Abstract
Background
There is increasing recognition that a competent and well-trained workforce is required for successful implementation of health information technology.
Methods
New and previous research was gathered through literature and Web searching as well as domain experts. Overall themes were extracted and specific data collated within each.
Results
There is still a paucity of research concerning the health information technology workforce. What research has been done can be classified into five categories: quantities and staffing ratios, job roles, gaps and growth, leadership qualifications, and education and competencies. From several countries it can be seen that substantial numbers of individuals are needed with diverse backgrounds and competencies.
Conclusions
Additional research is necessary to determine the optimal organization and education of the health information technology workforce.
Keywords: Health information technology, biomedical and health informatics, clinical informatics, workforce
Introduction
There is a growing recognition worldwide that an essential component for the successful deployment of health information technology (HIT) is a competent workforce. This is most evident from efforts that have focused on implementing HIT on a national scale. The first such effort was the Connecting for Health program in England, where the need for attention to the workforce was recognized early [1]. Subsequent efforts in other developed countries have also recognized this need [2, 3]. More recently, the substantial investment in the United States to achieve widespread “meaningful use” of the electronic health record (EHR) funded by the Health Information Technology for Economic and Clinical Health (HITECH) Act of the American Recovery and Reinvestment Act (ARRA) includes investment in workforce development [4]. Even in developing countries, the essential need for a well-trained workforce has become clear [5].
Despite the identified need, we know very little about how the HIT workforce is organized in different healthcare settings. This was determined from a review of the literature performed in late 2007 [6]. That study also found that knowledge of the quantities and activities of such a workforce was lacking. In addition, it determined that we know even less about the proper role for individuals who are trained in clinical (or related) informatics disciplines, including what jobs need knowledge and skills in clinical informatics or how much the non-informatics workforce needs to know about clinical informatics. The goal of this paper was to update the previous review of the literature, further analyze the literature in a new framework, and use that framework to elucidate further research and policy questions that still must be answered.
One example of the need for a competent workforce comes from a widely cited study reporting negative findings with computerized provider order entry (CPOE). In late 2005, Han et al. reported an increased mortality rate after implementation of CPOE in the pediatric intensive care unit (ICU) of Children’s Hospital of Pittsburgh [7]. Further investigation of the environment studied, however, demonstrated that its CPOE implementation failed to adhere to known best practices [8, 9]. The organization’s centralization of the pharmacy, installation of the system without adequate network and computational resources, and not permitting order entry prior to the patient arriving at the ICU were mistakes that those familiar with known best practices for CPOE would have avoided. Indeed, several other pediatric hospitals looked at their own data and failed to find increased mortality after CPOE implementation [10-13]. Other studies have documented the importance of “special people” in successful HIT implementations [14].
Another “data point” about the HIT workforce is the finding from the original [15] and follow-up [16] systematic reviews on the benefits of HIT interventions that 20-25% of all studies done have come from four US institutions. This raises questions about the generalizability of documented benefits, including whether other healthcare institutions will have the workforce to repeat their successes.
It is increasingly recognized that a well-trained HIT professional should have knowledge not only of information technology, but also of healthcare, business and management, and other disciplines. One survey of 91 healthcare chief information officers (CIOs) found that 88% agreed that understanding of healthcare environment was essential to IT practice in healthcare settings [17]. An earlier study that surveyed health system managers found a preference for those with clinical experience, understanding of healthcare, strong communication skills, and ability to work across boundaries within organizations [18].
An additional challenge is that we have little data that characterizes the HIT workforce and, in particular, how it is best trained and deployed for optimal use of the technology. A related problem is the traditional view in most hospitals and other healthcare settings to think separately of IT professionals, whom are mostly viewed as technologists, and health information management (HIM) professionals, who are mostly viewed as maintaining the (usually paper) medical record. This approach not only creates artificial distinctions, but also ignores the role that others play in HIT, in particular the increasing prevalence of clinical informatics professionals [19].
Another challenge is that some job categories, most notably clinical informatics, are not represented in standard occupational classifications, which results in these professionals not being represented in some types of workforce analyses. In the US, the Standard Occupational Classification (SOC) has codes for Health Diagnosing and Treating Practitioners (29-1000), Medical Records and Health Information Technicians (29-2070), and Computer Specialists (15-1000), but nothing that combines these elements of what the myriad of heterogeneous clinical and other informaticians do into a single code [20]. The same holds for the International Standard Classification of Occupations (ISCO, http://www.ilo.org/public/english/bureau/stat/isco/), which also has no codes for informatics [21].
In this analysis, we searched for all research data that could provide insight into the quantity, activities, and gaps of the HIT workforce. After developing a framework for analyzing this data, we developed recommendations for policy recommendations as well as further research.
Methods
We updated our previous review by searching for new data on the HIT workforce in both the peer-reviewed literature (Pubmed) as well as the general Internet (Google). From the information retrieved, we also pursued citations to additional possible sources. In addition, we consulted experts with knowledge of research looking at the HIT workforce. Unlike the previous review, we developed a framework for analysis and recommendations. We also searched for and assembled a collection of all documents making recommendations for competencies in biomedical and health informatics for various professionals, including HIT, informatics, and healthcare professionals.
