Abstract
Background
Mutations in the ryanodine receptor type 1 gene (RYR1) that encodes the skeletal muscle-specific intracellular calcium (Ca2+) release channel are a cause of malignant hyperthermia (MH). In this study we examined RYR1 mutations in a large number of North American MH-susceptible (MHS) subjects without prior genetic diagnosis.
Methods
RYR1 was examined in 120 unrelated MHS subjects from the United States in a tiered manner. The alpha-1 subunit of the dihydropyridine receptor gene (CACNA1S) was screened for four variants in subjects in whom no abnormality was found in 100 or more exons of RYR1.
Results
Ten known causative MH mutations were found in 26 subjects. Variants of uncertain significance in RYR1 were found in 36 subjects, 16 of which are novel. Novel variants in both RYR1 and CACNA1S were found in the one subject who died of MH. Two RYR1 variants were found in 4 subjects. Variants of uncertain significance were found outside and inside the hotspots of RYR1. Maximal contractures in the caffeine-halothane contracture test were greater in those who had a known MH mutation or variant of uncertain significance in RYR1 than in those who did not.
Conclusions
The identification of novel RYR1 variants and previously observed RYR1 variants of uncertain significance in independent MHS families is necessary for demonstrating the significance of these variants for MH susceptibility and supports the need for functional studies of these variants. Continued reporting of the clinical phenotypes of MH is necessary for interpretation of genetic findings, especially because the pathogenicity of most of these genetic variants associated with MHS remains to be elucidated.
Introduction
Dominant mutations in the ryanodine receptor type 1 gene (RYR1) encoding the skeletal muscle-specific intracellular calcium (Ca2+) release channel are a cause of malignant hyperthermia (MH) and central core disease (CCD). RYR1 variants associated with MH have been found in 50% to 86% of MH-susceptible (MHS) families depending on population of origin and study design.1–7 Recessive mutations in RYR1 are found in patients with congenital myopathies including nemaline myopathy, centronuclear myopathy and congenital fiber type disproportion.8 Most of the subjects of these reports live in Europe or Japan. Differences in the frequency of some RYR1 mutations causative for MH1–4 and different variants of uncertain significance (VUS)1, 3–5, 7 have been observed in different populations. The aim of the present study was to analyze RYR1 in a large number of MHS subjects from the United States without prior genetic diagnosis. The overall goal of this project was to determine the heterogeneity of variants and mutations in RYR1 in the MHS population of the United States. Such a compendium of variants is important for the genetic diagnosis of MHS and will help in differentiating RYR1 variants that could be causative for MH from rare nonsynonymous polymorphisms.
Methods
Population
Subject entry criteria included personal history of positive caffeine-halothane contracture test (CHCT), or in cases without CHCT results, personal anesthetic history of an MH event as judged by the MH Diagnostic Center Director at the Uniformed Services University of the Health Sciences (USUHS) (S.M.M.) or the Director of the North American MH Registry (B.W.B.), or a family history that included presumed death from MH and/or a positive CHCT in a family member. Subjects with histologic diagnosis of CCD were accepted into this study without CHCT results. Subjects were actively consented through the North American Malignant Hyperthermia Registry and the MH Diagnostic Center at the USUHS. Subjects in whom no genetic variants had been found in previous studies at USUHS3, 9–10 were included in the present study. These subjects had previously been recruited from several MH diagnostic centers in the United States. In addition, 12 anonymized specimens were obtained from one MH diagnostic center that was no longer active (Northwestern University). This study was approved by the IRB at the University of Pittsburgh, Northwestern University and USUHS.
Clinical information, including the personal and family histories of the subjects, was variably obtained from the subjects themselves, data from the North American Malignant Hyperthermia Registry, and records from the MH biopsy center directors. Acute MH episodes were described by the raw score of the Clinical Grading Scale (CGS)11 when clinical details were available. CHCTs were performed and interpreted according to the criteria established by the North American Malignant Hyperthermia Group.12 Individuals were diagnosed MHS if any one or more of the three muscle exposures produced a contracture exceeding the diagnostic threshold. The threshold values for a positive test were ≥ 0.7 g contracture in the presence of 3% halothane and/or ≥ 0.3 g contracture in the presence of 2 mM caffeine. The contracture with the greatest tension in each subject is reported in this study. Only one muscle strip per subject was reported in this study. CCD was diagnosed by muscle histology performed by a staff neuropathologist at the Armed Forces Institute of Pathology. The diagnosis of CCD was based on histochemical identification of amorphous areas (cores) that lack mitochondria and oxidative enzyme activity in type 1 muscle fibers.13
RYR1 screening
Genetic analysis was performed in a tiered manner. Initially 30 exons in the three mutational hotspots of RYR1 were screened for variants. Subsequently 50, 70, 100 exons or the entire RYR1 coding region was examined as material resources allowed. In 17 of the subjects, 100 or more exons of RYR1 were examined. Sequencing of RYR1 was performed as described previously.3 In brief, cDNA was synthesized using RNA extracted from the frozen muscle biopsy samples, and then amplified in 26 overlapping fragments. In the absence of muscle samples, exons were amplified using genomic DNA extracted from peripheral blood and intronic primers designed for each exon. The RYR1 variants were determined by direct sequencing using an ABI 3100 DNA analyzer (Applied Biosystems, Foster City, CA). The newly identified RYR1 variants were compared with the single nucleotide polymorphism database at the National Center for Biotechnology Information.a The variants of 2 subjects were identified by microarray technology using a Goldengate platform with VeraCode technology (Illumina, Inc., San Diego, CA) as previously described.14 The frequency of novel RYR1 variants identified in this study was determined in healthy unrelated population controls using restriction enzyme or DNA sequencing analysis as described previously.3 Controls were 100 Caucasian individuals, 50 of whom were MH negative by CHCT. The others were healthy individuals from unrelated families enrolled into a genetic study for screening of a familial MH mutation in RYR1.
Screening of other genes
In subjects in whom no abnormalities were found in 100 or more exons of RYR1, the alpha-1 subunit of the dihydropyridine receptor gene (CACNA1S) was screened for four variants, Arg174Trp in exon 4, Arg1086His and Arg1086Ser in exon 26, and Thr1354Ser in exon 44 using genomic DNA extracted from peripheral blood. Primers specific to these exons were designed; primer sequences are available upon request. Restriction enzyme MspI was used to screen Arg174Trp, and enzyme HhaI was used to screen Arg1086 and Arg1086Ser mutations. The Thr1354Ser was screened using direct sequencing of exon 44 polymerase chain reaction product. In one case of fatal MH, the entire CACNA1S was examined. In one case with histologic diagnosis of McArdle disease (glycogen storage disease type 5) and no findings in RYR1, the most common mutation, Arg50X, in the myophosphorylase gene (PYGM) was screened using NIaIII restriction enzyme analysis followed by sequencing.
