Abstract
Background
The Chicago Classification of Esophageal Motility Disorders (CC) is based on 10 water swallows performed in the supine position. The aim of the study was to assess whether upright and provocative swallows provided important information beyond that obtained from the standard supine manometric protocol.
Methods
Two independent investigators reviewed high resolution manometry (HRM) studies of 148 patients with both supine and upright liquid swallows and additional studies from patients with provocative swallows (increased volume, viscosity, and a marshmallow) for a resultant change in CC diagnoses. Significant diagnostic changes were defined as a change from normal or borderline motor function to abnormal motor function, EGJ outflow obstruction or achalasia. Discordant diagnoses were reviewed and the Kappa test was used to evaluate the agreement between diagnoses in the different protocols.
Key Results
The overall agreement in diagnosis between the 5 supine swallows and the 5 upright swallows was good (k=0.583). Changing to the upright position elicited a significant diagnostic change in 10.1% (15/148) of cases. The provocative swallows suggested an alternative diagnosis from the supine position in 14 of 75 studies (18.7%); 11 of these changed to EGJ obstruction during viscous or solid bolus challenges.
Conclusion
Changing position in HRM elicited a significant change in diagnosis in about 10% of studies while provocative bolus challenges with viscous liquid and marshmallows increased the detection of EGJ outflow obstruction. Performing manometric evaluations in both positions with provocative swallows may increase the yield of standard HRM technique.
Keywords: high resolution manometry, body position, Chicago classification
Introduction
The current standard protocol for high-resolution manometry (HRM) utilizing the Chicago Classification (CC) scheme for classifying esophageal motor disorders is based on 10 water swallows in the supine position(1). However, swallows in the upright position may be informative in assessing esophageal motor function, as this is deemed to be more “physiological” as eating is usually performed sitting upright. Previous studies have shown that bolus transit and esophagogastric junction pressure may be influenced by body position (2, 3) and that extrinsic compression of the esophagus by the heart and aorta may be reduced in the upright position (4). Additionally, Sweis et al reported normative ranges for upright swallows that were significantly different compared to those reported for the standard 5ml supine swallows (5). Thus, the optimal manometric protocol may be enhanced by changing position and modifying normative ranges associated with these positional changes.
In addition to body position, esophageal motility may also be influenced by swallow volume and bolus composition (6–8). Most patients relate their ongoing esophageal symptoms to specific foods, such as bread and meat. Thus, it may be useful to utilize various bolus challenges during HRM studies. Blonski et al reported that the viscous bolus challenges could increase the detection of impaired esophageal function (7). Similarly, Bernhard et al reported that using bread swallows in the upright position revealed abnormalities overlooked by liquid swallows alone (8). Thus, similar to the logic of studying patients in the upright position, provocative swallows with various bolus challenges might also represent a more “real life” clinical scenario for testing.
Given the previous data supporting that changing position and bolus consistencies may alter esophageal motor function, we hypothesized that upright and solid bolus swallows could be added to the standard supine protocol to increase the overall diagnostic yield of stationary HRM. Our aim was to compare the CC diagnosis obtained in the supine position using 10 supine 5 ml water swallows with that obtained from expanded protocols. This information could potentially help develop a standard protocol for HRM and improve the diagnostic impact of this test.
Methods
Subjects and study protocol
Esophageal pressure topography (EPT) studies of 148 patients (51 males, mean age 54, range 22–86) from October 2010 to November 2011 referred to the Esophageal Center at Northwestern were included in the analysis. This group was randomly selected from a consecutive series of 845 studies during that time frame to target a sample size of 150 patients; two patients were removed due to technical issues with the study. The study was carried out using our standardized protocol with the patients in the supine position (flat on the back at 0–10 degrees) for ten 5ml liquid swallows and then in the upright position (sitting in a chair at 75–90 degrees) for an additional five 5ml liquid swallows (Figure 1). In July 2011, our group instituted a provocative swallow component to our standardized clinical protocol. The EPT studies from an additional 75 patients (22 males, mean age 54, range 17–86) from July 2011 to November 2011with 10 liquid swallows in the supine position, 5 liquid swallows in the upright position, and 8 additional provocative swallows (PS) were also randomly selected to assess whether the provocative swallows significantly changed the overall diagnosis. For the provocative swallows, the patients were maintained in the upright position and asked to perform the following swallows: high-volume swallows (HVS) [two 10 ml & two 20 ml water swallows], viscous swallows [two 5 ml apple compote swallows] and solid swallows [two 1 cm3 marshmallow swallows] (Figure 1). The study protocol was approved by the Northwestern University Institutional Review Board and informed consent was obtained from each subject.
