Summary
Individuals with phenylketonuria (PKU) must follow a lifelong low-phenylalanine (Phe) diet to prevent neurological impairment. Compliance with the low-Phe diet is often poor owing to restriction in natural foods and the requirement for consumption of a Phe-free amino acid formula or medical food. Glycomacropeptide (GMP), a natural protein produced during cheese-making, is uniquely suited to a low-Phe diet because when isolated from cheese whey it contains minimal Phe (2.5–5 mg Phe/g protein). This paper reviews progress in evaluating the safety, acceptability and efficacy of GMP in the nutritional management of PKU. A variety of foods and beverages can be made with GMP to improve the taste, variety and convenience of the PKU diet. Sensory studies in individuals with PKU demonstrate that GMP foods are acceptable alternatives to amino acid medical foods. Studies in the PKU mouse model demonstrate that GMP supplemented with limiting indispensable amino acids provides a nutritionally adequate source of protein and improves the metabolic phenotype by reducing concentrations of Phe in plasma and brain. A case report in an adult with classical PKU who followed the GMP diet for 10 weeks at home indicates safety, acceptability of GMP food products, a 13–14% reduction in blood Phe levels (p<0.05) and improved distribution of dietary protein throughout the day compared with the amino acid diet. In summary, food products made with GMP that is supplemented with limiting indispensable amino acids provide a palatable alternative source of protein that may improve dietary compliance and metabolic control of PKU.
Introduction
Individuals with phenylketonuria (PKU) lack the enzyme phenylalanine (Phe) hydroxylase (PAH; EC 1.14.16.1) needed to metabolize the essential amino acid Phe to tyrosine. Without dietary management, they show an elevated level of Phe in blood that is toxic to the developing central nervous system. To prevent brain damage and cognitive impairment, they must follow a lifelong, highly restrictive diet that limits Phe intake to the minimum amount needed to support growth and protein turnover (NIH 2000). Individuals with classical PKU often tolerate less than 500 mg Phe per day, an amount that is less than 10% of the Phe consumed in a normal diet. The low-Phe or PKU diet requires two interrelated dietary practices (Bickel et al 1954). First, there is extensive restriction of natural foods because most natural foods contain protein containing 2.4–9% Phe by weight (US Department of Agriculture 2005). Second, supplementation with amino acids, usually in the form of a Phe-free formula or medical food, is required to provide adequate protein and energy owing to the restriction in natural foods. The diet is difficult to follow because of the off odour and bitter taste of the amino acid formulas as well as strong peer pressure to eat normal foods. Thus, it is not surprising that compliance with the PKU diet is poor during adolescence and adulthood, resulting in elevated Phe concentration in blood and brain and subsequent neuropsychological deterioration (Koch et al 2000, 2002; MacDonald 2000; Walter and White 2004). The risk associated with poor dietary compliance is especially high for pregnant women with PKU, whose infants show congenital anomalies when exposed to elevated maternal blood Phe concentration (Guttler et al 1999).
New dietary approaches are clearly needed to improve the palatability and variety of the low-Phe diet to enhance compliance, metabolic control and quality of life for individuals with PKU. Glycomacropeptide (GMP), a protein in cheese whey, is uniquely suited to the low-Phe diet because, in its pure form, it is the only known dietary protein that is naturally free of Phe. Thus, GMP could provide an alternative to amino acid formulas that currently provide the majority of protein in the PKU diet and pose the biggest obstacle to dietary compliance. Herein we review our progress in evaluating the safety, acceptability and efficacy of dietary GMP in the nutritional management of PKU. This paper discusses the ability to make palatable foods and beverages with GMP, studies in the PKU mouse model (McDonald et al 1990) that establish the nutritional adequacy and metabolic response to dietary GMP, and our experience in one adult with classical PKU who successfully adhered to a low-Phe diet that replaced all of the prescribed amino acid formula with GMP food products for 10 weeks at home.
Glycomacropeptide (GMP)
GMP is an abundant 64-amino-acid (AA) glycophosphopeptide produced during cheese-making when bovine kappa (κ)-casein is cleaved by chymosin into para-κ-casein, which remains with the curd, and GMP, which remains with the whey (Doultani et al 2003). GMP constitutes 15–20% of the protein in bovine cheese whey and is currently sold as a food ingredient. GMP has an excellent safety record as part of the human diet based on widespread supplementation of foods with whey protein and the use of whey-predominant infant formulas (Bruck et al 2006; Zhao et al 1986). Current research is addressing several interesting biological properties of GMP including prevention of viral and bacterial infections and suppression of appetite (Brody 2000; Keogh and Clifton 2008).
