Abstract
Objectives
There is limited evidence of the impact of advance care planning (ACP) on outcomes. We conducted a retrospective cohort study on deaths of all patients known to a hospice in a 2.5-year period to see if use of ACP affected actual place of death, hospital use and cost of hospital care in the last year.
Results
969 patients were included. 550 (57%) people completed ACP. 414 (75%) achieved their choice of place of death. For those who chose home, 34 (11.3%) died in hospital; a care home 2 (1.7%) died in hospital; a hospice 14 (11.2%) died in hospital and 6 (86%) who chose to die in hospital did so. 112 (26.5%) of people without ACP died in hospital. Mean number of days in hospital in the last year of life was 18.1 in the ACP group and 26.5 in the non-ACP group(p<0.001). Mean cost of hospital treatment during the last year of life for those who died in hospital was £11,299, those dying outside of hospital £7,730 (p<0.001). Mean number of emergency admissions for those who died in hospital was 2.2 and who died elsewhere was 1.7 (p<0.001).
Conclusions
ACP can be used routinely in a hospice setting. Those who used ACP spent less time in hospital in their last year. ACP is associated with a reduction in the number of days in hospital in the last year of life with less hospital costs, supporting the assumptions made in the End of Life Care Strategy 2008.
Keywords: Hospice care, Cancer, Chronic conditions, Communication, Service evaluation
Introduction
Advance care planning (ACP) is a fundamental part of the End of Life Care Strategy published by the Department of Health in 2008.1 However, the empirical evidence of the benefits of ACP is limited. An exploratory study of the acceptability of the use of ACP conducted by Jones et al2 concluded that patients with advanced cancer found that discussions were acceptable and possible. A study by Munday et al3 observed that both general practitioners and nurses found ACP discussions difficult, particularly if they were not initiated by the patient. Empirical studies, whether prospective or retrospective, assessing the impact of ACP on place of death are limited. A systematic review by Gomes and Higginson4 of 58 studies looking at factors which influenced home deaths concluded that patient preference was important. Use of ACP, do not attempt resuscitation orders and the Liverpool Care Pathway for the Dying implemented in nursing homes in Scotland5 showed a reduction in the number of hospital deaths. However, the numbers included in these studies were small. A study of hospice notes by Holdsworth and Fisher6 found that preferred place of death was recorded in 58% of 294 patients, with congruence of preferred place of death and actual place of death being 52% for home, 86% for hospice and 50% for care home. Congruence between preferred and actual place of death varied from 30% to 91% in a review by Bell et al.7 There are no studies that report the impact of ACP on the number of days spent in hospital in the last year of life and the number of admissions to hospital in the last year.
Figure 1.
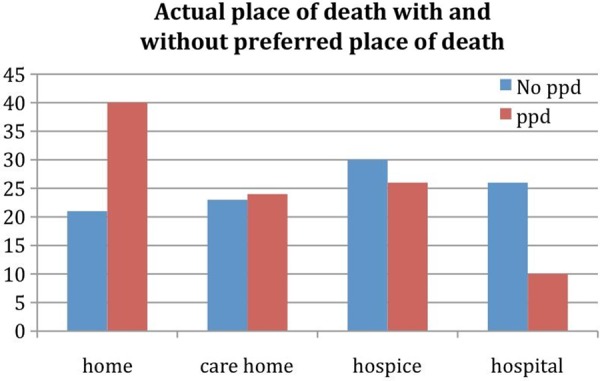
Actual place of death proportion with and without preferred place of death. ppd, preferred place of death.
Figure 2.
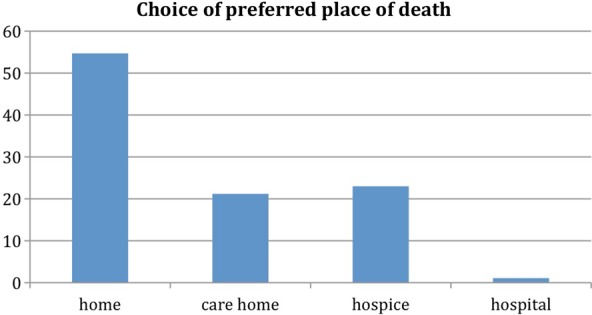
Choice of preferred place of death by proportion (by percentage) of patients completing advance care planning.
