In addition to evaluating intervention effects on substance misuse at the end of high school (11th and 12th grades, 5.5 and 6.5 years past baseline), we also evaluate intervention effects on growth in adolescent substance misuse across 6.5 years, and risk-related moderation of these effects.
METHODS
Community selection and assignment
Twenty eight communities participated; 14 in both Iowa and Pennsylvania. The sample size recruited was based on multilevel power calculations incorporating effect sizes and ICCs estimated from previous evaluation trials of programs on the PROSPER menu. Pairs of communities were matched (14 blocks) on school district size and geographic location, and then randomly assigned to either the partnership intervention or the “usual programming” comparison condition. Because the intervention condition involved collaboration between community stakeholders and local schools, a site’s eligibility for recruitment was based on school and community-level characteristics. School districts were required to have an enrollment of between 1,300 and 5,200 students. Additional details related to recruitment procedures are available in Spoth et al. (2007b).
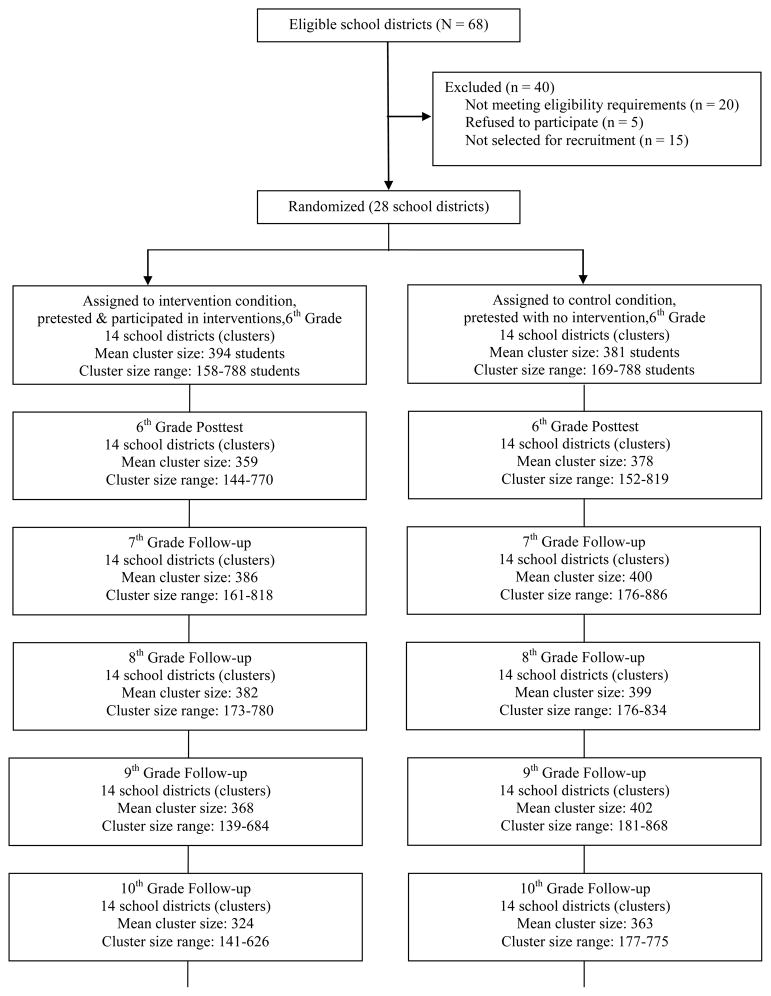
The study employed a cohort sequential design that included two successive cohorts of 6th graders (designated Cohort 1 and Cohort 2). School districts were informed of their assignment to condition after they enrolled. Figure 1 summarizes sample tracking over the eight waves of data collection. All enrolled 6th graders from the two cohorts were recruited for participation. Approximately 90% of the valid baseline sample provided some pretest data. Most students were Caucasian (85%); 51% were female, 64% lived with both biological parents, and 31% received free or reduced-cost school lunches. The participating universities’ Institutional Review Boards approved the study procedures.
Figure 1.
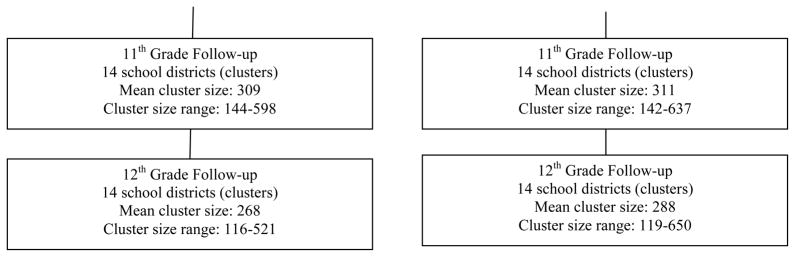
Study participation summary.