A variant was defined as any change to the wild type sequence, other than common polymorphisms previously found in one in 100 control subjects, whether it was found in MHS or control subjects. To be considered a candidate MH causative mutation, the variant must be nonsynonymous (alter the amino acid), be present in MHS subjects only, be absent in at least 100 control subjects, and be absent in all published databases listing RYR1 polymorphisms. The pathogenic MHS mutation should segregate with MHS in 2 unrelated families, and be shown to induce biophysical changes consistent with MHS.b The concomitant presence of nonsynonymous amino acid polymorphisms was not counted as a second or multiple variant in MHS subjects in this study. Mutations and variants identified in the RYR1 were denoted according to Human Genome Variation guidelines for nomenclature.c Variants are numbered by amino acid position according to the RYR1 protein sequence NP_000531.2.
Statistical analysis
Data are summarized using means and standard deviations and point estimates with 95% confidence intervals. Mean values of contractures in groups of subjects with different genetic findings were compared by analysis of variance followed by Student-Newman-Keuls tests using PASW Statistics 18.0.0 (SPSS).
Results
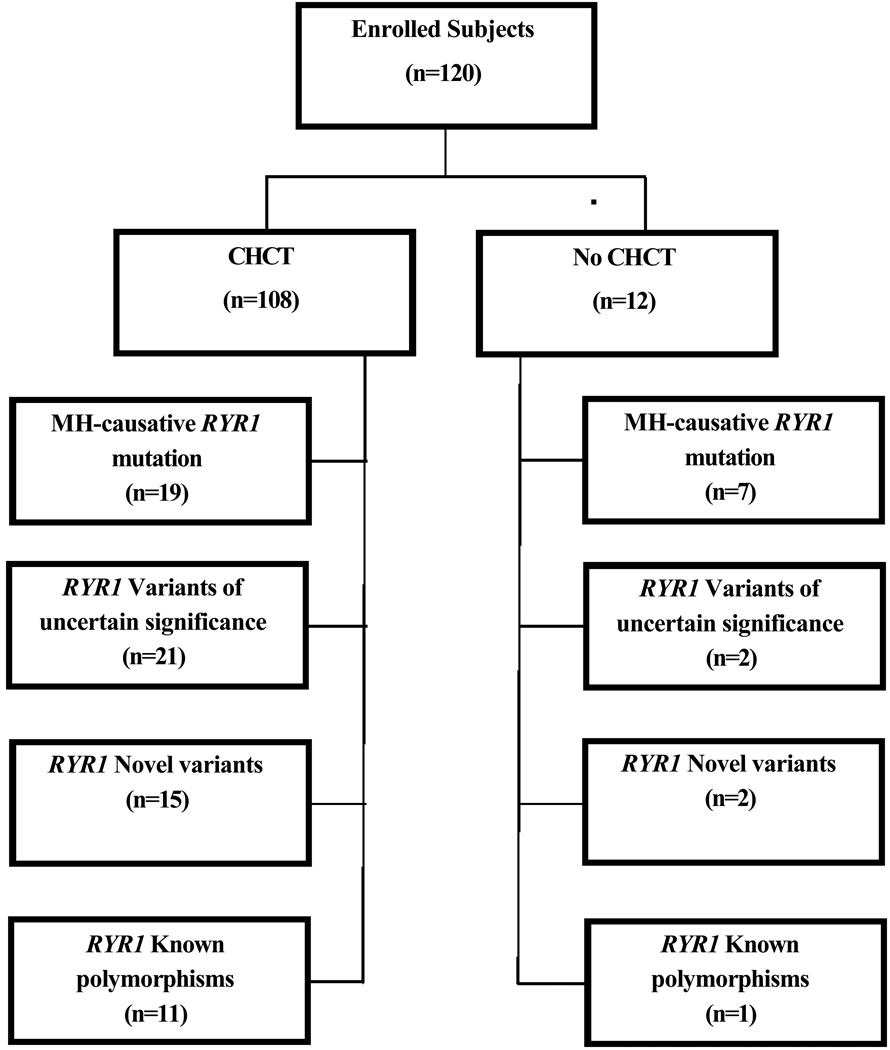
DNA analysis was performed on 120 unrelated subjects (Figure 1) (individual numbered subjects are described in the Web Supplement). CHCT were reported for 108 subjects, one of whom was found to have CCD diagnosed by histopathology (subject #52). In subjects who did not undergo CHCT, CGS scores of their suspected MH episodes, when calculable, ranged from 23 to 76. These seven subjects were numbered 6, 15, 25, 31, 51, 53 and 63 in the Web Supplement. Subject #53 died of MH (CGS 76). Subject #51 had progressive CCD, diagnosed by histopathology, after a severe MH episode during general anesthesia (CGS 53). Subjects #17 and #27 had CCD diagnosed after a suspected MH episode. Two subjects, #8 and #49, had no CHCT results because they underwent muscle contracture tests before standardization of the CHCT, due to their history suggestive of MH susceptibility (Web Supplement), with abnormal results. One subject, #50, had a very strong family history of MH, but was unable to undergo CHCT.
Figure 1.
This flow chart illustrates the outcomes of DNA sequencing for subjects with and without prior caffeine-halothane contracture test (CHCT). A variant of uncertain significance (VUS) is a variant that has been previously reported, but it is not yet proven to be malignant hyperthermia (MH)-causative. A novel variant is a variant that has not been previously reported, and it has not been proven to be MH-causative. A polymorphism is a change in the amino acid sequence of the gene that has been found at least once in 100 normal subjects and is not expected to be pathogenic. The numbers in parentheses are the numbers of subjects found to have this type of change in RYR1.
Two novel variants in the ryanodine receptor type one gene (RYR1) were found in one subject. A novel variant and a VUS in RYR1 were found in one subject. Two different VUS were found in 2 subjects. A VUS and a polymorphism were found in one subject. A novel variant and a polymorphism in RYR1 were found in another subject. One subject had 2 polymorphisms in RYR1. In summary, there were 7 subjects who had 2 different variants when polymorphisms in RYR1 are included in this count. Thus, the sum of the numbers in the sub-boxes is 7 more than the number of subjects in this study reported to have mutations, VUS, novel variants and/or polymorphisms. (see Table 4 and the Web Supplement)
Ryanodine receptor gene findings
Ten known RYR1 mutations causative for MH were identified in 26 subjects (Table 1). A previously reported variant of unknown significance or a novel variant in RYR1 was identified in an additional 36 subjects (Table 2).3–7,15–35 Thus 62 of 120 or 52% (95% CI 43% to 61%) of all the subjects had a causative mutation or other variant in RYR1.
