Abstract
Background
In the first population-based study of psychopathology conducted in Haiti, we documented earthquake-related experiences associated with risk for posttraumatic stress disorder (PTSD) and major depressive disorder (MDD) 2–4 months following the 2010 Haiti earthquake.
Methods
A population-based survey was conducted of 1,323 survivors randomly selected from the general nondisplaced community, internally displaced persons camps, and a community clinic. Respondents were from the Nazon area of Port-au-Prince, ~20 miles from the epicenter.
Results
Respondents (90.5%) reported at least one relative/close friend injured/killed, 93% saw dead bodies, and 20.9% lost their job post-earthquake. The prevalence of PTSD (24.6%) and MDD (28.3%) was high. History of violent trauma was associated with risk of PTSD and MDD (adjusted odds ratio [AOR] 1.4, 95% confidence interval [CI], 1.0–1.9; AOR, 1.7, 95% CI 1.3, 2.2, respectively). Low social support (AOR, 1.7, 95% CI 1.2, 2.3; AOR 1.4, 95% CI 1.0, 1.9, respectively) increased risk of PTSD and MDD among women. Suffering damage to the home increased risk of MDD in males (AOR 2.8, 95% CI 1.5, 5.5). Associations between being trapped in rubble, major damage to house, job loss, and PTSD; and participation in rescue/recovery, friends/family injured/killed, and MDD varied based on prior history of violent trauma.
Conclusions
Addressing mental health in a post-earthquake setting such as Haiti will require focusing resources on screening and treatment of identified vulnerable groups while targeting improvement of post-earthquake living conditions. Investment in sources of social support for women may make help mitigate the vulnerability of women to PTSD and MDD.
Keywords: depression, anxiety, posttraumatic stress disorder, trauma, mood disorders, life events/stressors, gender
INTRODUCTION
Haiti is the poorest country in the Western Hemisphere, with most persons living on less than $2/day, and half below the extreme poverty line of $1/day.[1] Hurricanes, political unrest, violence, and human rights abuses have contributed to the vulnerability of the population over the past decades.[1,2] The earthquake that struck Port-au-Prince on January 12, 2010 resulted in approximately 200,000 deaths, more than 300,000 injured, the destruction or damage of 286,000 of 411,00 homes, and more than 1 million internally displaced persons (IDP).[3]
Many risk factors have been described for the development of psychopathology, primarily posttraumatic stress disorder (PTSD) and major depressive disorder (MDD), in postdisaster settings.[4,5] These factors can be categorized as pre-event (prior personal or family history of a mental health disorder and history of exposure to traumatic events and life stressors),[6] perievent (loss of family members or close friends,[7] difficulty in contacting loved ones,[8] degree of injury,[9] and witnessing of dead bodies[10]) and postevent (loss of financial and social support resources[11]). However, marked heterogeneity exists in individual responses to the same event and some persons do well even after extreme experiences,[12] whereas certain population groups, such as those with a predisaster history of adversity, may be especially vulnerable to developing mental health problems after a disaster.[13–15] The confluence of stressors and traumas that characterized the daily pre-earthquake experience of the Port-au-Prince population suggests that pre-earthquake adversities may play a particularly strong role in the development of psychopathology following the disaster. To our knowledge, no prior population-based study has documented the determinants of postdisaster mental health status of the Haitian population.
Previous studies of natural disasters have shown that women are at higher risk for PTSD and depression following disasters.[16] Such a consistent finding has led to calls for secondary prevention efforts of PTSD and depression to focus on women. Yet before such targeted intervention efforts are possible, we must understand the particular impact that pre-, peri-, and postdisaster risk factors have on levels of psychopathology in women versus men. This is especially important in Haiti, where the high degree of gender inequality and gendered social roles may result in gender-specific effects of earthquake-related traumatic events and stressors such as exposure to violence, injury or sickness to family members, and job loss.[17]
Building on a body of literature that has well documented the burden of mental illness after disasters through population-based studies,[4,10] we conducted a population-based study in Port-au-Prince, Haiti to document the prevalence of earthquake experiences and the prevalence and determinants of PTSD and MDD, 2 months after the earthquake. Given the accumulation of adverse circumstances among the Haitian population before the earthquake, we also examined whether heterogeneity in responses to disaster-related adverse events existed by a predisaster history of violent trauma. All analyses were conducted for the total sample and by gender, to identify gender-specific risk factors for psychopathology. This is the first population-based survey on psychiatric disorders ever to be conducted in Haiti. Understanding risk for major psychiatric disorders after mass traumatic events in low-resourced settings such as Haiti can help us identify common determinants of psychopathology across distinct settings, and can offer evidence about the consequences of comparable future events in at-risk highly vulnerable populations.
MATERIALS AND METHODS
We randomly enrolled survivors in the Nazon area of Port-au-Prince (Fig. 1). This area not only exhibited a high level of displacement, loss of life, and destruction, but it also exhibited variation in level of damage and a range of living conditions (displaced vs. nondisplaced), which best allowed us to examine how level of exposure to different types of earthquake-related experiences was associated with PTSD and MDD. From March 12 through April 20, 2010 (2–3.5 months postevent), a population-based, random sample of survivors was obtained in three sampling frames: (1) nondisplaced survivors living within the community, (2) IDP living in official displacement camp sites, and (3) nondisplaced survivors attending a local primary healthcare clinic, all located in the same earthquake-affected area. Eligible individuals included those aged 18 or older who were present in the earthquake-affected zone during the earthquake and at least 1 month prior.
Figure 1.
Nazon Area of Port-au-Prince where nondisplaced, internally–displaced, and community clinic-attending survivors were sampled. The white circle represents the earthquake epicenter, 10 miles southwest of Port-au-Prince (shaded) as reported by the U.S. Geological Service. The black circle represents the Institut Fame Pereo (IFP) community clinic. Sources: Open street map; Global Administrative Areas; UN Office for the Coordination of Humanitarian Affairs.
To obtain the community sample, we compiled a comprehensive map of the area by merging preexisting open-source maps and conducting an on-ground assessment. Existing neighborhoods within the defined urban area were block-listed, and primary sampling units were created by dividing the catchment area into a grid comprising 32 zones, roughly 500 m2 each. Of these, 16 were randomly selected using Proc-Survey select in SAS (SAS Institute Inc. SAS 9.2. Cary, NC 2002–2008). The sampling proportion was equal across all zones with 32 persons/zone. From a predetermined starting point within each zone, interviewers approached a candidate to interview at each seventh extant dwelling on their left (temporary shelters included). If the dwelling was destroyed or had no eligible persons, the adjacent dwelling was selected. If more than one eligible respondent existed, the individual with the birthday closest to the interview date was selected.
The IDP camp sample was obtained by randomly selecting four of the eight official displacement sites within our catchment area as recognized by the World Food Programme (WFP).[18] The number of respondents sampled from each camp was weighted based on the published camp census.[18] Interviewers chose a central starting point within each camp, and approached an individual to interview at each third shelter on their left. If no eligible person was found, a person was approached at the adjacent shelter. If more than one eligible respondent was present, the closest birthday method was used. Sampling in both community and camp frames was conducted 7 days/week, during varying times of day.
Third, we recruited a sample of participants from a large community clinic in the middle of the catchment area by approaching every third patient registering for community care at Institut Fame Pereo (IFP). This study was approved by the Internal Review Board at Columbia University and was reviewed by the IFP administration and the Ministry of Health in Haiti. Written or oral (in case of illiteracy) consent in the presence of a witness was obtained from all participants. It is in compliance with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
INSTRUMENT DESIGN AND FIELDING
A structured questionnaire, based on previously validated measures, obtained information about pre-, peri-, and post-earthquake factors that included (a) demographic characteristics, (b) lifetime traumatic events, (c) experiences during and around the earthquake, (d) post-earthquake social support, as well as (e) earthquake related PTSD, and (f) earthquake related MDD. The instrument was developed in English then translated into Haitian Creole using the committee method.[19] Interviewers underwent an 8-hr training period that included cognitive interviewing, practice interviewing, and role playing.
