Abstract
Purpose
To describe the early experience of analyzing variations and time trends in bladder volume of the rectal cancer patients who received bladder ultrasound scan.
Materials and Methods
We identified 20 consecutive rectal cancer patients who received whole pelvic radiotherapy (RT) and bladder ultrasound scan between February and April 2012. Before simulation and during the entire course of treatment, patients were scanned with portable automated ultrasonic bladder scanner, 5 times consecutively, and the median value was reported. Then a radiation oncologist contoured the bladder inner wall shown on simulation computed tomography (CT) and calculated its volume.
Results
Before simulation, the median bladder volume measured using simulation CT and bladder ultrasound scan was 427 mL (range, 74 to 1,172 mL) and 417 mL (range, 147 to 1,245 mL), respectively. There was strong linear correlation (R = 0.93, p < 0.001) between the two results. During the course of treatment, there were wide variations in the bladder volume and every time, measurements were below the baseline with statistical significance (12/16). At 6 weeks after RT, the median volume was reduced by 59.3% to 175 mL. Compared to the baseline, bladder volume was reduced by 38% or 161 mL on average every week for 6 weeks.
Conclusion
To our knowledge, this study is the first to prove that there are bladder volume variations and a reduction in bladder volume in rectal cancer patients. Moreover, our results will serve as the basis for implementation of bladder training to patients receiving RT with full bladder.
Keywords: Rectal neoplasms, Urinary bladder, Ultrasonography, Observer variation, Radiotherapy
Introduction
Preoperative chemoradiotherapy (CRT) has been established as a current standard treatment on locally advanced rectal cancer since several randomized controlled trials have confirmed that it improves local control and increases sphincter preservation rate [1-4]. Even after an upfront surgery of localized rectal cancer, for tumors with adverse pathological features (T3-4 or N+ tumors), adjuvant CRT is known to improve oncologic outcome [5,6]. For rectal cancer patients, CRT on pelvic area is generally tolerable on most of the patients, but 8-40% of patients are reported to have acute toxicity (grade ≥3) and 24% of patients with late toxicity [1,7,8].
It is known that the risk of gastrointestinal (GI) complications is closely related to irradiated small bowel volume and dose within the radiation (RT) field [9]. There have been many studies to minimize irradiated small bowel volume and dose. Drzymara et al. [10] and Nijkamp et al. [11] reported that prone position was more effective than supine position in sparing small bowel. In the case of patients who are treated in prone position, using belly board or small bowel displacement device can move small bowel out of the RT field and, as a result, can lower the small bowel dose [12,13]. Therefore, in order to reduce GI complication risk in rectal cancer patients, our institution has been instructing all patients to maintain full bladder and treating them with belly board in prone position since 2009.
However, to date, no study on whether rectal cancer patients have been maintaining the same bladder volume during the 5 to 6 weeks of RT as they were during simulation has been published. Studies of bladder volume of cervix cancer and prostate cancer patients not only show wide inter-fraction variations in bladder volume during each RT but even a decrease in bladder volume during the course of treatment [14,15]. Therefore, in order to check bladder volume on a day by day basis just prior to RT, our institution introduced ultrasound bladder ultrasound scan in February 2011. The purpose of this study is to describe the early experience of analyzing variations and time trends in bladder volume of the 20 consecutive rectal cancer patients who received bladder ultrasound scan after the introduction of the device.
Materials and Methods
1. Study population
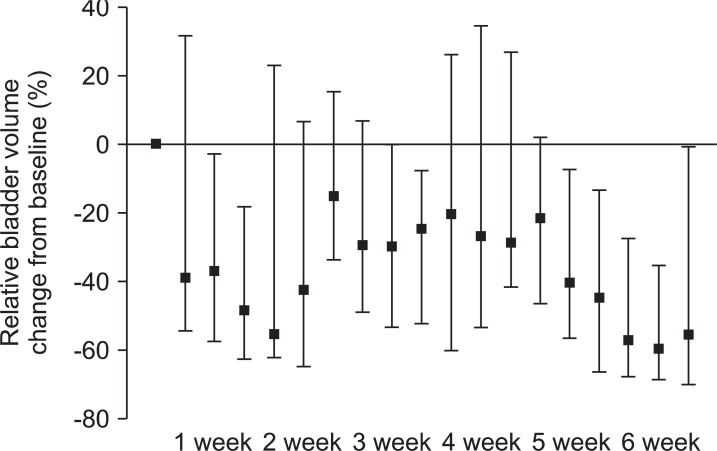
We identified 20 consecutive rectal cancer patients who received whole pelvic RT and bladder ultrasound scan between February 14 and April 15, 2012. The screening was performed after obtaining informed consent from all patients. Patients with the Eastern Cooperative Oncology Group (ECOG) performance status of 2 or higher, those who had functional disorder in their bladder, patients who underwent cystectomy, or those who showed strong aversion to retaining urine were excluded from bladder ultrasound scan. The clinical profiles of the 20 patients are shown in Table 1.
