Abstract
Background
The prevalence of anterior knee pain following intramedullary tibial nail insertion is high. Continuous peripheral nerve blockade is an alternative method of pain control to opiods. This case illustrates the use of femoral nerve and sciatic nerve peripheral catheters with an elastomeric infusion pump for major intramedullary nailing surgery.
Case report
A 36-year-old male with fractures to the left leg bones presented for placement of an intramedullary nail under spinal anesthesia. At the end of the procedure, access to the lateral femoral and sciatic continuous nerve block was achieved by using a stimulator connected to a 110 mm 18G Tuohy needle. Postoperative analgesia was provided with a 40-hour infusion of 0.1% bupivacaine (400 mL) at a rate of 10 mL hour−1 with an elastomeric pump. Anesthetic dispersion and contrast were investigated. The analog scale remained with scores below 3 during the 40 hours after surgery, and boluses were not necessary.
Conclusion
The use of a femoral and sciatic nerve peripheral catheter offered an alternative to conventional pain control. Continuous femoral–sciatic peripheral blockade via a skin puncture with an infusion of 0.1% bupivacaine with elastomeric pumps is a safe and effective procedure in adults.
Keywords: local anesthetic, bupivacaine, continuous peripheral nerve block, orthopedic surgery, tibia, elastomeric pump
Tibial shaft fracture is one of the most common types of long-bone fractures in orthopedic practice. Reamed intramedullary nailing is now commonly used in the management of tibial shaft fractures and is considered by some to be the treatment of choice in closed displaced fractures.1 After appropriate fracture reduction, one of three skin incisions may be used: a 5 cm longitudinal incision made medial to the patellar tendon between the tibial tubercle and the inferior border of the patella, a 5 cm longitudinal incision made transpatellar to the tendon between the tibial tubercle and the inferior border of the patella, or a transverse incision midway between the joint and tibial tuberosity. Anterior knee pain is the most common complication after intramedullary nailing of the tibia.2 The prevalence of chronic anterior knee pain following intramedullary tibial nail insertion has been reported as being between 10%3 to 86%.2 However, a recent meta-analysis of the literature estimated the incidence at 47.4%.4
Lumbar plexus block when combined with sciatic nerve block is a safe and effective alternative for analgesia in lower limb surgery. A lateral approach to sciatic–femoral block combined via a single skin injection was recently described.5 The objective of the present report was to describe a lateral, continuous, combined, femoral–sciatic nerve approach with a portable elastomeric device in a patient undergoing intramedullary tibial nail insertion.
Case report
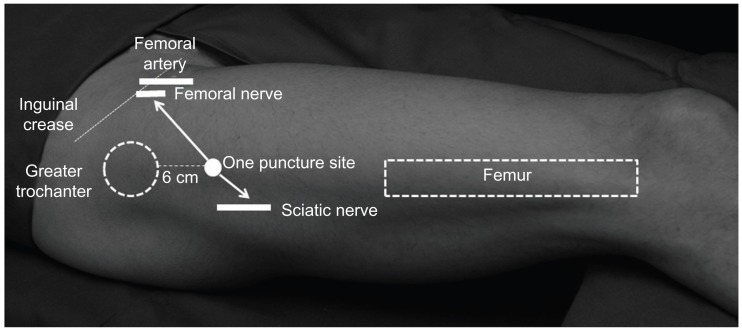
A 36-year-old man (66 kg, 170 cm, physical status American Society of Anesthesiology [ASA] I) with fractures to the left leg bones was scheduled for an intramedullary nail under spinal anesthesia. The patient was evaluated and signed the informed consent to undergo a single needle entry combined approach of continuous peripheral blocks (Figure 1). After routine monitoring, spinal anesthesia was performed with a 27G Quincke needle (BBraun, Melsungen, Germany) in the L3–L4 space through a median approach with the patient in a lateral position. The patient was injected with 15 mg of isobaric 0.5% bupivacaine.
Figure 1.
Diagram for insertion of the needle.
During the procedure, the patient was supine on a radiolucent table. Nail length was determined under traction with image intensification. A transpatellar approach was used for the proximal tibia, which was opened with a solid awl under image intensification. The proximal fracture site was opened and a reaming rod was inserted; the distal fracture site was reduced and closed. The segmentar fragment was locked with a Schanz screw. The canal was reamed, and one poller screw was inserted in the distal fragment. We introduced a 9 mm diameter cannulated nail and achieved distal locking with two screws (freehand locking technique). Proximal locking was with two screws. An end cap was inserted.