GMP has a unique profile of indispensable or essential amino acids compared with typical dietary proteins (Table 1). Pure GMP contains no Phe; however, isolation of GMP from cheese whey results in contamination with other whey proteins that contain Phe. Commercially available GMP contains 2.5–5.0 mg Phe per g of protein (http://www.arlafoodsingredients.com and http://www.DaviscoFoods.com). Concentrations of the indispensable large neutral amino acids (LNAA) isoleucine and threonine are 2- to 3-fold greater in GMP compared with other dietary proteins (Etzel 2004). GMP contains limiting amounts of four indispensable amino acids for individuals with PKU: histidine, leucine, tryptophan and tyrosine (IOM 2002). Thus, GMP food products supplemented with limiting indispensable amino acids, vitamins and minerals, i.e. GMP medical foods, are ideally suited to the PKU diet as an alternative to the Phe-free amino-acid medical foods currently required to control Phe levels in individuals with PKU.
Table 1.
Profile of indispensable amino acids for the PKU diet in pure GMP and in a commercial purified GMP isolate compared with average dietary protein
| Amino acid (grams per 100 g) | Pure GMPa | Lacprodan cGMP-20b | Average proteinc |
|---|---|---|---|
| Histidine | 0.0 | 0.2 | 2.6 |
| Isoleucine | 11.9 | 9.2 | 4.8 |
| Leucine | 1.7 | 2.0 | 7.8 |
| Lysine | 5.8 | 5.1 | 8.2 |
| Methionine | 2.0 | 1.6 | 2.0 |
| Phenylalanine | 0.0 | 0.16 | 4.7 |
| Threonine | 16.7 | 14.5 | 5.5 |
| Tryptophan | 0.0 | 0.03 | 1.9 |
| Tyrosine | 0.0 | 0.05 | 5.2 |
| Valine | 8.9 | 7.6 | 6.2 |
| BCAAd | 22.5 | 18.8 | 18.8 |
Theoretical amino acid profile of pure GMP, adapted from Etzel (2004).
Arla Foods Ingredients, Denmark; Lacprodan cGMP-20 is a GMP isolate purified specifically for application in PKU nutrition (http://www.arlafoodsingredients.com).
The amino acid profile of a theoretical average protein was calculated from 207 proteins of known sequence; adapted from Klapper MH (1977) Biochem Biophys Res Commun 78: 1018–1024.
BCAA is the sum of leucine, isoleucine and valine.
The functional properties of GMP are suitable for making low-Phe foods and beverages. For example, GMP has good heat stability, is soluble in acid with an isoelectric point of 2.8, and forms gels or foams (Etzel 2004). We have developed food products made with GMP, including beverages in a variety of flavours, puddings and a cinnamon crunch bar (Table 2). These products provide approximately 5–10 g protein and 15–30 mg Phe per serving. Sensory analysis studies in individuals with PKU demonstrate that GMP food products are acceptable and palatable (Lim et al 2007). In particular, PKU subjects rated the appearance, odour, taste and overall acceptability of a GMP chocolate beverage as significantly more acceptable than those of a commercial Phe-free amino acid chocolate beverage (Lim et al 2007). Low-Phe menus that incorporate GMP foods can easily be designed to replace at least one-half of the required amino acid formula for individuals with PKU of school age and older. GMP food products are not intended for use during infancy as a replacement for low-Phe infant formula. We hypothesize that GMP food products will enhance acceptability of the low-Phe diet by improving taste, variety and convenience.
Table 2.
Nutritional composition of GMP food productsa
| Product | Serving size | Energy [kJ (kcal)] | Protein (g) | Phe (mg) |
|---|---|---|---|---|
| Orange sports drink | 340 g (12oz) | 419 (100) | 12 | 33 |
| Chocolate beverage | 227 g (8oz) | 628 (150) | 10 | 33 |
| Caramel beverage | 227 g (8oz) | 670 (160) | 10 | 26 |
| Strawberrry pudding | 114 g (1/2 cup) | 921 (220) | 5 | 13 |
| Chocolate pudding | 114 g (1/2 cup) | 921 (220) | 5 | 21 |
| Ranch dressing | 45 g (1.5 oz) | 419 (100) | 5 | 15 |
| Cinnamon crunch bar | 55 g (1 bar) | 711 (170) | 5 | 14 |
GMP food products were developed in the Wisconsin Center for Dairy Research except for the ranch dressing and cinnamon crunch bar, which were developed by Cambrooke Foods of Boston.