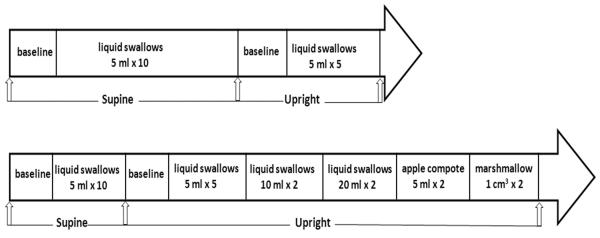
Figure 1.
Manometric protocol for the current study. The top panel illustrates the protocol with 10 liquid swallows in the supine position and 5 liquid swallows in the upright position. The bottom panel illustrates the protocol with 10 liquid swallows in the supine position, 5 liquid swallows and 8 provocative swallows in the upright position.
Data analysis
The EPT studies were blindly analyzed by the investigators using the following sequence for each patient: the first 5 supine swallows, all 10 supine swallows, the 5 upright swallows, and the provocative swallows. The second investigator repeated the analysis in the reverse sequence (YLX and FN). Hence, a final diagnosis was made for each patient based on 10 supine swallows, the first 5 supine swallows, and the 5 upright swallows by each of the two investigators. A blinded senior investigator (JEP) resolved discrepancies between the study investigators. The integrated relaxation pressure (IRP), peristaltic integrity, distal latency, contractile front velocity and distal contractile integral (DCI) for each swallow were measured and utilized for the final comparison (1)
The diagnostic criteria were defined according to the 2012 Chicago Classification (1) using ManoView™ software (Given Imaging, Duluth GA, USA). According to the CC, the diagnoses were sub-classified into 5 groups of disorders to test agreement (Table 1): A) achalasia [IRP>15 mmHg, no normal peristalsis], B) esophagogastric junction (EGJ) outflow obstruction [IRP>15 mmHg, evidence of normal peristalsis], C) abnormal motility [absent peristalsis, hypercontractile, or distal esophageal spasm], D) borderline motility [normal IRP, motor patterns beyond normative confidence intervals but not fulfilling criteria for abnormal motility], and E) normal.
Table 1.
Indications for HRM of the 148 patients with both supine and upright swallows
| High Resolution Manometry Diagnosis Based on 10 supine swallows | Total | ||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | |||
| Indications | Dysphagia | 8 | 9 | 14 | 22 | 8 | 61 |
| Reflux (heartburn, regurgitation) | 0 | 2 | 3 | 27 | 17 | 49 | |
| Chest pain | 0 | 0 | 1 | 8 | 6 | 15 | |
| Other* | 0 | 1 | 2 | 12 | 8 | 23 | |
| Total | 8 | 12 | 20 | 69 | 39 | 148 | |
A: Achalasia; B: EGJ outflow obstruction; C (Abnormal motility): Absent peristalsis, distal esophageal spasm, hypercontractile esophagus; D (Borderline): Weak peristalsis; frequent failed peristalsis; hypertensive peristalsis, rapid contraction; E: Normal
Other includes globus, cough, hoarseness, throat clearing.