Table 1.
Known Malignant Hyperthermia (MH) Causative Mutations
| Amino Acid Substitution |
Exon | Cases (n) |
|---|---|---|
| Arg163Cys | 6 | 2 |
| Gly248Arg | 9 | 2 |
| Gly341Arg | 11 | 2 |
| Arg614Cys | 17 | 5 |
| Arg2163His | 39 | 1 |
| Val2168Met | 39 | 1 |
| Thr2206Met | 40 | 4 |
| Gly2434Arg | 45 | 7 |
| Arg2454His | 45 | 1 |
| Arg4861His | 101 | 1 |
Known MH-causative mutations were found in 26 subjects, 21% of the total in this study (95% CI 5%–37%).
There is no statistically significant difference in the frequency of these mutations in this sample.
The subject with Val2168Met had central core disease (CCD) diagnosed by histopathology.
The anesthetic details that are available about each of these cases are presented in the Web Supplement.
Table 2.
RYR1 Variants of Uncertain Significance in Malignant Hyperthermia-Susceptible Subjects
|
RYR1 Variants Amino Acid Substitution |
Exon | Caffeine-Halothane Contracture Test (g) |
Inclusion criteria |
Citation | |
|---|---|---|---|---|---|
| Caffeine 2mM | Halothane 3% | ||||
| Leu13Arg | 1 | 0.34 | 2.55 | MH | 4, 5 |
| Gly40Ala | 2 | 0.83 | 2.7 | FH | Current study (16) |
| Leu487Pro | 14 | 2.4 | 3.6 | FH | Current study |
| Val518Ala (a) | 14 | 1.0 | 1.3 | MH | Current study |
| Arg975Trp | 24 | na | na | CCD | Current study |
| Arg1043Cys (d) | 24 | 3.3 | 5.7 | MH, FH | 5, 17 |
| Arg1043His | 24 | 0.95 | 1.8 | FH | Current study (5,17) |
| Arg2248His (b) | 41 | 0.3 | 2.3 | MH | Current study (7) |
| Arg2336His (d) | 43 | 3.3 | 5.7 | MH, FH | 5, 17 |
| Asn2342Ser | 43 | 0.2 | 1.5 | MH | 17 |
| del Glu2347 | 44 | 1.36 | 5.9 | FH | 18 |
| Asn2351His | 44 | 0.5 | 5.0 | MH | Current study |
| Val2354Met | 44 | 1.25 | 3.4 | MH | Current study |
| Arg2355Trp | 44 | 2.6 | 9.5 | MH | 17, 19, 20 |
| Arg2355Trp | 44 | 1.82 | 1.6 | MH | 17, 19, 20 |
| Arg2355Trp | 44 | 0.3 | 5.1 | MH | 17, 19, 20 |
| Ile2358Leu (b) | 44 | 0.3 | 2.3 | MH | Current study |
| Arg2435Leu | 45 | 1.9 | 1.1 | FH | 7, 17, 21–23 |
| Arg2508His | 47 | na | na | MH, CCD | 15, 24 |
| Arg3238Gly | 66 | 0 | 0 | CCD | Current study |
| Arg3283Gln* | 66 | na | na | MH Death | Current study |
| Arg3539His | 71 | 0.8 | 5.2 | MH | 25, 26 |
| Glu3583Gln (c) | 72 | 1.0 | 2.6 | MH, FH | 17 |
| Thr3711Arg | 76 | 0.85 | 7.5 | FH | Current study |
| Tyr3933Cys (a) | 86 | 1.0 | 1.3 | MH | 7, 27 |
| Trp3985Arg | 87 | 1.2 | 2.2 | MH | 28 |
| Asp3986Glu | 87 | 1.9 | 8.8 | MH | 17 |
| Asp3986Glu | 87 | 2.5 | 10.8 | MH | 17 |
| Gly4178Val | 90 | 1.77 | 6.95 | FH | Current study |
| Met4230Arg | 91 | 3.3** | 6.3** | MH, FH | Current study |
| Gln4837Glu | 100 | 0.5 | 9.9 | FH | Current study |
| Val4847Leu | 101 | na | na | MH | 6 |
| Val4849Ile | 101 | 1.9 | 9.8 | MH | 2, 3, 29 |
| Val4849Ile | 101 | 0.3 | 3.6 | FH | 2, 3, 29 |
| Val4849Ile | 101 | 0.9 | 5.0 | MH, FH | 2, 3, 29 |
| Val4849Ile (c) | 101 | 1.0 | 2.6 | MH, FH | 2, 3, 29 |
| Ala4906Gly | 102 | 0.4 | 2.1 | FH | Current study (30) |
| Asp4939Glu | 103 | 2.0 | 11.3 | MH, FH | 31 |
| Ala4940Thr | 103 | 0.84 | 8.42 | FH | 3, 32–34 |
| Pro4973Leu | 104 | 0.85 | 2.1 | 22, 35 | |
na = not done; MH indicates that a personal episode of malignant hyperthermia was reported; FH indicates that a family history of MH was reported; CCD = central core disease; del = deletion.
When no data were available regarding an anonymized subject the cell remains empty. The letters (a), (b), (c) and (d) indicate the variants were both observed in a single subject, (a), (b), (c) and (d) respectively. Therefore there are 36 subjects represented in the 40 rows of this Table. The number appearing in parentheses below "current study" refers to the citation in which a different amino acid variant was reported at the same location. This was the case in 4 subjects in Table 2.
One RYR1 variant and a novel variant in CACNA1S found in this subject.
Caffeine-halothane contracture test (CHCT) was from soleus muscle; the parent had positive CHCT results from deltoid muscle.
Further details that are available regarding these subjects are presented in the Web Supplement.
Eleven of the 16 novel variants reported here were found in one of the three previously defined hotspots of RYR127 in exons 2, 14, 41, 44, 90, 91, 100 and 102, and five were found outside of these hotspots, in exons 24, 66, and 76. Four novel variants were at amino acid residues, Gly40 in exon 2, Arg1043 in exon 24, Arg2248 in exon 41 and Ala4906 in exon 102, where different variants had been previously reported.5, 7, 16, 17, 30 These novel variants were not present in any of the 100 control subjects.
Contracture test results are described in Table 3. There were no significant differences between the maximum contractures in subjects with MH causative mutations and subjects with VUS in RYR1. The maximum number of contractures in subjects with MH mutations or VUS in RYR1 were significantly more than the maximum number of contractures in those with no abnormality, which includes polymorphisms, found in RYR1.
Table 3.