PKU mice fed GMP compared with amino acids
Before initiating dietary studies in humans with PKU, we conducted feeding studies in the PKU mouse model of PAH deficiency, the Pahenu2 mouse (McDonald et al 1990). The goal of these studies was to evaluate the nutritional adequacy of GMP in growing mice and its impact on metabolic control of Phe levels in plasma and brain when GMP was fed as the sole source of dietary protein compared with the usual amino acid diet (Ney et al 2008). Similar growth and feed efficiency were observed in weanling wild-type and PKU mice fed the GMP diet supplemented with limiting amino acids compared with casein or amino acid diets for 6 weeks. This establishes that GMP provides a nutritionally adequate source of dietary protein for growing mice.
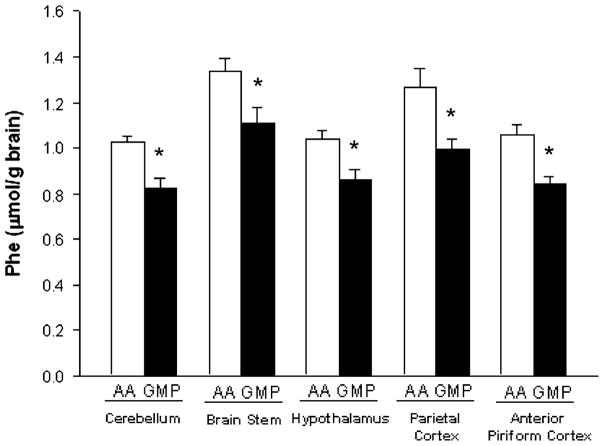
PKU mice fed the GMP diet showed improvement in the metabolic control of PKU. Significant decreases in the concentrations of Phe in plasma (11% decrease) and in five regions of brain (20% decrease) were noted in PKU mice fed the GMP diet compared with the amino acid diet with similar intake of Phe (Fig. 1) (Ney et al 2008). The decrease in concentration of Phe in brain is the most striking example of how GMP improves the metabolic control of PKU because the concentration of Phe in brain is the strongest correlate of mental impairment in individuals with PKU (Donlon et al 2007). Consistent with the unique amino acid profile of GMP, Table 1, increases in the concentrations of the LNAA, isoleucine, threonine and valine (40–200% increases), were noted in both plasma and brain with ingestion of GMP. The LNAA share a common transporter across the blood brain barrier and intestinal mucosa and compete with one another for transport in the brain and gut (Hidalgo and Borchardt 1990; Pardridge 1998). The most likely explanation for the reduced concentrations of Phe in the brain of PKU mice is that elevated plasma levels of LNAA with ingestion of GMP competitively inhibit Phe transport across the blood brain barrier via the LNAA carrier protein (Ney et al 2008). Supplementation with commercial preparations of LNAA has been noted to reduce brain and circulating levels of Phe in PKU mice (Matalon et al 2003, 2006) and to reduce brain Phe levels in PKU adults off diet as measured by magnetic resonance spectroscopy (Pietz et al 1999; Moats et al 2003). These data suggest that GMP provides a natural food source of LNAA that reduces the concentrations of Phe in plasma and brain of PKU mice and may have a similar benefit in humans with PKU.
Fig. 1.
The concentration of Phe in five sections of brain—cerebellum, brain stem, hypothalamus, parietal cortex, and anterior piriform cortex—of PKU mice fed the glycomacropeptide (GMP) or amino acid (AA) diet for 47 days. Values are means±SEM; n = 8. *Different from the AA diet, p ≤ 0.001. This figure was previously published by Ney et al (2008) and is reproduced with permission of the copyright owner, American Society for Nutrition
Case report of response to GMP diet
Approval was granted by the Health Sciences Institutional Review Board, University of Wisconsin-Madison to conduct an outpatient study in subjects with PKU to evaluate the safety and acceptability of dietary GMP. A 29-year-old male PKU subject with a genotype of R261Q and R408W was studied. The subject adhered to the low-Phe diet from birth through 12 years but was off diet during adolescence, which resulted in the development of spastic quadriparesis and a seizure disorder that was treated with standard anticonvulsant therapy. The subject completed a 15-week study comparing GMP with his usual prescribed amino acid formula (Phenylade and Amino Acid Blend; Applied Nutrition, Cedar Knolls, NJ, USA) as the primary source of dietary protein. The protocol consisted of a diet in which he consumed his usual amino acid formula for the first 3 weeks and the last 2 weeks of the study. During the middle 10 weeks of the study, GMP food products chosen by the subject replaced all of the amino acid formula and included: GMP orange sports beverage (28 oz/day; 28 g protein), GMP pudding (1.5 cups/day; 15 g protein) and GMP snack bar (1 bar/day; 5 g protein).
