Abstract
Objective
Results of the Austrian MOBITEL (MOBIle phone based TELemonitoring for heart failure patients) trial indicate that home-based telemonitoring improves outcome of chronic heart failure (CHF) patients and reduces both frequency and duration of hospitalizations. Based on lessons learned, we assessed the weak points to clear the way for routine operations.
Methods
We analyzed the system with respect to recommendations of the ESC Guidelines and experiences gained throughout the trial to identify potential improvements. The following components have been identified: a patient terminal with highest usability, integrated way to document drug-intake and well-being, and automated event detection for worsening of CHF. As a consequence the system was extended by Near Field Communication (NFC) technology and by an event management tool.
Results
Usability evaluation with 30 adults (14f, median 51y. IQR[45-65]) showed that 21 (8f) were able to immediately operate the system after reading a step-by-step manual. Eight (6f) needed one time demonstration and one man (80y) failed to operate the blood pressure meter. Routine operation of the revised system started in March 2009. Within 9 months, 15 patients (4f, median 74y. IQR[71-83], all NYHA-III) transmitted 17,149 items. 43 events were detected because of body weight gain of more then 2kg within 2 days. 49 therapy adjustments were documented. Three patients stopped using the system, two (1f) because of non-compliance and one (m, 82y) because of death. Overall, the rate of adherence to daily data transfer was 78%.
Conclusion
First results confirm the applicability of the revised telemonitoring system in routine operation.
Keywords: Heart failure, telemedicine, mobile phone, eHealth, near field communication technology
Introduction
Chronic Heart Failure (CHF) is a progressive disease with a high rate of hospital readmission caused by recurrent cardiac decompensation. Worsening CHF accounts for 5% of all hospital admissions with a readmission rate of about 50% in the first six months after the initial event [3-5]. The mean age of patients with CHF in developed countries is about 75 years and the prevalence in people aged 70 to 80 years is between 10 and 20% [2]. The overall prevalence of CHF is increasing due to demographic change and effects of improvements in medical treatment (e.g. increased survival after a coronary event) [2]. In general, the prognosis of patients with CHF is poor with a mortality rate of 50% after 4 years [6, 7]. In addition, Steward and McMurray showed that CHF accounts for about 2% of national expenditures in health with 69% being spent for hospital care due to high admission rates [8, 9].
As discussed in the “Guidelines for diagnosis and treatment of acute and chronic heart failure 2008” of the European Society of Cardiology (ESC Guidelines) [2], follow-up after hospitalization are frequently insufficient leading to inadequate support for patients at home and suboptimal treatment. Furthermore, CHF patients have low adherence to medical regimes and poor recognition of early signs of cardiac decompensation [10].
To improve the delivery of care after hospitalization, emphasis should be taken to shift the focus from acute episodes of illness toward stable chronic conditions. The guidelines recommend heart failure management programs with class Ia and level of evidence Ab for both CHF patients with recent hospitalization and high-risk patients. The recommendations of the ESC follow the final goal to empower the patient taking self-care actions if possible [2]. Various specific needs according to severity of CHF, social environment and cognitive ability of each individual patient have to be taken into account before including a patient into a specific program. Focusing on telemonitoring services, the following basic components and measures should be provided irrespective of specific requirements of a local health care provider:
-
1.
Telemonitoring should increase the accessibility of healthcare services, thus avoiding isolation of the patient at home. The service should support the patient-physician-contact whenever necessary.
-
2.
Equipment and devices should not only allow for monitoring of quantitative parameters (e.g. blood pressure, heart rate, body weight) but should also include symptom monitoring. This could help to interpret variations of the parameters and to educate patients in their ability to take appropriate self-care actions based on their own sense.
-
3.
The telemonitoring system should support flexible adjustment of diuretic use to allow for appropriate adaptations of the dosage.
-
4.
Follow-up at home should start as early as possible after discharge from the clinic.
-
5.
Sustainable patient education with special emphasis on adherence and self-care management should be supported.