During the procedure, 1000 mL of crystalloids and 500 mL of Voluven® (6% hydroxyethyl starch 130/0.4 in 0.9% saline) were administered. No urinary catheter was utilized during the procedure.
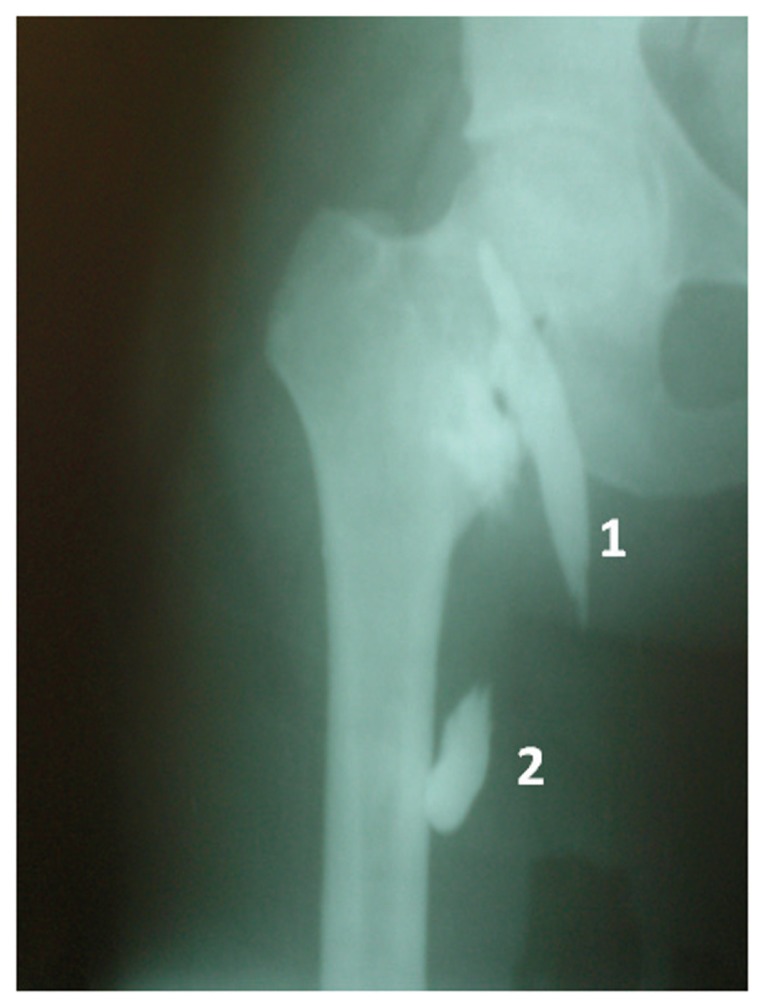
At the end of the procedure, access to lateral femoral and sciatic continuous nerve block was achieved using a stimulator (HNS12; BBraun) connected to a 110 mm 18G Tuohy needle (BBraun). The needle was advanced and the quadriceps were stimulated with a 0.5 mA current until a response was observed. After negative aspiration of blood, 20 mL of 0.2% bupivacaine was injected through an extension connector of the needle. While maintaining the needle in the same position, a 20G catheter was inserted 7 cm into the inguinal compartment and was fixed in place with adhesive material and an occlusive dressing. Another needle was then advanced posteriorly and caudally to reach the sciatic nerve, which was identified by stimulation of the common fibular nerve or tibial nerve, confirmed by movements of the foot. We then injected 20 mL of the same anesthetic solution. Approximately 5 mL of contrast (iohexol with 300 mg mL−1 Ominipaque®) was injected in each catheter to study the dispersion of the local anesthetic, and an anteroposterior X-ray was taken within 1 minute (Figure 2).
Figure 2.
The spread of contrast in combined continuous femoral and sciatic nerve block.
Notes: 1 is the spread of contrast in the continuous femoral nerve block; 2 is the spread of contrast in the continuous sciatic nerve block.
