A slightly increasing trend was found in CT use from 1996 to 2004–2005, and a relatively unchanged or slightly declining trend was seen for CT of different body regions since 2005.
Abstract
Purpose:
To evaluate the 15-year trend in the use of computed tomography (CT) in hospitalized pediatric trauma patients admitted to Harborview Medical Center (HMC) from 1996 to 2010.
Materials and Methods:
This Health Insurance Portability and Accountability Act–compliant retrospective study was approved by the institutional review board. The requirement for informed consent was waived. The HMC trauma registry was linked to the billing department data, and patient and injury-related characteristics were extracted, in addition to type and frequency of CT procedures. Patients discharged from the emergency department and patients hospitalized for less than 24 hours were not included in this study. Patients were classified into three categories according to age: 0–14 years, 15–18 years, and 19–54 years (reference group). Multivariate negative binomial regression was used to compare CT usage among different age groups by adjusting for patient sex, race and/or ethnicity, insurance status, mechanism of injury, injury severity, final disposition (dead vs alive), and year of admission. The trend for CT use in children and teenagers was also evaluated.
Results:
A total of 64 425 trauma patients 0–54 years of age were admitted during the study period. Compared with CT usage in adults 19–54 years old, usage in children up to 15 years of age was significantly lower for spine (incidence rate ratio [IRR], 0.89; 95% confidence interval [CI]: 0.85, 0.92), maxillofacial (IRR, 0.89; 95% CI: 0.81, 0.97), and thoracic (IRR, 0.91; 95% CI: 0.84, 0.99) CT. Increased use of head CT was observed in children up to 15 years old (IRR, 1.09; 95% CI: 1.05, 1.13) and 15–18 years old (IRR, 1.08; 95% CI: 1.04, 1.13). From 2008 to 2010, usage rates in children up to 15 years old and 15–18 years old was relatively unchanged or slightly decreased for almost all CT types.
Conclusion:
A decreasing or unchanged trend was observed in CT usage in hospitalized pediatric trauma patients in recent years.
© RSNA, 2013
Introduction
Computed tomography (CT) is the imaging modality of choice for the management of major trauma, mainly because of the short scan time, high quality of images, and availability and relative affordability of this imaging modality (1–7).
Precise anatomic detail and relative ease of acquisition come at a cost. First, advanced imaging technology has been an important driver for the escalating cost of health care (8,9). Second, CT uses ionizing radiation that could potentially be harmful in the long term, especially for children (3,7,10–13).
Driven by the health risks posed by the increasing use of CT, several groups recommended guidelines to curb the overuse of CT in the pediatric population (14–17). Others have implemented successful measures for reducing the dose delivered to patients who undergo CT (18,19). Despite these efforts, multiple studies suggest that the use of CT in the pediatric population has increased in recent years (2,4,5,7,20).
Limited information is available regarding the recent trends in CT use in the pediatric population among hospitalized patients (2,4,7,20). Even fewer studies have gone beyond basic trend analysis and have involved the evaluation of patient-related characteristics that could potentially influence resource usage. Injuries are one of the leading causes of mortality and morbidity among children in the United States (21). As a result, evaluation of the current trend in the use of CT for hospitalized pediatric trauma patients is of special importance from both potential health risk and financial perspectives.
Harborview Medical Center (HMC) is the only level I pediatric and adult trauma center in the northwest of the United States, with more than 5,000 trauma admissions per year. The purpose of this study was to evaluate the 15-year trend in the use of CT in hospitalized pediatric trauma patients admitted to HMC from 1996 to 2010. We hypothesized that there was an overall declining trend in the use of CT for pediatric trauma patients admitted to HMC in recent years. In addition, we hypothesized that the declining trend in usage rates was more significant for children than adults after adjustment for other covariates, such as injury severity, that could potentially influence the usage rate.
Materials and Methods
This Health Insurance Portability and Accountability Act–compliant retrospective study was approved by the local institutional review board. The requirement for informed consent was waived. We linked HMC’s trauma registry to the HMC billing department data (1996–2010). The trauma registry included detailed information regarding patient demographics, mechanism and severity of injury, hospital care, and outcome at the time of discharge. The billing department data included detailed information regarding all resources that were used for each patient during hospitalization, including type and frequency of each imaging modality used. From the trauma registry, we extracted the following information: patient age and sex, race and/or ethnicity, insurance status, mechanism of injury, injury severity score, length of hospitalization, admission to the intensive care unit, final disposition (dead vs alive), and year of admission.