Notes: In addition to consideration of eligibility criteria specific to school districts, an additional criterion was that all school districts for which there was no Cooperative Extension staff person available to serve the school district’s community were deemed ineligible. Two school districts (one each in IA and PA) dropped out during the pretesting period and were replaced with two comparably-sized school districts remaining in the eligible pool. A series of analyses suggested that the replacement schools did not bias results toward positive intervention-control differences. Student participation in the assessments at a given wave was not contingent on participation in prior waves (all enrolled students in the two study cohorts were recruited for participation at each wave). Cluster sizes include the students from both cohorts who completed assessments. Although there was considerable stability in the enrolled samples from year to year, those students who changed conditions (i.e., moved from a school district in one condition into a school district in a different condition) were eliminated from the sample to preserve randomization.
PROSPER Partnership Delivery System
The 14 intervention communities utilized PROSPER’s partnership model to deliver family-focused and school-based interventions (Spoth et al., 2004; Spoth et al. 2007a). Teams of 8–12 individuals, including the local CES-based team leader, a public school co-leader, representatives of local human service agencies (e.g., mental health, substance abuse), and parent and youth representatives were formed. Teams selected an evidence-based universal family-focused program from a menu of three choices.
All 14 community teams chose the Strengthening Families Program: For Parents and Youth 10–14 (SFP: 10–14). Program selection was followed by family recruitment and delivery of the program to families of Cohort 1 6th graders. During year 2 the family program was offered to families of Cohort 2 6th graders. Also in year 2, community teams selected one of three school-based EBIs for delivery to 7th graders in the first cohort. Life Skills Training and Project Alert were each selected by four teams; the All Stars curriculum was selected by the other six. The school-based program was implemented with Cohort 2 7th grade students the following year. Brief information on each program follows (for more detail, see Spoth et al., 2007a).
Family intervention for 6th graders
The Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14; see Molgaard et al., 1997) is a seven-session program that focuses on enhancing parenting skills — specifically nurturance, limit setting, and communication, as well as youth substance refusal and other prosocial skills. The SFP 10–14 originally was adapted from an earlier program developed by Kumpfer (called the Strengthening Families Program, or SFP). The SFP 10–14 differs from the earlier SFP in type, participant age range, and length. That is, the earlier SFP was a more intensive intervention (12–14 sessions) designed for younger (6–12 years) at-risk children and parents, whereas the SFP 10–14 is a briefer, universal intervention designed for general population youth and families (see Molgaard et al., 1997; Molgaard & Spoth, 2001; Spoth, Redmond, & Shin, 2001).
There were 142 program groups offered during the two years in the 14 intervention communities. A total of 1,064 families attended at least one session, representing 17% of all eligible families. Of these families, 90% attended at least four of the seven sessions and 63% attended at least six. Adherence to implementation quality protocols across both cohorts, measured by observer reports of specific prescribed activities actually performed, was over 90%.
School interventions for 7th graders
Life Skills Training (LST: Botvin, 2000; 1996) is a 15-lesson universal preventive intervention that is designed to promote the development of skills, such as peer resistance and self-management, and strategies for avoiding the use of substances (Botvin et al., 1984).
Project ALERT is an 11-session social influence-focused intervention (Rosenstock et al., 1988) which focuses on changing students’ beliefs about substance use norms, helping students identify and resist pro-substance use pressures from peers and the media, and strengthening their refusal self-efficacy.
The All Stars Program is a 13-session intervention which focuses on influencing students’ perceptions about substance use and violence, increasing accuracy of students’ beliefs about peer norms, having students make a personal commitment to avoid negative behaviors, and increasing their bonding to school (Hansen, 1996).
Each of the school-based interventions was delivered during class periods, generally by a regular classroom teacher. Across both cohorts, the implementation adherence rates for LST, Project ALERT, and All Stars were 89%, 89%, and 91%, respectively (Spoth et al., 2007c).
Data collection
Student data were collected via written questionnaires by research staff. Students were assured of confidentiality and that the information they provided would not be seen by parents or school staff. Pretest assessments were conducted with 6th graders during the fall semesters of 2002 (for Cohort 1) and 2003 (for Cohort 2). Follow-up assessments for the two cohorts were conducted annually from 0.5 years to 6.5 years past baseline (spring of 6th to 12th grade). On average, across the eight data points, 86% of all eligible students completed the surveys, with slightly higher rates of participation at earlier data collection points.
Measures
We used self-reported substance misuse measures similar to those used in previous studies (e.g., Spoth et al., 2001). Although self-report measures may be susceptible to social desirability biases, previous work has supported their validity (Elliott et al., 1983; Smith et al., 1995; Williams et al., 1995). Current use (past-month and past-year use) was assessed with dichotomous measures; additional measures captured the higher levels of use typically observed during later adolescence or behaviors exclusive to this stage (e.g., drinking and driving). With these additional measures and the consideration of space constraints, all other lifetime use outcomes are reported online (http://www.ppsi.iastate.edu/publicationsupplements/PF215/tables.pdf).