Results
The number of studies analyzing the HIT workforce is still both small and heterogeneous in scope. We identified countrywide studies from three English-speaking countries: England [1], Australia [2], and Canada [3]. We also identified eight analyses from the United States that looked at various sub-groups of the HIT workforce [4, 22-28]. From these studies, we developed a new framework for collating the data that included:
-
•
Quantities and staffing ratios
-
•
Job roles
-
•
Gaps and growth
-
•
Leadership qualifications
-
•
Education and competencies
Our framework was orthogonal to but not in conflict with a previous classification of three broad categories of HIT professionals that segmented their work into “academic” and “professional” roles [29]. For the purposes of this analysis, we used our previous definition of biomedical and health informatics (hereafter called informatics) as the overarching descriptor for the field, with clinical informatics viewed as the subset focused on informatics in healthcare settings [30]. While clinical informatics, like all branches of informatics, historically was led by individuals in the academic category, there is now most growth in the professional category, as healthcare and other organizations increasingly hire individuals into operational roles [31].
One challenge for professional roles in informatics is the lack of professional recognition. One analysis found that informatics has some but not all of the attributes that characterize professions, such as a well-defined set of competencies, certification of fitness to practice, shared professional identify, life-long commitment to the discipline, and a code of conduct [32]. Again, some of the most active leadership comes from England, where the establishment of professional identity has been a goal of the NHS [33]. In the US, the nursing profession historically has had certification [34], and there is now a proposal to establish medical board sub-certification [35-37].
Quantities and staffing ratios
The three countrywide assessments we identified attempted to quantify the number of HIT workers in their entire healthcare systems. Each study took a somewhat different approach, from its definition of worker types to how the counting and analysis was done. The earliest assessment was carried out in the English National Health Service (NHS) [1]. The study focused on the “health informatics” workforce but essentially counted all individuals who played any role in information systems. This assessment of the English workforce estimated the employment of 25,000 full-time equivalents (FTEs) out of 1.3 million workers in English NHS (and a general population of about 50 million). This equated to the employment of about one information technology (IT) staff per 52 non-IT workers.
The Australian analysis also focused on the “health informatics” workforce that included all individuals who were involved in health information systems [2]. This study estimated a workforce of about 12,000 individuals in a country with a population of about 21 million. The study made several attempts to estimate staffing ratios of informatics personnel to all healthcare personnel using different data, with most of them yielding ratios comparable with England of about one IT staff per 50 non-IT workers.
The analysis from Canada also focused on the entire system but also classified individuals into occupational groups, separating out, for example, IT and clinical informatics [3]. The study estimated about 32,450 HIT professionals in Canada, although did not provide overall numbers of healthcare professionals that would allow determination of staffing ratios. The population of Canada is about 33 million.
Studies of the HIT workforce in the US have focused on specific professional groups. Most analyses have focused on characterizing job roles rather than quantifying them. Many of these studies have also focused on specific care delivery settings, such as hospitals or integrated delivery systems.
Some studies have analyzed IT professionals. Gartner Research has focused on IT personnel in integrated delivery systems. Its most recent analysis of 40 integrated delivery systems found a staffing ratio of one IT staff per 48 non-IT staff [25]. Another study extrapolated data from a self-report database of hospital-focused IT attributes, the HIMSS Analytics Database™ (http://www.himssanalytics.com). This database contains self-reported data from about 5,000 US hospitals, including elements such as number of beds, total staff full-time equivalent (FTE), total IT FTE (as well as broken down by major IT job categories), applications, and the vendors used for those applications. The analysis found the overall IT staffing ratio to be 0.142 IT FTE per hospital bed. Extrapolating to all hospitals beds in the US, this suggested a total current hospital IT workforce size of 108,390 FTE. It also found an IT to total staff ratio of 60.7, which was similar to the various studies described above [26].
Analyses from the US Bureau of Labor Statistics have assessed the HIM workforce, although the statistics only include Registered Health Information Technology (RHIT, trained in community colleges) and not Registered Health Information Administrator (RHIA, having baccalaureate degrees) workers [28]. The most recent analysis estimated current employment at 172,500.
Another study took a somewhat orthogonal view and focused on individuals needed to build and maintain the Nationwide Health Information Network (NHIN) in the US. [24]. For a five-year implementation time frame, there would be an estimated need for 7,600 FTE for installation of EHRs for 400,000 practicing physicians who do not currently have them, 28,600 FTE for the 4,000 hospitals that do not have EHRs, and 420 FTE to implement the infrastructure to connect the network. Similarly, the Office of the National Coordinator for HIT (ONC) has estimated that the goals for EHR adoption in the HITECH legislation would require 50,000 new personnel [4].
There have also been some “ballpark” estimates of the clinical informatics workforce in the US. The American Medical Informatics Association 10x10 program is based on the assertion that there should be at least one physician and one nurse trained in medical informatics in each of the 6,000 hospitals in the US [38]. Dr. Charles Friedman of the ONC has estimated a need for 1,000 public health informaticians needed in federal, state, and local public health organizations (Keynote Address, Public Health Information Network, August 26, 2007). He used similar principles to estimate a need for 13,000 clinical informaticians [39].
Workforce Roles
Some of the previously described studies have attempted to identify and quantify the workforce roles within the groups studies. The English NHS study, for example, found workers to be distributed among information and communication technology staff (37%), health records staff (26%), information management staff (18%), knowledge management staff (9%), senior managers (7%), and clinical informatics staff (3%) [1].
The Australian study classified jobs into two broad categories, although noted that many individuals work in more than one role, either within or across the categories [2]:
-
1.
Those who work “in the system,” e.g., to paraphrase: records, analysis, direct, decision, communications, and training
-
2.
Those who work “on the system,” e.g., to paraphrase: systems, info structure, improvement, education, resource, and administration
The Canadian study broke individuals down among job categories as follows (approximately) [3]:
-
1.