PRE-EARTHQUAKE FACTORS
Demographic Characteristics
Information was collected on age, sex, marriage, education (completed secondary education or not), number of children, and pre-earthquake employment status.
Lifetime Violent Traumatic Event Experience
We assessed past traumas by asking 15 Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV category A traumas.[20] We modified this scale to include whether the respondent had ever been kidnapped, reported to be a problem in Haiti.[2] Respondents who reported violent or assaultive category A traumas were coded as having a prior history of violent trauma.
Someone Close with Mental Illness
We asked respondents whether, before the earthquake, they experienced the mental illness of someone close to them. Examples provided were clinical depression and anxiety disorder.
PERI-EARTHQUAKE FACTORS
Earthquake Experiences
We collected information on damages resulting from the earthquake, length of separation from relatives/friends, injuries to self, injuries/deaths of relatives/friends, seeing dead bodies, damage to house, and involvement in rescue/recovery efforts.
POST-EARTHQUAKE FACTORS
Family Member with Mental Illness
We asked respondents whether, after the earthquake, they experienced having a family member with a mental illness.
POST-EARTHQUAKE SOCIAL SUPPORT
We used four items from the Inventory of Postdisaster Social Support (α = 0.92), which summarizes the help received from family and friends post-earthquake.[21] The lowest tertile of this summary score represented low social support.
Loss of Occupation as a Result of the Earthquake
If the respondent or head of household were employed at the time of the earthquake but not after, they were coded as losing the occupation post-earthquake.
Assessment of Earthquake-Related PTSD
We used the PTSD Checklist (PCL), modified to include DSM-IV-TR diagnostic criteria A–F, to assess earthquake-related PTSD.[22] Respondents indicated, on a 5-point scale, the degree to which they were bothered by the 17 DSM-IV PTSD symptoms using the earthquake as the traumatic experience. The utility of the measure with diverse populations is supported.[23] We identified PTSD cases by using a PCL symptom cut-off of 3 or more for each question and then applying DSM-IV-TR criteria A through F.
Assessment of Earthquake-Related MDD
We used the Patient Health Questionnaire-9 (PHQ-9) to assess depression.[24] Respondents were asked to indicate whether, since the earthquake, they had ever had a period of at least 2 weeks during which they experienced each symptom, with response options of “yes” and “no.” This brief instrument possesses one-to-one correspondence to DSM-IV symptoms of major depression and its psychometric properties and construct validity are known.[24] We identified MDD cases by using an MDD symptom cutoff of 7 or more for each question and then applying DSM-IV-TR criteria.
Clinical Reappraisal of the Survey Instrument
An original validation the PCL has reported high convergent validity (correlations greater than 0.90 with other measures of PTSD symptom severity[23]), excellent internal consistency reliability (α = 0.95), and a 3-day test– retest reliability of 0.97.[23] These results are consistent with a clinical reappraisal on these measures, adapted for DMS-IV-TR, conducted in a different sample.[22] We further conducted a Haiti-specific reappraisal on a subsample of 56 participants enrolled in this study, both to assess validity of instrument in local setting and to obtain a more conservative assessment of MDD than in previous implementations. A licensed, trained psychologist conducted clinical interviews using the Structured Clinical Interview for DSM-IV-TR. We found comparably moderate-to-high internal consistency (α = 0.84 for PTSD and α = 0.65 for MDD) to previously published results and, high specificity but moderate sensitivity consistent with previous work.[22]
STATISTICAL ANALYSIS
χ2 statistics and the Kruskal–Wallis test were used for univariable analyses. Multivariable logistic models assessed the relation between pre-event, peri-earthquake, and post-earthquake factors and to the odds of PTSD and MDD for the total sample, for females, and for males. In order to test whether the relationship between peri and post-earthquake factors and PTSD and MDD differed by a pre-earthquake history of violent trauma, separate multivariable models were also estimated with interaction terms between an earthquake-related factor and prior violent trauma history. All statistical tests were two-sided and exact methods used when appropriate.
RESULTS
Of 1,328 survivors approached, 1,323 consented, of whom 8 did not meet inclusion criteria; 1,315 participants were assessed. Thus, 1,315 participants were assessed, of whom 524 (39.8%), 522 (39.6%), and 269 (20.4%) were from the community, IDP camps, and the clinic, respectively. Table 1 shows the prevalences of pre-, peri-, and post-earthquake factors in the three sampling groups. Strikingly, 90.5% of respondents reported at least one relative or close friend injured/killed because of the earthquake. Only 1.4 and 0.4% of respondents did not endorse symptoms of PTSD and MDD, respectively. Current PTSD was present in 24.6% of survivors (29.7, 19.1, and 25.2% in IDP camps, community, and clinic-based samples, respectively, P < .01) whereas current MDD with impairment was present in 28.3% (28.8, 21.9, and 39.8% in IDP camps, community, and clinic-based respondents, respectively, P < .01). PTSD and MDD were comorbid in 12.5% of respondents, 14.5% of females, and 7.5% of males (P < .001).
TABLE 1.
Demographic characteristics and earthquake related experiences in a cohort of Haitians in the BelAir-Nazon area of Port-au-Prince exposed to the January 12 earthquake, by sampling sitea
| Total (n = 1,313) | Camp (n = 522) | Community (n = 522) | Clinic (n = 269) | ||
|---|---|---|---|---|---|
| Characteristics | n (%)b | n (%)b | n (%)b | n (%)b | P valuei |
| Pre-earthquake factors | |||||
| Younger than 30 | 398 (30.8) | 197 (38.4) | 146 (28.4) | 53 (19.7) | <.01 |
| Female | 933 (71.1) | 371 (71.1) | 346 (66.3) | 216 (80.3) | <.01 |
| Married | 285 (21.7) | 77 (14.8) | 166 (31.8) | 42 (15.6) | <.01 |
| Number of children, mean (SD) | 2.3 (2.02) | 2.3 (2.09) | 2.12 (2.06) | 2.6 (1.76) | <.01 |
| Secondary education completed | 258 (20.1) | 56 (10.9) | 159 (31.5) | 43 (16.2) | <.01 |
| Mental illness of close friend/relative | 387 (29.7) | 137 (26.6) | 163 (31.5) | 87 (32.5) | >.05 |
| Prior history of violent traumac | 479 (36.5) | 177 (34) | 169 (32.4) | 133 (49.4) | <.01 |
| Peri-earthquake factors | |||||
| Major damage to housed | 757 (57.8) | 360 (69.1) | 236 (45.4) | 161 (59.9) | <.01 |
| Trapped by rubble during earthquake | 82 (6.3) | 43 (8.3) | 25 (4.8) | 14 (5.2) | .049 |
| Physically injured as a result of earthquake | 228 (17.4) | 99 (19) | 86 (16.5) | 43 (16) | >.05 |
| Saw dead bodies during/after earthquake | 1,210 (93) | 500 (96.5) | 465 (90.5) | 245 (91.1) | <.01 |
| Involved in rescue/recovery efforts | 429 (33) | 159 (31) | 187 (36.1) | 83 (31) | >.05 |
| Number of relatives and close friends killed or injured | |||||
| None | 123 (9.5) | 67 (13) | 37 (7.2) | 19 (7.1) | <.01 |
| Between 1 and 5 | 581 (44.7) | 237 (45.8) | 236 (45.8) | 108 (40.3) | |
| Between 6 and 10 | 307 (23.6) | 111 (21.5) | 124 (24.1) | 72 (26.9) | |
| Greater than 10 | 289 (22.2) | 102 (19.7) | 118 (22.9) | 69 (25.7) | |
| Post-earthquake factors | |||||
| Family member has mental illness | 91 (6.9) | 16 (3.1) | 47 (9) | 28 (10.4) | <.01 |
| Lost job as a result of earthquakee | 270 (20.9) | 111 (21.6) | 115 (22.5) | 44 (16.5) | <.01 |
| Low social supportf | 462 (35.3) | 188 (36.2) | 160 (30.8) | 114 (42.4) | <.01 |
| Had PTSDg | 310 (24.6) | 151 (29.7) | 95 (19.1) | 64 (25.2) | <.01 |
| Had MDDh | 371 (28.3) | 150 (28.8) | 114 (21.9) | 107 (39.8) | <.01 |
We recruited a representative sample of participants from three sampling frame: official internally displaced person’s camps in the area, participants who were still in their residence, and participants from a large community clinic in the middle of the catchment area.