Caffeine-Halothane Contractures are greater in Malignant Hyperthermia-Susceptible Subjects with RYR1 MH Mutations and Variants than in those with no abnormalities found in RYR1
| Genetic Result | N | CHCT (g) | ||
|---|---|---|---|---|
| Caffeine 2 mM | Halothane 3% | |||
| Group 1 | Known causative malignant hyperthermia mutations | 19 | 1.3 (0.8) | 5.6 (2.2) |
| Group 2 | VUS in RYR1 | 32 | 1.3 (0.9) | 4.9 (3.2) |
| Group 3 | Known polymorphisms in RYR1 | 8 | 0.6 (0.5) | 2.5 (1.9) |
| Group 4 | No variants in 100 or more exons of RYR1* | 17 | 0.6 (0.5) | 1.7 (0.7) |
| Group 5 | No variants in RYR1 after screening 70 or fewer exons* | 32 | 0.6 (0.7) | 2.2 (1.4) |
| ANOVA for difference among groups | P < 0.001 | P < 0.001 | ||
Data are mean (standard deviation).
VUS is variant of uncertain significance.
A polymorphism is a DNA change that is commonly observed and has not been associated with disease.
There was no significant difference between Groups 1 and 2 in either caffeine or halothane contracture tests. There were no significant differences between Groups 3, 4 and 5 in caffeine or halothane contracture tests. (Student-Newman-Keuls test). There was a significant difference between Groups 1 and 2 and Groups 3, 4 and 5, P < 0.001.
In 4 subjects in whom 100 or more exons were screened a previously reported polymorphism was in RYR1 was found. In 3 subjects in whom 70 or fewer exons were screened a known polymorphism in RYR1 was found, thus the numbers reported in this table differ slightly from those in the text. When both a polymorphism and a variant of uncertain significance were found, the contracture results of that subject were included in Group 2.
CHCT = Caffeine-halothane contracture test.
Known MH-causative RYR1 mutations were found in 7 of the 12 subjects (#6, 8, 15, 27, 31, 49 and 50 in the Web Supplement) who had not undergone CHCT. Previously reported VUS in RYR1 were found in 2 other subjects in this group (#51 and 63), one of whom also had histologically diagnosed CCD. Novel variants in RYR1 were found in 2 subjects (#17 and 53), one of whom was the anesthetic-induced fatality and the other had CCD with no history of MH. Only one of these 12 subjects (#25) who had not undergone CHCT had no findings in the 106 exons of RYR1 other than a known polymorphism. This subject experienced a MH event with CGS 38 (very likely MH). Clinical details of these cases are described further in the Web Supplement.
RYR1 was not examined to the same extent in all 58 subjects (one of whom did not undergo CHCT) in whom no variants were found because of the limited availability of DNA. However, there was no significant difference in maximum contractures between groups with more or fewer exons examined (Table 3).
Previously described polymorphisms (variants that are not expected to be pathologic that are found in at least 1 in 100 normal subjects) in RYR1 were found in 9 of these 58 subjects and in 2 subjects who had RYR1 VUS and 1 who had a novel RYR1 variant. Contracture test results for 8 of these 9 subjects are summarized in Table 3. The observed polymorphisms included Val974Met, Arg1109Leu, and Ile2321Val (each in one subject), Lys1393Arg, Pro1787Leu and Gly2060Cys (each in 3 subjects). In one subject both Pro1787Leu and Gly2060Cys were found. The clinical details of these subjects are presented in the Web Supplement.
RYR1 compound heterozygotes and variants in CACNA1S and PYGM
Two variants, novel or previously observed VUS in RYR1, were found in 4 of the 120 subjects (Table 4 and the Web Supplement). This count does not include polymorphisms. One subject listed in Table 4 was not included in Table 2, or in the total count of subjects in this study, because this subject had an MH episode after which a sibling underwent CHCT. Both siblings were entered into this study before it was recognized that they were related. The proband in this family had a known RYR1 mutation causative for MH and a novel variant. The sibling of this proband, who had strongly positive results on the contracture test (Table 2), had only the novel variant in RYR1. In the subject who died of MH, a novel variant, Val875Met, was found in exon 20 of CACNA1S in addition to a novel RYR1 variant, Arg3283Gln.
Table 4.
Individuals with Two Genetic Variants
| RYR1 | RYR1 |
CACNA1 S |
CHCT (g) | Clinical History | |
|---|---|---|---|---|---|
| Amino Acid Substitution | Caffeine 2mM | Halothane 3% | |||
| Arg2248Gln | Ile2358Leu | — | 0.3 | 2.3 | MH episode CGS 15 |
| Glu3583Gln | Val4849Ile | — | 1.0 | 2.6 | MH episode CGS 18, sibling was reported to have died of MH |
| Arg614Cys | Thr3711Arg | — | na | na | MH episode, no details available muscle cramps & rhabdomyolysis after exercise sibling had positive CHCT |
| Arg3283Gln | — | Val875Met | na | na | MH death, CGS 76 |
| Val518Ala | Tyr3933Cys | — | 1.0 | 1.3 | possible MH episode with postop rhabdomyolysis CGS 5 * |
| Arg1043Cys | Arg2336His | — | 3.3 | 5.7 | MH episode CGS 18, FH possible MH death, sibling had positive CHCT |
Of 120 subjects, 4 were found to have 2 variants in RYR1 that could be associated with MH and one had a variant in both RYR1 and CACNA1S. The compound heterozygote with R614C and T3711R was found in a subject, who after study entry was found to be related to the subject with only the novel T3711R finding. Therefore this compound heterozygote was not included in the count of total cases in Tables 1 or 2, but it was included here.
Indicates the subject described in McKenney KA, Holman SJ. Delayed postoperative rhabdomyolysis in a patient subsequently diagnosed as malignant hyperthermia susceptible. Anesthesiology 2002; 96:764–5. For more clinical details see Web Supplement.
CHCT = caffeine-halothane contracture test; na = not available; MH = malignant hyperthermia; CGS = Clinical Grading Scale; FH = Family History.
In the 17 subjects in whom no variants were found in more than 100 exons of RYR1, the CACNA1S was examined for four variants. None of the four CACNA1S variants associated with MHS in previous studies was found. Two of the 17 subjects reported that a first-degree relative died during anesthesia and 1 who reported that a more distant relative died during anesthesia. In contrast, in the families of 18 different subjects in whom RYR1 variants were found (8 causative MH mutations and 10 VUS), 13 subjects reported perioperative deaths in first-degree relatives and 5 reported perioperative deaths in more distant relatives. Unfortunately, the records documenting the cause of death were not available in most of these cases. It is certainly possible that the cause of death was not MH. Nevertheless these unexpected deaths motivated family members to undergo CHCT. The clinical data available for these cases are presented in the Web Supplement.