For six weeks of the study, weighed portions of food with precisely controlled Phe content were sent to the subject’s home. The Phe content of the diets was determined by analysis of selected foods for amino acid content and calculation of Phe content for the remaining foods matched in quantity and packing lot in both diets (US Department of Agriculture 2005). For the remaining 9 weeks of the study, the subject purchased and weighed his own food using menus planned with the metabolic dietician. Although Phe intake was well-controlled for 15 weeks, the results for Phe concentrations in blood and plasma presented here are based on the 6 weeks that food was provided to the subject.
The macronutrient profile provided by the amino acid and GMP diets was constant and included: 10 880–11 300 kJ/day (2600–2700 kcal/day), 10–11% energy from protein (0.84 g protein/kg), 24–26% energy from fat, and 63–66% energy from carbohydrate. The subject maintained a body weight of 87 kg during the study. The daily Phe content was 1100 mg Phe for 4 weeks and 1180 mg Phe for 2 weeks; this provided approximately 13 mg Phe per kg of body weight. The amino acid formula and GMP food products each provided 0.6 g protein per kg body weight. The GMP food products were supplemented to provide 130%, or 150% for tyrosine, of the amino acid scoring pattern for a complete protein for the following limiting amino acids, expressed as mg amino acid per g GMP protein (IOM 2002): histidine, 23; leucine, 72; tryptophan, 9; and tyrosine, 71. A multivitamin/mineral supplement, a calcium/phosphorus supplement and 500 mg of L-tyrosine twice a day were taken with the GMP diet to ensure intakes similar to those provided by the amino acid formula.
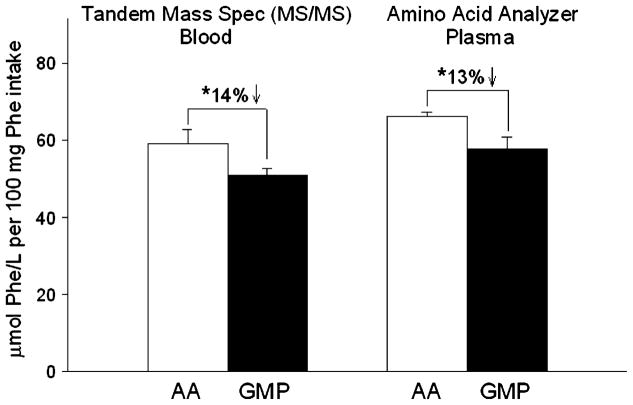
Blood samples were obtained after an overnight fast and prior to breakfast for determination of Phe concentration using one of two analytical methods known to give different values (Gregory et al 2007). Tandem mass spectroscopy (MS/MS) was used for analysis of Phe concentrations in blood spots collected on filter paper by the subject between 09:00 and 09:30 (Rashed et al 1995) and a Beckman 6300 amino acid analyser was used for analysis of the plasma amino acid profile obtained by venepuncture in a local clinic between 12:00 and 12:30 (Slocum and Cummings 1991). Statistical differences in blood and plasma amino acid concentrations for the amino acid and GMP dietary periods were evaluated by t-test with the assumption that the amino acid measurements were independent over time; p < 0.05 was considered significant. When expressed relative to 100 mg of Phe intake based on provision of meals with known Phe content, mean fasting plasma and blood Phe concentrations were significantly reduced by 13–14% with consumption of the GMP diet compared with the amino acid diet (Fig. 2). The absolute concentration of Phe in plasma was reduced by approximately 10% (from 736 to 667 μmol/L) with consumption of the GMP diet compared with the amino acid diet (Table 3). Plasma tyrosine concentration was not significantly different with the GMP and amino acid diets. No adverse effects were noted with consumption of the GMP diet based on physical examinations and the results of chemistry panel analyses which included electrolytes, albumin, prealbumin, and liver function tests.
Fig. 2.