Totals may not add up due to missing data.
Number of lifetime traumatic events greater than 5.
Major damage refers to houses that were uninhabitable or demolished as a result of the earthquake; referent is no damage or some damage but still habitable.
Respondent lost job or head of household lost job.
Lowest social support tertile; social support was measured by summing responses to four questions regarding support from family and friends measured on a Likert type scale.
To have PTSD, respondents had to meet DSM criteria A through E as well as have impairment or distress.
To have MDD, respondents had to endorse at least 5 PHQ items and have impairment.
χ2 P value.
Prior history of violent trauma and mental illness of a close friend or relative were the two pre-earthquake factors associated with increased risk of PTSD (OR = 1.38; 95% confidence interval [CI] = 1.03, 1.85 and OR = 1.75; 95% CI = 1.28, 2.39; respectively) (Table 2). During the earthquake, personal injury or injury of family members (i.e. having 1–6 or 6–10 family members injured/killed) were associated with higher risk of PTSD (OR = 1.49; 95% CI = 1.03, 2.16; OR = 1.95; 95% CI = 1.09,3.47; and OR = 2.16; 95% CI = 1.17, 3.98; respectively). Following the earthquake, job loss after earthquake and low social support were associated with increased risk of PTSD (OR = 1.44; 95% CI = 1.03, 2.02 and OR = 1.54; 95% CI = 1.15, 2.07; respectively). One pre-earthquake (mental illness of close friend/relative) and two post-earthquake factors (job loss after earthquake and low social support) increased risk of PTSD and one pre-earthquake factor (marriage) decreased risk of PTSD only among females. In contrast, one peri-earthquake factor (injured as a result of the earthquake) increased PTSD risk specifically in males.
TABLE 2.
Multivariable associations between demographic characteristics and earthquake related experiences and posttraumatic stress (PTSD)a and major depressive disorder (MDD)b in a cohort of Haitians in the BelAir-Nazon area of Port-au-Prince exposed to the January 12 earthquake
| PTSDa | MDDb | |||||
|---|---|---|---|---|---|---|
| Total (n = 1,315)c OR (Lower 95%, Upper 95%) |
Female OR (Lower 95%, Upper 95%) |
Male OR (Lower 95%, Upper 95%) |
Total (n = 1,315)c OR (Lower 95%, Upper 95%) |
Female OR (Lower 95%, Upper 95%) |
Male OR (Lower 95%, Upper 95%) |
|
| Pre-earthquake factors | ||||||
| Younger than 30 | 1.05 (0.74, 1.48) | 1.01 (0.69, 1.50) | 1.27 (0.56, 2.87) | 1.04 (0.75, 1.44) | 1.07 (0.74, 1.56) | 1.04 (0.48, 2.26) |
| Female | 1.43 (0.98, 2.08) | 1.40 (0.99, 1.98) | ||||
| Married | 0.75 (0.51, 1.09) | 0.60 (0.39, 0.94) | 1.6 (0.74, 3.46) | 1.25 (0.90, 1.74) | 1.15 (0.79, 1.69) | 1.56 (0.76, 3.20) |
| Number of children | 1.04 (0.96, 1.12) | 1.02 (0.93, 1.12) | 1.13 (0.97, 1.31) | 1.06 (0.99, 1.14) | 1.08 (0.99, 1.18) | 1.05 (0.90, 1.22) |
| Secondary education completed | 0.82 (0.54, 1.23) | 0.83 (0.50, 1.40) | 0.94 (0.46, 1.90) | 0.93 (0.64, 1.36) | 0.97 (0.60, 1.55) | 0.99 (0.51, 1.93) |
| Mental illness of close friend/relative | 1.75 (1.28, 2.39) | 1.89 (1.32, 2.70) | 1.31 (0.65, 2.66) | 1.75 (1.31, 2.34) | 1.78 (1.28, 2.49) | 1.68 (0.89, 3.17) |
| Prior history of violent trauma | 1.38 (1.03, 1.85) | 1.3 (0.93, 1.82) | 1.93 (0.99, 3.75) | 1.67 (1.27, 2.2) | 1.52 (1.11, 2.08) | 2.65 (1.42, 4.92) |
| Peri-earthquake factors | ||||||
| Major damage to housed | 1.0 (0.74, 1.35) | 0.97 (0.69, 1.36) | 1.2 (0.62, 2.33) | 1.34 (1.01, 1.78) | 1.11 (0.81, 1.53) | 2.83 (1.47, 5.46) |
| Trapped under rubble | 1.45 (0.85, 2.49) | 1.48 (0.81, 2.72) | 1.43 (0.41, 4.99) | 0.94 (0.54, 1.62) | 1.03 (0.56, 1.88) | 0.60 (0.16, 2.22) |
| Physically injured as a result of earthquake | 1.49 (1.03, 2.16) | 1.34 (0.88, 2.05) | 2.47 (1.07, 5.7) | 1.35 (0.94, 1.93) | 1.24 (0.83, 1.85) | 1.88 (0.82, 4.28) |
| Involved in rescue/recovery | 0.93 (0.66, 1.31) | 0.80 (0.52, 1.22) | 1.49 (0.76, 2.94) | 0.85 (0.61, 1.17) | 0.8 (0.54, 1.19) | 1.05 (0.57, 1.94) |
| Number of relatives and close friends killed or injured | ||||||
| None | ||||||
| Between 1 and 5 | 1.95 (1.09, 3.47) | 1.92 (0.98, 3.76) | 1.87 (0.57, 6.18) | 1.62 (0.97, 2.69) | 1.51 (0.83, 2.74) | 1.62 (0.58, 4.55) |
| Between 6 and 10 | 2.16 (1.17, 3.98) | 1.96 (0.96, 3.97) | 3.57 (0.98, 12.98) | 1.0 (0.57, 1.74) | 1.04 (0.55, 1.98) | 0.75 (0.22, 2.59) |
| Greater than 10 | 1.33 (0.71, 2.51) | 1.35 (0.65, 2.81) | 0.97 (0.26, 3.67) | 1.37 (0.79, 2.38) | 1.41 (0.74, 2.68) | 0.90 (0.28, 2.84) |
| Post-earthquake factors | ||||||
| Family member has a mental illness | 1.08 (0.61, 1.90) | 1.13 (0.59, 2.18) | 1.07 (0.30, 3.79) | 1.79 (1.07, 2.99) | 1.98 (1.08, 3.61) | 1.58 (0.50, 4.94) |
| Lost job due to earthquakee | 1.44 (1.03, 2.02) | 1.73 (1.18, 2.53) | 0.81 (0.36, 1.83) | 0.91 (0.65, 1.27) | 1.06 (0.73, 1.54) | 0.52 (0.22, 1.20) |
| Low social supportf | 1.54 (1.15, 2.07) | 1.68 (1.20, 2.34) | 1.27 (0.64, 2.50) | 1.27 (0.96, 1.68) | 1.41 (1.03, 1.94) | 0.95 (0.50, 1.81) |
| Sampling siteg | ||||||
| Clinic | 1 | 1 | 1 | 1 | 1 | 1 |
| Camp | 1.34 (0.92, 1.95) | 1.29 (0.85, 1.97) | 1.38 (0.55, 3.5) | 0.76 (0.54, 1.08) | 0.87 (0.58, 1.28) | 0.40 (0.18, 0.89) |
| Community | 0.75 (0.50, 1.12) | 0.71 (0.45, 1.11) | 0.78 (0.30, 2.05) | 0.53 (0.37, 0.76) | 0.59 (0.39, 0.89) | 0.30 (0.13, 0.69) |
To have PTSD, respondents had to meet DSM criteria A through E as well as have impairment or distress.