We report on the outcome of the use of ACP over a 2.5-year period in a hospice in the south west of England. We conducted a retrospective cohort study of hospice patients. We looked to see if ACP could be a routine part of end of life care. We wanted to see if the use of ACP was associated with difference in place of death, time spent in hospital in the last year of life and cost of hospital care.
Methods
The hospice has a catchment area of about 150 000 and is a mixture of rural countryside and towns. Approximately 700 patients are referred for specialist palliative care each year, which includes inpatient and outpatient services, visits from specialist palliative care community nurses at home and a day care centre. For the last 4 years, the hospice has been using a single document for ACP,8 ‘Planning Ahead’, which combines a modified version of the Preferred Priorities For Care document with a Putting Affairs In Order guide and an Advance Decision To Refuse Treatment document. ‘The Planning Ahead’ document was developed in response to requests from patients and their families to have a unified document for future care. It is part of the hospice assessment paperwork and is given out to patients and families at an appropriate time. Hospice practice has involved emphasising the use of ACP and ‘Planning Ahead’ has been accepted as the single unifying document across the local health community. The hospice uses an electronic patient record (EPR) for all clinical information, including recording the outcome of ACP discussions and actual place of death.
All the statistics were calculated using Stata 10.1 (Stata Corp 2009) using t tests (two-sided) to compare means. Logistic regression was done with the Logistic command in the Stata statistics package.
Study design
We conducted a retrospective observational cohort study of all patients who were known to the hospice who died between 01 January 2009 and 30 June 2011. All the patients had a life limiting disease and were referred to the hospice for specialist palliative care. The hospice uses an EPR for all clinical notes. Patient preferred place of death, actual place of death and reason for variance are recorded routinely. Use of ACP was defined by data entry in these fields. Although ACP is more complex than this, for the purpose of analysis, we used presence or absence of preferred place of death as a marker of whether ACP discussions had taken place. The hospice community nurses remain in contact with the patient up until death and then with the carers into bereavement. In addition, the hospice nurses inform the hospital team of any admission to hospital of a hospice patient. Likewise, deaths and discharges are passed on to the community by the hospital palliative care team. Each death is discussed at our multidisciplinary meeting, so presence or absence of ACP expressed at any time is reviewed. In addition, each relative receives a contact from our specialist palliative care community nurses to review both death and bereavement. We are therefore confident that, for the cohort of patients in this study, we were able to say whether ACP had taken place or not. Place of death was defined as being in the patient's home, in a care home (either nursing or residential), in the hospice or in hospital (acute general hospital or community hospital). Absence of ACP was defined as the patient not having expressed a preferred place of death. Reason for variance was a free text entry. The Secondary User Services database was used to match patient identifying information to find the number of days in hospital each patient spent in the last year of life. This included both day case and inpatient stays. Day case hospital stays were included as chemotherapy is often given on the oncology day unit. The cost figures were actual costs adjusted for length of stay and complexity of care, as per national agreement.
All patient data used in this study were handled and processed in accordance with National Health Service (NHS) best practice and Caldicott recommendations. Although the Data Protection Act does not specifically apply to deceased patient records, any common law duty was adhered to.
Results
Descriptive characteristics for the cohort are shown in table 1. The initial cohort included 971 deaths. Two were excluded as no actual place of death was recorded. When doing the analyses looking at the impact of ACP on place of death, 969 cases were used. To look at the impact of ACP on number of days in hospital and number of hospital admissions we had a truncated dataset. The following patients were excluded:
217: Non-residents who lived outside of Primary Care Trust catchment area (because admission data were not available)
85: Missing NHS number (link to hospital admissions not possible)
9: Recorded NHS number inconsistent with Cancer Register (SWPHO) and/or Primary Care Mortality Database (ONS)—(unsafe match with hospital admission data)
2: Missing place of death.
The total exclusions were 313 leaving 656 for analysis.
Table 1.