Information Technology – public sector 11,000-13,000, private sector 5,000-6,000
-
2.
Health Information Management – 4,300-5,800
-
3.
Project Management – public sector 760-900, private sector 1,100-1,300
-
4.
Organizational and Behavioral Management – public sector 1,100-1,300, private sector 1,900-2,300
-
5.
Analysis and Evaluation – 3,300-3,900
-
6.
Clinical Informatics – public sector 600-710, private sector 380-450
In the Gartner Research assessment of IT staff in integrated delivery systems, the major roles for IT staff were listed as programmer/analyst (51%), support (28%), and telecommunications (16%). A diversity of HIM roles in the US has also been noted, finding that the primary work setting for these individuals was hospital inpatient (53.4%), hospital outpatient (7.8%), physician office/clinic (7.2%), consulting firm (4.2%), and a variety of others settings [22]. For those involved in EHR implementation, two-thirds were on the planning team and half were on implementation team at their institutions.
The ONC recently released its assessment of workforce roles and competencies for EHR adoption, identifying roles in mobile support positions (i.e., moving from practice to practice, providing initial implementation), permanent staff of healthcare and public health organizations (i.e., providing ongoing support), and healthcare and public health informaticians. ONC also determined that the following roles would be predominantly trained in community colleges (denoted by *) or universities (denoted by †).
Mobile adoption support roles will support implementation at specific locations, for a period of time, and when their work is done, move on to new locations. These individuals might be employed by regional extension centers, vendors, or state/city public health agencies. The specific workforce roles include:
-
•
Implementation support specialist*
-
•
Practice workflow and information management redesign specialist*
-
•
Clinician consultant*
-
•
Implementation manager*
The permanent staff of healthcare delivery and public health sites will be needed for ongoing support of HIT at office practices, hospitals, health centers, long-term care facilities, health information exchange organizations, and state/city public health agencies. The roles include:
-
•
Technical/software support staff*
-
•
Trainer*
-
•
Clinician/public health leader†
-
•
Health information management and exchange specialist†
-
•
Health information privacy and security specialist†
Finally, the category of healthcare and public health informaticians includes individuals based in universities, research centers, government agencies, and research and development divisions of software companies. The roles include:
-
•
Research and development scientist†
-
•
Programmers and software engineer†
-
•
Health IT sub-specialist†
Growth and Gaps
Some but not all studies address anticipated job growth and/or the related issue of gaps between supply and demand for current or future HIT professionals. The English study does not estimate growth but voices concerns about pending shortages, especially if issues of professional development and competitive pay are not addressed [1]. The Australian study also does not assess growth but asserts a shortage that can be addressed by better organization of HIT implementation that can lead to the workforce being more efficiently deployed (and hence a need for fewer workers) [2]. The Canadian study, on the other hand, provides detailed estimates of anticipated growth [3]. The growth scenarios beyond the current 32,450 workers are based on the varying assumptions:
-
•
Low growth – across the board expenditure cuts by the Canadian health system
-
•
Medium growth – deferring of some capital investments
-
•
High growth – HIT investment unaffected by changes in healthcare spending
The cumulative employment growth for all categories combined to 2014 would then be:
-
•
Low growth – 7.6% growth to 35,020
-
•
Medium growth – 14.3% growth to 37,200
-
•
High growth – 26.1% growth to 41,030
In the US, the Bureau of Labor Statistics estimates growth rates for HIM from the current 172,500 employed in 2008 to 207,600 employed by 2018 [28]. The analysis of the HIMSS Analytics Database described earlier [26] was also used to identify growth by looking at the staffing rates per bed at different levels of HIT adoption using another component of the database, the EMR Adoption Model™ (EMRAM), which scores hospitals on eight stages to creating a “paperless record environment” [40] (see ►Table 1). “Advanced” HIT is generally assumed to be Stage 4, which includes computerized physician order entry (CPOE) and other forms of clinical decision support that have been shown to be associated with improvements in the quality and safety of healthcare [15, 16]. The attributes of Stages 3 and 4 correspond roughly to those required for “meaningful use” of HIT required for EHR adoption incentives in the HITECH legislation [41].
Table 1.
Description of stages for the EMR Adoption Model [40])
| Stage 7 | Medical record fully electronic; CDO able to contribute to EHR as byproduct of EMR |
| Stage 6 | Physician documentation (structured templates), full CDSS (variance & compliance), full R-PACS |
| Stage 5 | Closed loop medication administration |
| Stage 4 | CPOE, CDSS (clinical protocols) |
| Stage 3 | Clinical documentation (flow sheets), CDSS (error checking), PACS available outside radiology |
| Stage 2 | CDR, CMV, CDSS inference engine, may have document imaging |
| Stage 1 | Ancillaries – lab, radiology, pharmacy – all installed |
Average IT staffing ratios varied based on EMRAM stage [26]. ►Figure 1 shows a graph of the average staffing ratio for each of the stages (there were no hospitals at adoption Stage 7 at the time of the study). Average staffing ratios generally increased with adoption score, but hospitals at Stage 4 had a higher average staffing ratio than hospitals at Stages 5 or 6. If all hospitals were operating at the same staffing ratios as Stage 6 hospitals (0.196 IT FTE per bed), a total of 149,174 IT FTE would be needed to provide coverage, an increase of 40,784 FTE.
Fig. 1.