To have MDD, respondents had to endorse at least five PHQ items and have impairment.
Data on sex was missing for two respondents.
Major damage refers to houses that were uninhabitable or demolished as a result of the earthquake; referent is no damage or some damage but still habitable.
Respondent lost job or head of household lost job.
Lowest social support tertile; social support was measured by summing responses to four questions regarding support from family and friends measured on a Likert-type scale.
We recruited a representative sample of participants from three sampling frame: official internally displaced person’s camps in the area, participants who were still in their residence, and participants from a large community clinic in the middle of the catchment area.
Prior history of violent trauma and mental illness of a close friend or relative were also the two pre-earthquake predictors of MDD (OR = 1.67; 95% CI: 1.27, 2.20 and OR = 1.75; 95% CI: 1.31, 2.35; respectively) (Table 2). During the earthquake, major damage to the home was associated with higher risk of MDD (OR = 1.34; 95% CI = 1.01, 1.78). Following the earthquake, mental illness of a family member increased the risk of MDD (OR = 1.79; 95% CI = 1.07, 2.99). One pre-earthquake (close friend/family member had a mental illness) and two post-earthquake factors (family member had a mental illness and low social support) increased risk of MDD only among females, whereas one peri-earthquake factor (major damage to house) only increased risk of MDD among males.
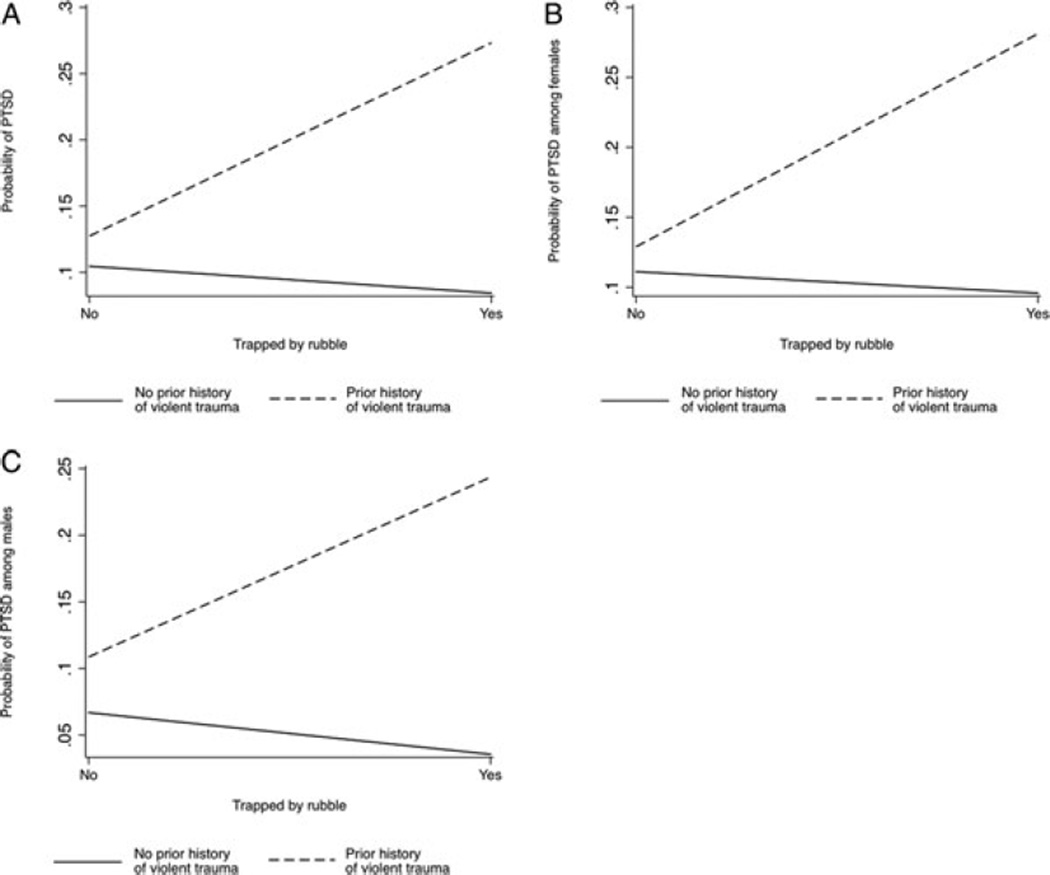
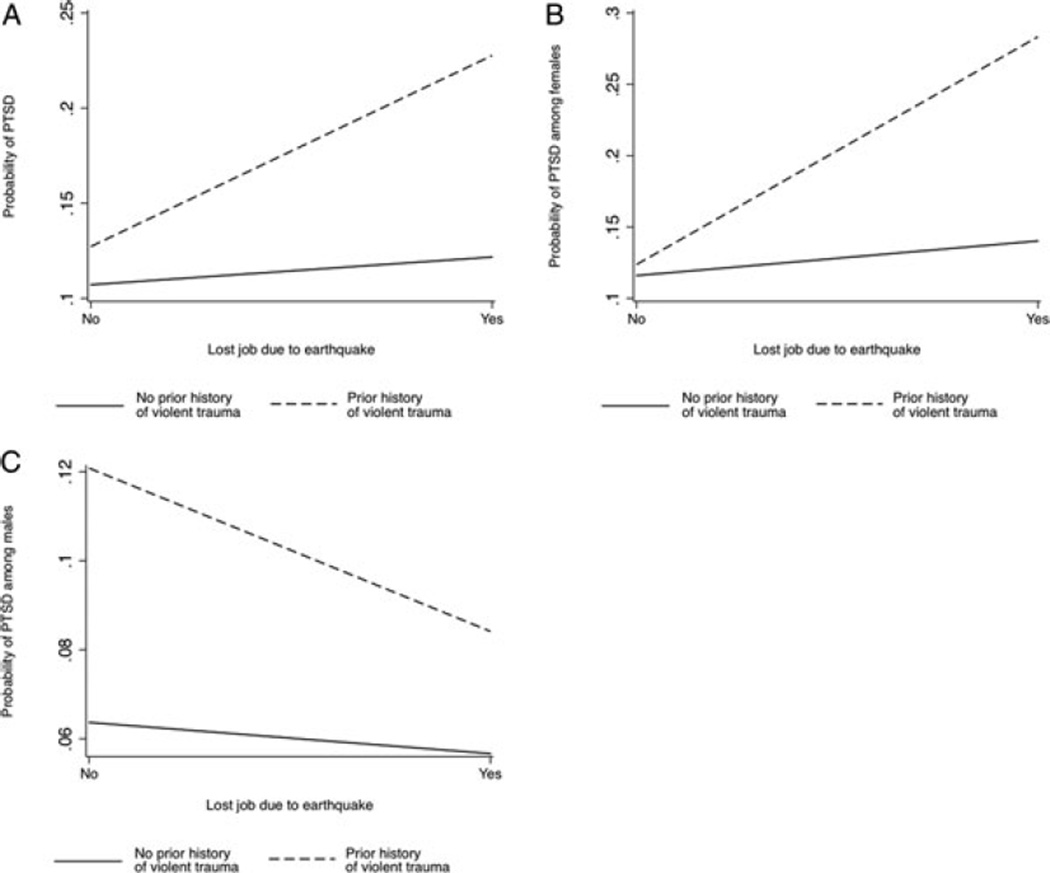
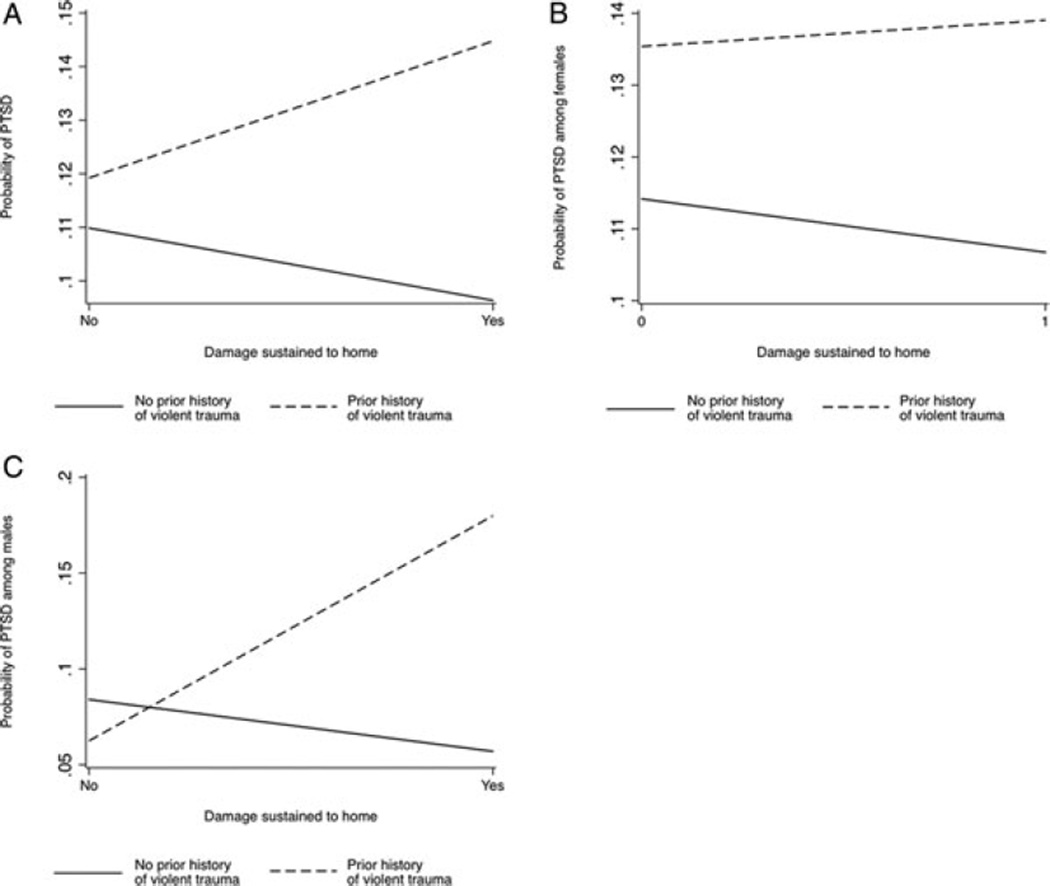
For those earthquake-related factors that had a different relationship with PTSD given a pre-earthquake history of violent trauma, Figures 2(A)– 4(C) present the relationships between peri- and post-earthquake factors and PTSD, by prior trauma history. In the total sample, respondents who had been trapped under rubble and had a prior history of violent trauma were more likely to exhibit PTSD than those who were trapped in the rubble but had no history of violent trauma; the interaction was not significant in the gender-specific samples. Males who had a house that suffered major damage and a prior history of violent trauma were more likely to have PTSD than those who experienced major home damage but had no prior violent trauma history; the interaction was not significant in the total sample or in females. In contrast, females who lost a job as a result of the earthquake and had a prior history of violent trauma had an increased risk of PTSD relative to those who lost a job but had no prior violent trauma history; this interaction was not significant in the total sample or in males.
Figure 2.
(A) Probability of posttraumatic stress disorder (PTSD) by being trapped by rubble and prior history of violent trauma in the total sample. (B) Probability of PTSD by being trapped by rubble and prior history of violent trauma among females. (C) Probability of PTSD by being trapped by rubble and prior history of violent trauma among males.
Figure 4.
(A) Probability of posttraumatic stress disorder (PTSD) by job loss and prior history of violent trauma in the total sample. (B) Probability of PTSD by job loss and prior history of violent trauma among females. (C) Probability of PTSD by job loss and prior history of violent trauma among males.