We focused on CT usage in the following body regions as the main outcomes of interest: head, spine, abdomen, pelvis, thorax, and maxillofacial region.
We plotted the mean number of body region–specific CT examinations per patient during hospitalization against the year of admission for the age groups 0–14 years, 15–18 years, and 19–54 years to describe the crude CT usage rates over the study period. Some prior multicenter study findings had suggested that resource usage and patient outcome for trauma patients 55 years and older were different from those for the younger patients (22). As a result, we deferred discussion about CT use for trauma patients 55 years and older to a separate analysis.
Statistical Analysis
The number of CT examinations performed for each trauma patient did not follow a normal or curved distribution. In other words, a substantial proportion of patients did not undergo any CT or underwent just one CT examination, while a minority underwent multiple CT examinations. This skewness in the distribution of CT examinations required the use of a special technique for multivariate analysis (23). Negative binomial regression is one of the most commonly used approaches for dealing with skewed data (23). We used negative binomial regression to evaluate the association between age group and CT usage in different body regions. All analyses were adjusted for the following covariates, which were a priori identified as potential confounding variables: year of admission, patient sex, race and/or ethnicity (white, black, Asian, other), insurance status (no insurance, Medicaid, Medicare, other), mechanism of injury (traffic related, fall, other), injury severity score (continuous), length of hospitalization (continuous), admission to the intensive care unit (yes or no), and final disposition (dead vs alive). We considered adults 19–54 years of age as the baseline for comparisons. The results are reported as incidence rate ratios (IRRs) with corresponding 95% CIs.
To evaluate the 15-year (1996–2010) trend in the use of CT within each age group, we performed multiple negative binomial regression analyses (one for each CT examination per body region), adjusted for the same covariates. For these trend analyses, we compared the annual usage of CT for each body region with the usage rate in 2000 (baseline for comparisons). All analyses were conducted by using statistical software (Stata, version 11.0; StataCorp, College Station, Tex). The level of significance was determined with a two-sided P value of less than .05.
Results
A total of 81 245 trauma patients were hospitalized at HMC during the study period. Of these, 64 425 (79%) were younger than 55 years and were included in our analyses. Most were aged 19–54 years (77%), with patients 0–14 years of age and 15–18 years of age accounting for 14% and 9% of the population, respectively. The distributions of demographic and injury-related characteristics of the patients are summarized in Table 1. With increasing age, an increase in the proportion of male patients, white patients, and uninsured individuals was observed. Length of stay and death rate tended to increase with age. The percentage of patients 0–14 years of age with an injury severity score from 0 to 8 was substantially higher (52%) than that in patients 15–18 years of age (37%). Further, the proportion of patients with the highest injury severity scores was lower in the younger patients (23%) than in adolescents (33%) and older patients (28%). There were no substantial changes in the distributions of demographic or injury characteristics for any of the age groups during the course of the study period.
Table 1.
Demographic and Injury-related Characteristics for Trauma Patients at HMC from 1996 to 2010
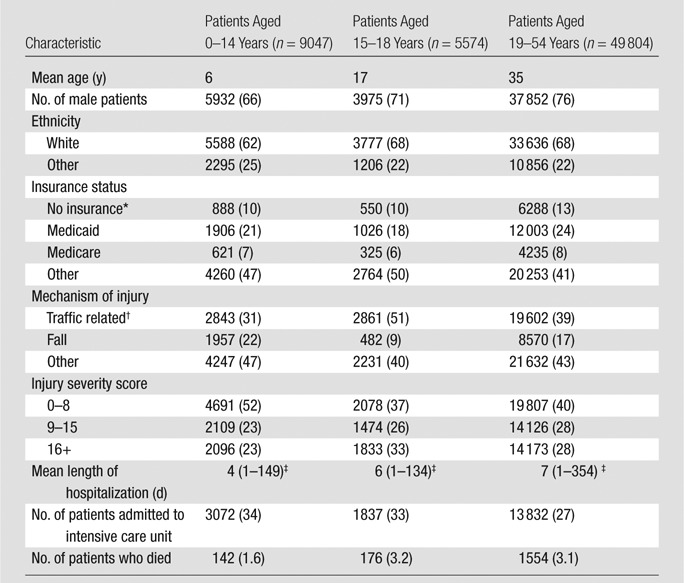
Note.—Data are numbers of patients, with percentages in parentheses except when indicated otherwise. Percentages may not add up to 100% because of missing data.