Mean Phe concentrations obtained after an overnight fast before breakfast from a single PKU subject fed an amino acid (AA) or glycomacropeptide (GMP) diet for 15 weeks at home. Data are shown for 6 weeks of the 15-week study period when only foods with known Phe content were provided to the subject: weeks 3 and 15 (AA diet) and weeks 4, 7, 11 and 13 (GMP diet). Phe concentrations in blood and plasma were corrected for Phe intake and expressed as μmol Phe/L per 100 mg Phe intake. Phe concentration was determined using one of two methods, blood spot collection analysed with tandem mass spectroscopy (MS/MS) and measurement of plasma Phe with an AA analyser. Values are means±SE; AA diet (n = 4 plasma Phe and n = 4 blood Phe), GMP diet (n = 4 plasma Phe and n = 8 blood Phe). *Different from the AA diet, p < 0.05
Table 3.
Fasting concentrations of amino acids in plasma with ingestion of the amino acid diet compared to the GMP diet in a single PKU subjecta
| Amino acid | Concentration (μmol/L)
|
||
|---|---|---|---|
| Amino acid diet | GMP diet | Normal range | |
| Alanine | 296 ± 26 | 331 ± 5 | 177–583 |
| Arginine | 58 ± 2 | 62 ± 3 | 15–128 |
| Citrulline | 26 ± 2 | 48 ± 7* | 12–55 |
| Cystine | 31 ± 1 | 42 ± 5 | 5–82 |
| Glutamate | 46 ± 10 | 53 ± 7 | 10–131 |
| Glutamine | 698 ± 22 | 858 ± 16** | 205–756 |
| Glycine | 428 ± 7 | 428 ± 22 | 151–490 |
| Histidine | 69 ± 3 | 75 ± 2 | 41–125 |
| Isoleucine | 42 ± 3 | 69 ± 1** | 30–108 |
| Leucine | 92 ± 3 | 91 ± 3 | 72–201 |
| Lysine | 189 ± 8 | 201 ± 5 | 48–284 |
| Methionine | 19 ± 1 | 19 ± 3 | 10–42 |
| Ornithine | 61 ± 7 | 51 ± 6 | 48–195 |
| Phenylalanine | 736 ± 13 | 667 ± 24b | 35–85 |
| Proline | 153 ± 7 | 214 ± 13** | 97–329 |
| Serine | 95 ± 1 | 88 ± 8 | 58–181 |
| Taurine | 65 ± 6 | 59 ± 13 | 54–210 |
| Threonine | 95 ± 4 | 246 ± 12** | 60–225 |
| Tryptophan | 33 ± 2 | 35 ± 2 | 10–140 |
| Tyrosine | 53 ± 5 | 45 ± 6 | 34–112 |
| Valine | 241 ± 15 | 275 ± 14 | 119–336 |
| BCAAc | 374 ± 17 | 435 ± 15* | 221–645 |
, **Different from the AA diet,
p<0.05,
p<0.01.
Values are means±SE, n=4; blood samples were obtained after an overnight fast and prior to breakfast between 12:00 and 12:30 on different days distributed across the 5 weeks of the amino acid diet and the 10 weeks of the GMP diet.
p=0.073.
BCAA=sum of leucine, isoleucine, and valine.
Consistent with the amino acid profile of GMP (Table 1) and studies in the PKU mouse (Ney et al 2008), significant increases in plasma concentrations of the LNAA were noted with ingestion of the GMP diet compared with the amino acid diet (Table 3). Threonine increased 2.6-fold, isoleucine increased 1.7-fold, and the sum of the branched-chain amino acids increased 16% with the GMP diet. Interestingly, this subject was previously given a supplementation trial with a mixture of indispensable LNAA (PreKUnil; NiLab, Korsoer, Denmark), but this was stopped because his seizures became worse. The LNAA preparation contained a larger proportion of amino acids from tyrosine and tryptophan and proportionately less from threonine and the branched-chain amino acids than GMP, which contains approximately 80% of indispensable amino acid content from a combination of threonine and the branched-chain amino acids. Thus, GMP appears to provide a safe dietary source of LNAA for this subject. Plasma concentration of proline increased 40% with the GMP diet in association with a 2-fold increase in proline ingestion with GMP compared with the amino acid formula. There was a small increase in plasma concentration of glutamine and citrulline with the GMP diet compared with the amino acid diet that was not associated with a change in liver function tests. Blood ammonia levels were not determined but will be included in future studies.