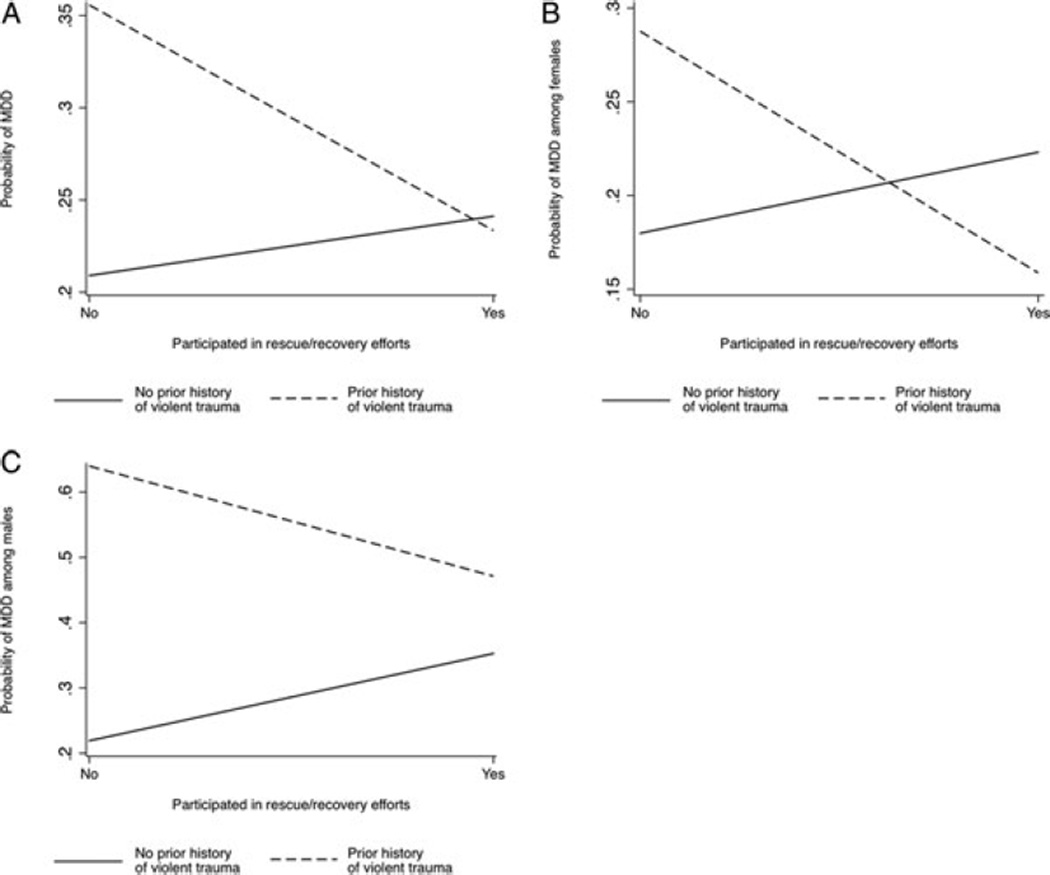
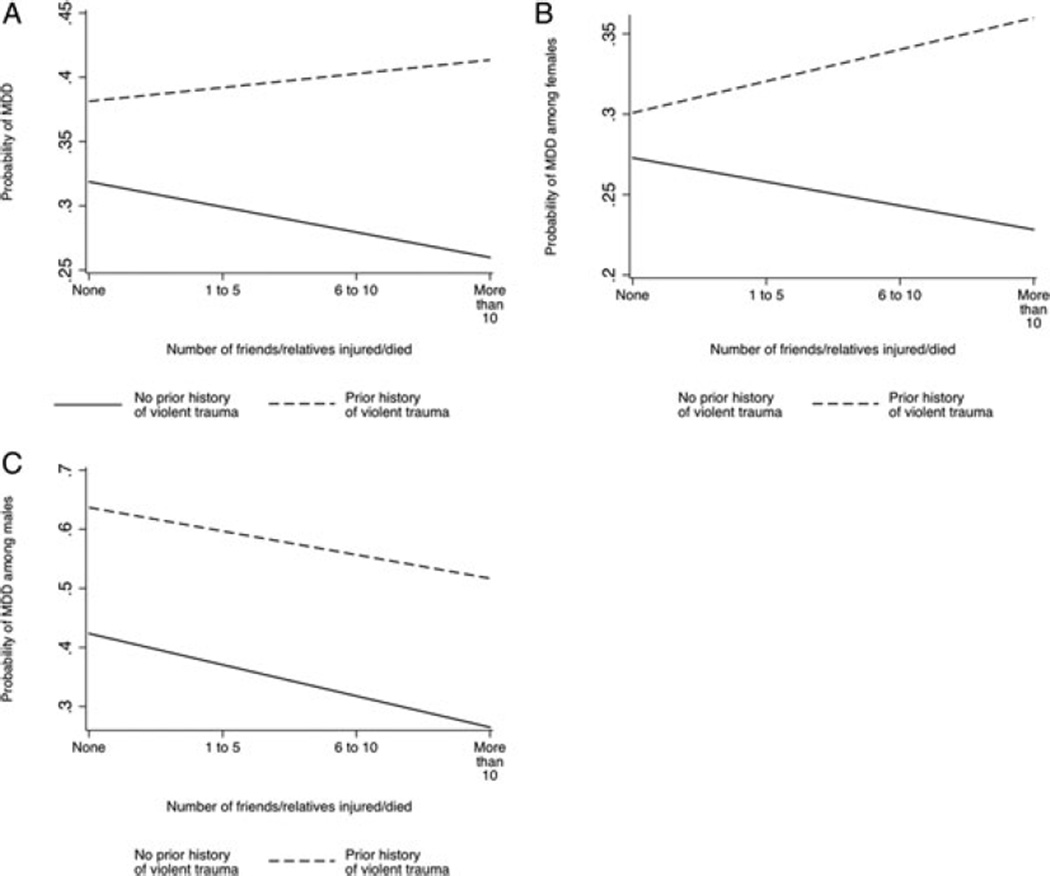
Figures 5(A)–6(C) present the relationships between peri- and post-earthquake factors and MDD that differ by pre-earthquake violent trauma history. In the total sample, those who participated in rescue and recovery and had a prior history of violent trauma were less likely to have MDD than those who participated in rescue and recovery but had no prior history of violent trauma. In the total sample and among females, those who had 1 to 5 or greater than 10 loved ones injured/killed and prior history of violent trauma had an increased risk of MDD than those who experienced injury or death of loved ones but had no prior violent trauma history.
Figure 5.
(A) Probability of major depressive disorder (MDD) by participation in rescue/recovery and prior history of violent trauma in the total sample. (B) Probability of MDD by participation in rescue/recovery and prior history of violent trauma among females. (C) Probability of MDD by participation in rescue/recovery and prior history of violent trauma among males.
Figure 6.
(A) Probability of major depressive disorder (MDD) by injury/death of loved ones and prior history of violent trauma in the total sample. (B) Probability of MDD by injury/death of loved ones and prior history of violent trauma among females. (C) Probability of MDD by injury/death of loved ones and prior history of violent trauma among males.
DISCUSSION
Five central observations emerge. First, there was an extraordinary burden of traumatic events and stressors experienced by the Port-au-Prince population after the earthquake. Second, the prevalence of PTSD and MDD meeting DSM-IV-TR criteria was very high 2 months after the event. Third, those with a history of high lifetime violent trauma faced significantly increased odds of both PTSD and MDD. Fourth, the impact of selected peri- and post-earthquake factors on PTSD and MDD was stronger for individuals who had a prior history of violent trauma. Fifth, experiences associated with MDD and PTSD differed at least marginally significantly between men and women.
The Port-au-Prince population suffered an extraordinary burden of post-earthquake traumatic events, stressors, PTSD, and MDD. The prevalence of injury in this study (17.4%) was higher than that reported in other studies: for example, following a similar magnitude earthquake in Peru, the prevalence of injury was 11.5%.[25] Consistent with the available pre-earthquake literature on Haiti,[26] roughly one third of respondents in this sample reported a prior history of violent or assaultive trauma. The fact that 39.8% of care-seeking survivors in the general practice clinic experienced symptoms consistent with MDD should alert health professionals to the magnitude of the problem in primary care settings after disasters.
The prevalence of PTSD (24.6%) and MDD(28.3%) were also higher than most other post-earthquake population-based studies, which reported prevalences ranging from 3.3 to 24.2% for PTSD, and 20 to 30% for MDD.