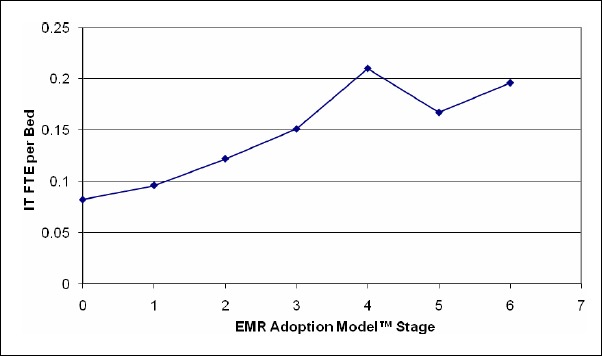
IT FTE per Bed vs. EMR Adoption [26].)
Leadership Qualifications
There is an even smaller amount of research assessing the qualifications of informatics leaders. A survey among members of the Association of Medical Directors of Information Systems (AMDIS, www.amdis.org) in the US found that of the 82 members who replied, few had formal training in informatics and nearly all of them valued of managerial and clinical over technical skills [42]. A more recent analysis looked in depth at five Chief Medical Information Officers (CMIOs) [23], finding that the skills they reported to be most important in carrying out their jobs were leadership, communication, and consensus-building. These CMIOs all stated a desire to be part of senior physician executive team and did not want to be seen as just “techie” doctors.
An additional source of information about CMIOs is the annual survey carried out by Gartner and AMDIS. The most recent of these surveys included 97 CMIOs [27]. For the majority responding, the “I” in their title was more likely to stand for “informatics” rather than “information.” The make-up of these individuals clearly reflected the types of organizations likely to hire CMIOs, namely large integrated delivery systems and hospitals. These institutions also had usage of HIT well beyond the national average, e.g., 30% with 75-100% penetration of CPOE. The CMIO position is virtually always an MD, with the specialties of internal medicine and family medicine most highly represented. Most CMIOs spent nearly all of their work time in informatics work, with half spending 80% or more time. CMIOs most commonly reported to CIOs, and less than half managed any staff, although most would prefer to report to a Chief Medical Officer, Chief Executive Officer, or Chief Operating Officer. Growing numbers of CMIOs were heading departments or units in healthcare organizations.
Another analysis of CMIOs found comparable results [43]. The CMIO position is well-compensated, with growing responsibilities and priorities for overseeing clinical applications in the healthcare enterprise. The position is almost always held a physician, over two-thirds of whom still participate in patient care.
Education and Competencies
A related problem to the lack of information characterizing the HIT workforce is the unclear view of the ideal levels of education and most important competencies to teach such individuals. In recognition of the need to promote awareness of the workforce challenges and increase visibility needed, AMIA and the American Health Information Management Association (AHIMA) held a summit in late 2005 [44]. The resulting report concluded that the benefits of HIT would not accrue to the US on a wide scale without a well-trained workforce to develop, implement, and evaluate systems. The report advocated:
-
•
Adopting the Institute of Medicine (IOM) “Quality Chasm” [45] vision.
-
•
Creating incentives to adopt “systems” that promote quality through use of HIT.
-
•
Establishing industry-wide advocacy for workforce training and development.
-
•
Building awareness of the need for workforce development.
-
•
Utilizing innovative learning environments to train the workforce.
-
•
Developing formal educational programs and promoting their value.
-
•
Disseminating tools and best practices for these new professionals to succeed.
There is no dearth of published competencies. ►Table 2 provides a list of competencies in informatics, both for informatics professionals as well as healthcare professionals, including their year published and targeted professional group. The competences of individual informatics educational programs are less well developed, but were recently analyzed and determined to be quite diverse [46]. Of course, these may change as the workforce and the discipline are better characterized. The IOM, which is a high-profile advocate for improving healthcare in the US, also sees an important role for informatics, designating it as one of three core competencies required for patient-centered care, along with employing evidence-based practice and applying quality improvement [47].
Table 2.
Inventory of competencies in biomedical and health informatics.