Overall, the subject enjoyed the GMP diet and reported that he felt more alert with that diet than with his usual amino acid diet. Because the subject enjoyed the GMP food products, he was more inclined to distribute them throughout the day. He consumed GMP food products approximately three times per day compared with once per day for the amino acid formula. It is well known that spacing the amino acid medical foods for PKU throughout the day lowers blood Phe levels owing to improved utilization of amino acids for protein synthesis (Harper et al 1970; MacDonald et al 2003, 2004). Thus, one explanation for the reduced blood Phe levels with consumption of GMP is improved protein synthesis due to consumption of a sufficient amount of high-quality protein throughout the day. Alternatively, the greater intake of LNAA with GMP may have contributed to the decrease in plasma Phe levels (Matalon et al 2007; Schindeler et al 2007), particularly the high intake of threonine (~70 mg per kg per day). A study in 12 subjects with hyperphenylalaninaemia and constant Phe intake showed a significant 26% decrease in plasma Phe level with oral supplementation of 50 mg threonine per kg per day for 8 weeks (Sanjurjo et al 2003).
Summary
Compliance with the highly restrictive, low-Phe diet required for the management of PKU remains poor during adolescence and adulthood, resulting in elevated blood Phe levels, neuropsychological deterioration, and the tragic consequences of maternal PKU. Dietary GMP, an abundant food ingredient naturally low in Phe content, provides an innovative approach to improving the nutritional management of PKU. Our studies indicate that incorporation of low-Phe foods and beverages made with GMP into the PKU diet improves the taste, variety and convenience of the diet. A more tasty and versatile low-Phe diet may lead to improved dietary compliance, metabolic control and ultimately quality of life for individuals with PKU. Studies in the PKU mouse model demonstrate that ingestion of GMP lowers Phe concentrations in blood, and to a greater extent in brain tissue, possibly through competitive inhibition of Phe transport across the blood–brain barrier due to the naturally occurring high concentration of LNAA in GMP. Future research is needed to evaluate the long-term safety and efficacy of GMP in the nutritional management of PKU.
Acknowledgments
This work was supported by the Mid Atlantic Connection for PKU and Allied Disorders, Michaux Family Foundation, Robert Draper Technology Innovation Fund and the USDA Cooperative State Research, Education and Extension Service, project WISO1084, University of Wisconsin-Madison; and by NIH R03-DK-071534 and P30-HD-03352. In addition, the authors acknowledge the assistance of Phillip Williams, Waisman Center Biochemical Genetics Laboratory, for conducting the plasma amino acid analyses; Kimberlee J. Burrington, Coordinator, Dairy Ingredients Applications Group, Wisconsin Center for Dairy Research for her support in developing the GMP food products; and Xiaowen Liu for assistance with statistical analysis. We also acknowledge the GMP Task Force for initially recognizing the potential contribution of GMP to the nutritional management of PKU and facilitating this research. Members of the Task Force include two whey-producing companies, Davisco Foods of Minnesota and Grande Cheese Co. of Wisconsin, and two companies that distribute medical foods for the PKU market, Cambrooke Foods of Boston and Applied Nutrition of New Jersey. Membership also includes faculty and staff of the University of Wisconsin-Madison, parents of children with PKU, and an adult with PKU.
Abbreviations
- AA
amino acid
- GMP
glycomacropeptide
- LNAA
large neutral amino acids
- MS/MS
tandem mass spectroscopy
- PAH
phenylalanine hydroxylase
- Phe
phenylalanine
- PKU
phenylketonuria
Footnotes
Competing interests: None declared
References to electronic databases: Phenylalanine hydroxylase: EC 1.14.16.1.
Presented at the International Conference on Tetrahydrobiopterin, PKU, and NOS, 23–28 March 2008, St Moritz, Champfér, Switzerland
Contributor Information
