Abstract
Aim:
This study was conducted to evaluate the clinical reversal of dental fluorosis with various combinations of calcium, vitamin D3, and ascorbic acid, along with changes in levels of certain biochemical parameters concerned with dental fluorosis. The role of fluoride level of drinking water in the etiology of dental fluorosis and the prevalence of dental fluorosis in both dentitions and teeth were also assessed.
Materials and Methods:
A total number of 50 patients with clinical features of dental fluorosis without trauma and any adverse habits were selected. Of these, in 30 co-operative patients, estimation of water fluoride level and pretreatment and post-treatment serum and urine fluoride levels were done with ion selective electrode method. The selected 30 patients were divided into three groups, that is, group A, group B, and group C, and were given various combinations of medications like calcium with vitamin D3 supplements, ascorbic acid with vitamin D3 supplements, and chlorhexidine mouthwash (placebo) for three months, respectively. These 30 patients were assessed for any change in the clinical grading of dental fluorosis.
Results:
No change in clinical grading of dental fluorosis was noted. Considerable reduction in serum and urine fluoride levels was noted in both group A and group B patients. Dental fluorosis was noted in permanent teeth more commonly than deciduous teeth, and permanent maxillary central incisors had the highest prevalence rate.
Conclusion:
This study comprises only 30 patients with three months of follow-up. So, this sample of patients and duration of follow-up period are conclusive to observe changes in biochemical parameters but not sufficient to observe changes in clinical grading.
Keywords: Ascorbic acid, calcium, dental fluorosis, fluorosis
INTRODUCTION
Dental fluorosis is a fluoride-induced disturbance in tooth formation, which results in hypomineralized enamel with increased porosity. It is caused by excessive intake of fluoride, but only during the period of tooth development. The most important risk factor for dental fluorosis is the amount of fluoride consumed from all sources during the critical period of tooth development.[1]
The relationship of dental fluorosis with fluoride level of drinking water [normal: 0.6-0.8 ppm (parts per million) at 26.3-32.6°C and 0.9-1.7 ppm at 10-12°C] is well established.[2–5] Fluoridated supplements, fluoridated dentifrices, and infant formulas before the age of seven are the three major risk factors other than fluoridated water for dental fluorosis.[4–14] The mechanism underlying the development of dental fluorosis has not been conclusively determined. It was believed previously that excessive intake of fluoride interfered with the function of ameloblasts, perhaps inhibiting the secretion of, or altering the composition of enamel matrix proteins. It now appears that the risk of dental fluorosis is the lowest during the secretory stage of enamel development. It is suggested that fluorosis causes subsurface hypomineralization or porosity of enamel. This subsurface porosity is most likely caused by a delay in the hydrolysis and removal of enamel proteins, particularly amelogenins, as the enamel matures. This delay could be due to the direct effect of fluoride on the ameloblasts or to an interaction of fluoride with the proteins or proteinases in the mineralizing matrix. Early maturation stage of enamel formation appears to be particularly sensitive to fluoride exposure. The risk of enamel fluorosis is lowest when exposure takes place only during the secretory stage of enamel formation, but highest when exposure occurs in both secretory and maturation stages of enamel formation.[15]
The clinical appearance of dental fluorosis varies according to its severity. It is characterized by either chalky white discoloration confined only to incisal edges of anterior teeth and cusp tips of posterior teeth or chalky white discoloration involving either less than one-third, one-third to two–thirds, or more than two-thirds of the surface, with or without light-to-dark brown discoloration associated with or without discrete pitting and/or with large areas of missing enamel.[16] Chronic fluoride toxicity may produce skeletal fluorosis characterized by stiffness in the back and various joints, deformity in hips, knees, and other joints, bony exostosis in limb bones, neurologic manifestations, difficulty in walking due to weakness, nausea, loss of appetite, pain in the stomach, constipation, diarrhea, and allergic manifestations.[17]
Fluorosis occurs mainly by systemic route and can be predicted from fluoride expression in biological fluids like serum, plasma, and urine. Fluoride level of serum and urine are good indicators of fluoride exposure of the patients. Fluoride level in hair and nail have also been used to evaluate the risk of dental fluorosis.[3,18–23]
In the past, vitamin C, vitamin D, and salts of calcium, magnesium, or aluminum were prescribed individually in an attempt to inhibit or reverse the adverse effects of fluorosis. But the results were inconclusive.[24] However, in a few studies, calcium, ascorbic acid, and vitamin D3 have been proved to be effective when prescribed in combination in an attempt at reversal of dental fluorosis.[17,24,25]
The present study was carried out to evaluate clinical grading of dental fluorosis, reversal of dental fluorosis in patients with calcium, vitamin D3, and ascorbic acid, and pretreatment and post-treatment levels of certain biochemical parameters concerned with dental fluorosis. The role of fluoride level of drinking water in dental fluorosis and prevalence of dental fluorosis in both dentitions and teeth were assessed.