The results of the randomized, controlled Austrian MOBIle phone based TELemonitoring for heart failure patients (MOBITEL) trial already indicated significant improvements of patient outcomes [1]. Reduced frequency and duration of heart failure hospitalizations compared to patients in the control group have been reported. The system used in the MOBITEL trial comprised of mobile phone based telemonitoring equipment for the patients, a remote data centre for automated data analysis and alert notification as well as a secure internet based graphical user interface for attending physicians. After self-assessment of blood pressure, heart rate and body weight patients were advised to enter the data together with their daily dose of heart failure medication using the keypad of the mobile phone. At the monitoring centre an automatically running algorithm checked whether body weight gain exceeded a threshold of 2 kg within 2 days and – if so – a notification was sent to the physician via email. Via a secure website physicians could access both numerical and graphical representations of data for individual patients. Whenever necessary, study physicians could give telemedical advice to the patients. Despite the promising results, some weaknesses of the system have been discussed in the paragraph lessons learned: (1) data entry via the keypad of the mobile phone was an insurmountable hurdle for 18% of the patients although the mean age of the patients in the MOBITEL trial was about 66 years, which is about eight years below the mean age of typical CHF patients, (2) several patients were not able to enter the daily dosage of the taken heart failure medication, and (3) notification about detected events via email sometimes resulted in a flood of emails due to inappropriately adjusted thresholds.
The objective of the present paper has been to elaborate on potential improvements and to describe modifications that had to be implemented before routine operation and to report on the initial experience with the resulting telemonitoring solution.
Methods
Analysis of patient eligibility for telemonitoring within the MOBITEL trial
Inclusion criteria in the MOBITEL trial were acute cardiac decompensation with hospital admission and age between 18 and 80 years. Patients with inabilities to read the display of a handheld phone were not eligible. The total patient group had a median age of 66 years. Although all patients fulfilled the criteria, twelve (18%) were unable to manage daily data acquisition (“never beginners”). According to the feedback of the never beginners, the primary reason was the inability to operate the mobile phones’ Internet browser via the keypad. Some patients failed to enter the daily dosage of CHF medication. As a consequence we looked for new technologies to keep the advantages of mobile phones but to overcome the hurdle of data entry via the keypad.
Improvement of usability of the patient terminal for elderly unskilled patients by utilizing Near Field Communication (NFC) Technology
Near Field Communication (NFC) might be the technology of choice. Unlike Bluetooth, NFC supports a touch-based method for data acquisition [11] without device pairing. In addition to data acquisition from medical devices, it provides access to data stored on radio frequency identification (RFID) tags (e.g. electronic barcodes), which can be used for acquisition of non quantitative data, too (e.g. information about medication intake or well-being of the patient). A special blood pressure monitor (UA 767 plus NFC, AND, Japan) (►Figure 1) and an NFC extension box to a body weight scales (UA 321, AND, Japan) have been developed in order to enable CHF patients collecting their data by touching sensor devices with a NFC-enabled mobile phone. A contactless Smart-Card (ID card) was used to identify the patient and to launch the JAVA software application installed on the mobile phone. A symbol based patient questionnaire concept (►Figure 2) was designed for answering questions displayed on the mobile phone by touching the appropriate symbols on the icon table. The first row of the icon table consists of four icons related to medication intake (“dosage taken as indicated”, “higher dosage taken”, “lower dosage taken”, or “not taken today”). The three different smiley icons in the second row are used to capture the well-being condition. Each icon consists of an inlaid RFID tag that stores the same information electronically as indicated by the respective symbol.
Figure 1.

Blood pressure meter UA-767 Plus NFC (AND, Japan) with integrated NFC module (AIT Austrian Institute of Technology, Austria) to allow for wireless transmission of measurement values based on the ISO 14443 standard.
Figure 2.
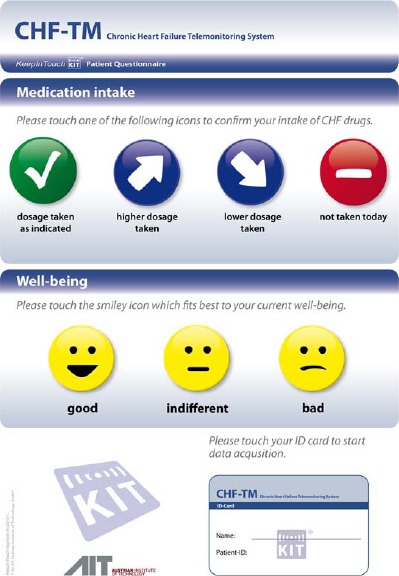
Icon table of the symbol based patient questionnaire concept with inlaid RFID-tags to indicate about medication intake and well-being condition.