Lifetime Illicit Substance Use Index
The Illicit Substance Use Index (ISUI) is the sum of five dichotomous lifetime substance use items (yielding scores ranging from 0 to 5). Items included “Have you ever…:” (a) “used methamphetamine;” (b) “used ecstasy;” (c) “smoked marijuana;” (d) “used drugs or medications that were prescribed by a doctor for someone else;” and (e) “used Vicodin, Percocet, or Oxycontin (not prescribed by a doctor).”
Current use/behavior
Dichotomous measures indicating whether a given substance was used or behavior occurred during the specified period included: past-month drunkenness, past-month cigarette smoking, past-year marijuana use, past-year use of inhalants, past-year use of methamphetamines, and past-year driving after drinking.
Frequency of use/behavior
Frequency of drunkenness, driving after drinking, and marijuana use were scored on a seven-point scale, ranging from 0 (never) to 7 (more than weekly).
Analyses
Longitudinal multi-level models (Level 2 = school district, Level 1 = individual) from posttest to 12th grade were applied to analyze both point-in-time 11th and 12th grade substance misuse outcomes and growth trajectories of those outcomes using the SAS PROC MIXED procedure. State, Cohort, Condition, Block were included as design factors in the model at the school-level (Level 2); Time and Risk status were included at the individual-level (Level 1), as were all corresponding interaction terms. Time was coded as the number of data collection points since pretest (i.e., 1 = 0.5 years after baseline, ranging to 7 = 6.5 years after baseline). Higher-risk status was determined by any lifetime use of alcohol, cigarettes, or marijuana at baseline.
To account for cross-time correlations in the repeated measure of outcomes, the ARH(1) option in SAS, auto-regressive covariance with heterogeneous variances, was employed in the mixed models. Outcome measure scores at pretest were included as individual-level covariates. Iterative parameter estimation was not feasible due to model complexity; consequently, the non-iterative MIVQUE0 (minimum variance quadratic unbiased estimator) option was employed to estimate variance components. It is noteworthy that MIVQUE0 tends to provide more conservative, larger standard errors than iterative methods such as REML and ML.
All analyses presented are intent-to-treat. To improve validity of the growth trajectory estimates, students were included if they completed surveys at three or more of the eight data collection points. Missing data were handled using full-information maximum likelihood estimation.
Point-in-time 11th and 12th grade analyses were conducted via specified contrasts (using CONTRAST statements in PROC MIXED) within the multilevel longitudinal model described above. Use of the contrast approach for intervention vs. control differences within the longitudinal model utilizes all available information and provides efficient parameter estimates through reduced experimental errors. Growth trajectory analyses from the 6th grade posttest through the spring of 12th grade were conducted utilizing the same model. Linear slope differences in substance use trajectories were evaluated using a repeated measures analysis with a linear CONTRAST statement. Because all intervention effects were in the expected direction at earlier waves, and prior evidence of program effectiveness was a criterion for inclusion on the menu of programs, primary emphasis is on one-tailed test results. Specific p-values are reported so that two-tailed significance levels can be calculated by doubling the reported one-tailed values.
Relative reduction rates were calculated to illustrate the practical significance of findings for dichotomous outcomes; they indicate the proportional behavioral reduction in the intervention group relative to controls. For the frequency of use outcomes, cut points for dichotomizing the variables were determined by considering public health impact. For drunkenness, a frequency level of more than once yearly was selected as the cut point; 36.7% and 42.2% of students (11th and 12th grade, respectively) were above the cut point. The same cut point was employed for marijuana use; 20.8% and 23.5% were above the cut point. For driving after drinking, any occurrence was considered a significant risk behavior; 22.1% and 29.1% were above the cut point. For the ISUI, any use was categorized as above threshold; 24.1% and 28.5% were above the cutoff.
RESULTS
Sample quality
Pretest equivalence of the two conditions was assessed; there were no significant differences on any sociodemographic measure (e.g., gender, age, race, school lunch status) or on any of the 10 outcomes. Differential attrition was assessed by examining whether the two-way interaction of Condition × Pretest score on the outcome variables predicted drop-out at each wave. No significant interactions were found.
Lifetime illicit substance use index
Point-in-time analyses of the ISUI showed significant overall intervention-control differences at both grades, with results indicating lower levels of use among the intervention group (see Table 1). The ISUI relative reduction rate indicates that lifetime use of any of the five substances included was 18.8% lower in the intervention group, relative to controls in 11th grade, and 15.0% lower in 12th grade. Significant Condition × Risk point-in-time effects showed larger intervention-control differences observed for students identified as higher-risk at pretest. Also significant were intervention effects on growth trajectories, showing (a) slower growth in lifetime illicit use from 6th to 12th grades for the intervention group (Condition × Linear Time); and (b) stronger intervention effects on growth in use for higher-risk students compared to lower-risk students (Condition × Risk × Linear Time—see Table 2).