Includes cases of no insurance, self-pay, and charity.
Includes motor vehicle collisions, as well as motorcycle, bicycle, and pedestrian injuries.
Data are number of days, with range in parentheses.
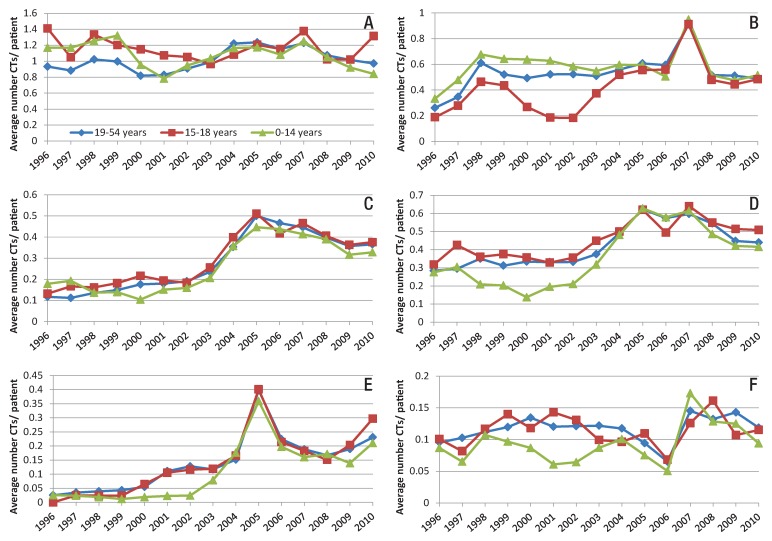
Figure 1 depicts the mean number of CT examinations per body region per patient during the study period. The use of head and maxillofacial CT either decreased slightly or remained relatively constant. Spine, abdominal, pelvic, and thoracic CT use increased over the study period for all age groups.
Figure 1:
Line graphs show the mean number of CT examinations conducted per patient per year for each age category at HMC from 1996 to 2010 by body region imaged, including A, head; B, spine; C, abdomen; D, pelvis; E, thorax; and F, maxillofacial region.
Table 2 summarizes the results of multiple negative binomial analyses. Overall, usage rates in children 14 years and younger were significantly lower for spine, maxillofacial, and thoracic CT compared with those in adults 19–54 years of age. Head CT was slightly more common in children 14 years and younger than in patients 19–54 years old (IRR, 1.09; 95% CI: 1.05, 1.13) after adjustment for other covariates.
Table 2.
Results of Negative Binomial Analyses for CT Use in Different Body Regions
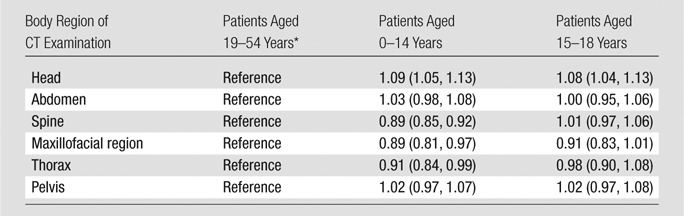
Note.—Data are adjusted IRRs, with 95% CIs in parentheses. Each line represents a separate negative binomial regression. Analyses were adjusted for patient sex, race and/or ethnicity, insurance status, mechanism of injury, injury severity score, final disposition (dead vs alive), and year of admission.
Data in the 19–54-year-old category served as the basis for reference.
Usage rates in patients aged 15–18 years were similar for abdominal, spine, maxillofacial, thoracic, and pelvic CT examinations compared with those in adults 19–54 years of age. As in the group of children up to 15 years old, head CT was slightly more common in patients 15–18 years old than in those 19–54 years old (IRR, 1.08; 95% CI: 1.04, 1.13).