| Organization or Journal [Reference] | Year | Discipline | Title |
|---|---|---|---|
| Association for Computing Machinery [49] | 1978 | Computer science | Health Computing: Curriculum for an Emerging Profession |
| [50] | 1992 | Informatics | Recommendations of the German Association for Medical Informatics, Biometry and Epidemiology |
| Association of American Medical Colleges [51] | 1999 | Medical students | Medical School Objectives Project: Medical Informatics |
| International Medical Informatics Association [52] | 2000 | Informatics | Recommendations of the International Medical Informatics Association (IMIA) on education in health and medical informatics (updated in 2010) |
| UK National Health Service [53] | 2001 | Informatics | Health Informatics Competency Profiles for the NHS |
| American Nurses Association [54] | 2001 | Nursing | A Delphi Study to Determine Informatics Competencies for Nurses at Four Levels of Practice |
| University of Waterloo, Canada [29] | 2001 | Informatics | Pointing the Way: Competencies and Curricula in Health Informatics |
| Northwest Center for Public Health Practice [55] | 2002 | Public health professionals | Informatics Competencies for Public Health Professionals |
| American Association of Critical-Care Nurses [56] | 2003 | Nurse Practitioners | Informatics Competencies for Nurse Practitioners |
| Advances in Dental Research [57] | 2003 | Dental Researchers | Biomedical informatics training for dental researchers |
| American College of Medical Informatics [58] | 2004 | Bioinformatics | Training the Next Generation of Informaticians: The Impact of “BISTI” and Bioinformatics |
| Commission on Accreditation for Health Informatics and Information Management Education [59] | 2005 | Health Information Management | HIM Baccalaureate Degree Program Standards |
| Commission on Accreditation for Health Informatics and Information Management Education [60] | 2005 | Health Information Management | HIM Associate Degree Program Standards |
| International Journal of Medical Informatics [61] | 2005 | Nursing | Nursing informatics knowledge and competencies: a national survey of nursing education programs in the United States |
| Australia [62] | 2006 | Informatics | Australian Health Informatics Educational Framework |
| Journal of Internet Research [63] | 2006 | “Information age” students | Health information literacy and competencies of information age students |
| UK Council of Health Informatics Professionals [64] | 2007 | Informatics | Health Informatics National Occupational Standards |
| Medical Library Association [65] | 2007 | Health Science Librarians | Health Information Science Knowledge and Skills |
| Methods of Information in Medicine [66] | 2007 | Informatics | Benchmarking Statement |
| Health Informatics Journal [46] | 2007 | Informatics | Competencies for graduate curricula in health, medical and biomedical informatics: a framework |
| COACH: Canada’s Health Informatics Association [67] | 2007 | Informatics | Health Informatics Professional Core Competencies |
| American Nurses Association [34] | 2008 | Nursing | Scope and Standards of Nursing Informatics Practice |
| Nursing Clinics of North America [68] | 2008 | Nursing | Technology and informatics competencies |
| AMIA-OHSU 10x10 Course [69] | 2009 | Informatics | AMIA-OHSU 10x10 Program - Detailed Curriculum, Learning Objectives |
| AMIA Core Content for Clinical Informatics [35] | 2009 | Informatics | Core content for certification of physicians (with others to follow later) |
| TIGER Nursing Informatics [70] | 2009 | Nursing Informatics | TIGER Informatics Competencies Collaborative (TICC) Final Report |
| Office of the National Coordinator for Health IT [71] | 2009 | Electronic health record adoption | HIT Workforce Competencies by Role |
| Centers for Disease Control and Prevention, [72] | 2009 | Informatics | Public Health Informatics Competencies |
| International Medical Informatics Association [73] | 2010 | Informatics | Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics |
The optimal education of the HIT workforce is another gap in our knowledge. Not only do we lack good characterization of the workforce as described above, but we cannot even begin to understand its ideal educational criteria. Despite that, informatics educational programs are growing in size and stature. There are comprehensive Web sites that list and link to such programs internationally (http://www.hiww.org/) and in the US (https://www.amia.org/informatics-academic-training-programs/). These sites demonstrates there are many models for such education. For example, training in the US, UK, and Canada tends to focus at the graduate level (with some notable exceptions), whereas there are many baccalaureate programs in Germany. Likewise, there is a growing use of distance learning in many programs.
As noted above, the HITECH Act called out the need for a competent workforce to reach its goals for meaningful use of EHRs. In particular, Section 3016 of the legislation set forth the ONC HIT Workforce Development Program, which has been allocated $118 million in four programs:
-
1.
Consortia to Educate Health Information Technology Professionals Program ($70M) – Establishment of short-term certificate programs in community colleges to train 10,000 professionals per year in the six community college workforce roles.
-
2.
Curriculum Development Centers Program ($10M) – Development of curricular materials for the community college consortia and their distribution via a National Training and Dissemination Center.
-
3.
Competency Examination for Community College Programs ($6M) – A competency exam for students completing the programs in the community college workforce roles.
-
4.
Program of Assistance for University-Based Training ($32M) – A training grant for university (mostly graduate-level) programs at the certificate and master’s degree levels for the university workforce roles.
Conclusions
There is growing evidence of the importance of a competent workforce for successful HIT implementation. There are also substantial opportunities in the three major types of professional in IT, HIM, and clinical informatics. These jobs tend to pay well and offer opportunity for career advancement and satisfaction. Indeed, one US newsmagazine recently listed informatics among ten “ahead of the curve” careers [48].
However, both healthcare leaders and informatics leaders still need more information upon which to base implementation of systems, optimal deployment of the workforce, and the best educational options for the workforce. There is a need for more research to better characterize the workforce of those who develop, implement, and evaluate HIT systems. This will then better inform the development of optimal competencies and curricula for their most effective education and training. Workforce research must go beyond the narrow focus of single groups (e.g., IT staff, HIM professionals, or clinicians) or applications (e.g., EHRs or health information exchanges). Instead, it must focus on the larger picture of all involved in supporting the use of information to improve human health. More effort should also be devoted to establishing occupational coding classifications for informatics jobs and promoting the profession to attract those with passion and competence for it.
Clinical Relevance
There is increasing recognition that a competent and well-trained workforce is required for successful implementation of health information technology. Yet there is little research concerning that workforce, especially for those who work in biomedical and health informatics. The research that has been done shows that substantial numbers of individuals are needed with diverse competencies. Particular attention must be paid to career pathways and progression.