Table 1.
Point-in-Time Intervention-Control Differences (11th and 12th Grades) for Iowa and Pennsylvania sites, 2008–2010*
| Results for 11th Grade | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Intervention Main Effect | Risk-Moderation Effect | |||||||
| I | C | F(1,72) (p) | RRR | I–H | I–L | C–H | C–L | F(1,78) (p) | |
| Lifetime Illicit Substance Use | 1.16 | 1.45 | 35.26 (.001) | 18.8% | 1.48 | 0.85 | 1.91 | 0.98 | 22.05 (.001) |
| Current Use | |||||||||
| Past Month Drunkenness | 0.35 | 0.38 | 1.33 (.126) | 6.3% | 0.45 | 0.26 | 0.49 | 0.27 | 2.01 (.080) |
| Past Month Cigarettes | 0.28 | 0.32 | 2.92 (.045) | 11.7% | 0.34 | 0.22 | 0.40 | 0.24 | 2.64 (.054) |
| Past Year Marijuana | 0.31 | 0.36 | 9.36 (.001) | 13.5% | 0.39 | 0.23 | 0.47 | 0.25 | 6.83 (.005) |
| Past Year Drive after Drinking | 0.19 | 0.22 | 2.02(.090) | 16.3% | 0.24 | 0.14 | 0.29 | 0.15 | 3.69 (.038) |
| Past Year Inhalants | 0.05 | 0.05 | 0.74 (.195) | 14.0% | 0.05 | 0.04 | 0.06 | 0.04 | 0.01 (.476) |
| Past Year Methamphetamine | 0.02 | 0.04 | 4.37 (.020) | 30.9% | 0.04 | 0.01 | 0.04 | 0.03 | 1.33 (.126) |
| Frequency of Use | |||||||||
| Drunkenness | 2.46 | 2.66 | 2.91 (.046) | 3.3% | 3.02 | 1.91 | 3.32 | 2.00 | 2.78 (.049) |
| Driving after Drinking | 0.80 | 1.01 | 2.77 (.061) | 15.9% | 1.03 | 0.56 | 1.36 | 0.66 | 5.23 (.019) |
| Marijuana | 1.57 | 1.86 | 12.84 (.001) | 15.1% | 2.07 | 1.08 | 2.48 | 1.23 | 4.96 (.014) |
| Results for 12th Grade | |||||||||
| Outcome | Intervention Main Effect | Risk-Moderation Effect | |||||||
| I | C | F(1,72) (p) | RRR | I–H | I–L | C–H | C–L | F(1,78) (p) | |
| Lifetime Illicit Substance Use | 1.43 | 1.68 | 25.53 (.001) | 15.0% | 1.79 | 1.07 | 2.16 | 1.20 | 10.97 (.001) |
| Current Use | |||||||||
| Past Month Drunkenness | 0.41 | 0.44 | 1.40 (.120) | 5.9% | 0.51 | 0.31 | 0.55 | 0.32 | 1.18 (.140) |
| Past Month Cigarettes | 0.33 | 0.37 | 3.32 (.036) | 11.3% | 0.41 | 0.25 | 0.46 | 0.28 | 0.37 (.271) |
| Past Year Marijuana | 0.35 | 0.39 | 3.30 (.036) | 8.0% | 0.44 | 0.27 | 0.50 | 0.27 | 5.67 (.009) |
| Past Year Drive after Drinking | 0.25 | 0.26 | 0.24 (.318) | 4.9% | 0.32 | 0.17 | 0.33 | 0.18 | 0.06 (.405) |
| Past Year Inhalants | 0.04 | 0.06 | 3.18 (.039) | 28.3% | 0.05 | 0.03 | 0.06 | 0.05 | 0.10 (.374) |
| Past Year Methamphetamine | 0.03 | 0.04 | 4.55 (.018) | 31.4% | 0.04 | 0.02 | 0.05 | 0.03 | 0.26 (.305) |
| Frequency of Use | |||||||||
| Drunkenness | 2.86 | 3.00 | 1.34 (.125) | 3.4% | 3.44 | 2.28 | 3.67 | 2.33 | 1.79 (.092) |
| Driving after Drinking | 1.09 | 1.26 | 1.57 (.117) | 4.5% | 1.45 | 0.73 | 1.65 | 0.86 | 0.47 (.252) |
| Marijuana | 1.83 | 2.05 | 6.79 (.005) | 14.4% | 2.37 | 1.28 | 2.71 | 1.38 | 3.14 (.040) |
Means are model-based from multi-level repeated measure analyses of covariance (as described in the text). Model includes data collected from 2 successive cohorts of students enrolled in the 11th and 12th grades in 2008–2010; covariates were assessed at the 6th grade pretest (2002–2003); interventions were conducted in 2003–2005.