Table 1.
Clinical profiles of 20 patients
ECOG, the Eastern Cooperative Oncology Group; RT, radiotherapy.
2. Treatment
Fourteen patients (70%) received RT for preoperative aim and 6 patients (30%) as postoperative aim. All patients received 5-fluorouracil based concurrent chemotherapy plus RT. The former group comprised of patients with stage III mid-lower rectal cancer. One of the 6 patients in the latter group had stage I cancer and had received local excision before the CRT, while the other 5 patients had stage IIIB cancer and had undergone laparoscopy or robot assisted low anterior resection (LAR). Preoperative CRT patients received whole-pelvic RT of 45 Gy followed by tumor bed boost of 5.4 Gy. On the other hand, Postoperative CRT patients only received whole-pelvic RT of 45 Gy, and additional boost of RT was given only according to their resection margin status.
3. Bladder volume evaluation
Patients were asked to drink unspecified volume of water because we thought there were wide variations of abilities in drinking water and retaining their urine. Instead, patients were instructed voluntarily at their first visit to regulate their volume of drinking water and time of retaining the urine so that the goal of the instructions was maintaining the similar desire to micturition before treatment. However, the patients were not forced to follow this protocol if they were not comfortable. During the simulation, patients were in prone position using bladder compression device and belly board designed by our institution. Details are included in previously reported paper [16]. Two trained doctors controlled the portable automated ultrasonic bladder scanner (Biocon-700; Mcube Technology, Seoul, Korea). Patients lied supine in a comfortable position. Then, scanner's probe was placed on the midline of abdomen, two fingers over the symphysis pubic bone and angled towards the bladder. A three-dimensional real-time image before scanning was displayed to operators in order to locate easily the bladder position for more accurate measurement. Before simulation computed tomography (CT), patients were scanned 5 times consecutively, and the median value was reported. Then a radiation oncologist contoured the bladder inner wall shown on simulation CT and calculated its volume. During the entire course of treatment, patients' bladder was scanned 3 days weekly (Monday, Wednesday, and Friday) just prior to the RT, and just as mentioned above, patients were scanned 5 times before reporting the median value. No additional planned instructions were provided to patients after full education at first visit. All measured volumes by bladder ultrasound scan were blinded to patients.
4. Data and statistical analysis
In order to assess the accuracy of bladder ultrasound scan, the bladder volumes contoured during the simulation CT and the baseline bladder volumes measured through the bladder ultrasound scan before the simulation CT were compared using Pearson correlation test. The bladder volumes measured during the RT and the baseline bladder volumes were compared using Wilcoxon signed rank test. Absolute and relative bladder volume changes (from the baseline) of all patients were also calculated each time. Then, using the median values of the measurements and interquartile range (IQR), a graph was drawn. It was defined statistically significant when p < 0.05 and SPSS ver. 20.0.0 (IBM, Armonk, NY, USA) was used.
