Abstract
Background and Purpose
We evaluated whether stent-assisted thrombectomy (SAT) is safer or more clinically beneficial than aggressive mechanical clot disruption (AMCD) for patients with acute intracranial artery occlusion.
Methods
We retrospectively analyzed the clinical data of 72 patients (33 with SAT and 39 with AMCD) who underwent intra-arterial thrombolysis for acute intracranial artery occlusions. Procedure parameters, clinical outcomes, and incidence of complications were compared between the SAT and AMCD groups.
Results
The time interval to recanalization was shorter in SAT patients (69.2±39.6 minutes, mean±standard deviation) than in AMCD patients (94.4±48.0 minutes, p<0.05). Recanalization was achieved in more SAT patients (91%) than AMCD patients (80%), but with no statistically significance. Urokinase was used less frequently in SAT patients (21%) than in AMCD patients (92%, p<0.05), and the incidence of symptomatic hemorrhages was lower in SAT patients (3%) than in AMCD patients (18%, p<0.05). Device-related complications in SAT patients comprised two cases of stent fracture and one case of distal migration of a captured thrombus. The proportion of patients with good outcomes, defined as scores from 0 to 3 on the modified Rankin Scale, was similar in the two groups at discharge (SAT, 46%; AMCD, 39%), but significantly higher in the SAT group than in the AMCD group at 3 months (64% vs. 40%, p<0.05) and 6 months (67% vs. 42%, p<0.05) after discharge.
Conclusions
The outcomes and clinical parameters were better for SAT during thrombolytic procedures for acute intracranial artery occlusions than for AMCD for up to 6 months. However, some device-related complications occurred during stent interventions.
Keywords: acute stroke, mechanical thrombolysis, stent-assisted thrombectomy
Introduction
Early recanalization after acute occlusion of large intracranial arteries is important to restore cerebral perfusion and to decrease future clinical deterioration.1,2 Even though intravenous and/or intra-arterial thrombolysis (IAT) have been used to increase the probability of early recanalization for large-intracranial-artery occlusions, incomplete or failed recanalization of the occluded vessels is a major problem.2 In particular, large thrombi within the terminal internal carotid artery expanding to the adjacent middle cerebral artery (MCA) and anterior cerebral artery (ACA) usually cannot be removed by pharmacological IAT alone.2,3 To improve recanalization rates during IAT, mechanical techniques such as aggressive mechanical clot disruption (AMCD) using microcatheters,4,5 balloon angioplasty,6 microsnares,7 and new devices such as the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) device8,9 and the Penumbra system10 have been developed and used for large-artery occlusions.
Stent-assisted thrombectomy (SAT) using retrievable stents has recently been applied as a mechanical thrombolytic technique to rapidly remove a thrombus from an occluded vessel.11-14 Some preliminary studies produced beneficial results when using SAT to treat large-intracranial-artery occlusions, including high recanalization rates and short procedure times.11-14 However, those studies obtained clinical and imaging data of SAT without comparing SAT with previous intra-arterial recanalization techniques such as conventional IAT or other mechanical techniques. The present study evaluated the technical safety and clinical benefits of SAT by comparing SAT with IAT performed by intra-arterial injection of a thrombolytic agent and/or AMCD.
Methods
Patients
We retrospectively analyzed clinical and imaging data of patients with acute cerebral infarction who were admitted to Chungnam National University Hospital, Daejeon, South Korea between January 2007 and September 2011 and who underwent IAT to recanalize acute occlusions of intracranial arteries. IAT was applied to patients who had a National Institutes of Health Stroke Scale (NIHSS) score of 4 or more, were older than 18 years, arrived at the emergency room within 6 hours of symptom onset, and had angiographically confirmed occlusion of the unilateral MCA and/or terminal internal carotid artery or the basilar artery. Conventional IAT using AMCD was performed from January 2007 to October 2010, while SAT using a retrievable stent (Solitaire AB®, ev3, Irvine, CA, USA) was performed from November 2010 to September 2011. Patients who had acute cerebral infarctions caused by occlusion of the distal common carotid artery, proximal ICA, or extracranial vertebral artery were excluded, as were those who met the exclusion criteria of the National Institute of Neurological Disorders and Stroke protocol for thrombolysis.15 The study protocol was reviewed and approved by the Institutional Review Board of Chungnam National University Hospital.