MATERIALS AND METHODS
The present study was conducted in 50 patients, randomly selected from the Oral Diagnosis, Oral Medicine and Dental Radiology Department of the Government Dental College and Hospital, Ahmedabad. All the 50 patients were evaluated thoroughly, and of them, 30 patients were treated with various medications to see the reversal changes, as 20 patients did not return for follow-up.
Criteria of selection
Patients belonging to any age group
Patients were to have chalky white and/or brownish discoloration of teeth with or without pitting of enamel
Patients were not to have any adverse habit or any cause other than dental fluorosis for discoloration of teeth
Patients with fracture of anterior teeth were not included in the study.
History of the patient was taken with various questions to evaluate the etiology of dental fluorosis and involvement of deciduous teeth to rule out other possible causes of discoloration of teeth. Patients were asked about bone pain, stiffness, and other complaints to rule out systemic fluorosis which was not present in any of the cases in the present study.
Examination of the patients
Extraoral and intraoral examination were carried out. In local examination, s ize and shape of teeth, type of discoloration whether chalky white and/or brownish were recorded. The extent of discoloration was recorded, whether it was affecting less than one-third, one-third to two-thirds, or more than two-thirds of the labial/buccal, lingual/palatal, and incisal/occlusal surfaces separately. Surfaces of teeth, pitting/grooves, and chipping of enamel were checked. Affected dentition was noted to evaluate the time of fluoride ingestion.
Evaluation of patients
All patients were thoroughly evaluated. Detailed examination of teeth was carried out to evaluate clinical grading of dental fluorosis. Grading of dental fluorosis was done on the basis of tooth surface index of fluorosis [Table 1].[16] Grades of dental fluorosis for labial/buccal, lingual/palatal, and occlusal/incisal surfaces were recorded separately before and after various medicinal treatments. In patients of dental fluorosis, involvement of multiple teeth was present. To simplify the clinical grading of dental fluorosis, the most severely affected tooth was considered for various grades in different tooth surfaces.
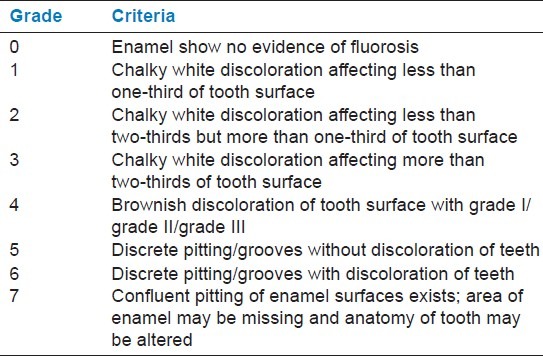
Table 1.
Diagnostic criteria and scoring system for the tooth surface index of fluorosis
Investigations
After evaluating clinical grading of dental fluorosis, various investigations (fluoride levels of serum, urine, and water) were carried out.
Collection of samples
To analyze the level of fluoride in urine, spot urine samples of the patients were collected from the 30 patients in nonreactive plastic containers and brought to the National Institute of Occupational Health (NIOH), Ahmedabad in an ice box. To analyze the level of fluoride in serum, a 3 mL venous blood sample was collected from the 30 patients by venipuncture. These samples were incubated at 25°C for two hours, centrifuged at 1500 rpm for 15 minutes, and the serum was separated into clean polyethylene tubes. Hemolyzed samples were discarded. Water, serum, and urine samples were stored at −20°C until assayed for fluoride in NIOH, Ahmedabad.
Method of estimation of fluoride level
Estimation of fluoride level in drinking water as well as serum fluoride and urine fluoride levels before and after administering various medicinal treatments was carried out in the 30 patients by ion selective electrode method (ion selective electrode method through the Orion model 96-09 fluoride – ALPHA, 1989) [Figure 1].