References
- 1.Eardley T. NHS Informatics Workforce Survey. 2006, ASSIST: London, England: http://www.bcs.org/upload/pdf/finalreport_20061120102537.pdf [Google Scholar]
- 2.Legg M, Lovelock B. A Review of the Australian Health Informatics Workforce. 2009, Health Informatics Society of Australia: Melbourne, Australia: http://www.hisa.org.au/files/File/Australian_Health_Informatics_Workforce_Review_v1_1.pdf [Google Scholar]
- 3.O’Grady J. Health Informatics and Health Information Management: Human Resources Report. 2009, Prism Economics and Analysis: Toronto, Ontario: http://www.ictc-ctic.ca/uploadedFiles/Labour_Market_Intelligence/E-Health/HIHIM_report_E_web.pdf [Google Scholar]
- 4.Monegain B. Health IT effort to create thousands of new jobs, says Blumenthal, Healthcare IT News. October 6, 2009. http://www.healthcareitnews.com/news/health-it-effort-create-thousands-new-jobs-says-blumenthal [Google Scholar]
- 5.Hersh W, Margolis A, Quirós F, Otero P. Building a health informatics workforce in developing countries. Health Affairs. 2010; 29: 274–277 [DOI] [PubMed] [Google Scholar]
- 6.Hersh W. Health and Biomedical Informatics: Opportunities and Challenges for a Twenty-First Century Profession and its Education, in: IMIA Yearbook of Medical Informatics 2008, Geissbuhler A, Ku-likowski C, 2008; 138-145 Schattauer: Stuttgart, Germany: [PubMed] [Google Scholar]
- 7.Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005; 116: 1506-1512 [DOI] [PubMed] [Google Scholar]
- 8.Phibbs CS, Milstein A, Delbanco SD, Bates D. No proven link between CPOE and mortality. Pediatrics 2005. http://pediatrics.aappublications.org/cgi/eletters/116/6/1506 [Google Scholar]
- 9.Sittig DF, Ash JS, Zhang J, Osheroff JA, Shabot MM. Lessons from “unexpected increased mortality after implementation of a commercially sold computerized physician order entry system”. Pediatrics 2006; 118: 797-801 [DOI] [PubMed] [Google Scholar]
- 10.DelBeccaro MA, Jeffries HE, Eisenberg MA, Harry ED, Computerized provider order entry implementation: no association with increased mortality rates in an intensive care unit. Pediatrics 2006; 118: 290-295 [DOI] [PubMed] [Google Scholar]
- 11.Longhurst C, Sharek P, Hahn J, Sullivan J, Classen D, Perceived increase in mortality after process and policy changes implemented with computerized physician order entry. Pediatrics 2006; 117: 1450-1451 [DOI] [PubMed] [Google Scholar]
- 12.Jacobs BR, Brilli RJ, Hart KW. Perceived increase in mortality after process and policy changes implemented with computerized physician order entry. Pediatrics 2006; 117: 1451-1452 [DOI] [PubMed] [Google Scholar]
- 13.Rosenbloom ST, Harrell FE, Lehmann CU, Schneider JH, Spooner SA, Johnson KB, Perceived increase in mortality after process and policy changes implemented with computerized physician order entry. Pediatrics 2006; 117: 1452-1455 [DOI] [PubMed] [Google Scholar]
- 14.Ash JS, Stavri PZ, Dykstra R, Fournier L. Implementing computerized physician order entry: the importance of special people. International Journal of Medical Informatics 2003; 69: 235-250 [DOI] [PubMed] [Google Scholar]
- 15.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine 2006; 144: 742-752 [DOI] [PubMed] [Google Scholar]
- 16.Goldzweig CL, Towfigh A, Maglione M, Shekelle PG. Costs and benefits of health information technology: new trends from the literature. Health Affairs 2009; 28: w282-w293 [DOI] [PubMed] [Google Scholar]
- 17.Monegain B. Healthcare IT: is it a breed apart? Healthcare IT News. September,2004; 4 http://www.healthcareitnews.com/story.cms?id=1522 [Google Scholar]
- 18.Sable JH, Hales JW, Bopp KD. Medical informatics in healthcare organizations: a survey of healthcare information managers. Proceedings of the AMIA 2000 Annual Symposium 2000; 745-748 Los Angeles, CA: Hanley & Belfus; [PubMed] [Google Scholar]
- 19.Detmer DE, Lumpkin JR, Williamson JJ. Defining the medical subspecialty of clinical informatics. Journal of the American Medical Informatics Association 2009; 16: 167-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anonymous Standard Occupational Classification (SOC) User Guide. 2004, US Department of Labor - Bureau of Labor Statistics: Washington, DC.http://www.bls.gov/soc/socguide.htm [Google Scholar]
- 21.DalPoz MR, Kinfu Y, Dräger S, Kunjumen T. Counting health workers: definitions, data, methods and global results, in Background Paper for the World Health Report 2006. 2006, World Health Organization: Geneva, Switzerland: http://www.who.int/hrh/documents/counting_health_workers.pdf [Google Scholar]
- 22.Wing P, Langelier M, Continelli T, Armstrong D. Data for Decisions: the HIM Workforce and Workplace - 2002 Member Survey. 2003, American Health Information Management Association: Chicago, IL: http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_018947.pdf [Google Scholar]
- 23.Leviss J, Kremsdorf R, Mohaideen MF, The CMIO - a new leader for health systems. journal of the American Medical Informatics Association 2006; 13: 573-578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anonymous Nationwide Health Information Network (NHIN) Workforce Study. 2007, Altarum Institute: Ann Arbor, MI: http://aspe.hhs.gov/sp/reports/2007/NHIN/NHINReport.pdf [Google Scholar]
- 25.Shaffer V. U.S. Integrated Delivery System IT Budget and Staffing Survey, 2008. 2008, Gartner: Stamford, CT [Google Scholar]