Results
1. Measurement of bladder volume
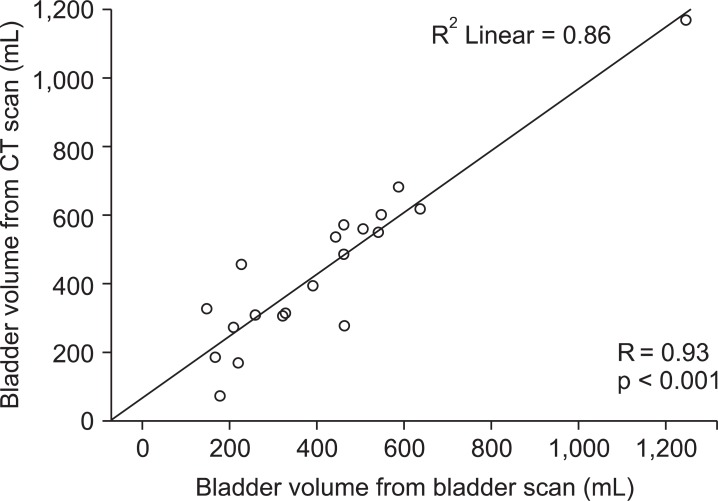
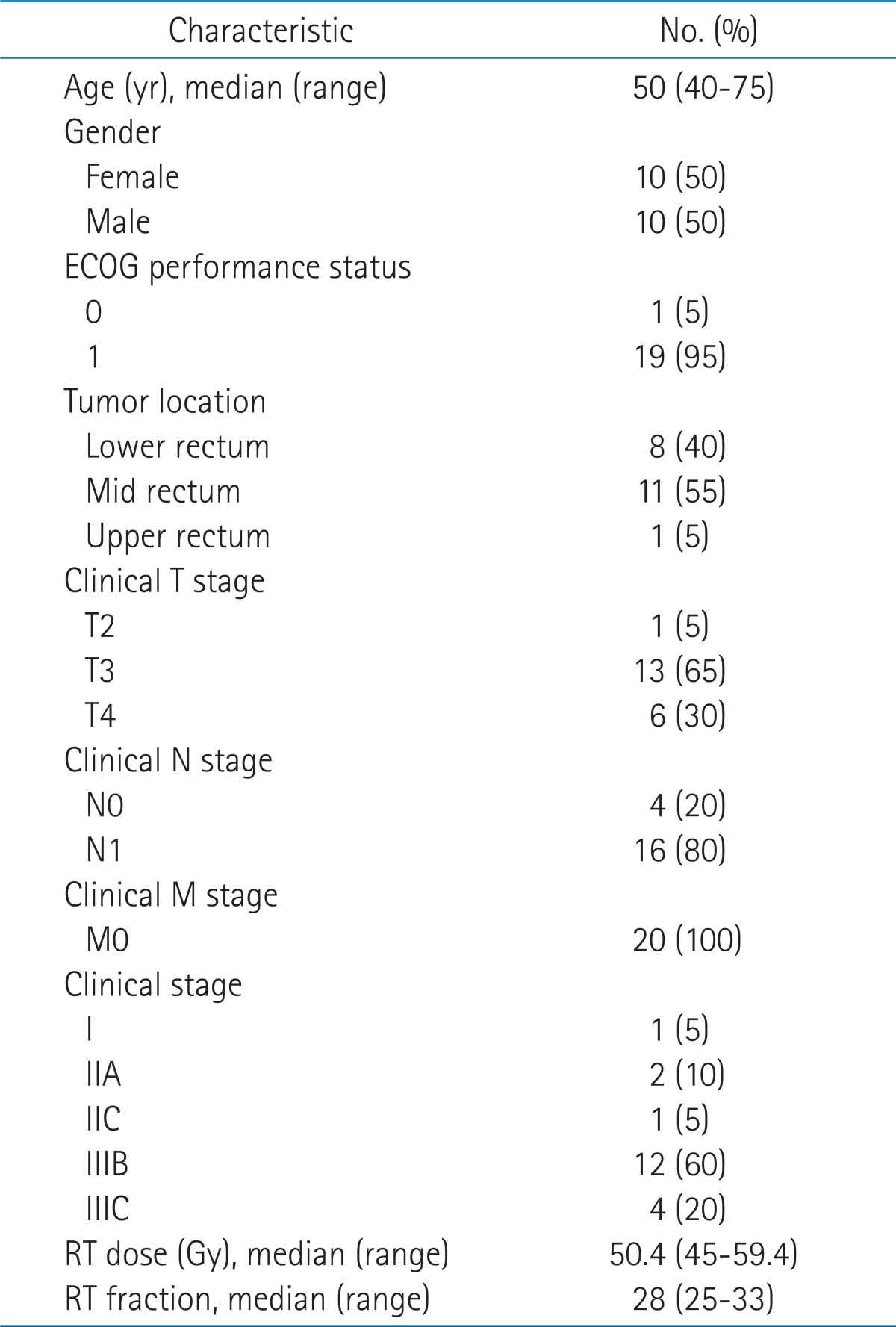
Twenty patients were scheduled to receive bladder ultrasound scans at a median number of 18 times (range, 15 to 19 times; 3 days a week according to the RT schedule) in total. Ninety percent of the scans were carried out as planned, and patients had scans at a median number of 16 times (range, 12 to 19 times) in total. The median bladder volume measured using simulation CT was 427 mL (IQR, 291 mL; range, 74 to 1,172 mL). The median volume measured using bladder ultrasound scan before the simulation CT on the same day was 417 mL (IQR, 222 mL; range, 147 to 1,245 mL). There was strong linear correlation (R = 0.93, p < 0.001; R2 = 0.86, p < 0.001) between the two results (Fig. 1). The bladder volume measurements and the number of patients are recorded in Table 2.