Descriptive characteristics of cohort, comparing cancer and non-cancer diagnoses and presence or absence of ACP
| Female | Male | People | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Count | Mean age | SD | Count | Mean age | SD | Count | Mean age | SD | |
| Cancer | |||||||||
| ACP | 223 | 74.9 | 13.0 | 250 | 75.0 | 11.4 | 473 | 74.9 | 12.2 |
| No ACP | 174 | 73.7 | 12.9 | 192 | 73.8 | 12.0 | 366 | 73.7 | 12.4 |
| Total | 397 | 74.3 | 12.9 | 442 | 74.4 | 11.6 | 839 | 74.4 | 12.3 |
| Non-cancer | |||||||||
| ACP | 36 | 81.8 | 10.1 | 38 | 73.7 | 9.5 | 74 | 77.6 | 10.5 |
| No ACP | 35 | 80.2 | 11.1 | 21 | 80.2 | 9.4 | 56 | 80.2 | 10.4 |
| Total | 71 | 81.0 | 10.5 | 59 | 76.0 | 9.9 | 130 | 78.7 | 10.5 |
| ACP | 259 | 75.8 | 12.8 | 288 | 74.8 | 11.2 | 547 | 75.3 | 12.0 |
| No ACP | 209 | 74.7 | 12.8 | 213 | 74.4 | 11.9 | 422 | 74.6 | 12.3 |
| Grand Total | 468 | 75.4 | 12.8 | 501 | 74.6 | 11.5 | 969 | 75.0 | 12.1 |
ACP, advance care planning.
Main results
There were 501 male subjects, average age 75.4, and 468 female subjects, average age 74.6. The mean age was 75 (range 27–105) years at date of death. A total of 839 (87%) patients had a cancer diagnosis and 130 (13%) a non-cancer diagnosis. Of the 969 patients, 309 (32%) died at home, 265 (27%) died in the hospice, 227 (23%) died in a care home and 168 (17%) died in hospital. In all, 549 (56%) of patients completed ACP, 422 (44%) did not. During the first 6 months of the study period, 42% of patients completed ACP. During the last 6 months, this had increased to 69%. This figure had steadily increased, when looked at in 6-month periods. The mean number of days between completion of ACP and death was 86 (range 0–555 days) with 40% of people having done ACP within 100 days before dying and 75% within 364 days. Overall, 55% of female subjects completed ACP and 57% of male subjects. Mean age of female subjects completing ACP was 75.8 years and non-ACP was 74.7 years. Mean age of male subjects who completed ACP was 74.8 years and non-ACP was 74.4 years. Impact of ACP on place of death is shown in figure 1.
The overall percentage hospital death rate for patients who had completed ACP was 11% (table 2) Choice of preferred place of death is shown in figure 2. Table 3 compares choices for cancer and non cancer diagnoses. For those without ACP, this was 26%; p value<0.001.
Table 2.
Proportion of patients achieving their preferred place of death and percentage hospital deaths
| Number | Achieved preferred place of death | Percentage | Number who died in hospital | Percentage who died in hospital | |
|---|---|---|---|---|---|
| Care home | 115 | 110 | 96 | 2 | 2 |
| Home | 302 | 204 | 68 | 34 | 11 |
| Hospice | 125 | 93 | 74 | 21 | 17 |
| Hospital | 7 | 6 | 86 | 6 | 86 |
| Overall | 549 | 413 | 75 | 63 | 11 |
In all, 50 (10%) of the cancer patients who did ACP died in hospital and 94 (26%) of the cancer patients without ACP died in hospital; p value<0.001.
Overall, 88% of people who had completed ACP had at least one emergency admission in the last year of life and 91% of people who had not done ACP had at least one emergency admission; p value 0.71.
For people who died in hospital, the mean number of days spent in hospital in the last year was 26.5 days. For people who did not die in hospital, the mean number of days in hospital in the last year was 20.5 days. The mean cost of hospital care in the last year of life for those who died in hospital was £11 298. The mean cost of hospital care for those who died outside of hospital was £7730, with a difference of £3569; p value of <0.001 (table 4).
Table 4.