Imaging and thrombolysis protocol
Brain computed tomography (CT) was initially performed within 3 hours after symptom onset. After confirmation that there was neither hemorrhage nor low density involving greater than one-third of the MCA territory on the CT scan, 0.9 mg/kg recombinant tissue plasminogen activator was infused for 1 hour after a bolus injection of 10% of the calculated amount of recombinant tissue plasminogen activator. We continued AMCD or SAT if the neurological status of the patient did not improve after intravenous therapy and mismatches between diffusion-weighted images and perfusion-weighted images re-mained on magnetic resonance imaging (MRI) scans. When a patient arrived between 3 and 6 hours after symptom onset, AMCD or SAT was performed without intravenous thrombolysis after confirming the presence of DWI-PWI mismatch on MRI and no hemorrhage on CT.
IAT
AMCD and SAT have both been used for IAT in our hospital. During the first part of the study period, from January 2007 to October 2010, AMCD was performed in acute-intracranial-occlusion patients. We performed aggressive mechanical catheterization using a microcatheter and/or a J-shaped guide-wire tip within the occluded arterial lumen.4 The efficacy of thrombolysis was increased in some patients by also injecting urokinase. During the second part of the study period, from November 2010 to September 2011, we performed SAT for acute-cerebral-infarction patients. A retrievable stent (Solitaire AB®, ev3) was first deployed within the impacted thrombus at the occluded vessels. After 10-15 minutes the stent was retrieved within a guiding catheter. We then withdrew the entire guiding catheter and simultaneously applied negative pressure with an aspiration device to reduce the likelihood of distal migration of the captured thrombi. Finally, we performed angiography to confirm recanalization of the occluded vessel. If reocclusion occurred within the recanalized artery after SAT, intra-arterial urokinase injection, balloon angioplasty, and/or stenting were performed after SAT.
Evaluation of clinical parameters
We compared clinical parameters between patients who received SAT and those who received AMCD. First, to evaluate whether SAT recanalized the occluded vessels more rapidly than AMCD, we compared the door-to-puncture times and puncture-to-recanalization times between the two thrombolysis groups. We also compared the rates of recanalization, which was evaluated using the Thrombolysis in Cerebral Infarction (TICI) Scale,16 with successful recanalization defined as grade 2 or 3 on the TICI Scale.4
Next, to compare differences in early and late functional recoveries between the AMCD and SAT groups, we evaluated the NIHSS and modified Rankin Scale (mRS) scores before and immediately after interventions, at discharge, and at 3 and 6 months after discharge. To evaluate clinical outcomes after IAT, the proportion of good outcomes (mRS score of 0 to 317) was compared between the two groups.
Finally, the safety of SAT and AMCD were compared based on the frequencies and doses of urokinase injections and incidences of hemorrhagic transformation in the two groups. Hemorrhagic transformation was classified into four categories: 1) small petechiae within the infracted lesion, 2) confluent petechiae without space-occupying effects, 3) small hematoma (≤30% of infarcted area) with a slight space-occupying effect, and 4) large hematoma (>30% of the infarcted area) or outside hemorrhage with a substantial space-occupying effect.18,19 Symptomatic intracerebral hemorrhage (ICH) was defined as clinical aggravation (increase in the NIHSS score of ≥4) and simultaneous large hematoma or outside hemorrhage on CT or MRI performed within 24 hours of thrombolysis.20
Statistical analyses
Changes in the NIHSS score between admission and discharge, and the time intervals from symptom onset or start of intra-arterial interventions to recanalization of the occluded vessels were compared between the SAT and AMCD groups using t-tests. The recanalization rates and hemorrhagic complications of the two groups were compared using Fisher's exact test.