Fig. 1.
A Pearson correlation scatter plot for 20 patients between the two different bladder volume detection methods. CT, computed tomography.
Table 2.
Time trends of bladder volume from CT scans and bladder scans
IQR, interquartile range; CT, computed tomography; VCT, bladder volume measured from simulation CT scans; VB-SCAN, bladder volume scanned by bladder scan prior to simulation CT scans; Vx-x week, bladder volume scanned by bladder scan at post-RT x-x week.
2. Time trends of bladder volume
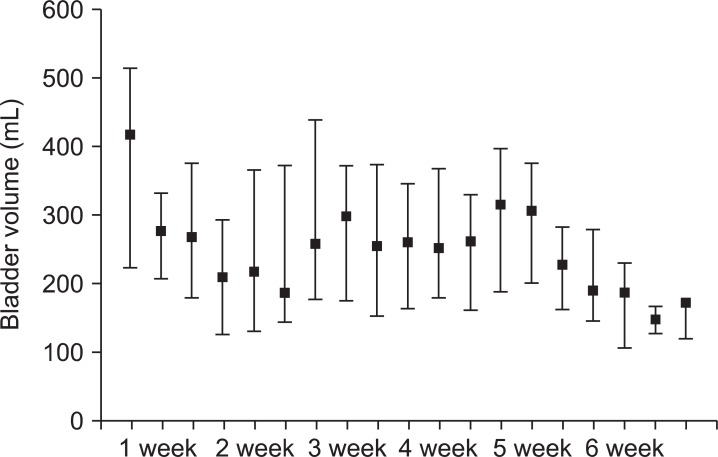
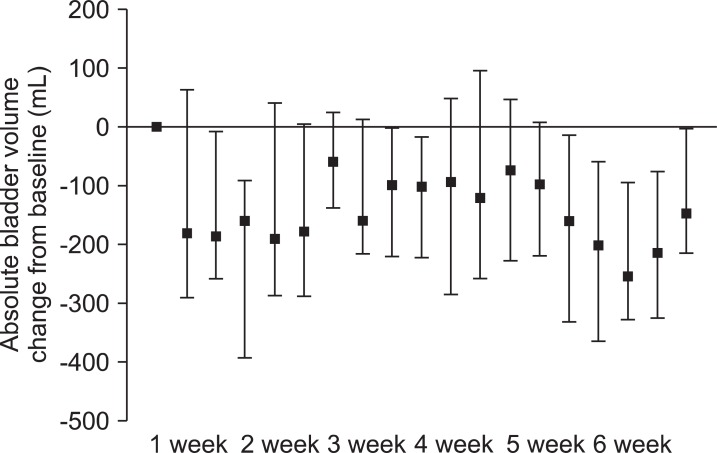
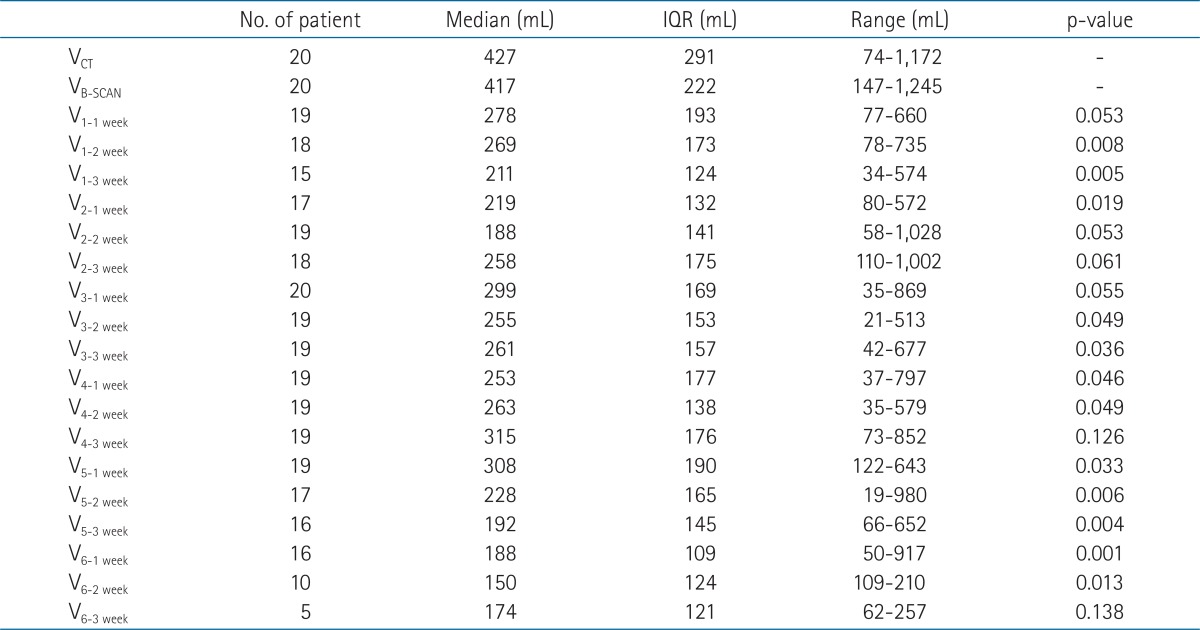
The time trends of bladder volume were depicted in Fig. 2. Measured volumes during RT were always below the baseline volume, and most were of statistical significance (12/16) or borderline significance (3/16). On the third day of the third week (3-3 weeks) after the RT, the median volume decreased by 38.9% to 261 mL (IQR, 157 mL), and at by the third day of the sixth week (6-3 weeks), it was reduced by 59.3% to 175 mL (IQR, 121 mL). The relative and absolute bladder volume changes from each patient's baseline values are displayed in Figs. 3 and 4. Compared to the baseline, bladder volume was reduced by 38% (standard deviation [SD], 14%) or 161 mL (SD, 53 mL) on average every week for 6 weeks. To see the intrapatient variation, we calculated overall mean and SD of each patient's standard deviation (mean ± SD, 155 ± 100 mL).
Fig. 2.
Bladder volume measured by bladder scan over the course of treatment. Error bars represent the median ± interquartile range.
Fig. 3.
Absolute bladder volume change from baseline over the course of treatment. Error bars represent the median ± interquartile range.
Fig. 4.
Relative bladder volume change from baseline over the course of treatment. Error bars represent the median ± interquartile range.
Discussion and Conclusion
This study demonstrated that during pelvic RT of rectal cancer patients with full bladder, there are wide variations in bladder volume as well as significant reduction in bladder volume from the baseline. As far as we are aware, this study is the first to analyze variations in bladder volume and time trend during RT in patients with rectal cancer.
There have been many studies on the accuracy of bladder ultrasound scan [15,17,18]. Ahmad et al. [15] used bladder phantom to prove that bladder volume measured with CT or bladder ultrasound scan agrees with real bladder volume. It also reported that the difference between measurements of 4 healthy volunteers' bladder volume before and after urination equaled to actual urination volume. Although this study also showed strong positive correlation (R = 0.89), there is a slight difference from other studies. This may be due to the time gap between CT scan and bladder ultrasound scan, which range from as little as a few minutes to as much as an hour. In order to minimize such error when evaluating the accuracy of bladder ultrasound scan, two bladder ultrasound scans (before and after CT scan) may be necessary.