The diagnosis obtained from the ten 5 ml swallows in the supine position served as the standard diagnosis. To evaluate the validity of comparing 5 swallows to obtain a diagnosis, the agreement of the diagnosis between the first 5 supine swallows and all 10 supine swallows were reviewed. The agreement between the standard diagnosis and the corresponding diagnosis from the 5 upright swallows of the same patient were compared to assess whether the body position change altered the diagnosis. Provocative swallows were assessed individually to determine whether an abnormal motor pattern or evidence of obstruction was elicited that would alter the diagnosis. A chart review was performed to determine whether additional studies or treatments were offered based on these findings.
Statistical analysis
Mean IRP and DCI were compared amongst the different protocols using Wilcoxon test. Kappa test was used to evaluate the agreement between the diagnoses in the different protocols. All P values were two-tailed with the level of significance defined at 0.05.
Results
Diagnostic agreement between the first 5 and all 10 supine swallows
The overall agreement of diagnosis between the standard 10 supine swallow protocol and the first 5 swallows was excellent at 0.814 (P <0.001). Both the mean IRP and DCI were similar between the 10 supine swallows and the first 5 supine swallows (mean IRP: 8.1 vs 8.3 respectively, p=0.746; mean DCI: 936 vs 942, respectively, p=0.212).
Nineteen (12.8 %) patients had a discrepancy in subclassification diagnosis. Sixteen of the 19 discrepancies were attributable to the increased weighting of single swallows with the smaller swallow sample size (20% change): 13 discrepancies were between borderline and normal motility, 2 discrepancies were a diagnosis shift from frequent failed peristalsis (in the 10 supine swallows) to absent peristalsis (in the first 5 of the series) and one was related to abnormal motility (hypercontractile) being classified as hypertensive when only the first 5 swallows were used. The remaining 3 discrepancies were due to a change in the mean IRP which was related to an increased weighting of a single swallow with the smaller number analyzed. No cases of achalasia, spasm, or absent peristalsis were missed by using the 5 swallow protocol. Altogether, a significant change in diagnosis was elicited in only 6 of 148 (4%) patients when only 5 swallows were used.
Diagnostic agreement between the supine swallows and upright swallows
The overall agreement in diagnosis between the first 5 supine swallows and the 5 upright swallows in the 148 patients is presented in Table 2. Both the mean IRP and DCI from the first 5 supine swallows were greater than that in the upright 5 swallows (mean IRP: 8.3 vs 5.6,; mean DCI: 942 vs 637 respectively, both p<0.001). The kappa value for the overall agreement between the supine and the upright diagnoses was good at 0.583 (p<0.001).
Table 2.
Agreement in diagnoses between protocols according to either first 5 supine swallows or upright 5 swallows
| 5 upright swallows | Total | ||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | |||
| 5 supine swallows | A | 7 | 1 | 0 | 0 | 0 | 8 |
| B | 0 | 10 | 0 | * 2 | * 1 | 13 | |
| C | 0 | 0 | 18 | α 3 | 0 | 21 | |
| D | 0 | † 4 | α 3 | 55 | 5 | 67 | |
| E | 0 | † 1 | α 1 | 21 | 16 | 39 | |
| Total | 7 | 16 | 22 | 81 | 22 | 148 | |
A: Achalasia; B: EGJ outflow obstruction; C (Abnormal motility): Absent peristalsis, distal esophageal spasm, hypercontractile esophagus; D (Borderline): Weak peristalsis; frequent failed peristalsis; hypertensive peristalsis, rapid contraction; E: Normal
Discrepancy due to an increase in the IRP in the upright position
Discrepancy due to the change in contractility related to the position change
Diagnosis change from EGJ outflow obstruction to weak peristalsis or normal when shift to upright
Forty-two (28.4%) of the 148 patients had a different diagnosis when the first 5 supine swallows were compared to the 5 upright swallows (Table 2). Twenty of the 42 had decreased contractility when upright and 13 had an unexpected increase in contractility leading to a reclassification. Five of the 42 reclassifications were due to issues related to an increased IRP in the upright position. Three subjects with EGJ outflow obstruction in the supine position were reclassified as weak peristalsis or normal in the upright position. Achalasia was diagnosed concordantly in 7 of 8 cases with the one discordant patient categorized as achalasia in the supine position and EGJ outflow obstruction in the upright position.