Differences in the clinical outcomes between the two groups were analyzed by comparing the proportion of patients with a good outcome at discharge (mRS score of 0-3) with the proportion of patients discharged, and the proportion of patients with good outcomes at 3 and 6 months after discharge using Fisher's exact test. All statistical analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA).
Results
This retrospective study reviewed clinical and procedure data from 72 patients (45 males and 27 females; age 65.4±12.8 years, mean±standard deviation) who underwent intra-arterial recanalization for acute cerebral infarction. Thirty-nine patients were treated by AMCD while the other 33 patients were treated by SAT to recanalize the occluded vessels. There was no significant difference in age at onset or incidences of underlying risk factors for cerebral infarction such as hypertension, smoking, atrial fibrillation, or previous cerebrovascular diseases between the two groups (Table 1).
Table 1.
Baseline characteristics of the patients
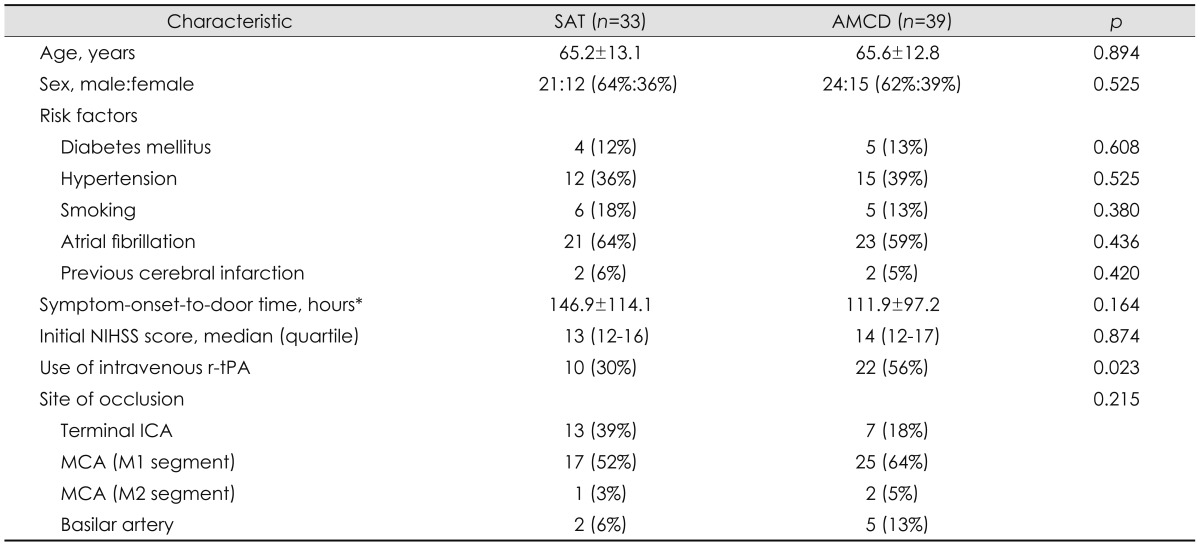
Data are n (%) or mean±SD values.
*Time interval from the symptom onset to arrival at the emergency room.
AMCD: aggressive mechanical clot disruption, ICA: internal carotid artery, MCA: middle cerebral artery, NIHSS: National Institutes of Health Stroke Scale, r-tPA: recombinant tissue plasminogen activator, SAT: stent-assisted thrombectomy.
Differences in clinical parameters between the SAT and AMCD groups
Recanalization was achieved more rapidly from the start of intra-arterial interventions by SAT (69.2±39.6 minutes) than by AMCD (94.4±48.0 minutes, p<0.05). The rate of successful recanalization (TICI-Scale score of 2 or 3) was higher in SAT patients (91%) than in AMCD patients (80%), but it was not statistically significant (p>0.05) (Table 2).
Table 2.