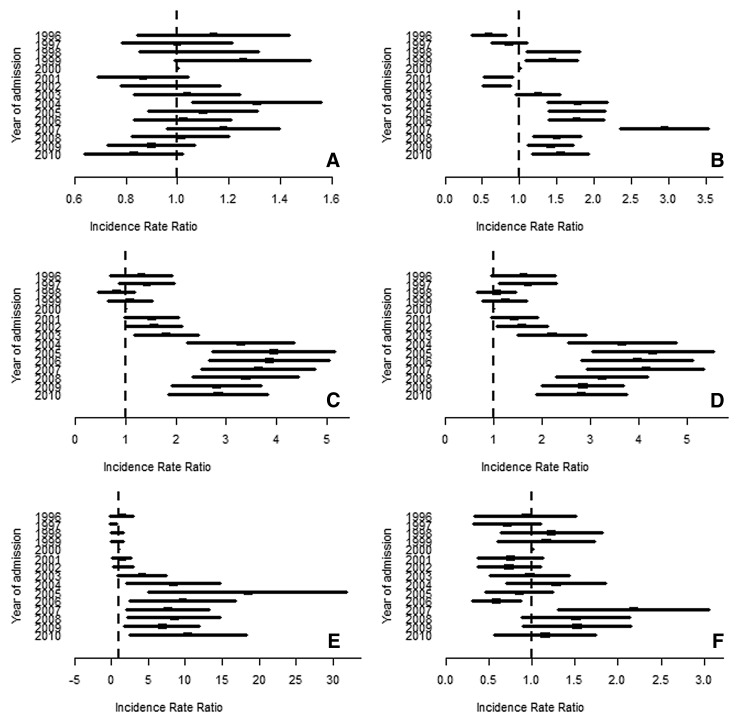
The change in IRR for the CT examinations performed most commonly in children 0–14 years old during the study period, considering data for the year 2000 as the baseline for comparison, is summarized in Figure 2. In children 0–14 years of age, the usage rate for head CT increased slightly from 2000 to 2004 and decreased gradually, reaching its lowest point in 2010 (IRR in 2010, 0.84; 95% CI: 0.67, 1.06). Pelvic CT had its peak usage rate in 2005 (IRR, 4.30; 95% CI: 3.21, 5.75) and decreased gradually until 2010, although the usage rate in 2010 was still higher than that in 2000 (IRR, 2.82; 95% CI: 2.03, 3.92). Abdominal CT had relatively the same pattern as that of pelvic CT. The rate of spine and thoracic CT use was higher between 2004 and 2010, compared with that in 2000, but remained relatively unchanged during the past 5 years. The high IRR and wide CIs for thoracic CT use are most likely due to the small sample number of CT examinations in this age group.
Figure 2:
Point graphs show the results of negative binomial analyses conducted to evaluate the trend in CT use over the study period (2000 is the baseline for comparison) for CT examinations performed in each body region in children 0–14 years old. Analyses were adjusted for patient sex, race and/or ethnicity, insurance status, mechanism of injury, injury severity score, final disposition (dead vs alive), and year of admission. Body regions imaged included A, head; B, spine; C, abdomen; D, pelvis; E, thorax; and F, maxillofacial region.