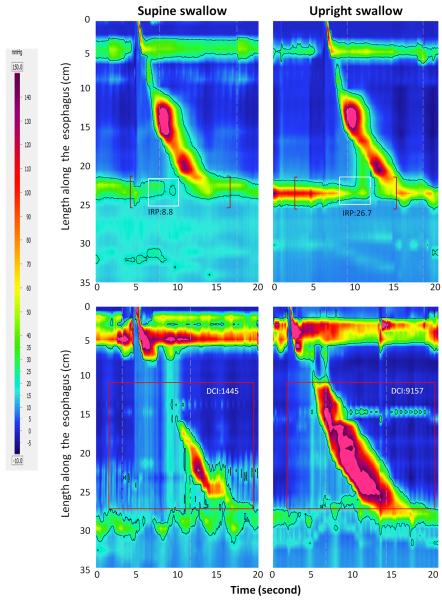
Overall, 9 subjects changed from borderline/normal motility in the supine position to either abnormal motility or EGJ outflow obstruction (Figure 2) in the upright position. Among the five reclassified to EGJ outflow obstruction, 2 had hiatal hernia on endoscopy, 1 had a dilated distal esophagus for unknown reason, 1 had a lower esophageal ring on endoscopy, and one had a normal endoscopy. Three patients were reclassified to hypercontractile esophagus when positioned into the upright position, the other patient was reclassified to absent peristalsis when shifted to the upright position. In contrast, 6 patients had a significant change to a less severe diagnosis going from the supine position to the upright position. Three EGJ outflow obstruction patients with borderline IRP in the supine position were reclassified as either normal or weak peristalsis when the position was shifted to upright as this removed a vascular artifact through the EGJ. Two patient's diagnoses changed from absent peristalsis to weak peristalsis and one patient had a hypercontractile diagnosis in the supine position and hypertensive in the upright position. Altogether, changing position elicited a significant diagnosis change in 15 of 148 (10.1%) of cases.
Figure 2.
Altered diagnoses associated with shifting the body position from supine (left) to upright (right). The top panels illustrate a change in the IRP in the upright position that resulted in the diagnosis of an EGJ outflow obstruction. The bottom panels illustrate an instance in which the shift in the body position evoked a hypercontractile pattern in a patient with a small LES- crural diaphragm separation in the supine position.
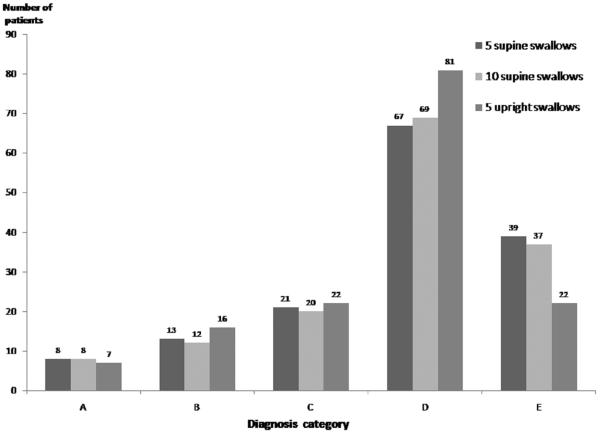
The overall agreement between the diagnoses from 10 supine swallows or the 5 upright swallows in the 148 patients is presented in Table 3. The kappa value for the overall agreement between the supine and the upright diagnoses was good at 0.70 (p<0.001). Thirty of the 148 patients (20.3%) had a different diagnosis when the 10 supine swallows were compared to the 5 upright swallows (Table 3). The discrepancies in the diagnoses were due to similar causes noted between the 5 supine and 5 upright swallows. Overall, changing position elicited a significant diagnosis change in 11 of 148 (7.4%) of cases. The overall comparison of the diagnosis categories obtained from 5 supine swallows, 10 supine swallows and 5 upright swallows is presented in Figure 3.