[25, 27–29]. As one of the worst disasters of the century, the level of damage produced by the Haiti earthquake was significantly more far reaching in terms of deaths, injuries, and infrastructure damage than disasters previously studied in the United States. Further, the predisaster level of economic deprivation, low life expectancy, high rates of infectious disease, and exposure to violence probably led to a ubiquitous predisaster burden of psychological disability in the general population, which substantially influenced the potential for recovery in the general population after this disaster. We are not aware of any comparable pre-earthquake population-based studies of adult psychiatric disorders conducted in Haiti that we could use to empirically compare our post-earthquake results. However, we do know that prior to the earthquake, 40% of children receiving mental health care had been exposed to violence, kidnapping, death of family member, rape, or gang-related violence, which probably led to high baseline levels of psychopathology.[30] Further, a study of immigrant Haitian youth in the United States showed high rates of PTSD and depression (11.6 and 14.0%, respectively).[31] This information indicates that there was likely a significant proportion of the population in Haiti living with, or at risk for, depression and PTSD before the earthquake, although available data indicate that the rates were markedly lower than those we found in this study.
Clinic-based respondents had the highest rates of depression in the study. Multiple epidemiologic studies have found a high prevalence of psychiatric disorders among physically ill patients in clinical settings.[32–34] This phenomenon is due to the disabling consequences of mental disorders: general population based studies have found that psychiatric disorders are associated with somatic complaints and higher general health care service use.[35, 36]
PTSD and MDD had three common risk factors: pre-earthquake history of violent trauma and mental illness of a close friend or relative and post-earthquake low social support. Accumulation of violent traumatic events throughout the life course has been found to increase risk for psychiatric disorders such as PTSD and depression.[37, 38] Pre-earthquake mental illness of a loved one may represent a significant caregiving burden that makes individuals particularly vulnerable to the impact of an earthquake. Prior research also indicates that social support plays a particularly important role in disaster recovery.[39]
Peri-earthquake traumatic events, including physical injury from the earthquake and injury or death of relatives or friends, increased the odds of PTSD but not MDD.[40, 41] Prior studies have also failed to detect a relationship between disaster-related trauma and depression.[40, 41] In contrast, peri- and post-earthquake stressors, such as earthquake-related job loss (in the case of PTSD), post-earthquake family mental illness and major home damage (in the case of MDD), and low social support were associated with both PTSD and MDD.[42–44] The central role of postdisaster material and social resources in shaping the capacity to recover after an instance of mass trauma, and hence exhibit vulnerability to PTSD and depression, is consistent with Conservation of Resources Theory.[45–48] These findings suggest that risk of PTSD is shaped by a range of acute and long-term disaster-related exposures, including peri-earthquake traumatic events but also post-earthquake social and financial stressors. Depression, in contrast, depends more on the accumulation of long-term stressful consequences resulting from acute instances of traumatic experiences.