I: Intervention; C: Control; RRR: Relative Reduction Rate; I–H: Higher Risk at Intervention; I–L: Lower Risk at Intervention; C–H: Higher Risk at Control; C–L: Lower Risk at Control. Reported p-values are for 1-tailed tests; 2-tailed significance levels can be calculated by doubling the reported 1-tailed values.
Table 2.
Growth Trajectory Analysis (6th 12th grades) for Iowa and Pennsylvania sites, 2002–2010
| Outcome | Condition Main Effect F(1,12) (p) | Condition* Risk F(1,12) (p) | Condition* Time (Linear) F(1,72) (p) | Condition* Risk* Time (Linear) F(1,78) (p) |
|---|---|---|---|---|
| Lifetime Illicit Substance Use | 16.72 (.001) | 16.69 (.001) | 51.90 (.001) | 14.22 (.001) |
| Current Use | ||||
| Past Month Drunkenness | 1.47 (.124) | 2.80 (.059) | 2.32 (.066) | 1.76 (.094) |
| Past Month Cigarettes | 1.71 (.107) | 3.64 (.040) | 3.95 (.025) | 0.46 (.250) |
| Past Year Marijuana | 11.82 (.002) | 14.95 (.001) | 3.10 (.041) | 3.87 (.026) |
| Past Year Driving after Drinking* | 1.01 (.166) | 1.58 (.116) | N/A | N/A |
| Past Year Inhalants | 4.21 (.031) | 1.95 (.093) | 0.16 (.345) | 2.18 (.071) |
| Past Year Methamphetamine | 9.91 (.004) | 1.09 (.158) | 6.44 (.006) | 1.53 (.110) |
| Frequency of Use | ||||
| Drunkenness | 2.32 (.076) | 4.09 (.032) | 2.98 (.044) | 1.62 (.103) |
| Driving after Drinking* | 2.34 (.076) | 2.92 (.056) | N/A | N/A |
| Marijuana | 12.03 (.002) | 9.36 (.004) | 10.08 (.001) | 3.82 (.027) |
Measure only available at 11th and 12th grades, linear growth effects not calculated.
Reported p-values are for 1-tailed tests; 2-tailed significance levels can be calculated by doubling the reported 1-tailed values.
Current use/behavior
Point-in-time current use results are presented in Table 1; growth trajectory results are presented in Table 2. Significant intervention main effects were found at one or both time points for all current-use outcomes except those concerning alcohol (past-month drunkenness and past-year driving after drinking). Point-in-time intervention main effects were significant for past-month cigarette use, past-year marijuana use, and past-year methamphetamine use at both grades; effects on past-year inhalant use were significant at 12th grade only. Relative reduction rates for most current use outcomes showing significant intervention effects were in the 12% to 16% range; exceptions were past-year methamphetamine use at both grades (with relative reduction rates of approximately 31%), and past year inhalant use at 12th grade (28.3%).
Intervention effects were significantly stronger for higher-risk students at 11th grade for past-year marijuana use and past-year drinking after driving; they approached significance for past-month cigarette use. At 12th grade, Condition × Risk effects were significant only for past-year marijuana use.
Condition × Linear Time effects (growth) on substance use from 6th to 12th grade were significant for each outcome except past-month drunkenness and past-year inhalant use. Condition × Risk × Linear Time growth effects (larger intervention-control slope differences for higher-risk students) were significant for past-month marijuana use. In all instances, intervention effects were stronger for higher-risk students and showed larger intervention-control slope differences among higher-risk students.
Frequency of use/behavior
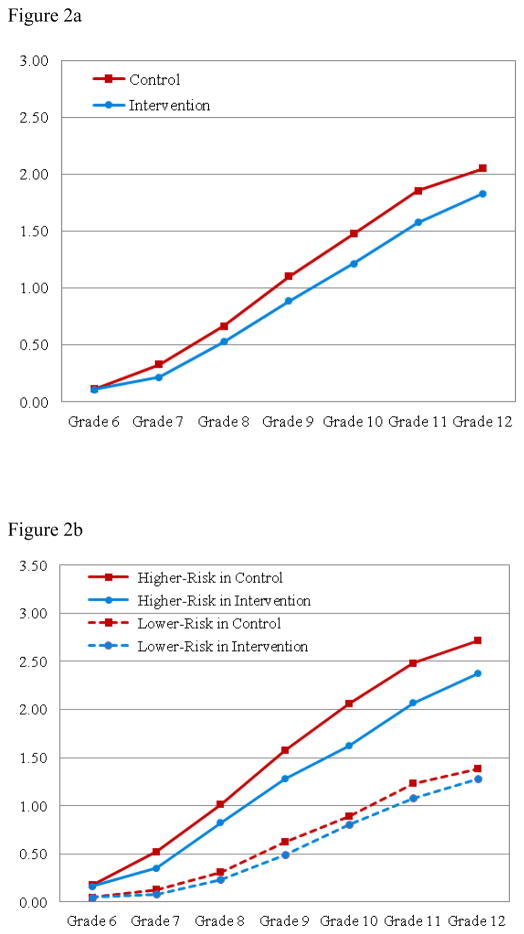
Frequency of use/behavior findings showed significant point-in-time intervention effects on marijuana use at both grades; relative reduction rates were 15.1% and 14.4% at the 11th and 12th grades (see Table 1). There also was significant risk moderation of intervention effects at both grades (Condition × Risk), with stronger effects for higher-risk students, as well as significantly slower growth in use among the intervention youth (Condition × Linear Time). Risk moderation of intervention effects on growth (Condition × Risk × Linear Time) also was significant. The Condition × Linear Time and Condition × Risk × Linear Time results for marijuana use are illustrated in Figures 2a and 2b.