Clinical parameters in the SAT and AMCD groups
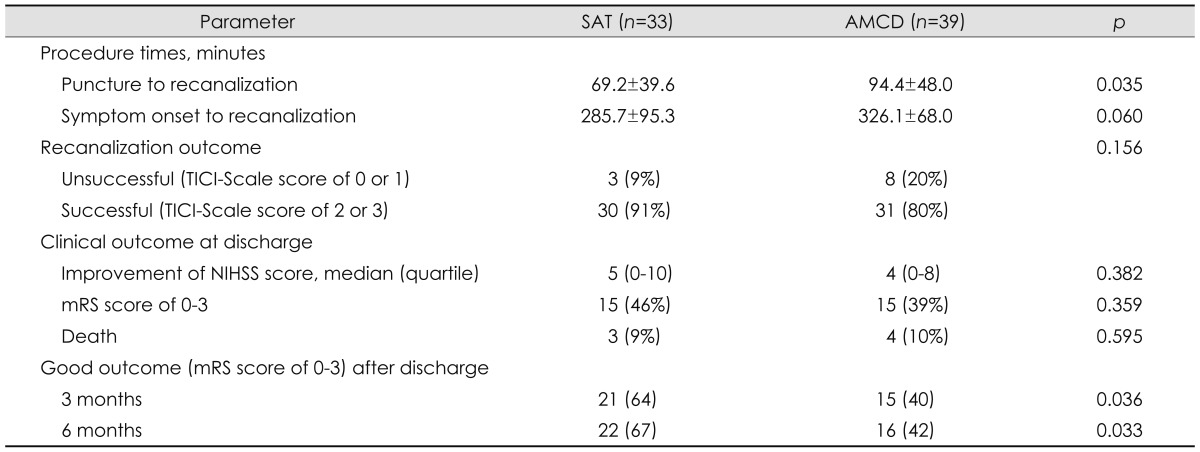
Data are n (%) or mean±SD values.
AMCD: aggressive mechanical clot disruption, mRS: modified Rankin Scale, SAT: stent-assisted thrombectomy, TICI: Thrombolysis in Cerebral Infarction.16
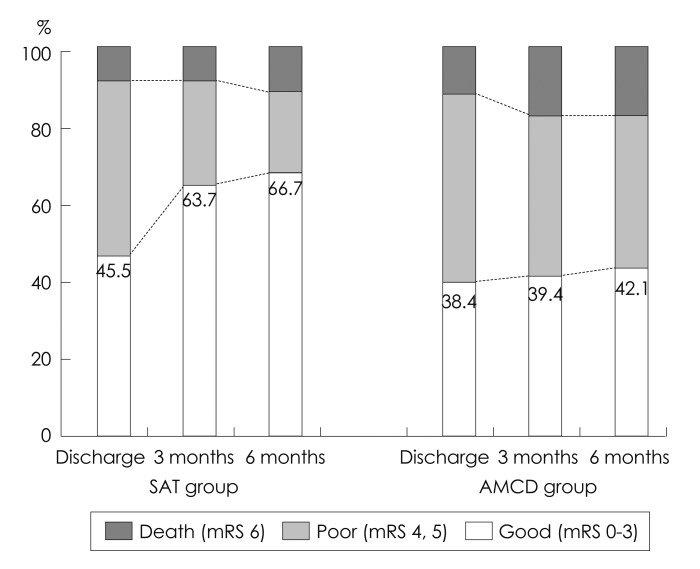
With regard to clinical outcomes at discharge, the improvement in the NIHSS score (SAT, 5.8±6.1; AMCD, 4.7±4.9; p>0.05) and the proportion of good early neurological outcomes, as defined by an NIHSS score of 0 or 1 or an improvement of 8 or more in the NIHSS score (SAT, 27%; AMCD, 31%; p>0.05), were similar in the SAT and IAT groups. The proportion of good outcomes (mRS score of 0 to 3) was similar in the two groups at discharge (SAT, 46%; AMCD, 39%; p>0.05), but was significantly higher in patients who underwent SAT than those that underwent AMCD at both 3 months (SAT, 64%; AMCD, 40%; p<0.05) and 6 months (SAT, 67%; AMCD, 42%; p<0.05) after discharge (Table 2). Interestingly, the improvements in the mRS score were more favorable in the SAT group than in the AMCD group; the proportion of patients with a good outcome (mRS score of 0 to 3) increased from 46% to 67% after 6 months, while the proportion of patients with a not-good outcome (mRS score of 4 to 6) decreased from 54% to 33% during the same time period, despite the AMCD group having similar proportions of patients with good and not-good outcomes (defined based on mRS scores) during the follow-up period (Fig. 1).