- 26.Hersh WR, Wright A. What workforce is needed to implement the health information technology agenda? An analysis from the HIMSS Analytics™ Database. AMIA Annual Symposium Proceedings. 2008; 303-307 Washington, DC: American Medical Informatics Association; [PMC free article] [PubMed] [Google Scholar]
- 27.Shaffer V, Lovelock JD. Results of the Gartner-AMDIS Survey of Chief Medical Informatics Officers. 2009, Gartner: Stamford, CT [Google Scholar]
- 28.Anonymous Medical Records and Health Information Technicians, in Occupational Outlook Handbook, 2010-11 Edition. 2009, Bureau of Labor Statistics: Washington, DC: http://www.bls.gov/oco/ocoS103.htm [Google Scholar]
- 29.Covvey HD, Zitner D, Bernstein R. Pointing the Way: Competencies and Curricula in Health Informatics. 2001, University of Waterloo: Waterloo, Ontario, Canada: http://www.cs.uwaterloo.ca/health_info/health_docs/CurriculaMASTERDocumentVersion1Final.zip [Google Scholar]
- 30.Hersh W. A stimulus to define informatics and health information technology. BMC Medical Informatics & Decision Making 2009; 9: 24 http://www.biomedcentral.com/1472-6947/9/24/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hersh WR. Who are the informaticians? What we know and should know. Journal of the American Medical Informatics Association 2006; 13: 166-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joyub R. The Professionalisation of Health Informatics in the United Kingdom, UK Health Informatics Today. Spring, 2004; 42: 1-2, 4 http://www.bmis.org/ebmit/2004_42_spring.pdf [Google Scholar]
- 33.Anonymous Making information count: a human resources strategy for health professionals. 2002, UK Department of Health: London, England: http://www.dh.gov.uk/assetRoot/04/07/30/84/04073084.pdf [Google Scholar]
- 34.Anonymous Scope and Standards of Nursing Informatics Practice. 2008, Washington, DC: American Nurses Association; [DOI] [PubMed] [Google Scholar]
- 35.Gardner RM, Overhage JM, Steen E, Munger BS, Holmes JH, Williamson JJ, et al. Core content for the subspecialty of clinical informatics. Journal of the American Medical Informatics Association 2009; 16: 153-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safran C, Shabot MM, Munger BS, Holmes JH, Steen EB, Lumpkin JR, et al. ACGME program requirements for fellowship education in the subspecialty of clinical informatics. Journal of the American Medical Informatics Association 2009; 16: 158-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Detmer DE, Munger BS, Lehmann CU. Medical informatics board certification: history, current status, and predicted impact on the medical informatics workforce. Applied Clinical Informatics 2010; 1: 11-18 doi: 10.4338/ACI-2009-11-R-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Safran C, Detmer DE. Computerized physician order entry systems and medication errors. Journal of the American Medical Association 2005; 294: 179. [DOI] [PubMed] [Google Scholar]
- 39.Friedman CP. Building the Health Informatics Workforce. 2008, University of California Davis Invited Presentation: Sacramento, CA [Google Scholar]
- 40.Anonymous The EHR Adoption Model. 2007, Healthcare Information Management and Systems Society: Chicago, IL: http://www.himssanalytics.org/docs/EMRAM_att_corrected.pdf [Google Scholar]
- 41.Davis MW. The State of U.S. Hospitals Relative to Achieving Meaningful Use Measurements. 2009, HIMSS Analytics: Chicago, IL: http://www.himssanalytics.org/docs/HA_ARRA_100509.pdf [Google Scholar]
- 42.Conn J. In IT, it pays to think big – survey puts metrics to medical informatics, Modern Physician. 7: 18-19 [Google Scholar]
- 43.Stevens M. CMIO 2010 Compensation Survey: The Results Are In!, CMIO Magazine. February, 2010. 4-7 http://www.cmio.net/index.php?option=com_articles&view=article&id=20446 [Google Scholar]
- 44.Anonymous Building the Work Force for Health Information Transformation. 2006, American Health Information Management Association and American Medical Informatics Association: Chicago, IL and Bethesda, MD: http://www.ahima.org/emerging_issues/Workforce_web.pdf [Google Scholar]
- 45.Anonymous Crossing the Quality Chasm: A New Health System for the 21st Century. 2001, Washington, DC: National Academies Press; [PubMed] [Google Scholar]
- 46.Huang QR. Competencies for graduate curricula in health, medical and biomedical informatics: a framework. Health Informatics Journal 2007; 13: 89-103 [DOI] [PubMed] [Google Scholar]
- 47.Greiner AC, Knebel E, Health Professions Education: A Bridge to Quality. 2003, National Academies Press: Washington, DC: [PubMed] [Google Scholar]
- 48.Nemko M. Ahead-of-the-Curve Careers, US News & World Report. December 19, 2007. http://www.usnews.com/articles/business/best-careers/2007/12/19/ahead-of-the-curve-careers.html [Google Scholar]
- 49.Duncan KA, Austing RH, Katz S, Pengov RE, Pogue RE, Wasserman AI. Health Computing: Curriculum for an emerging profession – report of the ACM curriculum committee on health computing education. Proceedings of the 1978 ACM Annual Conference/Annual Meeting. 1978; 277-285 Washington, DC: ACM Press; http://portal.acm.org/ft_gateway.cfm?id=804112&type=pdf&coll=GUIDE&dl=GUIDE&CFID=47975758&CFTOKEN=19987037 [Google Scholar]
- 50.Haux R, Dudeck J, Gaus W, Leven FJ, Kunath H, Michaelis J, et al. Recommendations of the German Association for Medical Informatics, Biometry and Epidemiology for education and training in medical informatics. Methods of Information in Medicine 1992; 31: 60-70 [PubMed] [Google Scholar]