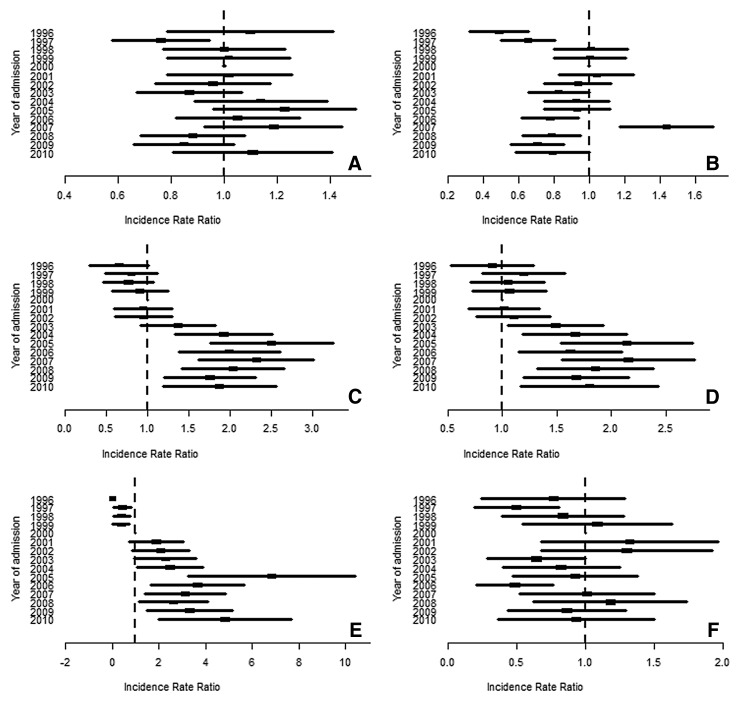
Figure 3 demonstrates that for children 15–18 years of age, the use of head and maxillofacial CT did not change materially during the study period. Spine CT use was slightly less in more recent years when compared with that in 2000, although the difference in usage rate between 2010 and 2000 was not significant (P = .468). Pelvic and abdominal CT use increased gradually to reach a peak in 2004–2005 and has remained relatively unchanged since then. The use of thoracic CT reached its peak in 2005 (IRR, 6.8; 95% CI: 3.1, 10.7). While the change in usage has not been significant since 2006, as compared with 2000, thoracic CT use was significantly higher in 2010 (IRR, 4.8; 95% CI: 1.9, 7.8).
Figure 3:
Point graphs show the results of negative binomial analyses conducted to evaluate the trend in CT use over the study period (2000 is the baseline for comparison) for CT examinations performed in each body region in children 15–18 years of age. Analyses were adjusted for patient sex, race and/or ethnicity, insurance status, mechanism of injury, injury severity score, final disposition (dead vs alive), and year of admission. Body regions imaged included A, head; B, spine; C, abdomen; D, pelvis; E, thorax; and F, maxillofacial.
Discussion
We found that even though there was a slight increasing trend in the use of abdominal, pelvic, and thoracic CT in children 18 years and younger between 1996 and 2004–2005, the usage pattern has been relatively unchanged or declining between 2005 and 2010. In addition, the use of head CT remained relatively unchanged during the study period. These findings are in contrast to those of most recent studies, which have demonstrated escalating trends in the use of CT in different healthcare settings.
The results of our previous analyses in at Parkland Hospital, a level I trauma center in Dallas, Texas, demonstrated that between 1996 and 2006, CT usage in teenagers treated in an adult level I trauma center had the same escalating pattern for most body regions as that in adults (7). In the present study, we have added to our prior study by focusing on the trend over a similar time period, including data from more recent years (2006–2010) in the complete pediatric population treated at our level I adult and pediatric trauma center.
Townsend et al (24) conducted a nationwide survey of pediatric hospitals. They reported a steady decline in CT use at these hospitals from 2003 to 2007; however, the underlying cause of ordering CT was not addressed. Using National Hospital Ambulatory Medical Care Survey data, Korley et al (25) demonstrated a significantly increasing trend in the use of CT and magnetic resonance (MR) imaging in children aged 3–18 years admitted to emergency departments for injuries from 1998 to 2007. More important, they focused only on the trend in the odds of receiving a procedure (not frequency of use) in their analyses and did not adjust their estimates for patient and injury characteristics that could affect CT usage. By using the same data, Kocher and colleagues (26) reported a 330% increase in the use of CT in emergency department visits from 1998 to 2007. Such an increase was not observed in our study.
Broder and colleagues (4) reviewed emergency department data from a children’s hospital and reported a significant increase in the use of head (23%), chest (435%), and abdominal CT (49%) between 2000 and 2006 for children up to 18 years of age. In contrast to our findings that this age group was not significantly associated with CT use, Broder et al (4) found a more rapid increase in CT usage for children 13–17 years of age, when compared with other age groups.
Blackwell et al (2) used National Hospital Ambulatory Care Survey data (1995–2003) to evaluate the national trend in the use of CT for trauma patients. The authors concluded that overall CT use had increased significantly for all age groups, especially for patients 10–18 years old. However, those investigators did not differentiate between specific types of CT procedures. Second, the authors focused only on the use versus lack of use of CT, and the frequency of CT use was not taken into consideration. Third, no adjustment for injury- and patient-related characteristics was performed.