Fig. 1.
Change in score on the modified Rankin Scale (mRS) after stent-assisted thrombectomy (SAT) and aggressive mechanical clot disruption (AMCD).
Periprocedure complications associated with intra-arterial procedures
Urokinase for recanalizing the occluded vessel was used more frequently in the AMCD group (92%) than in the SAT group (21%). Furthermore, more urokinase was injected in the AMCD group than in the SAT group (median urokinase doses of 430000 IU vs. 270000 IU) (Table 3). The incidence rates of confluent petechiae and smaller hematomas were higher in the SAT group than in the AMCD group (Table 3). However, the incidence of symptomatic ICH with a large hematoma was significantly higher in the AMCD group than in the SAT group (p<0.05). One patient in the SAT group showed symptomatic ICH combined with subarachnoid hemorrhage.
Table 3.
Hemorrhagic and procedure-related complications in the SAT and AMCD groups
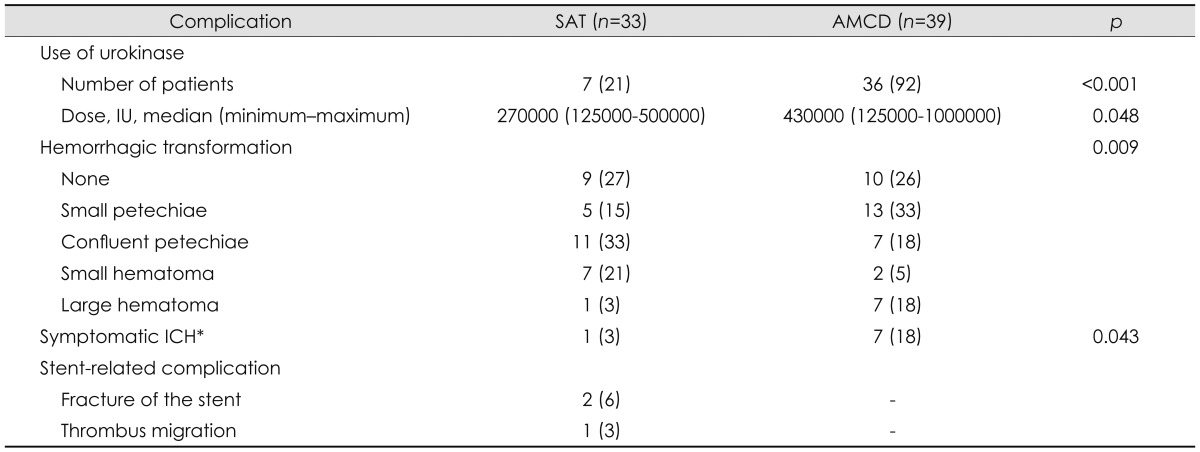
Data are n (%) values except where stated otherwise.
*Hemorrhagic transformation on computed tomography or magnetic resonance imaging follow-up within 24 hours after intra-arterial thrombolysis, which was associated with an increase of at least 4 points relative to the initial NIHSS score.20
AMCD: aggressive mechanical clot disruption, ICH: intracerebral hemorrhage, SAT: stent-assisted thrombectomy.