Figure 2.
Figure 2a: Longitudinal growth results for frequency of marijuana use through 6.5 years past baseline.
Note: Frequency of marijuana use was scored on a seven-point scale, ranging from 0 (never) to 7 (more than weekly).
Figure 2b: Longitudinal growth results for frequency of marijuana use: Higher- vs. lower-risk subgroups.
Note: Higher risk = initiation of alcohol, cigarette or marijuana use prior to baseline; lower risk = no initiation at baseline.
Point-in-time intervention effects were observed for drunkenness (p = .046), with marginally significant (p = .061) effects for driving after drinking at 11th grade, but not at 12th grade. Corresponding 11th grade relative reduction rates were 3.3% and 15.9% for drunkenness and driving after drinking. Significant risk moderation of intervention effects (Condition × Risk) was found for both alcohol outcomes at 11th grade, with stronger effects for higher-risk students. Slower growth (Condition × Linear Time) in drunkenness for the intervention group was found for the full sample.
DISCUSSION
Overall, the effects of interventions delivered via the PROSPER partnership-based delivery system on long-term, adolescent substance use outcomes were robust, considering both growth across the middle- and high-school years, as well as point-in-time results for 5.5 and 6.5 years past-baseline. Positive long-term effects were observed for lifetime illicit use and for current use and frequencies of use, for all types of substances. Relative reduction rates for point-in-time outcomes ranged from 3.3% to 31.4%. Notably, intervention effects on growth in substance use from 6th to 12th grades were significant for all outcomes, except past month drunkenness (p = .066) and past-year inhalant use, with increasing intervention-control differences across time. It is noteworthy that both the intent-to-treat analyses and the use of non-iterative estimator calculations contribute to relatively conservative estimates of effects.
Although there were significant effects for frequency of drunkenness and marginally significant effects on driving after drinking at 11th grade, overall, effects on alcohol-related outcomes were relatively weaker. As previously noted (Spoth et al., 2011), this may be a consequence of the sensitivity of long-term intervention effects to baseline levels of use; higher levels of use at baseline constrain subsequent effects. Alcohol is the substance of choice among adolescents and a higher proportion of youth were drinking at baseline, compared with other types of use that are less normative. Earlier research suggests that higher proportions of users in a peer network increases use opportunities and other factors disposing non-users to initiate use. As concerns non-significant driving after drinking results in 12th grade, booster sessions during high school, targeting safe driving behavior, may be indicated.
Examination of risk-related moderation showed that intervention effects for the higher-risk subsample were comparable to or, in a majority of cases, stronger than effects for the lower-risk subsample. In fact, effects on marijuana use were primarily significant in the high-risk group. The findings address the contention that only lower-risk populations benefit from universal interventions (Spoth et al., 2006). Overall, this pattern suggests that the goal of producing main effects across the full spectrum of youth, including benefits specifically for higher-risk participants—is being realized.
Another aspect of the findings that warrants discussion is point-in-time outcomes at 11th grade, compared with those at 12th grade. The general pattern of intervention main effects was similar at both grades; however, point-in-time risk moderation of effects was more evident at 11th grade than at the later assessment. Additional investigation is needed to determine whether this pattern is due to diminishing intervention effects for higher-risk students, or to increased sample loss (e.g., school dropout, higher absenteeism) among the higher-risk subgroup, resulting in reduced power to detect effects.
To place these findings in context, it is important to reference three possible mechanisms of observed effects. The first is suggested by separate analyses of social network data reported by our participants. These analyses revealed that in middle school the interventions reduced the influence of adolescents who use substances on other students, by reducing the network centrality of substance-using youth (Osgood et al., unpublished results). The second potential mechanism is that the intervention had proximal positive effects on key putative mediators of substance misuse in later adolescence, including enhanced young adolescent skills, parenting, and family environment (Redmond et al., 2009). Finally, previous findings showed that early initiation of use was reduced by the intervention; early initiation is one of the most powerful predictors of later substance misuse. Earlier outcome reports showed relative delays in initiation among intervention group youth and such delays typically are associated with reduced substance misuse in late adolescence and young adulthood. This point underscores the age-related growth of substance use and the critical importance of the developmental timing of intervention. PROSPER community teams delivered the interventions when students were beginning to experiment with substance use, but before they moved to more frequent or serious use.