►Table 1 shows a step-by-step workflow for structured and easy data acquisition that was designed and implemented in a JAVA application running on off-the-shelf available NFC enabled mobile phones (Nokia 6131 and 6212, Nokia Finland). NFC is a wireless connectivity technology evolving from a combination of contactless identification and networking technologies. It is based on magnetic inductive coupling, works in the unlicensed frequency band of 13.56 MHz and enables convenient short-range communication between electronic devices and smart objects. The short communication range of only a few centimeters is the major feature of this technology, because it enables rapid and easy communications between two NFC enabled devices just by bringing them close together. NFC is intended to be integrated in various types of consumer devices, in particular in handheld devices like mobile phones.
Table 1.
Step-by-step workflow for the acquisition of body weight, blood pressure, heart rate, medication intake, and well-being by the patient using NFC technology (BW … body weight, BP … blood pressure, HR … heart rate).
| Step | Interaction by the patient | Behavior of mobile phone application |
|---|---|---|
| 1 | measure BW, BP and HR | |
| 2 | touch ID card | application launch, user authentication next: ask for BW |
| 3 | touch NFC interface box of BW scales | read BW data next: ask for BP and HR data |
| 4 | touch BP meter | read BP and HR data next: ask for CHF medication |
| 5 | touch one of the following icons to confirm intake of CHF drugs
|
read the tag data of the touched icon next: ask for next CHF drug (repeat step 5, up to 4 times) or next: ask for well-being (continue with step 6) |
| 6 | touch the smiley icon which fits best to the current well-being
|
read the tag of the touched icon next: transmit all data and close application |
For flexible adjustment of CHF medication, any documented change in the drug regime was directly pushed to the patient terminal. The system was extended by an integrated workflow (►Table 2) in order to display the relevant CHF medication including the dosage on the mobile phone. The patient had to confirm the medication intake by touching one the four icons with the mobile phone. After the documentation of the medication a question about the well-being was displayed that also could be answered by touching the smiley icon which fits best to the current well-being of the patient (“good”, “indifferent”, or “bad”).
Table 2.
Workflow to document the adjustments of CHF medication and automatically notify the patient about the changes.
| Step | Web interface (physician or nurse) | Mobile interface (patient) |
|---|---|---|
| 1 | Document adjustment of CHF medication
|
|
| 2 | Send short message (SMS) to indicate adjustments of CHF medication | |
| 3 | Touch ID card to launch application and press OK to download new settings as indicated on the screen next: Application asks for BW data, etc.(continue with workflow as described in ►Table I) |
|
Analysis of user feedback
Patients of the MOBITEL trial were recruited at eight public hospitals in Austria with 19 physicians being responsible for patient monitoring. During the course of the study, interviews were performed with most of the physicians in order to assess hands-on user experiences. The following issues have been figured out as potential improvements:
-
1.
Because of off-limit conditions, a notification was sent via email to the responsible physicians of the hospital where the patient had been recruited. Basically, this helped to focus the attention to patients who probably needed advice. However, it happened that a flood of notifications (emails) was generated due to inappropriately adjusted thresholds for some patients.
-
2.
The common sense about the necessity to integrate general practitioners (GP) and home care nurses (i.e. extramural care givers) into the monitoring scenario. Due to the fact that prescription of medication is one of the responsibilities of GPs, integrated information exchange between physicians responsible for monitoring and GPs should be supported by the system. For patients with limited cognitive abilities, home care nurses might use the patient terminal to send the data necessary for enhanced telemedical treatment support.
Automated event detection and management tool
The issue of alerts management in everyday clinical needs was solved by establishing an event list as a central element of the user interface. All authorized users (physicians as well as specifically educated nurses) of the system were presented a structured list of all patients with at least one event. The events were categorized in off-limit condition, missing values and weekly check. All new monitoring data was immediately compared to given thresholds resulting in off-limit condition events, if indicated. The event ‘missing values’ was generated in the absence of new data at a given time. Weekly assessments of the monitoring data was guaranteed by weekly check events attributed to each patient in a seven-day cycle. An automated event detection algorithm managed the daily update of the event list. The physician could individually adjust any parameter of the algorithm (e.g. manually entered or automatically generated thresholds, trends, time intervals) for each patient. Through the daily processing of the event list, an optimized distribution of attention was given in a reasonable time without neglecting individual patients. The physician acknowledged the individual events after inspection of the corresponding monitoring data. If necessary, the physician could trigger an intervention, which also had to be documented in the system.