Table 3.
Agreement in diagnoses between protocols according to either 10 supine swallows or the 5 upright swallows
| 5 upright Swallows | Total | ||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | |||
| 10 supine swallows | A | 7 | 1 | 0 | 0 | 0 | 8 |
| B | 0 | 11 | 0 | * 1 | 0 | 12 | |
| C | 0 | 0 | 18 | # 2 | 0 | 20 | |
| D | 0 | α 2 | # 3 | 62 | 2 | 69 | |
| E | 0 | α 2 | # 1 | 16 | 20 | 39 | |
| Total | 7 | 16 | 22 | 81 | 22 | 148 | |
A: Achalasia; B: EGJ outflow obstruction; C (Abnormal motility): Absent peristalsis, distal esophageal spasm, hypercontractile esophagus; D (Borderline): Weak peristalsis; frequent failed peristalsis; hypertensive peristalsis, rapid contraction; E: Normal
Discrepancies due to an increase in the IRP in the upright position
Diagnosis change from EGJ outflow obstruction to weak peristalsis when shift to upright
Discrepancies due to the change in contractility related to the position change
Figure 3.
The overall comparison of diagnostic categories obtained from 5 supine swallows, 10 supine swallows and 5 upright swallows.
Diagnostic agreement between the standard protocol and provocative swallows
Both the mean IRP and DCI were greater with the supine 10 swallows than in the provocative swallows (mean IRP: 7.2 vs 5.4,; mean DCI: 1014 vs 789, respectively, both p<0.001). However, the IRP and DCI were similar between the upright and provocative swallows (mean IRP: 5.7 vs 5.4, p=0.053; mean DCI: 546 vs 789, p=0.381).
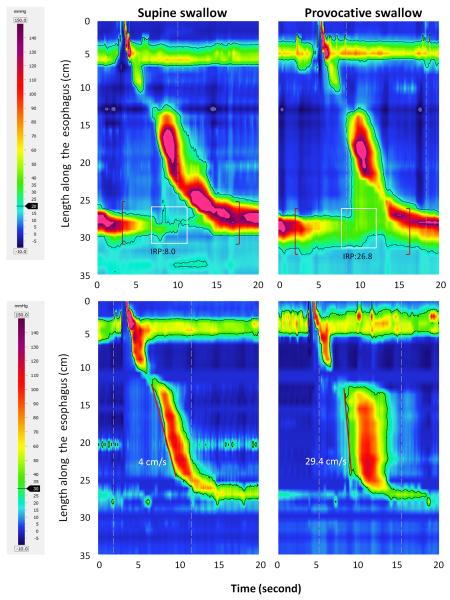
Each high volume swallow, viscous and solid swallow was evaluated for evidence of an alternative CC diagnosis or a subclinical obstruction. Such evidence was found in 14 of 75 (18.7%) patients and all of these were attributable to the viscous (n=11) or solid swallows (n=3). Eleven of these 14 patients (14.7%) exhibited EGJ outflow obstruction during one of the viscous or solid swallow when the standard protocol IRP was normal or borderline in the supine position (Figure 4). Among these 11 patients, an obstructive pathology was discovered in 3 subjects (extrinsic compression, esophageal ring and EGJ outflow obstruction secondary to old peptic injury treated with dilation). Of the remaining 8 patients, no overt mechanical obstruction was found: 2 patients were treated successfully as achalasia (1- myotomy, 1-BoTox) and 6 did not have any clear explanation for their dysphagia/regurgitation. Two additional patients exhibited rapid contraction with normal latency and 1 had a premature contraction after viscous or solid swallows, when these abnormalities were not found in the 10-swallow protocol. Among the other 61 patients, the provocative swallow patterns were consistent with the standard diagnosis.
Figure 4.