A homozygous Arg50X mutation was found in PYGM in one subject who had repeated episodes of muscle weakness and pain after exercise. His basal creatine kinase was 3000 to 6000 IU. After moderate exercise creatine kinase increased to >100,000 IU. He had never had anesthesia, but a second-degree relative was reported to have had anesthetic complications; therefore, CHCT was performed. The maximum contracture was 0.28 g in the presence of 2 mM caffeine and 2.68 g in the presence of 3% halothane. Examination of the entire RYR1 gene did not identify a variant. An additional muscle biopsy was performed and McArdle disease was diagnosed histologically.
Clinical history of subjects in whom no RYR1 variants or polymorphisms and none of 4 CACNA1S variants were found
All 49 of these subjects had CHCT results (Web Supplement). In this group, 17 underwent CHCT because of a family history of an MH event. In 3 families between 3 and 5 positive CHCTs per family unit were documented. In one of these 3 families there was a perioperative death. In another family there was a perioperative cardiac arrest with death and subsequently positive CHCT in a first-degree relative who is a subject in this study. The clinical presentation of the 7 subjects who were reported to have had a MH event, with no family history of MH, in whom no RYR1 or CACNA1S variants were observed, included masseter muscle rigidity in 2 and 1 with CGS of 38 (very likely MH).11 Another had a CGS of 18 and the rest had CGS of 15 or less. Rhabdomyolysis without more evidence for MH was the indication for CHCT in 3 subjects. There was no documented indication for CHCT in 22 of the subjects in whom there were no genetic findings. There were no deaths attributed to MH in the 49 subjects in whom no genetic variants were found in RYR1 or CACNA1S or in the 9 subjects in whom only a polymorphism in RYR1 was observed.
Discussion
In this sample of 120 subjects with the diagnosis of MHS, we found 10 MH causative mutations, 16 novel RYR1 variants, one novel CACNA1S variant and 18 previously reported VUS in RYR1. A 2005 study of 30 subjects from North America, using direct sequencing of the entire coding region of RYR1,3 found 7 previously reported known MH mutations in 10 subjects, 2 VUS in 2 subjects, and 9 novel RYR1 variants in 9 other subjects. Seven of these previously observed mutations and variants were also found in this study of 120 subjects, but none of the 9 novel variants reported in 2005 was observed again. Gly2423Arg was the most frequent MH mutation reported in 2001, 2005 and in the current study. This mutation was also the most frequently observed MH mutation in Great Britain36 and Canada,6 but not in France,2 Japan,4 Australia,27 Switzerland,5 or Italy.7 Numerous cohort and case studies have reported RYR1 variants in subjects with clinical evidence of MH, including positive contracture tests. When these reports were comprehensively reviewed by Robinson et al. in 2006, 178 missense RYR1 variants were identified.17 As of November 2012, 414 unique variants in RYR1 had been reported in the Leiden Open Variation Database.d This report adds more RYR1 variants to this list. Thus, the number of described RYR1 variants is increasing rapidly, but the number proven to meet the strict criteria of a causative mutation is an order of magnitude lower.
Previous studies reported a high percentage of RYR1 variants thought to be unique or private to one family. This report supports the reassignment of variants from the private to the recurrent category. In 8 subjects in this study a variant of uncertain significance was found that had been published only once before.6, 17, 18, 28, 31 Other VUS observed in this study have been reported at least twice previously, but not yet widely accepted as MH-causative mutations.4, 5, 7, 17, 19, 20–27, 30, 32–35 Thus, this report provides data to support the potential MH-causative nature of many VUS in RYR1. Many variants listed in Table 2 have been observed previously in association with MHS, but the functional tests needed to prove that these variants cause the MH syndrome have not yet been performed.
The novel variants and VUS in RYR1 documented in this study support the need for examination of the entire RYR1 gene in MHS patients when searching for the genetic marker of this condition. Nine of the VUS observed in this study were outside of the RYR1 hotspots as these were defined.27 Fatal episodes of MH, MH death in a sibling, CCD, positive CHCT results and observation of the same variant in other studies4 were reported in these nine subjects.
In contrast to earlier claims that RYR1 variants associated with CCD are found in the C terminal exons 85–103,17 we observed RYR1 variants in exons 24, 47 and 66 in subjects with CCD. The same variant in exon 47 was observed in Japanese subjects with MH and CCD.4 The other 2 are novel RYR1 variants.
The subjects in this report who underwent CHCT were evaluated by anesthesiologists at one of several MH diagnostic centers. Review of personal medical and anesthetic history and family history are part of these evaluations. These anesthesiologists may consult with a neurologist before proceeding with CHCT so that maximum diagnostic use can be made of the patient’s muscle biopsy. Not all patients who present for CHCT are accepted for this procedure. If there is not a high prior probability of MH being present, the CHCT is not warranted.37
Individuals who had not undergone CHCT were subject to similar scrutiny before entry into this study. The high yield of RYR1 findings in this subset without a personal history of CHCT is likely due to the rigor of that review. Review of medical records before testing an individual for MHS includes detailed review of the anesthetic record, including minute ventilation and exhaled gas concentrations. These details can be clearly provided by the electronic anesthetic record.38 Other clinical and laboratory data should also be part of this assessment.39 Often, however, medical records, especially paper records, are incomplete. Additionally, because anesthesia providers should intervene to treat MH before it becomes fulminant, severe hypercarbia and rhabdomyolysis are averted. Thus, in many cases a CGS associated with “very likely MH” (CGS of 35 to 49) or “almost certain MH,” (CGS of 50 or more),11 will not be observed. This was the case in the cohort reported here.
The observation of subjects with 2 variants is consistent with the previous claim that the frequency of an MH-causative genetic variant may be as much as 1 in 2,000 to 3,000 people in the general population.4,35
The percentage of subjects in this study in whom variants in RYR1 were identified is less than in several previously published studies. This is likely due in part to our inability to examine the entire RYR1 gene in all subjects due to the limited amount of genetic material available from MH diagnostic centers that have closed. Nevertheless it is of interest that in those subjects in whom 100 or more RYR1 exons were examined without identification of any variant, the average maximum contractures were less than in the groups in which either known MH-causative mutations or VUS were found in the RYR1 gene. Because of the high sensitivity and low specificity of the CHCT there can be false positive CHCT results in as many as 22% of those tested.40 Therefore the personal anesthetic and medical histories and family histories have to be re-examined in order to diagnose the underlying condition. It may be that the low specificity of the CHCT produces clinically positive results in individuals who are not really at increased risk of experiencing MH. For example, the subject who was homozygous for a mutation causing McArdle disease had a maximum caffeine contracture less than 0.3 g, but was enlisted in this study because he had a maximum halothane contracture of more than 2 g and suspicion of an adverse anesthetic event in a relative. The medical history of the individual should guide testing so that the differential diagnosis of exercise-induced rhabdomyolysis, the chief complaint of this individual, includes more than RYR1 variants.