With regards to prostate cancer, there have been many studies reported on bladder volume [11,14,18,19]. Nakamura et al. [14] reported that measurements of bladder volume during RT using megavoltage CT over the course of treatment showed 38% of mean volume reduction from the baseline at the end of treatment (p < 0.001). Other studies that used daily or weekly bladder ultrasound scans reported 16-50% of volume reduction from the baseline [6,11,18]. In the case of cervix cancer, Ahmad et al. [15] and other studies that used bladder ultrasound scan reported an average of 71% of volume reduction. In our study, there was 59% reduction, which is roughly consistent with the results from prostate cancer studies. We also observed the bladder volume was already decreased at the first week of treatment (median, 417 mL) when compared to those at the time of simulation as baseline (211 to 278 mL). The most plausible explanation is that the full bladder instruction at the first visit alone was not sufficient to maintain the patient's compliance until and though treatment (the interval between first visit and treatment start was generally one week).
That bladder volume is not reproducible and rather reduces every time means that RT dose on organ at risk could be higher than planned. Therefore, efforts to minimize the reduction of bladder volume are needed. Stam et al. [17] and O'Doherty et al. [18] showed that providing labor-intensive education to patients could help maintain bladder volume consistency. O'Doherty et al. [18] instructed 41 patients to drink 350 mL of water and retain their urine for an hour and a half, and then asked them about their bladder fullness. Only 25 of them were given patient information sheet, and the bladder volumes of the two groups were compared. Patient information sheet was developed by a multidisciplinary team, and it contained the information regarding the importance of full bladder, how to achieve a comfortably full bladder successfully, and how to manage if the patient could not hold the full bladder. Patients without the information sheet showed a significant reduction in bladder volume (mean, 362 mL → 251 mL), but the other group maintained consistency (mean, 286 mL → 312 mL). Stam et al. [17] provided bio-feedback to only 18 of 34 patients and not for the remaining 16 patients, then compared to two groups. To elaborate, if daily measurements of bladder volume were below 80% or above 120% of the baseline bladder volume, patients were given negative feedback, and if the measurements were between 80% and 120%, they were given positive feedback (drink the same amount of water the next day). The group with bio-feedback showed 7% improvement. Our institution is also planning to develop ways to educate and perform prospective evaluations on patients in order to raise rectal cancer patients' compliance to full bladder instruction during the course of treatment.
There are several limitations to this study; therefore, interpreting the results requires some caution. First of all, although the study was a retrospective non-interventive observation study, there could have been unexpected bio-feedback in the process of bladder ultrasound scan, which could have affected the result. Secondly, this study included not only patients who underwent preoperative RT but also 6 patients who received postoperative RT. Patients who had underwent an operation could have had bowel adhesion and showed different complications after receiving RT, which could have affected the result as well. Even so, this study is the first to prove that there are bladder volume variations and a reduction in bladder volume in not only prostate and cervix cancer but also rectal cancer patients. Moreover, our results will serve as the basis for implementation of bladder training to patients receiving RT with full bladder.
Our institution plans to continue studying in order to develop the optimal bladder ultrasound scan schedule and patient education method, and ultimately find effective intervention methods by identifying patients with wide bladder volume variations or those at high risk of bladder volume reduction. Moreover, compared to three-dimensional conformal RT, further study of bladder filling will be necessary for the pelvic intensity modulated RT that requires longer treatment time and different dose distribution to the organ at risks.
In conclusion, there were wide variations in bladder volume during treatment between rectal cancer patients who received concurrent chemotherapy and those who were treated with pelvic RT. Moreover, there was significant reduction from the baseline volume. This study was able to measure the bladder volume in a non-invasive manner using ultrasound-bladder scanner.