Legal and organizational aspects for protection of human subjects
In additional to technical improvements, legal and organizational measures had to be prepared in corporation between the technical (AIT Austrian Institute of Technology GmbH, Graz, Austria) and medical (Allgemein öffentliches Krankenhaus der Elisabethinen Linz GmbH, Linz, Austria) service provider. According to the Austrian data protection law [12], the application was registered by the Austrian data protection committee. Terms of use for responsible physicians as well as for patients were defined. A workshop was held to educate physicians in operation of the system and to instruct patients in using the telemonitoring devices. Patients were informed about potential usage of anonym data for scientific purpose. Informed consent was signed by all patients. For immediate technical questions a help-desk was set up for second level support of patients and first level support of physicians. An integrated device management tool was developed to allow for efficient handling of the telemonitoring equipment directly at the hospital. Together with the medical director of the hospital it had been decided that the outpatient clinic for cardiovascular disease should be announced to be both the entry point for new CHF patients and the primary contact point for routine patient support. Patients’ adherence to the telemonitoring system was expressed as the ratio of effectively received to expected data sets.
Results
Result from usability evaluation of patient terminal
Usability evaluation was performed with 30 untrained adults (14f, median 51y. IQR [45-65]). All persons received the modified, NFC based telemedicine equipment and a graphical step-by-step manual. 97% (29 out of 30) were able to operate the system appropriately, 21 (8f) immediately after reading the step-by-step manual only, eight (6f) needed one time demonstration about how to read out data values from the devices by touching the device with the mobile phone appropriately. One male (80y) failed to operate the blood pressure meter and did also not manage to operate the mobile phone.
Result from routine operation
The telemonitoring system (►Figure 3) started operation at the hospital of Elisabethinen, Linz, on March, 1st 2009. During a period of 9 months 15 CHF patients (4 females, median age 73 years, IQR [71-83]) which had been hospitalized because of cardiac decompensation were admitted to the service before discharge. Patients were educated how to use the devices properly in groups of two to four. They were advised to send their data once a day. Patient equipment consisted of blood pressure meter (UA 767 plus NFC, AND, Japan), a body weight scales (UA 321, AND, Japan) including an NFC interface box (AIT Austrian Institute of Technology GmbH, Austria), a personal ID card, an icon table and a mobile phone (Nokia 6131 NFC, Nokia, Finland). First results are summarized in ►Table 3. During this period 17,149 (median 1,290, IQR [500-1,734] per patient) data items were received in the course of 2,043 data transmission sessions (median 166, IQR [60-197] per patient). In 2,043 out of the 2,879 cumulative patient monitoring days a complete set of values was sent which resulted in a patient adherence rate of 78%. Until now, three patients stopped using the system, two (1f) didn’t want to operate the system every day and one (m, 82y) because of death. 43 off-limit events were detected because of body weight gain more then 2 kg within 2 days leading to 49 documented adaptations of the drug regimen.
Figure 3.
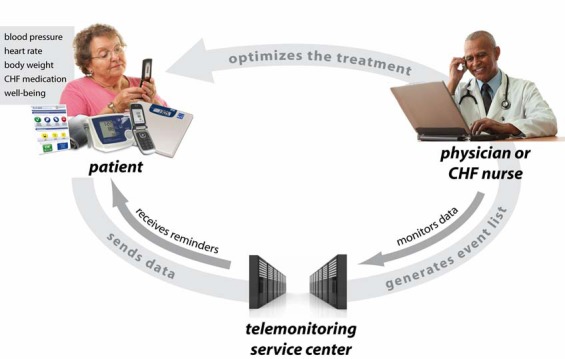
Schematic depiction of the telemonitoring system. After self-assessment of blood pressure, heart rate and body weight, patients were advised to transfer the data together with a confirmation of drug intake and information about their personal well-being via the mobile phone. Physicians and specifically educated nurses had access to a secure website of the telemonitoring service centre providing both numerical and graphical representations of the data. Whenever necessary, treating physicians could contact patients using the mobile phone.
Table 3.