CHCT may have positive results, diagnostic of MHS, in myopathic conditions with elevated calcium in muscle that do not include genetic abnormalities of RYR1. Appropriately focused blood testing could provide a diagnosis without performing muscle biopsy. When muscle biopsy is performed, comprehensive pathologic examination should be carefully planned prospectively to maximize diagnostic yield. If muscle contracture testing is needed to evaluate MHS, the biopsy should be performed at a MH diagnostic center (see www.mhaus.org for a list of active MH diagnostic centers in North America). CHCT remains the only method available in North America to confirm that the diagnosis is not MHS.
Previous work has demonstrated that greater halothane contractures are more likely to be found in individuals with MH-causative mutations in RYR1.41 Yet our subjects without abnormalities in RYR1 had been diagnosed as MHS by the CHCT. They or their first degree relatives experienced adverse anesthetic events. It is necessary to continue to collect detailed anesthetic records, family histories and biologic specimens from such people to discover the genetic factors associated with these adverse events. It may be that a new genetic locus for MH can be identified in subjects with strong family histories of adverse anesthetic events without RYR1 variants. Variants in regulatory regions and deep intronic variants of RYR1, or in areas of CACNA1S not examined in this study, may be responsible for the MHS diagnosis in this group. Given the dispersion of the population and potential difficulty confirming anesthetic details, it is necessary to continue collection of data in a central repository such as the North American MH Registry, so that future studies of this potentially life-threatening syndrome can be supported.
In summary, these results contribute to increasing the utility of genetic testing of MHS by documenting the presence of RYR1 variants in independent families and by describing novel variants. These results are consistent with previous work that identified MH-causative mutations more often in those with greater muscle contractures on in vitro testing.41 Technologic improvements in electronic health records and genetic analysis should lead to a more comprehensive view of both the phenotype and the genetic basis of MHS. Continued detailed reporting of the phenotypes of MHS is necessary to support interpretation of genetic results.
Supplementary Material
Acknowledgments
Funding: Malignant Hyperthermia Association of the United States, Uniformed Services University of the Health Sciences, NIH, Interdisciplinary Research and Creative Activities Award from the University of Buffalo Office of the Vice President for Research, and Dept of Anesthesiology of University of Pittsburgh Medical Center. This research was funded by National Institutes of Health grant number RO1HL085800.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This manuscript was presented, in part, at ASA 2009.
DISCLOSURES:
Name: Barbara W. Brandom, MD
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript
Attestation: Barbara W. Brandom has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the author responsible for archiving the study files
Conflicts of Interest: Barbara W. Brandom received research funding from MHAUS. I have received research support from Malignant Hyperthermia Association of the United States which is a not for profit group. I am the current Director of the North American MH Registry which is a subsidiary of MHAUS.
Name: Saiid Bina, PhD
Contribution: This author helped write the manuscript and with laboratory work
Attestation: Saiid Bina has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Cynthia A. Wong, MD
Contribution: This author helped conduct the study, write the manuscript, and provided subject materials
Attestation: Cynthia A. Wong has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Tarina Wallace, MS
Contribution: This author helped conduct the study and with laboratory work
Attestation: Tarina Wallace has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Mihaela Visoiu, MD
Contribution: This author helped conduct the study and write the manuscript
Attestation: Mihaela Visoiu has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Paul J. Isackson, PhD
Contribution: This author helped with laboratory work
Attestation: Paul J. Isackson has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Georgirene D. Vladutiiu, PhD
Contribution: This author helped with laboratory work
Attestation: Georgirene D. Vladutiiu has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Nyamkhishig Sambuughin, PhD
Contribution: This author helped conduct the study, write the manuscript, and genetic analysis
Attestation: Nyamkhishig Sambuughin has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Sheila M. Muldoon, MD
Contribution: This author helped design the study, conduct the study, and write the manuscript
Attestation: Sheila M. Muldoon has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Recuse Note: Dr. Cynthia Wong is the Section Editor for Obstetric Anesthesiology for the Journal. This manuscript was handled by Dr. Steven L. Shafer, Editor-in-Chief, and Dr. Wong was not involved in any way with the editorial process or decision.
Contributor Information
Barbara W. Brandom, Department of Anesthesiology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania (Current Affiliation: Department of Anesthesiology, North American Malignant Hyperthermia Registry, Pittsburgh, Pennsylvania).
Saiid Bina, Department of Anesthesiology, Uniformed Services University of the Health Sciences, Bethesda, Maryland.
Cynthia A. Wong, Department of Anesthesiology, Northwestern University, Chicago, Illinois.
Tarina Wallace, Department of Anesthesiology, Uniformed Services University of the Health Sciences, Bethesda, Maryland.
Mihaela Visoiu, Children's Hospital, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania.
Paul J. Isackson, Departments of Pediatrics, Neurology, Pathology & Anatomical Sciences, School of Medicine & Biomedical Sciences, State University of New York at Buffalo, Buffalo, New York.
Georgirene D. Vladutiu, Departments of Pediatrics, Neurology, Pathology & Anatomical Sciences, School of Medicine & Biomedical Sciences, State University of New York at Buffalo, Buffalo, New York.
Nyamkhishig Sambuughin, Department of Anesthesiology, Uniformed Services University of the Health Sciences, Bethesda, Maryland.
Sheila M. Muldoon, Department of Anesthesiology, Uniformed Services University of the Health Sciences, Bethesda, Maryland.