Death in hospital compared with death elsewhere (95% CI)
| People | Mean stay | Mean number of admissions, all people | Mean number of emergency admissions, all people | Mean cost of all admissions, all people (£) | |
|---|---|---|---|---|---|
| Death in hospital | 108 | 26.5 (20.8 to 32.2) | 6.4 (4.9 to 7.9) | 2.2 (1.9 to 2.5) | 11 299 (9161 to 13 436) |
| Death elsewhere | 556 | 20.6 (18.5 to 22.7) | 4.7 (4.3 to 5.4) | 1.6 (1.4 to 1.7) | 7730 (7079 to 8381) |
| Total | 664 | 21.5 (19.6 to 23.5) | 5.1 (4.5 to 5.6) | 1.7 (1.5 to 1.8) | 8310 (7659 to 8962) |
| t Test two-sided p value | 0.03 | 0.03 | <0.001 | <0.001 |
The p value for the difference in the number of days in hospital for cancer patients (20.2 days) compared with non-cancer (30.6 days) was <0.001 (table 5).
Table 5.
Impact of ACP on mean number of days in hospital in the last year of life, number of admissions and costs of emergency admissions in the last year of life (95%CI)
| People | Mean stay for all those with an admission | Mean stay for those with or without an admission | Mean number of admissions | Mean number of emergency admissions | Mean cost of emergency admissions (£) | |
|---|---|---|---|---|---|---|
| ACP | 389 | 20.7 (18.4 to 23.0) | 18.1 (16.0 to 20.2) | 4.8 (4.2 to 5.4) | 1.61 (1.4 to 1.8) | 5260.4 (4586 to 5934) |
| No ACP | 275 | 28.9 (25.1 to 32.8) | 26.4 (22.8 to 30.0) | 5.5 (4.5 to 6.4) | 1.75 (1.6 to 1.9) | 5690.9 (4984 to 6398) |
| Total | 664 | 24.2 (22.0 to 26.3) | 21.5 (19.6 to 23.5) | 5.1 (4.5 to 5.6) | 1.66 (1.5 to 1.8) | 5438.8 (4948 to 5929) |
| t Test two-sided p value | <0.001 | <0.001 | 0.2 | 0.3 | 0.4 |
p Value compares ACP with non-ACP.
Multivariate analysis investigating factors affecting the likelihood of death in hospital suggests that ACP is a significant factor. People who have had ACP reduce the odds of dying in hospital nearly 70% lower than people who do not. Gender, age or cause of death did not have a significant effect.
ACP, advance care planning.
Discussion
This study shows that it is possible to make ACP a routine part of care for hospice patients. During the first 6 months of the study period, 42% of patients had completed ACP. This had increased to 69% during the final 6 months and in the subsequent 6 months following the study had further increased to 77%. ACP has been seen as an integral part of the work of the whole hospice and effort has been made to make its use part of normal care. The proportional impact of ACP on place of death remained constant throughout the study. The use of an EPR has meant that it has been possible to monitor the use of ACP and the impact on place of death on a monthly basis. The use of the EPR has made data collection and analysis a lot more straightforward. The monthly audit of the EPR has meant that data completeness has been very high, with only two of 971 records not having place of death recorded.
The use of ACP was correlated with a significant impact on place of death, with 75% of patients dying in their place of choice. Hospital death rates for people who had completed ACP were 11%. Without ACP this was 26%. This latter figure is still low in comparison with national averages, where the hospital death rate for England is 54%.9 This is likely to reflect in part the impact of specialist palliative care on place of death. Hospices have historically done well enabling patients to stay out of hospital even without ACP. The use of ACP helps further over and above the impact of specialist palliative care alone.
In our study, this approach appears to be justified in both the cancer and non-cancer settings. Specialist palliative care has become increasingly involved in non-cancer terminal illnesses. In all, 59% of the non-cancer patients used ACP. The overall hospital death rate in this group was 18%. It seems unlikely that the non-cancer group was representative of non-cancer terminal diagnoses in the population, as the numbers were relatively small. The majority of patients with non-cancer terminal diagnoses do not receive specialist palliative care. The referred group will have had particular needs that required the use of hospice services. Nevertheless, the results suggest that use of ACP is applicable in the non-cancer setting and this has a significant impact on place of death. What was notable was that none of the non-cancer patients chose to die in hospital.