Development of significant abnormal HRM parameters with provocative swallows. Panels on the left illustrate the supine swallows and panels on the right illustrate the corresponding provocative swallows in the same patient. Panels on the top illustrate the occurrence of EGJ outflow obstruction with the viscous bolus swallow. Panels on the bottom illustrate the occurrence of a rapid contraction with the viscous bolus.
Time for the procedure with different protocols
The duration of the procedure with different protocols was calculated once the catheter positioning and the baseline period for accommodation were completed. For the protocol with the 10 swallows in the supine position, the total duration was 7.1± 2.3 minutes. If 5 upright swallows were added into the procedure, the study duration was 9.9±2.6 minutes. If 2 solid and 2 viscous swallows were added, the study duration increased to 14.0±3.6 minutes.
Discussion
We performed HRM in both the supine and upright positions with liquid and provocative bolus challenges to determine the optimal swallow protocol for clinical HRM. Our findings suggest that adding 5 upright swallows resulted in a significant change in diagnosis in 10% of cases and provocative bolus challenges (5 ml apple compote and 1 cm3 marshmallow) increased the detection of EGJ outflow obstruction. These findings suggest that an optimal protocol for performing HRM should include at least 10 liquid swallows in the supine position, 5 liquid swallows in the upright position and additional provocative swallows using viscous and solid boluses.
Esophageal contraction is influenced by body position as the vigor of contraction becomes weaker in the upright position with gravity assisting esophageal emptying (3, 5, 8, 9). Thus, it should not be surprising for some diagnoses to differ in the upright position using normative ranges derived for the supine position. Indeed, our findings confirmed that positional changes did alter some diagnoses and that the position change also helped remove a vascular artifact that would have led to an inaccurate diagnosis of EGJ outflow obstruction in three patients. However, we were surprised to find that 9 patients with borderline/normal motility in the supine position exhibited a significant abnormality in the upright position that would have been missed if only the supine swallows were analyzed (Figure 2); five patients developed an EGJ outflow obstruction in the upright position and 3 patients developed an abnormal motor pattern (from normal or borderline abnormality to hypercontractile). These alterations may be the result of postural related conformational change at the EGJ such as angulation or a small herniation that could increase outflow obstruction. An additional patient was found to have an esophageal ring and treated with dilation. At the very least, these results suggest that evaluation of the patient in both positions is complimentary and can reduce vascular artifacts found at the EGJ in some patients.
Our results also suggest that the inclusion of viscous and solid bolus challenges may be helpful in eliciting a subtle obstruction at the EGJ that would have been missed using only supine water swallows. Although the viscous and solid provocative swallows provoked an obstructive pattern at the EGJ in only 11 patients, three of these patients proved to have significant pathology that altered management. Even though this number may seem small, this is a substantial clinical benefit when one considers how often manometric studies are either negative or borderline without impact on clinical management. These results are also in line with results from Blonski et al who reported a 10% increase in the detection of abnormal motility using viscous swallows (7). The addition of these 4 swallows adds minimal cost and time to the evaluation and should become an integral part of the manometric protocol, especially if patients report solid food dysphagia. Patients with an EGJ obstruction may benefit from further evaluation with imaging or endoscopic ultrasound.
A potential limitation of this study was the inclusion of only 5 upright swallows for the comparison with the 10 supine swallows. This was done to minimize the added time necessary to complete the manometric protocol. However, there did not appear to be a significant difference between the 10 and 5 supine swallow protocol or a substantial difference when we compared the 5 and 10 supine swallow protocols to the 5 upright swallow protocol independently. Thus, it is unlikely that our data would have changed substantially if the swallow protocol was increased to include 10 upright swallows.
Another potential limitation of the study was that we utilized supine normative data to classify the upright swallows into the Chicago Classification diagnosis. Previous studies using conventional manometry or HRM have shown that the distal esophageal contraction and EGJ morphology and pressure profile change after shifting to the upright position (3, 8). This, in and of itself, could alter some diagnoses in borderline cases. However, the major findings in our study were of large changes in IRP or DCI that could not be explained by the relatively minor postural related changes. Hence, the EGJ obstruction and hypercontractility exhibited in those patients would be significant regardless of the thresholds utilized. Furthermore, normative ranges in a small control population have recently been published and our results would not be altered if we utilized those threshold values for IRP and DCI (5).