Stent-related complications occurred in three patients in the SAT group (Table 3). Two of these patients experienced accidental fracture of the stent during retrieval occurred at the occluded MCA sites: one underwent balloon dilatation within the remaining stent, while the other underwent intracranial stent deployment within the fractured stent using a metal stent. The intraluminal patency of the ballooned-fractured stent or metal stent was well maintained on follow-up angiography performed 2 days after SAT. The third patient with a stent-related complication experienced distal migration of an initially captured thrombus within the stent occurred. In this patient the thrombus captured at the proximal MCA migrated and impacted the ipsilateral ACA during stent retrieval. The thrombus located in the ACA was immediately and completely removed by repeated SAT, and no further infarction was detected after this intervention.
Discussion
Our comparison of SAT and IAT revealed that direct thrombus removal using retractable stents resulted in better clinical outcomes at 6 months after the intervention. The short procedure time intervals, high recanalization rates, and low incidence of hemorrhagic complications are further advantages of using SAT for recanalization.
Short time intervals to recanalization and higher recanalization rates have been suggested to be important to achieving good mechanical thrombolysis outcomes.2 The mean recanalization time was 25 minutes shorter in the SAT group than in the AMCD group, consistent with the results of previous SAT studies.11-13 Moreover, our time interval for SAT is even shorter than that recently found in the MERCI trial (mean 96 minutes, range 72-138 minutes).8 High recanalization rates were reported after AMCD using microcatheters (75%)5 or other mechanical thrombectomies using multi-MERCI (69.5%)8 or Penumbra system (81.6%).8,10 The recanalization rate was also high when SAT was used to treat intracranial occlusions.11-13 Our finding that recanalization rates were higher for SAT (91%) than for AMCD (80%) is consistent with the results of previous studies. A short interval to recanalization and high recanalization rate therefore appear to be important determinants of good clinical outcomes after SAT.
The large amounts of thrombolytic agents used for recanalization could be responsible for the high rate of hemorrhagic conversion after thrombolysis.20 AMCD frequently requires the use of thrombolytic agents, and symptomatic hemorrhage has been reported in 9.4% of cases.4 Fewer patients in our SAT group than our AMCD group required urokinase, and the mean dose was lower in the SAT group. Furthermore, the incidence of symptomatic hemorrhages was significantly lower in the SAT group than in the AMCD group. Fewer hemorrhagic complications will improve the good clinical outcomes after SAT.
Unexpected device-related complications can be encountered when performing intra-arterial interventions using mechanical devices; complication rates of 5.5% and 12.8% have been reported for the MERCI8 and Penumbra10 systems, respectively. Three patients (9.1%) in our SAT group experienced device-related complications, including fracture of the stent and distal migration of the captured thrombi. Even though these complications were immediately and successfully resolved during thrombolysis, great care is required when manipulating the retrievable stent in order to decrease the incidence of device-related complications.
In conclusion, we have studied the benefits and limitations of SAT for early recanalization of occluded intracranial vessels. Patients treated with SAT had shorter recanalization times, higher recanalization rates, a lower incidence of hemorrhagic complications, and required a lower dose of urokinase than patients treated with AMCD. These clinical benefits of SAT may account for the good clinical outcomes observed 6 months after the intervention. However, SAT should be performed cautiously in patients with acute cerebral infarction due to the possibility of unexpected device-related complications during interventional procedures.
