Introduction
Complete androgen insensitivity syndrome (AIS) is a medical condition which affects the development of the genital and reproductive system. This raises some very uncomfortable issues about gender identity that are difficult to put into words.
The first medical report on AIS was published in 1953 by J. M. Morris, an American gynecologist.
Case History
A 21-year-old young female patient came with a history of primary amenorrhea and swelling in both inguinal regions with a married life of 2 years.
Her siblings had normal puberty (Fig. 1).
Fig. 1.
Bilateral inguinal swelling
On examination, she was 152 cm in height and 52 kg in weight with a BMI of 23 kg/m2. Her vitals were within the normal limit. On local examination, there was sparse axillary and pubic hair. The breast development was normal (Tanner grade IV) (Fig. 2).
Fig. 2.

Normal development of breast
On per abdominal examination, two swellings at the level of the external inguinal ring approximately 4.4 × 2.5 cm were seen. Testes were present in the inguinal canal. The introitus was normal (Fig. 3).
Fig. 3.

Palpable inguinal testes
On local examination, a normal vaginal opening was present, the lower 1/3rd of the vagina was approximately 4 cm in length, and a blind pouch was seen.
On per rectal examination, the uterus was absent, no other palpable mass was felt, and both fornices were free. Routine blood investigations were normal. The karyotyping report revealed a normal male karyotype (46XY). On buccal smear, barr bodies were present. High resolution USG with 7.5 MHz transducer at the level of the right inguinal ring revealed oval isoechoic to hypoechoic structures indicative of testes. Anechoic cystic structures were seen adjacent to the superior aspect indicative of an epididymal cyst (Fig. 4).
Fig. 4.

USG showing Right inguinal testes with epididymal cyst
CT Scan
Bilateral masses were present in the pre-pubic fat with bilateral epididymal cysts with a morphology resembling that of the testes (Fig. 5).
Fig. 5.
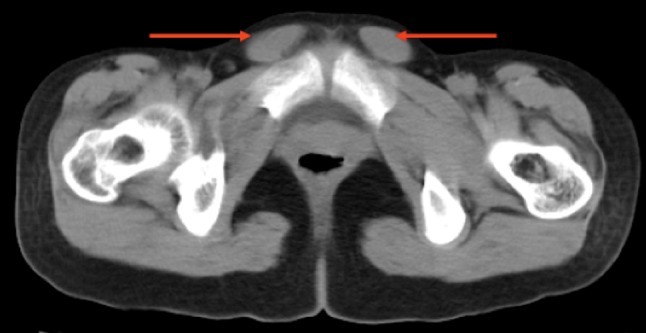
CT revels Bil. Testes with epididymal cyst
Bilaterial orchidectomy was done. The sac was dissected till the internal inguinal ring and then the testes were clamped and excised. The postoperative period was uneventful (Figs. 6, 7).
Fig. 6.

Intra operative photograph showing testes
Fig. 7.

Testes with epididymis
A specimen was sent for histopathologic examination. HPE of the excised gonads showed seminiferous tubules with a thickened basement membrane lined predominantly by Sertoli cells. Occasional germ cells were seen. The interstitium was unremarkable, with no evidence of intratubular germ cell neoplasia or malignancy. She is on regular follow-ups and is doing well (Fig. 8).
Fig. 8.

Bil. testes removed
Discussion
Androgen insensitivity syndrome, also referred to as androgen resistance syndrome, is a set of disorders of sexual differentiation caused by mutations of the gene encoding the androgen receptor [1]. This alteration in the gene blocks the body’s response to masculinizing hormones (androgen) during fetal development and after birth. It makes the body insensitive to androgen, and masculine development that would occur in the presence of a normal gene is impossible. The incidence of complete AIS is about in 1 in 20,000.
The body can respond to feminizing hormones (estrogen), but not androgen. Mullerian insensitivity function (MIF) is a condition which inhibits the complete development of the uterus, cervix, fallopian tubes, ovaries, and the upper 2/3rd of the vagina.
The most common causes of AIS are point mutations in the androgen receptor gene resulting in a defective receptor protein which is unable to bind hormone or bind to DNA [2].
In a fetus with CAIS, androgen does not have the usual masculinizing effect on genital development. The reason is that its body cells lack a special anchoring substance called androgen receptor, and without the androgen receptor [3], the cells cannot respond to androgen, no matter how much is present.
Clinical manifestation are primary amenorrhea, absent pubic and axillary hair, a short vagina, an absent cervix and uterus, and normal breast development. Diagnosis can be made by blood test karyotype, 17-hydroxy-progesterone, testosterone, dihydro-testosterone (DHT), androstenedione, and human chorionic gonadotrophin (HCG). Special investigations include USG, CT scan, and MRI Scan.
Successful management of patients with this condition requires counseling, gonadectomy, vaginal enlargement, estrogen replacement, and genetic counseling. Gonadectomy is usually done after 18 years of age. The advantage of retaining the (usually intra-abdominal) testes until after puberty is that pubertal changes will happen “naturally,” without hormone replacement. This happens because the testosterone produced by the testes gets converted to estrogen in the body tissues (a process known as aromatization).
Retaining the testes has little benefit and may develop benign/malignant change [4]. Once the testes have been removed, estrogen needs to be taken in order to maintain feminity.
The dilemma that this disease causes to the patient and family members is such that unless help is sought and provided well, they may not be able to understand this condition, much less deal with it. Timely and appropriate intervention helped to provide a better lifestyle for this patient.
References
- 1.McPhaul MJ. Androgen receptor mutations and androgen insensitivity. Mol Cell Endocrinol. 2002;198:61–67. doi: 10.1016/S0303-7207(02)00369-6. [DOI] [PubMed] [Google Scholar]
- 2.Nitsche EM, Hiort O. The molecular basis of androgen insensitivity. Horm Res. 2000;54:327–333. doi: 10.1159/000053282. [DOI] [PubMed] [Google Scholar]
- 3.Brinkmann AO. Molecular basis of androgen insensitivity. Mol Cell Endocrinol. 2001;179:105–109. doi: 10.1016/S0303-7207(01)00466-X. [DOI] [PubMed] [Google Scholar]
- 4.Wisniewski AB, Migeon CJ, Meyer-Bahlburg HF, et al. Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome. J Clin Endocrinol Metab. 2000;85:2664–2669. doi: 10.1210/jc.85.8.2664. [DOI] [PubMed] [Google Scholar]