Results from routine operation of the telemonitoring system at the hospital of Elisabethinen, Linz. From March, 1st until November, 30th 2009 15 CHF patients (four females) were admitted to the service. Patient adherence was expressed as a percentage of expected to effectively received data sets.
| Parameter | Total | Median per patient [IQR] |
|---|---|---|
| Patients (female) [n] | 15 (4) | |
| NYHA classification [I – IV] | 3 [3-3] | |
| Age [years] | 74 [71-83] | |
| Monitoring period [days] | 2,879 | 213 [164-263] |
| Transmissions [n] | 2,043 | 166 [60-197] |
| Received data items [n] | 17,149 | 1,290 [500-1,734] |
| Detected events because of body weight gain more then 2 kg within 2 days [n] | 43 | 1 [0-3] |
| Adjustments of medication [n] | 49 | 3 [2-6] |
| Patients’ adherence rate [%] | 78 |
Physicians were advised to check the event list at least once a day. Telemedical assessment of the patients’ health status was supported by numerical tables and trend charts (►Figure 4).
Figure 4.
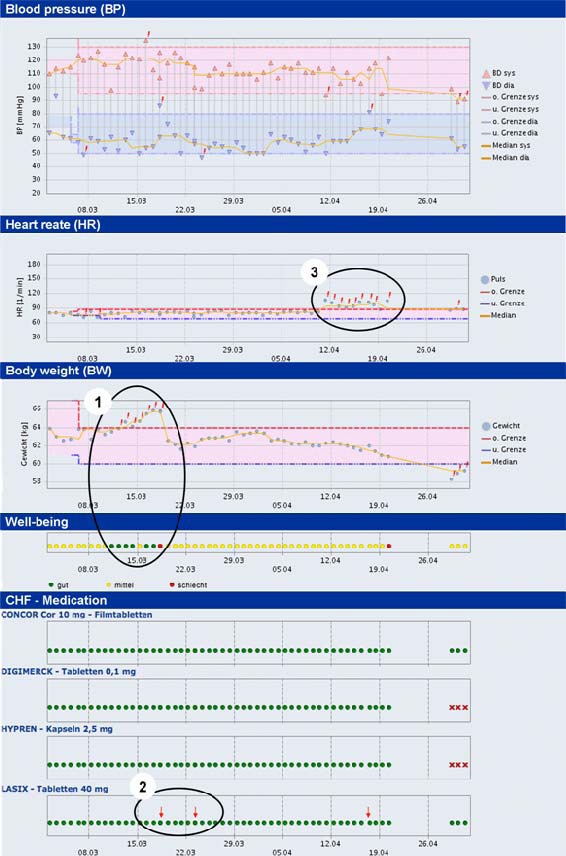
Typical trend chart of a patient (male, 82 years) over a period of about two months of telemedical follow-up. Each dot represents a transmitted value of (from top to bottom) systolic and diastolic blood-pressure, heart rate, body weight, well-being, and CHF medication.
Episode 1) Increase of body weight led to off-limit conditions indicated by red exclamation marks. During the first days of this episode the patient indicated his well-being status mostly with “good” follow by “bad” on the day before the intervention.
Episode 2) Physicians reacted on the trend and temporarily increased the dosage of diureticum indicated by the red arrows resulting in a reduction of the body weight.
Episode 3) Because of an ongoing increase in heart rate over a period of eight days the patient was hospitalized to examine the presence of cardiac arrhythmia. Again the patient indicated “bad” well-being on the last day before hospital admission.
Discussion
The utilization of telemonitoring services for CHF patients in routine operation is an important step toward achieving “continuity of care” from the clinics to the patients’ home. Telemonitoring in general has already been shown to provide a powerful solution to detect early warning signs for worsening of CHF [13]. However, there are still uncertainties about the proper monitoring tool. A simple tool for monitoring body weight did not show consistent results [14] but led to further developments.