In Haiti, different types of peri- and post-earthquake social and financial stressors increased the risk for PTSD and MDD among males and females, reflecting gender division of caregiving and property ownership. Job loss was associated with a higher risk of PTSD among women, suggesting that loss of resources may be more distressing for those responsible for the care and wellbeing of their children.[4] In a related fashion, mental illness of a loved one that occurred prior to the earthquake, as well as family mental illness that occurred as a result of the earthquake, increased the risk for PTSD and MDD among women, perhaps reflecting the particular burden females carry for the care of sick family members and friends. In addition, low social support was associated with a higher risk for PTSD and MDD among women, suggesting that although women report more social support than men, they also experience a greater negative impact from their social relations than men.[49–51] Such differences may reflect gender differences in the need to share feelings and problems with others, and in the appreciation and expectations of the existing sources of social support.[49]
In contrast, major damage to the home was associated with MDD among males, potentially related to male control of property titles and responsibility for structural home maintenance.
Pre-earthquake experiences of violent trauma shaped the impact of peri- and post-earthquake risk factors on PTSD and MDD. Earthquake-related traumatic and stressful experiences of loss, including loss and injury to loved ones, damage to the home, and job loss, particularly increased the risk for PTSD or MDD among individuals with prior experience of violent trauma. These findings are consistent with a perspective of “cumulative adversity,”[13–15] which suggests that the accumulation of distal (such as lifetime exposure to violent trauma) and proximal (such as loss of a job after a disaster) stress exposures overwhelms individual capacity to adopt coping mechanisms in future instances of acute trauma, and make individuals especially vulnerable to psychiatric disorders.[37] The interaction functioned in the opposite way when we examined how a history of violent trauma shaped the consequences of involvement in postdisaster rescue and recovery efforts: among individuals with a history of violent trauma, involvement in post-earthquake reconstruction was associated with a lower probability of MDD, whereas no association was found between rescue/recovery efforts and MDD among those with no history of violent trauma. Such findings fit within a challenge model of resilience, which posits that recurrent exposure to moderate levels of risk may lead individuals to mobilize resources, so they are better equipped to overcome adversity in the future.[52] In this case, the sensation of control over the consequences of the earthquake that was provided by rescuing victims and rebuilding communities may be particularly helpful for individuals who had felt no control over prior experiences of violent trauma. The heterogeneity of responses to disaster-related adverse conditions given a prior history of adverse conditions makes the case for shifting away from a uniform postdisaster mental health intervention, to an approach tailored to the needs of individuals that have difficulty adjusting on their own[53, 54]
This study shares with others the limitations of cross-sectional data. Although we tailored the PCL and PHQ-9 to measure earthquake-related PTSD and MDD symptoms, we cannot rule out that individuals exhibited these symptoms prior to the earthquake. Second, neither the PCL nor the PHQ-9are diagnostic instruments; however, both instruments have been validated in several settings and show good reliability and validity.[23, 24] A clinical reappraisal in Haiti found these instruments to be specific but less sensitive suggesting that our estimates of the prevalence of mental illness here may be conservative. Third, reporting of experiences during and after the earthquake may have been affected by recall bias. However, results from longitudinal studies have shown reporting of acute stress exposure to be reliable and generally free from recall bias.[55] Fourth, although we took into account a variety of factors, we may have missed important confounders, such as pre-earthquake psychopathology, income, and housing quality, which could have influenced the impact of the earthquake on PTSD and depression. Fifth, the low number of male respondents (n = 382) may have limited our ability to detect particular associations in the male sample.
CONCLUSION
These limitations notwithstanding, we document a high prevalence of earthquake-related stressors and PTSD and MDD in a representative, population-based study of Haitians exposed to the January 12, 2010 earthquake and identify particularly vulnerable groups. As Haiti prepares to invest in post-earthquake reconstruction this year, these results can provide insight and guidance for the crucial planning and implementation of mental health interventions. Scarce expert mental health resources should focus first on those at greatest risk. Particular attention should also be paid to the caregiving burden placed on women in postdisaster Haiti—investment in formal and informal sources of social support for women may make help mitigate the particular vulnerability of women to PTSD and MDD. Post-earthquake capacity-building efforts such as home rebuilding efforts and employment support programs will provide benefit in parallel by addressing ongoing disaster-related adverse circumstances shown here to be associated with PTSD and MDD. Rebuilding efforts are not to be dissociated from their mental public health impact.
Figure 3.
(A) Probability of posttraumatic stress disorder (PTSD) by damage to house and prior history of violent trauma in the total sample. (B) Probability of PTSD by damage to house and prior history of violent trauma among females. (C) Probability of PTSD by damage to house and prior history of violent trauma among males.
Acknowledgments
This work was supported by the Mailman School of Public Health intramural research funds. SG is partially supported by the Anna CheskisGelman and Murray Charles Gelman Professorship of Epidemiology. MD is partially supported by the EHESP Chair of Chronic Disease. The authors did not enter an agreement with the funding organization that may have limited their ability to complete the research as planned. The authors have full control of all primary data.
REFERENCES
- 1.Verner D. Making Poor Haitians Count: Poverty in Rural and Urban Haiti Based on the First Household Survey for Haiti. Washington, DC: World Bank Policy Research Working Paper Series; 2008. [Google Scholar]
- 2.Kolbe AR, Hutson RA. Human rights abuse and other criminal violations in Port-au-Prince, Haiti: a random survey of households. Lancet. 2006;368(9538):864–873. doi: 10.1016/S0140-6736(06)69211-8. [DOI] [PubMed] [Google Scholar]
- 3.Magnitude 7.0 – HAITIREGION. United States Geological Survey. 2010 Jan 12; [Google Scholar]
- 4.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65(3):207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 5.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65(3):240–260. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- 6.Galea S, Brewin CR, Gruber M, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wickrama KA, Kaspar V. Family context of mental health risk in tsunami-exposed adolescents: findings from a pilot study in Sri Lanka. Soc Sci Med. 2007;64(3):713–723. doi: 10.1016/j.socscimed.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 8.Stimpson J. Short communication: prospective evidence for a reciprocal relationship between sense of control and depressive symptoms following a flood. Stress Health. 2006;22:161–166. [Google Scholar]
- 9.North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. J Am Med Assoc. 1999;282(8):755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- 10.Galea S, Ahern J, Resnick H, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- 11.Kaniasty K, Norris FH. A test of the social support deterioration model in the context of natural disaster. J Pers Soc Psychol. 1993;64(3):395–408. doi: 10.1037//0022-3514.64.3.395. [DOI] [PubMed] [Google Scholar]
- 12.Norris FH, Stevens SP, Pfefferbaum B, et al. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. Am J Community Psychol. 2008;41(1–2):127–150. doi: 10.1007/s10464-007-9156-6. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd DA, Turner RJ. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug Alcohol Depend. 2008;93(3):217–226. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. J Health Soc Behav. 1995;36(4):360–376. [PubMed] [Google Scholar]