D. M. Ney, Email: ney@nutrisci.wisc.edu, Department of Nutritional Sciences, University of Wisconsin, 1415 Linden Drive, Madison, WI 53706, USA
S. T. Gleason, Department of Nutritional Sciences, University of Wisconsin, 1415 Linden Drive, Madison, WI 53706, USA
S. C. van Calcar, Waisman Center, University of Wisconsin, Madison, Wisconsin, USA
E. L. MacLeod, Department of Nutritional Sciences, University of Wisconsin, 1415 Linden Drive, Madison, WI 53706, USA
K. L. Nelson, Wisconsin Center for Dairy Research, University of Wisconsin, Madison, Wisconsin, USA
M. R. Etzel, Department of Food Science, University of Wisconsin, Madison, Wisconsin, USA
G. M. Rice, Waisman Center, University of Wisconsin, Madison, Wisconsin, USA
J. A. Wolff, Waisman Center, University of Wisconsin, Madison, Wisconsin, USA
References
- Bickel H, Gerrard J, Hickmans EM. The influence of phenylalanine intake on the chemistry and behavior of a phenylketonuric child. Acta Paediatr. 1954;43:64–77. doi: 10.1111/j.1651-2227.1954.tb04000.x. [DOI] [PubMed] [Google Scholar]
- Brody EP. Biological activities of bovine glycomacropeptide. Br J Nutr. 2000;84(Supplement 1):S39–S46. doi: 10.1017/s0007114500002233. [DOI] [PubMed] [Google Scholar]
- Bruck WM, Redgrave M, Tuohy KM, et al. Effects of bovine alpha-lactalbumin and casein glycomacropeptide-enriched infant formulae on faecal microbiota in healthy term infants. J Pediatr Gastroenterol Nutr. 2006;43:673–679. doi: 10.1097/01.mpg.0000232019.79025.8f. [DOI] [PubMed] [Google Scholar]
- Donlon J, Levy H, Scriver C. Chapter 77: Hyperphenyla-laninemia: phenylalanine hydroxylase deficiency. In: Scriver C, Beaudet A, Sly W, Valle D, editors. Metabolic and Molecular Basis of Inherited Disease. New York: McGraw-Hill; 2007. http://www.ommbid.com. [Google Scholar]
- Doultani S, Turhan KN, Etzel MR. Whey protein isolate and glycomacropeptide recovery from whey using ion exchange chromatography. J Food Sci. 2003;68:1389–1395. doi: 10.1111/j.1365-2621.2003.tb09655.x. [DOI] [Google Scholar]
- Etzel MR. Manufacture and use of dairy protein fractions. J Nutr. 2004;134:996S–1002S. doi: 10.1093/jn/134.4.996S. [DOI] [PubMed] [Google Scholar]
- Gregory CO, Yu C, Singh RH. Blood phenylalanine monitoring for dietary compliance among patients with phenylketonuria: comparison of methods. Genet Med. 2007;9:761–765. doi: 10.1097/GIM.0b013e318159a355. [DOI] [PubMed] [Google Scholar]
- Guttler F, Azen C, Guldberg P, et al. Relationship among genotype, biochemical phenotype, and cognitive performance in females with phenylalanine hydroxylase deficiency: report from the Maternal Phenylketonuria Collaborative Study. Pediatrics. 1999;104:258–262. doi: 10.1542/peds.104.2.258. [DOI] [PubMed] [Google Scholar]
- Harper AE, Benevenga NJ, Wohlhueter RM. Effects of ingestion of disproportionate amounts of amino acids. Physiol Rev. 1970;50:428–439. doi: 10.1152/physrev.1970.50.3.428. [DOI] [PubMed] [Google Scholar]
- Hidalgo IJ, Borchardt RT. Transport of a large neutral amino acid (phenylalanine) in a human intestinal epithelial cell line: Caco-2. Biochim Biophys Acta. 1990;1028:25–30. doi: 10.1016/0005-2736(90)90261-L. [DOI] [PubMed] [Google Scholar]
- IOM. Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Protein and Amino Acids (Macronutrients) Washington, DC: National Academy Press; 2002. [Google Scholar]
- Keogh JB, Clifton P. The effect of meal replacements high in glycomacropeptide on weight loss and markers of cardiovascular disease risk. Am J Clin Nutr. 2008;87:1602–1605. doi: 10.1093/ajcn/87.6.1602. [DOI] [PubMed] [Google Scholar]
- Koch R, Moats R, Guttler F, Guldberg P, Nelson M., Jr Blood–brain phenylalanine relationships in persons with phenylketonuria. Pediatrics. 2000;106:1093–1096. doi: 10.1542/peds. 106.5.1093. [DOI] [PubMed] [Google Scholar]
- Koch R, Burton B, Hoganson G, et al. Phenylketonuria in adulthood: a collaborative study. J Inherit Metab Dis. 2002;25:333–346. doi: 10.1023/A:1020158631102. [DOI] [PubMed] [Google Scholar]
- Lim K, van Calcar SC, Nelson KL, Gleason ST, Ney DM. Acceptable low-phenylalanine foods and beverages can be made with glycomacropeptide from cheese whey for individuals with PKU. Mol Genet Metab. 2007;92:176–178. doi: 10.1016/j.ymgme.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald A. Diet and compliance in phenylketonuria. Eur J Pediatr. 2000;159(Supplement 2):S136–S141. doi: 10.1007/PL00014375. [DOI] [PubMed] [Google Scholar]