- 51.Anonymous Medical School Objectives Project: Medical Informatics Objectives. 1999, Association of American Medical Colleges: Washington, DC: http://www.aamc.org/meded/msop/start.htm [Google Scholar]
- 52.Anonymous Recommendations of the International Medical Informatics Association (IMIA) on education in health and medical informatics. Methods of Information in Medicine 2000; 39: 267-277 http://www.imia.org/pubdocs/rec_english.pdf [PubMed] [Google Scholar]
- 53.Anonymous Health Informatics Competency Profiles for the NHS. 2001, National Health Service Information Authority: London, England: http://www.nhsia.nhs.uk/nhid/pages/resource_informatics/hi_competencyprofiles.pdf [Google Scholar]
- 54.Staggers N, Gassert CA, Curran C. A Delphi study to determine informatics competencies at four levels of practice. Nursing Research 2002; 51: 383-390 [DOI] [PubMed] [Google Scholar]
- 55.O’Carroll PW. Informatics Competencies for Public Health Professionals. 2002, Northwest Center for Public Health Practice: Seattle, WA: http://www.cphi.washington.edu/resources/competencies-professionals.pdf [Google Scholar]
- 56.Curran CR. Informatics competencies for nurse practitioners. AACN Clinical Issues 2003; 14: 320-330 [DOI] [PubMed] [Google Scholar]
- 57.Johnson LA. Biomedical informatics training for dental researchers. Advances in Dental Research 2003; 17: 29-33 [DOI] [PubMed] [Google Scholar]
- 58.Friedman CP, Altman RB, Kohane IS, McCormick KA, Miller PL, Ozbolt JG, et al. Training the next generation of informaticians: the impact of ‘BISTI’ and bioinformatics; a report from the American College of Medical Informatics. Journal of the American Medical Informatics Association 2004; 11: 167-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anonymous Standards for Health Information Management Education – Baccalaureate Degree Program Standards. 2005, Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM): Chicago, IL: http://library.ahima.org/xpedio/groups/public/documents/accreditation/bok1_026307.pdf [Google Scholar]
- 60.Anonymous Standards for Health Information Management Education -– Associate Degree Program Standards. 2005, Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM): Chicago, IL: http://library.ahima.org/xpedio/groups/public/documents/accreditation/bok1_026306.pdf [Google Scholar]
- 61.McNeil BJ, Elfrink VL, Pierce ST, Beyea SC, Bickford CJ, Averill C. Nursing informatics knowledge and competencies: a national survey of nursing education programs in the United States. International Journal of Medical Informatics 2005; 74: 1021-1030 [DOI] [PubMed] [Google Scholar]
- 62.Garde S, Hovenga E. Australian Health Informatics Educational Framework. 2006, Australian College of Health Informatics: Brunswick East, Australia: http://www.achi.org.au/documents/publications/Health_Informatics_Educational_Framework_20060326.pdf [Google Scholar]
- 63.Ivanitskaya L, O’Boyle I, Casey AM. Health information literacy and competencies of information age students: results from the interactive online Research Readiness Self-Assessment (RRSA). Journal of Medical Internet Research 2006; 8(2): e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. http://www.jmir.org/2006/2/e6/ [Google Scholar]
- 65.Anonymous Health Informatics National Occupational Standards. 2007, UK Council for Health Informatics Professions: London, England: http://www.hinos.org.uk/ [Google Scholar]
- 66.Anonymous Health Information Science Knowledge and Skills. 2007, Medical Library Association: Chicago, IL: http://www.mlanet.org/education/platform/skills.html [Google Scholar]
- 67.Pigott K, deLusignan S, Rapley A, Robinson J, Pritchard-Copley A. An informatics benchmarking statement. Methods of Information in Medicine 2007; 46: 394-398 [DOI] [PubMed] [Google Scholar]
- 68.Anonymous Health Informatics Professional Core Competencies. 2007, COACH: Canada’s Health Informatics Association: Toronto, Ontario: http://www.coachorg.com/opendoc.asp?docID=1179 [Google Scholar]
- 69.Gassert CA. Technology and informatics competencies. Nursing Clinics of North America 2008; 43: 507-521 [DOI] [PubMed] [Google Scholar]
- 70.Hersh W. AMIA-OHSU 10x10 Program – Logistics, Accessing Demo, Detailed Curriculum, Learning Objectives, and Additional Information. 2009, Oregon Health & Science University: Portland, OR: http://www.billhersh.info/10x10.html [Google Scholar]
- 71.Gugerty B, Delaney C, TIGER Informatics Competencies Collaborative (TICC) Final Report. 2009, Technology Informatics Guiding Educational Reform (TIGER) Initiative. http://tigercompetencies.pbworks.com/f/TICC_Final.pdf [Google Scholar]
- 72.Anonymous, HIT Workforce Competencies by Role 2009, Office of the National Coordinator for Health IT: Washington, DC: http://healthit.hhs.gov/portal/server.pt?open=18&objID=888534&parentname=CommunityPage&parentid=15&mode=2&in_hi_userid=11113&cached=true [Google Scholar]
- 73.Anonymous Public Health Informatics Competencies. 2009, Centers for Disease Control and Prevention: Atlanta, GA: http://www.cdc.gov/InformaticsCompetencies/downloads/PHI_Competencies.pdf [Google Scholar]
- 74.Mantas J, Ammenwerth E, Demiris G, Hasman A, Haux R, Hersh W, et al. Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics – 1st revision. Methods of Information in Medicine 2010; 49: 105-120 [DOI] [PubMed] [Google Scholar]