References
- 1.Rueffert H, Olthoff D, Deutrich C, Meinecke CD, Froster UG. Mutation screening in the ryanodine receptor 1 gene (RYR1) in patients susceptible to malignant hyperthermia who show definite IVCT results: identification of three novel mutations. Acta Anaesthesiol Scand. 2002;46:692–698. doi: 10.1034/j.1399-6576.2002.460610.x. [DOI] [PubMed] [Google Scholar]
- 2.Monnier N, Kozak-Ribbens G, Krivosic-Horber R, Nivoche Y, Qi D, Kraev N, Loke J, Sharma P, Tegazzin V, Figarella-Branger D, Romero N, Mezin P, Bendahan D, Payen JF, Depret T, Maclennan DH, Lunardi J. Correlations between genotype and pharmacological, histological, functional, and clinical phenotypes in malignant hyperthermia susceptibility. Hum Mutat. 2005;26:413–425. doi: 10.1002/humu.20231. [DOI] [PubMed] [Google Scholar]
- 3.Sambuughin N, Holley H, Muldoon S, Brandom BW, de Bantel AM, Tobin JR, Nelson TE, Goldfarb LG. Screening of the entire ryanodine receptor type 1 coding region for sequence variants associated with malignant hyperthermia susceptibility in the North American population. Anesthesiology. 2005;102:515–521. doi: 10.1097/00000542-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Ibarra MC, Wu S, Murayama K, Minami N, Ichihara Y, Kikuchi H, Noguchi S, Hayashi YK, Ochiai R, Nishino I. Malignant hyperthermia in Japan: mutation screening of the entire ryanodine receptor type 1 gene coding region by direct sequencing. Anesthesiology. 2006;104:1146–1154. doi: 10.1097/00000542-200606000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Levano S, Vukcevic M, Singer M, Matter A, Treves S, Urwyler A, Girard T. Increasing the number of diagnostic mutations in malignant hyperthermia. Hum Mutat. 2009;30:590–598. doi: 10.1002/humu.20878. [DOI] [PubMed] [Google Scholar]
- 6.Kraeva N, Riazi S, Loke J, Frodis W, Crossan ML, Nolan K, Kraev A, Maclennan DH. Ryanodine receptor type 1 gene mutations found in the Canadian malignant hyperthermia population. Can J Anaesth. 2011;58:504–513. doi: 10.1007/s12630-011-9494-6. [DOI] [PubMed] [Google Scholar]
- 7.Tammaro A, Di Martino A, Bracco A, Cozzolino S, Savoia G, Andria B, Cannavo A, Spagnuolo M, Piluso G, Aurino S, Nigro V. Novel missense mutations and unexpected multiple changes of RYR1 gene in 75 malignant hyperthermia families. Clin Genet. 2011;79:438–447. doi: 10.1111/j.1399-0004.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- 8.Jungbluth H, Sewry CA, Muntoni F. Core myopathies. Semin Pediatr Neurol. 2011;18:239–249. doi: 10.1016/j.spen.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Sambuughin N, Sei Y, Gallagher KL, Wyre HW, Madsen D, Nelson TE, Fletcher JE, Rosenberg H, Muldoon SM. North American malignant hyperthermia population: screening of the ryanodine receptor gene and identification of novel mutations. Anesthesiology. 2001;95:594–599. doi: 10.1097/00000542-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Sei Y, Sambuughin NN, Davis EJ, Sachs D, Cuenca PB, Brandom BW, Tautz T, Rosenberg H, Nelson TE, Muldoon SM. Malignant hyperthermia in North America: genetic screening of the three hotspots in the type I ryanodine receptor gene. Anesthesiology. 2004;101:824–830. doi: 10.1097/00000542-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Larach MG, Localio AR, Allen GC, Denborough MA, Ellis FR, Gronert GA, Kaplan RF, Muldoon SM, Nelson TE, Ording H, Rosenberg H, Waud BE, Wedel DJ. A clinical grading scale to predict malignant hyperthermia susceptibility. Anesthesiology. 1994;80:771–779. doi: 10.1097/00000542-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Larach MG. Standardization of the caffeine halothane muscle contracture test. North American Malignant Hyperthermia Group. Anesth Analg. 1989;69:511–515. [PubMed] [Google Scholar]
- 13.Monnier N, Romero NB, Lerale J, Nivoche Y, Qi D, MacLennan DH, Fardeau M, Lunardi J. An autosomal dominant congenital myopathy with cores and rods is associated with a neomutation in the RYR1 gene encoding the skeletal muscle ryanodine receptor. Hum Mol Genet. 2000;9:2599–2608. doi: 10.1093/hmg/9.18.2599. [DOI] [PubMed] [Google Scholar]
- 14.Vladutiu GD, Isackson PJ, Kaufman K, Harley JB, Cobb B, Christopher-Stine L, Wortmann RL. Genetic risk for malignant hyperthermia in non-anesthesia-induced myopathies. Mol Genet Metab. 2011;104:167–173. doi: 10.1016/j.ymgme.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu S, Ibarra MC, Malicdan MC, Murayama K, Ichihara Y, Kikuchi H, Nonaka I, Noguchi S, Hayashi YK, Nishino I. Central core disease is due to RYR1 mutations in more than 90% of patients. Brain. 2006;129:1470–1480. doi: 10.1093/brain/awl077. [DOI] [PubMed] [Google Scholar]
- 16.Jungbluth H, Lillis S, Zhou H, Abbs S, Sewry C, Swash M, Muntoni F. Late-onset axial myopathy with cores due to a novel heterozygous dominant mutation in the skeletal muscle ryanodine receptor (RYR1) gene. Neuromuscul Disord. 2009;19:344–347. doi: 10.1016/j.nmd.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Robinson R, Carpenter D, Shaw MA, Halsall J, Hopkins P. Mutations in RYR1 in malignant hyperthermia and central core disease. Hum Mutat. 2006;27:977–989. doi: 10.1002/humu.20356. [DOI] [PubMed] [Google Scholar]
- 18.Sambuughin N, McWilliams S, de Bantel A, Sivakumar K, Nelson TE. Single-aminoacid deletion in the RYR1 gene, associated with malignant hyperthermia susceptibility and unusual contraction phenotype. Am J Hum Genet. 2001;69:204–208. doi: 10.1086/321270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McWilliams S, Nelson T, Sudo RT, Zapata-Sudo G, Batti M, Sambuughin N. Novel skeletal muscle ryanodine receptor mutation in a large Brazilian family with malignant hyperthermia. Clin Genet. 2002;62:80–83. doi: 10.1034/j.1399-0004.2002.620111.x. [DOI] [PubMed] [Google Scholar]
- 20.Wehner M, Rueffert H, Koenig F, Olthoff D. Functional characterization of malignant hyperthermia-associated RyR1 mutations in exon 44, using the human myotube model. Neuromuscul Disord. 2004;14:429–437. doi: 10.1016/j.nmd.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Barone V, Massa O, Intravaia E, Bracco A, Di Martino A, Tegazzin V, Cozzolino S, Sorrentino V. Mutation screening of the RYR1 gene and identification of two novel mutations in Italian malignant hyperthermia families. J Med Genet. 1999;36:115–118. [PMC free article] [PubMed] [Google Scholar]