In conclusion, our results demonstrate that HRM parameters can be altered by changes in posture and that this leads to a change in diagnosis beyond what was seen with the standard Chicago Classification swallow protocol, which is limited to 10 supine swallows. Additionally, it appears that provocative bolus challenges with viscous liquid and a solid bolus are helpful in eliciting a subtle EGJ obstruction that can be missed with only liquid swallows. Together, these finding suggest that an optimal protocol for HRM should include a combination of 10 supine water swallows, 5 upright water swallows, and provocative viscous and solid swallows to increase the diagnostic yield of HRM. The proposed swallow protocol can be performed in a reasonable time period and should not significantly add to the overall cost of the procedure.
Acknowledgments
Funding: This work was supported by R01 DK079902 (JEP) and R01 DK56033 (PJK) from the Public Health Service.
Footnotes
Specific author contributions: Study concept, acquisition of data, analysis, drafting, study supervision : Yinglian Xiao; Acquisition of data and analysis: Frédéric Nicodème, Zhiyue Lin and Roman Sabine; Study concept, acquisition of data, analysis, drafting, study supervision, finalizing the manuscript: Peter J. Kahrilas and John E. Pandolfino
Conflict of interest: John E. Pandolfino [Given imaging and Sandhill Scientific (consulting, educational), Sabine Roman [Given imaging (consulting)]
No other conflicts for remaining authors (YX, FN, PJK, ZL)
Reference
- 1.Bredenoord MF AJ, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJPM. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(S1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sears VW, Jr., Castell JA, Castell DO. Comparison of effects of upright versus supine body position and liquid versus solid bolus on esophageal pressures in normal humans. Dig Dis Sci. 1990;35(7):857–64. doi: 10.1007/BF01536799. [DOI] [PubMed] [Google Scholar]
- 3.Tutuian R, Katz PO, Gideon RM, Castell DO. Normal values for esophageal manometry in the sitting position. Am J Gastroenterol. 2001;96(Suppl):S41. [Google Scholar]
- 4.Babaei A, Mittal RK. Cardiovascular compression of the esophagus and spread of gastro-esophageal reflux. Neurogastroenterol Motil. 2011;23(1):45–51. doi: 10.1111/j.1365-2982.2010.01606.x. [DOI] [PubMed] [Google Scholar]
- 5.Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011;23(6):509–e198. doi: 10.1111/j.1365-2982.2011.01682.x. [DOI] [PubMed] [Google Scholar]
- 6.Allen ML, Orr WC, Mellow MH, Robinson MG. Water swallows versus food ingestion as manometric tests for esophageal dysfunction. Gastroenterology. 1988;95(3):831–3. doi: 10.1016/s0016-5085(88)80036-2. [DOI] [PubMed] [Google Scholar]
- 7.Blonski W, Hila A, Jain V, Freeman J, Vela M, Castell DO. Impedance manometry with viscous test solution increases detection of esophageal function defects compared to liquid swallows. Scand J Gastroenterol. 2007;42(8):917–22. doi: 10.1080/00365520701245702. [DOI] [PubMed] [Google Scholar]
- 8.Bernhard A, Pohl D, Fried M, Castell DO, Tutuian R. Influence of bolus consistency and position on esophageal high-resolution manometry findings. Dig Dis Sci. 2008;53(5):1198–205. doi: 10.1007/s10620-007-0014-z. [DOI] [PubMed] [Google Scholar]
- 9.Roman S, Damon H, Pellissier PE, Mion F. Does body position modify the results of oesophageal high resolution manometry? Neurogastroenterol Motil. 2010;22(3):271–5. doi: 10.1111/j.1365-2982.2009.01416.x. [DOI] [PubMed] [Google Scholar]