The relative reduction rates (RRRs) reflect potential public health significance. For this study a “caseness” approach to the RRRs was considered appropriate. Using the cutoff points described in the Methods section, RRRs ranged from 3.3% to 14.4%. For example, if the RRR for the frequency of marijuana use were to hold when scaling up the PROSPER partnership model, for every 100 general population 12th graders (in non-intervention school districts) using marijuana more often than yearly, approximately 86 students in PROSPER sites would be using at that frequency. Generalization to populations that differ in characteristics, such as ethnicity or geographic location, however, has not yet been established.
The combination of positive outcomes and the cost-efficiency of the PROSPER partnership model (Crowley et al., 2012; Spoth and Greenberg, 2011) suggests its potential public health value, particularly if future research supports generalizibility of findings to other populations. A recent National Research Council and Institute of Medicine Report (2009), along with other literature (Hawkins et al., 2008; 2012), note the practical benefits of community-based prevention delivery systems for EBIs, particularly those embedded in national delivery systems and/or those supporting practitioner-scientist partnerships (Grumbach and Mold, 2009; Spoth and Greenberg, 2011). These delivery systems, as illustrated by the PROSPER model, supported by the results herein, can facilitate more rapid, effective and efficient translation of the science of preventive health intervention into community practice.
Supplementary Material
Highlights.
We examine long-term effects of PROSPER, an evidence-based prevention system.
We measure lifetime, current, and frequency of misuse for a range of substances.
PROSPER reduced substance misuse; rates were up to 31.4% lower than the control.
There were greater intervention benefits for higher- versus lower-risk youth.
Partnership-based delivery systems have potential for public health impact.
Acknowledgments
Work on this paper was supported by the National Institute on Drug Abuse (grant DA 013709).
Footnotes
The authors have no conflict of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Botvin GJ. Life Skills Training and the prevention of adolescent drug abuse. In: Clark D, editor. Preparing Youth for the 21st Century. Washington, DC: The Aspen Institute; 1996. [Google Scholar]
- Botvin GJ. Life Skills Training. Princeton, NJ: Princeton Health Press; 2000. [Google Scholar]
- Botvin GJ, Baker E, Renick NL, Filazzola AD, Botvin EM. A cognitive-behavioral approach to substance abuse prevention. Addict Behav. 1984;9:137–147. doi: 10.1016/0306-4603(84)90051-0. [DOI] [PubMed] [Google Scholar]
- Crowley DM, Jones DE, Greenberg MT, Feinberg ME, Spoth RL. Resource consumption of a dissemination model for prevention programs: The PROSPER delivery system. J Adolescent Health. 2012;50:256–263. doi: 10.1016/j.jadohealth.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Ageton SS, Huizinga D, Knowles BA, Canter RJ. The prevalence and incidence of delinquent behavior: 1976–1980. Boulder, CO: Behavioral Research Institute; 1983. [Google Scholar]
- Gold MS, Bailey J. Addiction treatment: Science and policy for the twenty-first century. JAMA. 2008;299:2570–2571. [Google Scholar]
- Greenberg MT, Feinberg ME, Johnson LE, Perkins DF, Spoth RL. Factors that predict financial sustainability of community coalitions: Five years of findings from the PROSPER partnership project. Unpublished results. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grumbach K, Mold JW. A health care cooperative extension service: Transforming primary care and community health. JAMA. 2009;301:2589–2591. doi: 10.1001/jama.2009.923. [DOI] [PubMed] [Google Scholar]
- Hansen WB. Prevention programs: What are the critical factors that spell success?. Plenary session presented at the NIDA National Conference on Drug Abuse Prevention Research; September 19, 1996; Washington, DC. 1996. [Google Scholar]
- Harwood H. Updating estimates of the economic costs of alcohol abuse in the United States: Estimates, update methods, and data. Washington, DC: National Institute on Alcohol Abuse and Alcoholism; 2000. [Google Scholar]
- Harwood HJ, Bouchery E. NCJ-190636. Washington, DC: Office of National Drug Control Policy; 2001. The economic costs of drug abuse in the United States, 1992–1998. [Google Scholar]
- Hawkins JD, Catalano RF, Arthur MW, Egan E, Brown EC, Abbott RD, Murray DM. Testing Communities That Care: The rationale, design and behavioral baseline equivalence of the community youth development study. Prev Sci. 2008;9:178–190. doi: 10.1007/s11121-008-0092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW. Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Arch Pediatr Adolesc Med. 2012;166:141–148. doi: 10.1001/archpediatrics.2011.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2011. Ann Arbor: Institute for Social Research, The University of Michigan; 2012. [Google Scholar]