Mannix and colleagues (27) recently compared the use of cervical spine CT between adult and pediatric trauma centers and reported a higher usage rate in the former. The utility and importance of CT in trauma patients cannot be understated (2,28,29). However, optimal use of these resources is the ultimate goal of all ongoing campaigns, guidelines, and protocols. Imaging technology often influences outcomes through a change in the physician’s decision-making process. As a result, evaluation of the direct influence of CT or MR imaging on a patient’s outcome is challenging. Conducting multicenter studies that allow the comparison of resource usage and patient outcome among different settings could be a useful initial approach for evaluation of the association between usage rate and patient outcome.
Although differences in practice could partially explain some of the observed differences in CT use between our study and others in the published literature, the following major differences in research methodology should not be overlooked. First, in spite of most previous studies that have addressed CT use regardless of the reason for hospital admission or visit to the emergency department, we focused only on trauma patients who were hospitalized. Second, the target population in our study constituted more seriously injured patients admitted at a level I trauma center.
Our study has some limitations. First, we focused on patients admitted to one level I trauma center. This restricts the generalizability of our findings, because patients treated and released from the emergency department were not included in our study. Second, available information did not allow us to evaluate the appropriateness of the imaging performed.
In conclusion, most recent studies have demonstrated an escalating trend in the use of CT for the pediatric population. However, we found a slightly increasing trend in CT use from 1996 to 2004–2005 and a relatively unchanged or slightly declining trend in the use of CT in different body regions since 2005.
Advances in Knowledge.
• In children 0–14 years old, the adjusted usage rate for head CT increased slightly from 2000 to 2004 and decreased gradually to reach its lowest point in 2010 (incidence rate ratio [IRR] to compare rates in 2010 and 2000, 0.84; 95% confidence interval [CI]: 0.67, 1.06).
• Pelvic CT had its peak usage rate in 2005 (IRR to compare with 2000 rate, 4.30; 95% CI: 3.21, 5.75) and decreased gradually until 2010 (IRR to compare 2010 rate with that of 2000, 2.82; 95% CI: 2.03, 3.92); abdominal CT had relatively the same pattern as pelvic CT.
• In children 15–18 years old, the adjusted usage rate for head CT for the years 2001–2010 was not significantly different from the usage rate in 2000 (P > .05).
• The adjusted IRR for spine CT was significantly lower in 1996 (P < .001) and 1997 (P = .001) than that in 2000.
• The use of abdominal, pelvic, and thoracic CT increased gradually between 1996 and 2004 and decreased gradually afterward.
Implication for Patient Care.
• A stable or declining trend in the use of CT in more recent years has not been associated with a higher mortality rate among hospitalized pediatric trauma patients in our trauma center.
Disclosures of Conflicts of Interest: B.S.R. No relevant conflicts of interest to disclose. K.J.P. No relevant conflicts of interest to disclose. M.S.V. No relevant conflicts of interest to disclose. C.D.M. No relevant conflicts of interest to disclose. J.G.J. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: Author was a member of the CER Board for GE Healthcare and is a consultant for HealthHelp, a radiology benefits management company. Other relationships: none to disclose.
Received April 18, 2012; revision requested June 4; revision received October 10; accepted November 1; final version accepted November 13.
Funding: This research was supported by the National Institutes of Health (grant R01-AA017497).