Before his discharge, a disposable elastomeric pump (Easypump®, BBraun) containing 400 mL of 0.1% bupivacaine was connected to the catheters of both nerves. The pump was programmed for infusion at a rate of 10 mL · hour−1. Upon completion the patient was transferred to the postanesthesia care unit. An analog scale was used to divide patients pain into categories of mild or no pain (0–3), moderate pain (4–7), and severe pain (8–10). The patient remained with scores below 3 during the 40 hours after surgery. He received instructions to trigger the bolus device, which is part of the pump, in case of severe pain. Toxicity symptoms of the local anesthetic were recorded. During the 40 postoperative hours, boluses were not necessary. Both catheters were removed without intercurrences and were sent for bacteriological examination after removal; pain was then controlled with oral ketoprofen and dypirone.
Discussion
The use of a lateral, continuous, combined, femoral–sciatic nerve approach via a single skin puncture for postoperative analgesia for tibial intramedullary nailing has not been reported. Since this method administers a local anesthetic close to the continuous combined femoral–sciatic nerve, analgesia can be prolonged, especially in patients with a tibial shaft fracture. The results of this case demonstrate that an elastomeric pump for a continuous peripheral nerve block with infusion of a local anesthesia in adult patients is an effective and safe analgesic method after extensive orthopedic procedures. The use of rescue analgesia was minimal.
Although many closed fractures of the tibial shaft can be treated nonoperatively,6 there are numerous indications for operative treatment. The choice of surgical approach, specifically using the transpatellar or parapatellar tendon, has been reported as a contributory factor in chronic anterior knee pain following tibial nail insertion. In a retrospective study in which a nail was inserted via a paratendinous incision in 65 fractures and via a tendon-splitting incision in 36 fractures, insertion of an intramedullary nail through the paratendinous incision resulted in a 50% incidence of knee pain, whereas this incidence in the transtendinous incision group was 77%.7 This is in contrast to other reports of no significant difference.8 In this case study the incision was transpatellar.
A lateral entrance in the inguinal lumbar plexus allows the needle to find the femoral nerve before reaching the femoral artery. An entry perpendicular and below the greater trochanter reaches the sciatic nerve after touching the femur bone. The lateral entrance reduced the risk of lateral displacement, facilitating the movement of the patient and allowing personal hygiene, such as changing the dressing to reduce the risk of infection.
The use of bupivacaine (0.1% to 0.25%) as used in our case study did not result in toxic blood levels in postoperative analgesia for 24–72 hours.9 The venous level of bupivacaine during continuous lumbar plexus analgesia was 0.5–1.8 μg mL−1,10 while levels above 2 μg mL−1 are considered toxic. Continuous peripheral nerve block analgesia, regardless of catheter location, provided superior postoperative analgesia and fewer opioid-related side effects when compared with an opioid analgesia.11 In surgery, the continuous plexus block is used primarily to improve the quality of postoperative analgesia and allow early rehabilitation. There was no difference in pain between rest and movement, showing that continuous analgesia decreased the incidence of postoperative pain to 3 on the visual analog scale during the 48 hours following the operation.
A lateral, continuous, combined, femoral–sciatic block was performed with a peripheral nerve stimulator, and we observed the distribution of contrast around both nerves. The distribution of contrast showed a higher level in the inguinal region through the femoral nerve and below the subtrochanteric femur in the region through the sciatic nerve.
Portable pumps are increasingly being used in continuous regional anesthesia. Those pumps are frequently used in outpatients without medical supervision. If the elastomeric pump lies below the catheter tip, the delivery of the agent can be impaired to a variable extent. Our case study demonstrated that the patient received adequate analgesia in both catheters. The rate of flow of the anesthetics is dictated by the elastomeric reservoir and the gauge of the tube, which prevents the infusion of a large bolus and overdose. Although the pump has its own bacterial filter, we used a second filter to increase patient safety. The elastomeric pump has several advantages over the electronic pump, including portability, ease of use, and few technical problems, such as undesirable alarms.12
Severe infectious complications have been reported after continuous blockade, with about 29% of peripheral nerve catheters being colonized with up to 3% bacteria, resulting in localized inflammation.13 Continuous peripheral nerve block (CPNB) duration (>48 hours) was a strong risk factor for local infectious problems.13 We prospectively reported an incidence of 57% colonized femoral catheters (1.5% with bacteremia) after 48 hours of continuous infusion of bupivacaine or ropivacaine.14 Given the results of infection after 48 hours, the pump was scheduled to stop 48 hours after surgery. With lateral access to the axilar brachial plexus and inguinal lumbar plexus, we did not observe any bacterial growth in 20 catheters, similar to our finding that in 48 hours there was no sign of inflammation at the puncture site.15 Likewise, bacteriological examination of both catheters found no bacterial growth.