- Mathurin P, Deltenre P. Effect of binge drinking on the liver: An alarming public health issue? Gu. 2009;58:613–617. doi: 10.1136/gut.2007.145573. [DOI] [PubMed] [Google Scholar]
- McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: A systematic review of cohort studies. PLoS Med. 2011;8(2):e1000413. doi: 10.1371/journal.pmed.1000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller T, Hendrie D. DHHS Pub No (SMA) 07–4298. Rockville, MD: Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services Administration; 2008. Substance Abuse Prevention Dollars and Cents: A Cost-Benefit Analysis. [Google Scholar]
- Molgaard VM, Kumpfer K, Fleming E. Strengthening Families Program for Parents and Youth 10–14: A video-based curriculum. Ames, IA: Institute for Social and Behavioral Research; 1997. [Google Scholar]
- Molgaard V, Spoth R. Strengthening Families Program for young adolescents: Overview and outcomes. In: Pfeiffer SI, Reddy LA, editors. Innovative mental health programs for children: Programs that work. Binghamton, NY: The Haworth Press, Inc; 2001. pp. 15–29. [Google Scholar]; Co-published simultaneously as Residential treatment for children & youth. 3. Vol. 18. Binghamton, NY: Haworth Press; pp. 15–29. [Google Scholar]
- [Accessed 12–14–2009];National Institute on Drug Abuse. 2009 Retrieved from: http://www.nida.nih.gov/consequences.
- National Research Council and Institute of Medicine. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Committee on the prevention of Mental Disorders and substance Abuse Among Children, Youth and Young Adults; Research Advances and Promising Interventions. In: O’Connell MC, Boat T, Warner KE, editors. Board on Children, Youth and Families, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- Osgood DW, Ragan DT, Wallace L, Gest SD, Feinberg ME, Moody J. Peers and the emergence of alcohol use: influence and selection processes in adolescent friendship networks. Unpublished results. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond C, Spoth RL, Shin C, Schainker L, Greenberg M, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community-university partnership. J Prim Prevent. 2009;30:513–530. doi: 10.1007/s10935-009-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Quart. 1988;88(15):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Smith GT, McCarthy DM, Goldman MS. Self-reported drinking and alcohol-related problems among early adolescents: Dimensionality and validity over 24 months. J Stud Alcohol. 1995;36:383–394. doi: 10.15288/jsa.1995.56.383. [DOI] [PubMed] [Google Scholar]
- Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: Maintenance of community-based partnership recruitment results and associated factors. J Fam Psychol. 2007b;21:137–146. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg M. Impact challenges in community science-with-practice: Lessons from PROSPER on transformative practitioner-scientist partnerships and prevention infrastructure development. Am J Community Psychol. 2011;48:106–119. doi: 10.1007/s10464-010-9417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg MT, Bierman K, Redmond C. PROSPER Community-university partnerships model for public education systems: Capacity-building for evidence-based, competence-building prevention [Invited article for Special issue] Prev Sci. 2004;5:31–39. doi: 10.1023/B:PREV.0000013979.52796.8b. [DOI] [PubMed] [Google Scholar]
- Spoth R, Guyll M, Lillehoj CJ, Redmond C, Greenberg M. PROSPER study of evidence-based intervention implementation quality by community-university partnerships. J Community Psychol. 2007c;35:981–999. doi: 10.1002/jcop.20207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community-university partnerships: Randomized controlled trial outcomes 4½ years past baseline. Am J Prev Med. 2011;40:440–447. doi: 10.1016/j.amepre.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes four years following baseline. J Consult Clin Psychol. 2001;69:627–642. doi: 10.1037/0022-006X.69.4.627. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance use outcomes at 18 months past baseline: The PROSPER community-university partnership trial. Am J Prev Med. 2007a;325:395–402. doi: 10.1016/j.amepre.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Shin C, Guyll M, Redmond C, Azevedo K. Universality of effects: An examination of the comparability of long-term family intervention effects on substance use across risk-related subgroups. Prev Sci. 2006;7:209–224. doi: 10.1007/s11121-006-0036-3. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Greenberg MT. Toward a comprehensive strategy for effective practitioner-scientist partnerships and larger-scale community benefits. Am J Community Psychol. 2005;35:107–126. doi: 10.1007/s10464-005-3388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CL, Perry CL, Dudovitz B, Veblen-Mortenson S, Anstine PS, Komro KA, Toomey TL. A home-based prevention program for sixth-grade alcohol use: Results from Project Northland. J Prim Prev. 1995;16:125–147. doi: 10.1007/BF02407336. [DOI] [PubMed] [Google Scholar]
- Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299:211–213. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.