- 22.Galli L, Orrico A, Cozzolino S, Pietrini V, Tegazzin V, Sorrentino V. Mutations in the RYR1 gene in Italian patients at risk for malignant hyperthermia: evidence for a cluster of novel mutations in the C-terminal region. Cell Calcium. 2002;32:143–151. doi: 10.1016/s0143-4160(02)00138-0. [DOI] [PubMed] [Google Scholar]
- 23.Tammaro A, Bracco A, Cozzolino S, Esposito M, Di Martino A, Savoia G, Zeuli L, Piluso G, Aurino S, Nigro V. Scanning for mutations of the ryanodine receptor (RYR1) gene by denaturing HPLC: detection of three novel malignant hyperthermia alleles. Clin Chem. 2003;49:761–768. doi: 10.1373/49.5.761. [DOI] [PubMed] [Google Scholar]
- 24.Chan B, Chen SP, Wong WC, Mak CM, Wong S, Chan KY, Chan AY. RYR1-related central core myopathy in a Chinese adolescent boy. Hong Kong Med J. 2011;17:67–70. [PubMed] [Google Scholar]
- 25.Dekomien G, Gencik M, Gencikova A, Klenk Y, Epplen JT. Gene symbol: RYR1. Disease: malignant hyperthermia. Hum Genet. 2005;118:543. [PubMed] [Google Scholar]
- 26.Monnier N, Marty I, Faure J, Castiglioni C, Desnuelle C, Sacconi S, Estournet B, Ferreiro A, Romero N, Laquerriere A, Lazaro L, Martin JJ, Morava E, Rossi A, Van der Kooi A, de Visser M, Verschuuren C, Lunardi J. Null mutations causing depletion of the type 1 ryanodine receptor (RYR1) are commonly associated with recessive structural congenital myopathies with cores. Hum Mutat. 2008;29:670–678. doi: 10.1002/humu.20696. [DOI] [PubMed] [Google Scholar]
- 27.Gillies RL, Bjorksten AR, Davis M, Du Sart D. Identification of genetic mutations in Australian malignant hyperthermia families using sequencing of RYR1 hotspots. Anaesth Intensive Care. 2008;36:391–403. doi: 10.1177/0310057X0803600311. [DOI] [PubMed] [Google Scholar]
- 28.Kaufmann A, Kraft B, Michalek-Sauberer A, Weigl LG. Novel ryanodine receptor mutation that may cause malignant hyperthermia. Anesthesiology. 2008;109:457–464. doi: 10.1097/ALN.0b013e318182a93b. [DOI] [PubMed] [Google Scholar]
- 29.Jungbluth H, Muller CR, Halliger-Keller B, Brockington M, Brown SC, Feng L, Chattopadhyay A, Mercuri E, Manzur AY, Ferreiro A, Laing NG, Davis MR, Roper HP, Dubowitz V, Bydder G, Sewry CA, Muntoni F. Autosomal recessive inheritance of RYR1 mutations in a congenital myopathy with cores. Neurology. 2002;59:284–287. doi: 10.1212/wnl.59.2.284. [DOI] [PubMed] [Google Scholar]
- 30.Tilgen N, Zorzato F, Halliger-Keller B, Muntoni F, Sewry C, Palmucci LM, Schneider C, Hauser E, Lehmann-Horn F, Muller CR, Treves S. Identification of four novel mutations in the C-terminal membrane spanning domain of the ryanodine receptor 1: association with central core disease and alteration of calcium homeostasis. Hum Mol Genet. 2001;10:2879–2887. doi: 10.1093/hmg/10.25.2879. [DOI] [PubMed] [Google Scholar]
- 31.Shepherd S, Ellis F, Halsall J, Hopkins P, Robinson R. RYR1 mutations in UK central core disease patients: more than just the C-terminal transmembrane region of the RYR1 gene. J Med Genet. 2004;41:e33. doi: 10.1136/jmg.2003.014274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sewry CA, Muller C, Davis M, Dwyer JS, Dove J, Evans G, Schroder R, Furst D, Helliwell T, Laing N, Quinlivan RC. The spectrum of pathology in central core disease. Neuromuscul Disord. 2002;12:930–938. doi: 10.1016/s0960-8966(02)00135-9. [DOI] [PubMed] [Google Scholar]
- 33.Quinlivan RM, Muller CR, Davis M, Laing NG, Evans GA, Dwyer J, Dove J, Roberts AP, Sewry CA. Central core disease: clinical, pathological, and genetic features. Arch Dis Child. 2003;88:1051–1055. doi: 10.1136/adc.88.12.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis MR, Haan E, Jungbluth H, Sewry C, North K, Muntoni F, Kuntzer T, Lamont P, Bankier A, Tomlinson P, Sanchez A, Walsh P, Nagarajan L, Oley C, Colley A, Gedeon A, Quinlivan R, Dixon J, James D, Muller CR, Laing NG. Principal mutation hotspot for central core disease and related myopathies in the C-terminal transmembrane region of the RYR1 gene. Neuromuscul Disord. 2003;13:151–157. doi: 10.1016/s0960-8966(02)00218-3. [DOI] [PubMed] [Google Scholar]
- 35.Monnier N, Krivosic-Horber R, Payen JF, Kozak-Ribbens G, Nivoche Y, Adnet P, Reyford H, Lunardi J. Presence of two different genetic traits in malignant hyperthermia families: implication for genetic analysis, diagnosis, and incidence of malignant hyperthermia susceptibility. Anesthesiology. 2002;97:1067–1074. doi: 10.1097/00000542-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Carpenter D, Robinson RL, Quinell RJ, Ringrose G, Hogg M, Casson F, Booms P, Eles DE Halsall PJ, Steele DS, Shaw MA, Hopkins PM. Genetic variation in. RYR1 and malignant hyperthermia phenotypes. Br J Anaesth. 2009;103:538–548. doi: 10.1093/bja/aep204. [DOI] [PubMed] [Google Scholar]
- 37.Loke JC, MacLennan DH. Bayesian modeling of muscle biopsy contracture testing for malignant hyperthermia susceptibility. Anesthesiology. 1998;88:589–600. doi: 10.1097/00000542-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Maile MD, Patel RA, Blum JM, Tremper KK. A case of malignant hyperthermia captured by an anesthesia information management system. J Clin Monit Comput. 2011;25:109–111. doi: 10.1007/s10877-011-9285-1. [DOI] [PubMed] [Google Scholar]
- 39.Larach MG, Gronert GA, Allen GC, Brandom BW, Lehman EB. Clinical presentation, treatment, and complications of malignant hyperthermia in North America from 1987 to 2006. Anesth Analg. 2010;110:498–507. doi: 10.1213/ANE.0b013e3181c6b9b2. [DOI] [PubMed] [Google Scholar]
- 40.Allen GC, Larach MG, Kunselman AR. The sensitivity and specificity of the caffeine-halothane contracture test, a report from the North American Malignant Hyperthermia Registry. Anesthesiology. 1998;88:579–588. doi: 10.1097/00000542-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Ginz HF, Girard T, Censier K, Urwyler A. Similar susceptibility to halothane, caffeine and ryanodine in vitro reflects pharmacogenetic variability of malignant hyperthermia. Eur J Anaesthesiol. 2004;21:151–157. doi: 10.1017/s0265021504002121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.