Gomes and colleagues conducted an extensive study using telephone interviews to ask the general population about their preferences of place of death.10 In this study, depending on region, more than 60% of people would chose to die at home (range 60%–67%), 26%–32% would chose to die in a hospice, and the remaining would chose to die in a care home, hospital or elsewhere. In our study, which had 87% cancer patients, 55% chose to die at home, 23% chose the hospice, 21% chose a care home and 1% chose hospital. These latter figures are for patients who have a terminal illness and are making a decision about where they would like to die. Although there are some similarities in these figures, the differences are likely to be due to a combination of the reality of having a terminal illness as well as our study population all being known to the hospice.
The hospital death rate for cardiovascular cause of death for any mention on the death certificate for England is 60.5% and for respiratory disease is 67.6%.11 These results suggest that the more widespread use of ACP in the non-cancer setting could result in a shift of deaths from hospital into the community. In this study, only a small percentage of non-cancer patients chose to die in the hospice. It is hard to know if this result is generalisable. It has meant that the hospice has not been overwhelmed by large numbers of non-cancer patients wanting to die on the inpatient unit.
The mean number of days spent in hospital in the last year of life for those patients who had completed ACP was 8.3 days less than those who had not. The overall cost of hospital admissions in the last year was £3569 less for those people who died outside of hospital. Both of these figures had highly significant p values. It seems likely that this figure is an underestimate of changes that would result in ACP being used more widely. The hospital death rate in the non-ACP group was 26%. The hospice is effective at reducing hospital death rates even when ACP has not been done. The national average is 54%.
The mean number of admissions in the last year was 5.4 in the ACP group and 6.1 in the non-ACP group. This latter figure did not have a significant p value. The mean number of emergency admissions in the group of people who died in hospital was significantly higher than those who died outside of hospital, although the total number of admissions in ACP verses non-ACP group was not significant. This may indicate that the final admission was an emergency one and could potentially be avoided.
A previous paper in our locality12 showed the mean cost of the final admission to be £3093 in 2006. The mean difference in costs in the last year of life is larger than this figure and suggests that potential reinvestment and savings opportunities exist based on the results from this study. Estimation of hospital costs is complicated by whether or not there was a difference in the use of chemotherapy in the ACP group compared with the non-ACP group. Similar numbers of hospital admissions, including day case, suggest that both ACP and non-ACP patients had similar amounts of chemotherapy. The oncology and palliative care services in our locality work closely together and shared care of patients is common as their disease progresses. This may indicate that decision making about the use of chemotherapy has already been optimised to reflect end of life care. Irrespective of ACP, death in hospital increased significantly the number of days spent in hospital in the last year of life, with increased mean costs of £11 299 compared with £7730 for death outside of hospital.
The impact of the use of ACP on length of life is unknown. A study of lung cancer in the USA13 showed that those who accessed specialist palliative care lived longer and used less chemotherapy than those who did not. Chemotherapy use in the UK may well be different from that in the USA. The mean cost of admissions in the last year of life was £8310. This is slightly higher than the study published by Bardsley and coworkers,14 in which the mean hospital inpatient cost in the last year of life in the three sites studied was £6231, when taking into account day case costs. The number of days spent in hospital in the last year in the same study was 30 days, which differs considerably from our result of 21.5 days. These differences are likely to reflect that the current study was mainly of cancer patients.
Although the number of patients in this study was large in comparison with previous studies, the use of a retrospective cohort design means that we were able to look at associations rather than elucidate causative relationships. A prospective randomised study is needed to be able to determine the relationships of ACP use, place of death and cost with more certainty. The study was able to demonstrate associations among use of ACP, reduced total days spent in hospital in the last year and reduced hospital costs for those people who died outside of hospital.