Abbreviations:
- CI
- confidence interval
- HMC
- Harborview Medical Center
- IRR
- incidence rate ratio
References
- 1.American College of Radiology ACR Appropriateness Criteria: Head Trauma 2008. http://acsearch.acr.org/VariantList.aspx?topicid=69145. Accessed January 1, 2010
- 2.Blackwell CD, Gorelick M, Holmes JF, Bandyopadhyay S, Kuppermann N. Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med 2007;49(3):320–324 [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007;357(22):2277–2284 [DOI] [PubMed] [Google Scholar]
- 4.Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department, 2000-2006. Emerg Radiol 2007;14(4):227–232 [DOI] [PubMed] [Google Scholar]
- 5.Larson DB, Johnson LW, Schnell BM, Goske MJ, Salisbury SR, Forman HP. Rising use of CT in child visits to the emergency department in the United States, 1995–2008. Radiology 2011;259(3):793–801 [DOI] [PubMed] [Google Scholar]
- 6.Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP. National trends in CT use in the emergency department: 1995–2007. Radiology 2011;258(1):164–173 [DOI] [PubMed] [Google Scholar]
- 7.Roudsari B, Moore DS, Jarvik JG. Trend in the utilization of CT for adolescents admitted to an adult level I trauma center. J Am Coll Radiol 2010;7(10):796–801 [DOI] [PubMed] [Google Scholar]
- 8.Beinfeld MT, Gazelle GS. Diagnostic imaging costs: are they driving up the costs of hospital care? Radiology 2005;235(3):934–939 [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T. High and rising health care costs. Part 2: technologic innovation. Ann Intern Med 2005;142(11):932–937 [DOI] [PubMed] [Google Scholar]
- 10.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176(2):289–296 [DOI] [PubMed] [Google Scholar]
- 11.Mueller DL, Hatab M, Al-Senan R, et al. Pediatric radiation exposure during the initial evaluation for blunt trauma. J Trauma 2011;70(3):724–731 [DOI] [PubMed] [Google Scholar]
- 12.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 2009;169(22):2078–2086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 2009;251(1):175–184 [DOI] [PubMed] [Google Scholar]
- 14.Broder JS. CT utilization: the emergency department perspective. Pediatr Radiol 2008;38(Suppl 4):S664–S669 [DOI] [PubMed] [Google Scholar]
- 15.Goske MJ, Applegate KE, Boylan J, et al. The Image Gently campaign: working together to change practice. AJR Am J Roentgenol 2008;190(2):273–274 [DOI] [PubMed] [Google Scholar]
- 16.Macias CG, Sahouria JJ. The appropriate use of CT: quality improvement and clinical decision-making in pediatric emergency medicine. Pediatr Radiol 2011;41(Suppl 2):498–504 [DOI] [PubMed] [Google Scholar]
- 17.Maguire JL, Boutis K, Uleryk EM, Laupacis A, Parkin PC. Should a head-injured child receive a head CT scan? A systematic review of clinical prediction rules. Pediatrics 2009;124(1):e145–e154 [DOI] [PubMed] [Google Scholar]
- 18.Donnelly LF. Reducing radiation dose associated with pediatric CT by decreasing unnecessary examinations. AJR Am J Roentgenol 2005;184(2):655–657 [DOI] [PubMed] [Google Scholar]
- 19.Singh S, Kalra MK, Moore MA, et al. Dose reduction and compliance with pediatric CT protocols adapted to patient size, clinical indication, and number of prior studies. Radiology 2009;252(1):200–208 [DOI] [PubMed] [Google Scholar]
- 20.Fenton SJ, Hansen KW, Meyers RL, et al. CT scan and the pediatric trauma patient—are we overdoing it? J Pediatr Surg 2004;39(12):1877–1881 [DOI] [PubMed] [Google Scholar]
- 21.National Center for Injury Prevention and Control Injury fact book 2001-2002. Atlanta, Ga: Centers for Disease Control and Prevention, 2001 [Google Scholar]
- 22.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 2006;354(4):366–378 [DOI] [PubMed] [Google Scholar]
- 23.Roudsari B, Mack C, Jarvik JG. Methodologic challenges in the analysis of count data in radiology health services research. J Am Coll Radiol 2011;8(8):575–582 [DOI] [PubMed] [Google Scholar]
- 24.Townsend BA, Callahan MJ, Zurakowski D, Taylor GA. Has pediatric CT at children’s hospitals reached its peak? AJR Am J Roentgenol 2010;194(5):1194–1196 [DOI] [PubMed] [Google Scholar]
- 25.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA 2010;304(13):1465–1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Ann Emerg Med 2011;58(5):452–462, e3 [DOI] [PubMed] [Google Scholar]
- 27.Mannix R, Nigrovic LE, Schutzman SA, et al. Factors associated with the use of cervical spine computed tomography imaging in pediatric trauma patients. Acad Emerg Med 2011;18(9):905–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 2005;58(5):902–905 [DOI] [PubMed] [Google Scholar]
- 29.Markel TA, Kumar R, Koontz NA, Scherer LR, Applegate KE. The utility of computed tomography as a screening tool for the evaluation of pediatric blunt chest trauma. J Trauma 2009;67(1):23–28 [DOI] [PubMed] [Google Scholar]