Acknowledgments
Thanks to Wonmi Nam for her valuable help. This work was supported by Seoul Metropolitan Government, Seoul Business Agency (2012).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–1740. doi: 10.1056/NEJMoa040694. [DOI] [PubMed] [Google Scholar]
- 2.Peeters KC, Marijnen CA, Nagtegaal ID, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg. 2007;246:693–701. doi: 10.1097/01.sla.0000257358.56863.ce. [DOI] [PubMed] [Google Scholar]
- 3.Sebag-Montefiore D, Stephens RJ, Steele R, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373:811–820. doi: 10.1016/S0140-6736(09)60484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sauer R, Liersch T, Merkel S, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30:1926–1933. doi: 10.1200/JCO.2011.40.1836. [DOI] [PubMed] [Google Scholar]
- 5.Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet. 2001;358:1291–1304. doi: 10.1016/S0140-6736(01)06409-1. [DOI] [PubMed] [Google Scholar]
- 6.Douglass HO, Jr, Moertel CG, Mayer RJ, et al. Survival after postoperative combination treatment of rectal cancer. N Engl J Med. 1986;315:1294–1295. doi: 10.1056/NEJM198611133152014. [DOI] [PubMed] [Google Scholar]
- 7.Roh MS, Colangelo LH, O'Connell MJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol. 2009;27:5124–5130. doi: 10.1200/JCO.2009.22.0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerard JP, Conroy T, Bonnetain F, et al. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620–4625. doi: 10.1200/JCO.2006.06.7629. [DOI] [PubMed] [Google Scholar]
- 9.Kavanagh BD, Pan CC, Dawson LA, et al. Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S101–S107. doi: 10.1016/j.ijrobp.2009.05.071. [DOI] [PubMed] [Google Scholar]
- 10.Drzymala M, Hawkins MA, Henrys AJ, et al. The effect of treatment position, prone or supine, on dose-volume histograms for pelvic radiotherapy in patients with rectal cancer. Br J Radiol. 2009;82:321–327. doi: 10.1259/bjr/57848689. [DOI] [PubMed] [Google Scholar]
- 11.Nijkamp J, Doodeman B, Marijnen C, Vincent A, van Vliet-Vroegindeweij C. Bowel exposure in rectal cancer IMRT using prone, supine, or a belly board. Radiother Oncol. 2012;102:22–29. doi: 10.1016/j.radonc.2011.05.076. [DOI] [PubMed] [Google Scholar]
- 12.Kim TH, Chie EK, Kim DY, et al. Comparison of the belly board device method and the distended bladder method for reducing irradiated small bowel volumes in preoperative radiotherapy of rectal cancer patients. Int J Radiat Oncol Biol Phys. 2005;62:769–775. doi: 10.1016/j.ijrobp.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Park W, Huh SJ, Lee JE, et al. Variation of small bowel sparing with small bowel displacement system according to the physiological status of the bladder during radiotherapy for cervical cancer. Gynecol Oncol. 2005;99:645–651. doi: 10.1016/j.ygyno.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura N, Shikama N, Takahashi O, et al. Variability in bladder volumes of full bladders in definitive radiotherapy for cases of localized prostate cancer. Strahlenther Onkol. 2010;186:637–642. doi: 10.1007/s00066-010-2105-6. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad R, Hoogeman MS, Quint S, Mens JW, de Pree I, Heijmen BJ. Inter-fraction bladder filling variations and time trends for cervical cancer patients assessed with a portable 3-dimensional ultrasound bladder scanner. Radiother Oncol. 2008;89:172–179. doi: 10.1016/j.radonc.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Yoon HI, Chung Y, Kim JH, et al. The efficacy of the change in belly board aperture location by the addition of bladder compression device for radiotherapy of rectal cancer. J Korean Soc Ther Radiol Oncol. 2010;28:231–237. [Google Scholar]
- 17.Stam MR, van Lin EN, van der Vight LP, Kaanders JH, Visser AG. Bladder filling variation during radiation treatment of prostate cancer: can the use of a bladder ultrasound scanner and biofeedback optimize bladder filling? Int J Radiat Oncol Biol Phys. 2006;65:371–377. doi: 10.1016/j.ijrobp.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 18.O'Doherty UM, McNair HA, Norman AR, et al. Variability of bladder filling in patients receiving radical radiotherapy to the prostate. Radiother Oncol. 2006;79:335–340. doi: 10.1016/j.radonc.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Hynds S, McGarry CK, Mitchell DM, et al. Assessing the daily consistency of bladder filling using an ultrasonic Bladderscan device in men receiving radical conformal radiotherapy for prostate cancer. Br J Radiol. 2011;84:813–818. doi: 10.1259/bjr/50048151. [DOI] [PMC free article] [PubMed] [Google Scholar]