Use of ACP is an integral part of the End of Life Care Strategy.1 If we are going to offer choices about place of death to people with terminal diagnoses, we need to be able to identify them and have the discussion around ACP with sufficient time. In all, 75% of patients who did ACP stated their wishes within the last year of life, with a mean value of expressing preferred place of death 86 days before dying. This means that hospice staff manage to identify and complete ACP discussions on average 3 months before people die. Prediction of prognosis is notoriously difficult. It may be that the advent of ACP discussions is a marker for terminal decline.
Table 3.
Proportion of choices for preferred place of death for cancer and non-cancer patients
| PPD | Cancer % (numbers) | Non-cancer % (numbers) |
|---|---|---|
| Home | 53 (253) | 67 (49) |
| Care home | 20 (97) | 27 (20) |
| Hospice | 26 (123) | 6 (4) |
| Hospital | 1 (7) | 0 |
A total of 8 (11%) patients with a non-cancer diagnosis who had completed ACP died in hospital. Of those who did not complete ACP, 16 (29%) died in hospital (p value 0.14).
ACP, advance care planning; PPD, preferred place of death.
Conclusions
The assumptions made in the End of Life Care Strategy 2008 that more people when asked would choose to die outside of hospital, and that it is possible to look after people successfully in their place of choice, are strengthened by the results from this paper, particularly for patients with cancer. It remains to be seen as to whether the same principles are applicable in the non-cancer setting. The routine use of ACP has yet to be proven, particularly as the bulk of these discussions would need to be done by generalists in palliative care.
Acknowledgments
Clare-Louise Nicholls and Anne Sumerhill from North Somerset PCT helped with data collection for days in hospital and costs.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Open Access: This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
References
- 1.End of Life Care Strategy Promoting high quality care for all adults at the end of life. London: Department of Health, 2008 [Google Scholar]
- 2.Jones L, Harrington J, Barlow CA, et al. Advance care planning in advanced cancer: can it be achieved? An exploratory randomized patient preference trial of a care planning discussion. Palliat Support Care 2011;9:3–13 [DOI] [PubMed] [Google Scholar]
- 3.Munday D, Petrova M, Dale J. Exploring preferences for place of death with terminally ill patients: qualitative study of experiences of general practitioners and community nurses in England. BMJ 2009;339:b2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomes B, Higginson I. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006;332:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hockley J, Watson J, Oxenham D, et al. The integrated implementation of two end-of-life care tools in nursing care homes in the UK: an in-depth evaluation. Palliat Med 2010;24:828–38 [DOI] [PubMed] [Google Scholar]
- 6.Holdsworth L, Fisher S. A retrospective analysis of preferred and actual place of death for hospice patients. Int J Palliat Nurs 2010;16:424. [DOI] [PubMed] [Google Scholar]
- 7.Bell CL, Somogyi-Zalud E, Masaki KH. Factors associated with congruence between preferred and actual place of death. J Pain Symptom Manage 2010;39:591–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Planning Ahead. http://www.westonhospicecaregroup.org.uk/wp-content/uploads/2012/04/AdvancePlanning-3logos-18-11-10.pdf (accessed 8 Jun 12)
- 9. http://www.endoflifecare-intelligence.org.uk/profiles/2/Place_of_Death/atlas.html (accessed 8 Jun 2012)
- 10.Gomes B, Calanzani N, Higginson I. Local preferences and place of death in regions within England 2010. Cicely Saunders International, 2011 [Google Scholar]
- 11. http://www.endoflifecare-intelligence.org.uk/profiles/2/Place_Cause_of_Death/atlas.html (accessed 8 Jun 2012)
- 12.Abel J, Rich A, Griffin T, et al. End-of-life care in hospital: a descriptive study of all inpatient deaths in 1 year. Palliative Medicine 2009;00:1–7 [DOI] [PubMed] [Google Scholar]
- 13.Temel j, Greer J, Muzikansky A, et al. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N Engl J Med 2010;363:733–42 [DOI] [PubMed] [Google Scholar]
- 14.Bardsley M, Georghiou T, Dixon J. Social care and hospital use at the end of life. http://www.nuffieldtrust.org.uk/sites/files/nuffield/social_care_and_hospital_use-full_report_081210.pdf (accessed 13 Apr 2012).