- 15.Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: racial/ethnic contrasts. Addiction. 2003;98(3):305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- 16.Bromet EJ, Havenaar JM. Mental health consequences of disasters. In: Sartorius N, Gaebel W, López-Ibor J, Maj M, editors. Psychiatry in Society. Chichester, UK: John Wiley & Sons; 2002. pp. 241–262. [Google Scholar]
- 17.Padgett A, Warnecke T. Diamonds in the rubble: The women of Haiti institutions, gender equity and human development in Haiti. J Econ Issues. 2011;45(3):527–557. [Google Scholar]
- 18.Port-au-Prince IDP camps and main distribution sites. World Food Program. 2010 Feb 18; [Google Scholar]
- 19.Schoua-Glusberg A. Translating research instruments: committee approach + focus groups research support services. 2004 [Google Scholar]
- 20.Breslau N, Peterson EL, Poisson LM, et al. Estimating posttraumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychol Med. 2004;34(5):889–898. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- 21.Kaniasty K, Norris FH. Help-seeking comfort and receiving social support: the role of ethnicity and context of need. Am J Community Psychol. 2000;28(4):545–581. doi: 10.1023/a:1005192616058. [DOI] [PubMed] [Google Scholar]
- 22.Uddin M, Aiello AE, Wildman DE, et al. Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proc Natl Acad Sci U S A. 2010;107(20):9470–9475. doi: 10.1073/pnas.0910794107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weathers F, Litz B, Herman D, et al. Meeting of the International Society of Traumatic Stress Studies. San Antonio TX: 1993. Oct, The PTSD checklist (PCL): reliability, validity, and diagnostic utility. [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cairo JB, Dutta S, Nawaz H, et al. The prevalence of posttraumatic stress disorder among adult earthquake survivors in Peru. Disaster Med Public Health Prep. 4(1):39–46. [PubMed] [Google Scholar]
- 26.Geneva, Switzerland: World Health Organization; 2010. Mental health in Haiti: a literature review: Department of Mental Health and Substance Abuse. [Google Scholar]
- 27.Chadda RK, Malhotra A, Kaw N, et al. Mental health problems following the 2005 earthquake in Kashmir: findings of community-run clinics. Prehosp Disaster Med. 2007;22(6):541–545. doi: 10.1017/s1049023x00005409. discussion 546. [DOI] [PubMed] [Google Scholar]
- 28.Wang L, Zhang Y, Shi Z, Wang W. Symptoms of posttraumatic stress disorder among adult survivors two months after the Wenchuan earthquake. Psychol Rep. 2009;105(3 Pt 1):879–885. doi: 10.2466/PR0.105.3.879-885. [DOI] [PubMed] [Google Scholar]
- 29.Lai TJ, Chang CM, Connor KM, et al. Full and partial PTSD among earthquake survivors in rural Taiwan. J Psychiatr Res. 2004;38(3):313–322. doi: 10.1016/j.jpsychires.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Aea Jaimes. Haiti-Quebec-Canada: towards a partnership in mental health proceedings. Quebec, Canada: 2008. Apr, Haiti santé mental. [Google Scholar]
- 31.Fawzi MCS, Betancourt TS, Marcelin L, et al. Depression and post-traumatic stress disorder among Haitian immigrant students: implications for access to mental health services and educational programming. Bmc Public Health. 2009;9:482–493. doi: 10.1186/1471-2458-9-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler LG, Burns BJ, Shapiro S, et al. Psychiatric diagnoses of medical service users: evidence from the Epidemiologic Catchment Area Program. Am J Public Health. 1987;77(1):18–24. doi: 10.2105/ajph.77.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rapp SR, Parisi SA, Wallace CE. Comorbid psychiatric disorders in elderly medical patients: a 1-year prospective study. J Am Geriatr Soc. 1991;39(2):124–131. doi: 10.1111/j.1532-5415.1991.tb01613.x. [DOI] [PubMed] [Google Scholar]
- 34.Martucci M, Balestrieri M, Bisoffi G, et al. Evaluating psychiatric morbidity in a general hospital: a two-phase epidemiological survey. Psychol Med. 1999;29(4):823–832. doi: 10.1017/s0033291799008491. [DOI] [PubMed] [Google Scholar]
- 35.Koopmans GT, Donker MC, Rutten FH. Commonmental disorders and use of general health services: a review of the literature on population-based studies. Acta Psychiatr Scand. 2005;111(5):341–350. doi: 10.1111/j.1600-0447.2005.00496.x. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Campayo J, Ayuso-Mateos JL, Caballero L, et al. Relationship of somatic symptoms with depression severity, quality of life, and health resources utilization in patients with major depressive disorder seeking primary health care in Spain. Prim Care Companion J Clin Psychiatry. 2008;10(5):355–362. doi: 10.4088/pcc.v10n0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bremner J, Southwick S, Brett E, Fontana A. Dissociation and posttraumatic stress disorder in Vietnam combat veterans. Am J Psychiatry. 1992;149:328–332. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- 38.Palacios L, Heinze G. Post-traumatic stress disorder: a review (part one) Salud Ment. 2002;25(3):19–26. [Google Scholar]
- 39.Kaniasty K, Norris FH. Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. J Trauma Stress. 2008;21(3):274–281. doi: 10.1002/jts.20334. [DOI] [PubMed] [Google Scholar]
- 40.Gabriel R, Ferrando L, Corton E, et al. Psychopathological consequences after a terrorist attack: an epidemiological study among victims, the general population, and police officers. Eur Psychiatry. 2007;22(6):339–346. doi: 10.1016/j.eurpsy.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 41.Miguel-Tobal J, Cano-Vindel A, Gonzalez-Ordi H, et al. PTSD and depression after the Madrid March 11 train bombings. J Traumat Stress. 2006;14(3):511–526. doi: 10.1002/jts.20091. [DOI] [PubMed] [Google Scholar]
- 42.Kun P, Han S, Chen X, Yao L. Prevalence and risk factors for posttraumatic stress disorder: a cross-sectional study among survivors of the Wenchuan 2008 earthquake in China. Depress Anxiety. 2009;26(12):1134–1140. doi: 10.1002/da.20612. [DOI] [PubMed] [Google Scholar]
- 43.Norris F, Perilla J, Riad J, et al. Stability and change in stress, resources, and psychological distress following natural disaster: findings from Hurricane Andrew. Anxiety Stress Coping. 1999;12:363–396. doi: 10.1080/10615809908249317. [DOI] [PubMed] [Google Scholar]
- 44.Rhodes J, Chan C, Paxson C, et al. The impact of Hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am J Orthopsychiatry. 2010;80(2):237–247. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bleich A, Gelkopf M, Melamed Y, Solomon Z. Mental health and resiliency following 44 months of terrorism: a survey of an Israeli national representative sample. BMC Med. 2006;4 doi: 10.1186/1741-7015-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hobfoll SE, Canetti-Nisim D, Johnson RJ, et al. The association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to repeated acts of terrorism in Israel. J Trauma Stress. 2008;21(1):9–21. doi: 10.1002/jts.20307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing Conservation of Resources theory. Appl Psychol. 2001;50(3):337–370. [Google Scholar]
- 48.North CS, Kawasaki A, Spitznagel EL, Hong BA. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J Nervous Ment Dis. 2004;192(12):823–829. doi: 10.1097/01.nmd.0000146911.52616.22. [DOI] [PubMed] [Google Scholar]
- 49.Sonnenberg CM, Deeg DJ, van Tilburg TG, et al. Gender differences in the relation between depression and social support in later life. Int Psychogeriatr. 2012:1–10. doi: 10.1017/S1041610212001202. [DOI] [PubMed] [Google Scholar]
- 50.Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry. 2001;158(4):587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- 51.Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–451. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- 52.Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 53.Litz BT. Early intervention for trauma: where are we and where do we need to go? A commentary. J Trauma Stress. 2008;21(6):503–506. doi: 10.1002/jts.20373. [DOI] [PubMed] [Google Scholar]
- 54.Litz BT, Gray MJ, Bryant RA, Adler AB. Early intervention for trauma: current status and future directions. Clin Psychol. 2002;9(2):112–134. [Google Scholar]
- 55.Norris FH, Kaniasty K. A longitudinal study of the effects of various crime prevention strategies on criminal victimization, fear of crime, and psychological distress. Am J Community Psychol. 1992;20(5):625–648. doi: 10.1007/BF00941775. [DOI] [PubMed] [Google Scholar]