Conclusion
The use of extended local anaesthesia for postoperative pain has previously been reported and has several advantages over other methods, including ease of placement, safety, reliability, lower cost, and effectiveness. We conclude that continuous femoral–sciatic peripheral nerve block via a single skin puncture with infusion of 0.1% bupivacaine via an elastomeric pump is a safe and effective procedure in adults for surgical treatment of tibia fractures by intramedullary nailing.
Footnotes
Disclosure
The authors have no conflicts of interest to report.
References
- 1.Court-Brown CM, Will E, Christie J, McQueen MM. Reamed or unreamed nailing for closed tibial fractures. A prospective study in Tscherne C1 fractures. J Bone Joint Surg. 1992;74-B:770–774. [PubMed] [Google Scholar]
- 2.Toivanen JA, Vaisto O, Kannus P, Latvala K, Honkonen SE, Jarvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nailinsertion techniques. J Bone Joint Surg Am. 2002;84-A:580–585. doi: 10.2106/00004623-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Karachalios T, Babis G, Tsarouchas H, et al. The clinical performance of a smaller diameter tibial nailing system with a mechanical distal aiming device. Injury. 2003;31:451–459. doi: 10.1016/s0020-1383(00)00024-3. [DOI] [PubMed] [Google Scholar]
- 4.Katsoulis E, Court-Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br. 2006;88-B:576–580. doi: 10.1302/0301-620X.88B5.16875. [DOI] [PubMed] [Google Scholar]
- 5.Imbelloni LE. A new lateral combined femoral-sciatic nerve approach via a single skin puncture (Letter to Editor) J Pain Relief. 2012;1:102. [Google Scholar]
- 6.Nicoll EA. Fractures of the tibial shaft. A survey of 705 cases. Bone and Joint Surg. 1964;46-B:373–387. [PubMed] [Google Scholar]
- 7.Keating JF, Orfaly R, O’Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11:10–13. doi: 10.1097/00005131-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Väistö O, Toivanen J, Paakkala T, Järvelä T, Kannus P, Järvinen M. Anterior knee pain after intramedullary nailing of a tibial shaft fracture. An ultrasound study of the patellar tendons of 36 patients. J Orthop Trauma. 2005;19:311–316. [PubMed] [Google Scholar]
- 9.Liu SS, Salinas FV. Continuous plexus and peripheral nerve blocks for postoperative analgesia. Anesth Analg. 2003;96:263–272. doi: 10.1097/00000539-200301000-00053. [DOI] [PubMed] [Google Scholar]
- 10.Anker-Moller E, Spangsbersg N, Dahl JB, et al. Continuous blockade of the lumbar plexus after knee surgery: a comparison of the plasma concentrations and analgesic effect of bupivacaine 0.250% and 0.125% Acta Anaesthesiol Scand. 1990;34:468–472. doi: 10.1111/j.1399-6576.1990.tb03125.x. [DOI] [PubMed] [Google Scholar]
- 11.Richman J, Liu SS, Courpas G, et al. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg. 2006;102:248–257. doi: 10.1213/01.ANE.0000181289.09675.7D. [DOI] [PubMed] [Google Scholar]
- 12.Capdevila X, Macaire P, Aknin P, et al. Patient-controlled perineural analgesia after ambulatory orthopedic surgery: a comparison of electronic versus elastomeric pumps. Anesth Analg. 2003;96:414–417. doi: 10.1097/00000539-200302000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Capdevila X, Pirat P, Bringuier S, et al. French Study Group on Continuous Peripheral Nerve Blocks. Continuous peripheral nerve blocks in hospital wards after orthopedic surgery. A multicenter prospective analysis of the quality of postoperative analgesia and complications in 1416 patients. Anesthesiology. 2005;103:1035–1045. doi: 10.1097/00000542-200511000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Cuvillon P, Ripart J, Lalourcey L, et al. The continuous femoral nerve block catheter for postoperative analgesia: bacterial colonization, infectious rate and adverse effects. Anesth Analg. 2001;93:1045–1049. doi: 10.1097/00000539-200110000-00050. [DOI] [PubMed] [Google Scholar]
- 15.Imbelloni LE, Silva Neto EJ, Carneiro AF, Lobão A, Imperiano B, Grigório R. A new continuous lateral access to axillary and femoral nerves decreases pain in movement and catheter contamination. Sci J Med Clin Trials. 2012;2:1–8. [Google Scholar]