The limitations of our study included the clinical data being collected retrospectively from a small number of patients admitted to a single stroke center. In particular, AMCD and SAT were performed at different time periods at our institute. However, the obtained results suggest that SAT is a viable alternative technique to AMCD for treating patients with acute intracranial artery occlusion. Future randomized studies involving large numbers of patients should attempt to verify the benefits of SAT described herein.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA, et al. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009;73:1066–1072. doi: 10.1212/WNL.0b013e3181b9c847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38:967–973. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 3.Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002;33:2066–2071. doi: 10.1161/01.str.0000021001.18101.a5. [DOI] [PubMed] [Google Scholar]
- 4.Noser EA, Shaltoni HM, Hall CE, Alexandrov AV, Garami Z, Cacayorin ED, et al. Aggressive mechanical clot disruption: a safe adjunct to thrombolytic therapy in acute stroke? Stroke. 2005;36:292–296. doi: 10.1161/01.STR.0000152331.93770.18. [DOI] [PubMed] [Google Scholar]
- 5.Sorimachi T, Fujii Y, Tsuchiya N, Nashimoto T, Harada A, Ito Y, et al. Recanalization by mechanical embolus disruption during intra-arterial thrombolysis in the carotid territory. AJNR Am J Neuroradiol. 2004;25:1391–1402. [PMC free article] [PubMed] [Google Scholar]
- 6.Watanabe M, Mori T, Imai K, Izumoto H, Kamiya T. Intra-arterial fibrinolysis combined with balloon angioplasty in patients with serious symptoms due to acute embolic total occlusion of the carotid artery [abstract] Stroke. 2004;35:298. [Google Scholar]
- 7.Imai K, Mori T, Izumoto H, Watanabe M. Successful thrombectomy in acute terminal internal carotid occlusion using a basket type microsnare in conjunction with temporary proximal occlusion: a case report. AJNR Am J Neuroradiol. 2005;26:1395–1398. [PMC free article] [PubMed] [Google Scholar]
- 8.Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39:1205–1212. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 9.Flint AC, Duckwiler GR, Budzik RF, Liebeskind DS, Smith WS MERCI and Multi MERCI Writing Committee. Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials. Stroke. 2007;38:1274–1280. doi: 10.1161/01.STR.0000260187.33864.a7. [DOI] [PubMed] [Google Scholar]
- 10.The Penumbra Pivotal Stroke Trial Investigators. The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–2768. doi: 10.1161/STROKEAHA.108.544957. [DOI] [PubMed] [Google Scholar]
- 11.Castaño C, Dorado L, Guerrero C, Millán M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010;41:1836–1840. doi: 10.1161/STROKEAHA.110.584904. [DOI] [PubMed] [Google Scholar]
- 12.Nayak S, Ladurner G, Killer M. Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent: preliminary experience. Br J Radiol. 2010;83:1017–1022. doi: 10.1259/bjr/42972759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seifert M, Ahlbrecht A, Dohmen C, Spuentrup E, Moeller-Hartmann W. Combined interventional stroke therapy using intracranial stent and local intraarterial thrombolysis (LIT) Neuroradiology. 2011;53:273–282. doi: 10.1007/s00234-010-0719-0. [DOI] [PubMed] [Google Scholar]
- 14.Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010;41:2559–2567. doi: 10.1161/STROKEAHA.110.592071. [DOI] [PubMed] [Google Scholar]
- 15.The National institute of Neurological Disorders and Stroke (NINDS) rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 16.Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34:e109–e137. doi: 10.1161/01.STR.0000082721.62796.09. [DOI] [PubMed] [Google Scholar]
- 17.Keris V, Rudnicka S, Vorona V, Enina G, Tilgale B, Fricbergs J. Combined intraarterial/intravenous thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol. 2001;22:352–358. [PMC free article] [PubMed] [Google Scholar]
- 18.Pessin MS, Del Zoppo GJ, Estol CJ. Thrombolytic agents in the treatment of stroke. Clin Neuropharmacol. 1990;13:271–289. doi: 10.1097/00002826-199008000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Wolpert SM, Bruckmann H, Greenlee R, Wechsler L, Pessin MS, del Zoppo GJ The rt-PA Acute Stroke Study Group. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. AJNR Am J Neuroradiol. 1993;14:3–13. [PMC free article] [PubMed] [Google Scholar]
- 20.Khatri P, Wechsler LR, Broderick JP. Intracranial hemorrhage associated with revascularization therapies. Stroke. 2007;38:431–440. doi: 10.1161/01.STR.0000254524.23708.c9. [DOI] [PubMed] [Google Scholar]