The results of the usability evaluation supported the expectations that NFC may be the enabling technology for intuitive data acquisition. This solution empowered even elderly, technically unskilled patients to perform the necessary steps in order to take advantage of CHF monitoring. Both, acquisition of quantitative data like blood pressure, heart rate, and body weight as well as qualitative, therapy and symptom-relevant information like well-being or the confirmation of drug intake were integrated parts of the device equipment. Other than in the MOBITEL trial, where contract research associates were in charge of individual patient training, patients were now educated in the appropriate use of the NFC based telemedicine equipment by physicians or nurses just before discharge. At home the devices provided “out of the box” connectivity i.e. no setup of telephone line or device connection (e.g. Bluetooth pairing) had to be done. Although the overall rate of adherence was about 17% below the result of the MOBITEL trial, the number of transmissions was still very high and the average age of the patients now was 8 years older. The cause of more than 50% of missing data values was actually a technical problem (software bug) during the first month of operation. An additional essential component of the telemonitoring-system, potentially influencing the therapy of the patient, was the event detection algorithm for focusing the doctors’ attention to patients with one or more off-limit conditions. The experience in the proper alignment of thresholds was of importance to detect the true-positive events and to prevent them from disappearing in a flood of false-positive events. The setting of the default thresholds had been based on the experience of the previous MOBITEL trial. Nevertheless, the patient had to be informed that in the case of acute worsening health conditions the general practitioner or emergency doctor had to be contacted immediately, because the telemonitoring system was not intended for emergency use.
Limitations
By now not enough data has been collected to judge the medical benefits (e.g. the number of read-mission because of worsening of heart failure). Furthermore, experiences exist for only a single hospital so far. Therefore, further adaptation might be necessary to cope with diverse patient management scenarios from different care givers.
Conclusion
Results of the Austrian MOBITEL trial and the experiences gained by the attending physicians and patients have been analyzed. Usability evaluation with untrained persons confirmed the improvements of the patient terminal for elderly unskilled patients by utilizing NFC Technology. A revised version of the system was successfully launched in March, 2009 at the hospital of Elisabethinen, Linz. During the first 9 months of operation, data was acquired from 15 CHF patients. The median age of 74 years supports the assumption that the usability problem for elderly and technically unskilled patients could be resolved. The event detection algorithm and the integrated event list render possible to use the system in daily clinical routine. Active integration of extramural care givers remains a challenging part for collaborative treatment of CHF patients.
Conflict of interest statement
None of the authors have any conflicts of interest associated with the work presented in this manuscript.
Footnotes
References
- 1.Scherr D, Kastner P, et al. , and the MOBITEL investigators Effect of Home-Based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients After an Episode of Acute Decompensation: Randomized Controlled Trial, J Med Internet Res 2009; 11(3): e34.URL: http://www.jmir.org/2009/3/e34/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dickstein K, Cohen-Solal A, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008; 29(19): 2388-2442 [DOI] [PubMed] [Google Scholar]
- 3.Komajda M, Follath F, et al. The euroheart failure survey programme – a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur Heart J 2003; 24(5): 464-474 [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Parent EM, et al. Readmission after hospitalization for congestive heart failure among medicare beneficiaries. Arch Intern Med 1997; 157: 99-104 [PubMed] [Google Scholar]
- 5.Martinez A, Everss E, et al. A systematic review of the literature on home monitoring for patients with heart failure. Journal of Telemedicine and Telecare 2006; 12: 234-241 [DOI] [PubMed] [Google Scholar]
- 6.Rich M, Beckham V, et al. Repetitive hospital admissions for congestive heart failure in the elderly. Am J Geriatr Cardiol 1996; 5(3): 32-36 [PubMed] [Google Scholar]
- 7.Cleland JG, Gemmell I, et al. Is the prognosis of heart failure improving? Eur J Heart Fail 1999; 1: 229-241 [DOI] [PubMed] [Google Scholar]
- 8.Stewart S, Jenkins A, et al. The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail 2002; 4(3): 361-371 [DOI] [PubMed] [Google Scholar]
- 9.McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart 2000; 83: 596-602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Wal MH, Jaarsma T, et al. Non-compliance in patients with heart failure; how can we manage it? Eur J Heart Fail 2005; 7(1): 5-17 [DOI] [PubMed] [Google Scholar]
- 11.Morak J, Kollmann A, et al. Feasibility and usability of a home monitoring concept based on mobile phones and near field communication (NFC) technology. Medinfo 2007; 12(Pt 1): 112-116 [PubMed] [Google Scholar]
- 12.Jahrbuch der Gesundheitsstatistik 2006, Statistik Austria. Available from: http://www.statistik.at/dynamic/wcmsprod/idcplg?IdcService=GET_NATIVE_FILE&dID=50610&dDocName=028435
- 13.Clark RA, Inglis SC, et al. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007; 334(7600): 942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg LR, Piette JD, et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: The Weight Monitoring in Heart Failure (WHARF) trial. Am Heart J 2003;146: 705-712 [DOI] [PubMed] [Google Scholar]