- MacDonald A, Daly A, Davies P, et al. Protein substitutes for PKU: what’s new? J Inherit Metab Dis. 2004;27:363–371. doi: 10.1023/B:BOLI.0000031099.79046.65. [DOI] [PubMed] [Google Scholar]
- MacDonald A, Rylance G, Davies P, Asplin D, Hall SK, Booth IW. Administration of protein substitute and quality of control in phenylketonuria: a randomized study. J Inherit Metab Dis. 2003;26:319–326. doi: 10.1023/A:1025186217369. [DOI] [PubMed] [Google Scholar]
- Matalon R, Surendran S, Matalon KM, et al. Future role of large neutral amino acids in transport of phenylalanine into the brain. Pediatrics. 2003;112:1570–1574. [PubMed] [Google Scholar]
- Matalon R, Michals-Matalon K, Bhatia G, et al. Large neutral amino acids in the treatment of phenylketonuria (PKU) J Inherit Metab Dis. 2006;29:732–738. doi: 10.1007/s10545-006-0395-8. [DOI] [PubMed] [Google Scholar]
- Matalon R, Michals-Matalon K, Bhatia G, et al. Double blind placebo control trial of large neutral amino acids in treatment of PKU: effect on blood phenylalanine. J Inherit Metab Dis. 2007;30:153–158. doi: 10.1007/s10545-007-0556-4. [DOI] [PubMed] [Google Scholar]
- McDonald JD, Bode VC, Dove WF, Shedlovsky A. Pahhph-5: a mouse mutant deficient in phenylalanine hydroxylase. Proc Natl Acad Sci U S A. 1990;87:1965–1967. doi: 10.1073/pnas.87.5.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moats RA, Moseley KD, Koch R, Nelson M., Jr Brain phenylalanine concentrations in phenylketonuria: research and treatment of adults. Pediatrics. 2003;112:1575–1579. [PubMed] [Google Scholar]
- Ney DM, Hull AK, van Calcar SC, Liu X, Etzel MR. Dietary glycomacropeptide supports growth and reduces the concentrations of phenylalanine in plasma and brain in a murine model of phenylketonuria. J Nutr. 2008;138:316–322. doi: 10.1093/jn/138.2.316. [DOI] [PubMed] [Google Scholar]
- NIH . Phenylketonuria (PKU): screening and management. NIH Consensus Statement. 2000;17:1–33. [PubMed] [Google Scholar]
- Pardridge WM. Blood–brain barrier carrier-mediated transport and brain metabolism of amino acids. Neurochem Res. 1998;23:635–644. doi: 10.1023/A:1022482604276. [DOI] [PubMed] [Google Scholar]
- Pietz J, Kreis R, Rupp A, et al. Large neutral amino acids block phenylalanine transport into brain tissue in patients with phenylketonuria. J Clin Invest. 1999;103:1169–1178. doi: 10.1172/JCI5017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashed MS, Ozand PT, Bucknall MP, Little D. Diagnosis of inborn errors of metabolism from blood spots by acylcarnitines and amino acids profiling using automated electrospray tandem mass spectrometry. Pediatr Res. 1995;38:324–331. doi: 10.1203/00006450-199509000-00009. [DOI] [PubMed] [Google Scholar]
- Sanjurjo P, Aldamiz L, Georgi G, Jelinek J, Ruiz JI, Boehm G. Dietary threonine reduces plasma phenylalanine levels in patients with hyperphenylalaninemia. J Pediatr Gastroenterol Nutr. 2003;36:23–26. doi: 10.1097/00005176-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Schindeler S, Ghosh-Jerath S, Thompson S, et al. The effects of large neutral amino acid supplements in PKU: an MRS and neuropsychological study. Mol Genet Metab. 2007;91:48–54. doi: 10.1016/j.ymgme.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Slocum RH, Cummings JG. Amino acid anaylsis of physiological samples. In: Hommes FA, editor. Techniques in Diagnostic Human Biochemical Genetics: A Laboratory Manual. New York: Wiley-Liss; 1991. pp. 87–126. [Google Scholar]
- US Department of Agriculture ARS. USDA Nutrient Database for Standard Reference, Release 18. 2005 http://www.nal.usda.gov/fnic/foodcomp.
- Walter JH, White FJ. Blood phenylalanine control in adolescents with phenylketonuria. Int J Adolesc Med Health. 2004;16:41–45. doi: 10.1515/ijamh.2004.16.1.41. [DOI] [PubMed] [Google Scholar]
- Zhao XH, Wen ZM, Meredith CN, Matthews DE, Bier DM, Young VR. Threonine kinetics at graded threonine intakes in young men. Am J Clin Nutr. 1986;43:795–802. doi: 10.1093/ajcn/43.5.795. [DOI] [PubMed] [Google Scholar]