Figure 1.
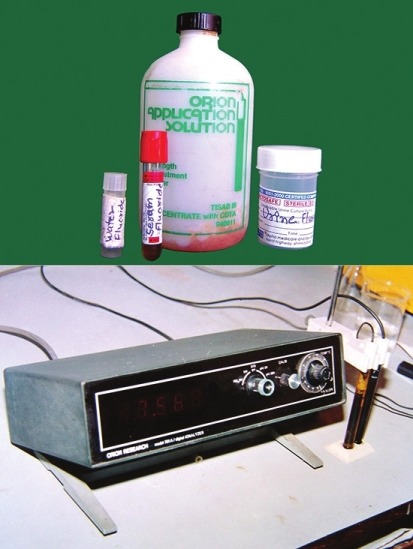
Fluoride estimation by ion selective electrode method
Treatment and follow-up
The selected 30 patients (age range from 8 to 17 years) were divided randomly into three groups, that is, group A, group B, and group C. No changes were made in food or water consumption. All of the patients were on a regular follow-up for the 90 days of therapy.
Group A: Medication group: Calcium (250 mg once daily) and vitamin D3 supplements (60,000 I.U. in 1 g sachets—in the morning—once a week) were given to 10 patients for three months.
Group B: Medication group: Ascorbic acid (500 mg once daily) and vitamin D3 (60,000 I.U. in 1 g sachets—in the morning—once a week) supplements were given to 10 patients for three months.
Group C: Control group: Chlorhexidine mouthwash [gargling twice a day (in the morning and before going to sleep)] as a placebo was given to 10 patients for three months.
Follow-up
Follow-up of the patient was done every 15 days for three months. Local examination of the patient was done on every follow-up and change in clinical grades of dental fluorosis was recorded in the pro forma in a tabulated form every 15 days.
Follow-up after three months of treatment
Improvement in clinical grading of dental fluorosis was checked and post-treatment biochemical parameters were assessed and recorded in treated patients.
Pretreatment and post-treatment clinical grades of dental fluorosis and serum fluoride level and urine fluoride level were compared and recorded.
RESULTS
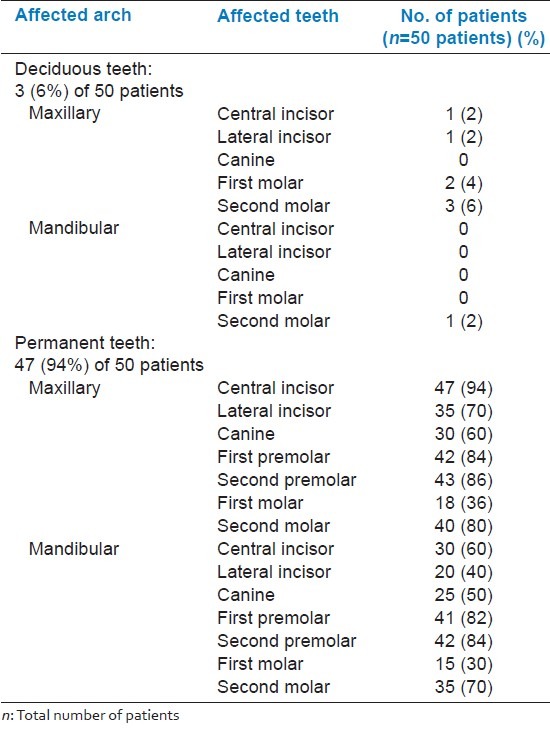
Drinking water can be a good source of fluoride. Of the 30 patients, fluoride levels of drinking water were normal in 14 (46.6%) patients, above normal level in 10 (33.33%) patients, and below normal level in six (20%) patients [Figure 2]. Distribution of patients according to affected teeth is reported in Table 2. Of the 50 patients, permanent dentition was affected more commonly [47 patients (94%)] than deciduous dentition [3 patients (6%)] and maxillary teeth affected more commonly than homologous mandibular teeth. In permanent teeth, the maxillary central incisor was found to be the most commonly affected [47 (94%) patients] followed by maxillary and mandibular first and second premolar teeth. Mandibular first molar was the least commonly affected.
Figure 2.
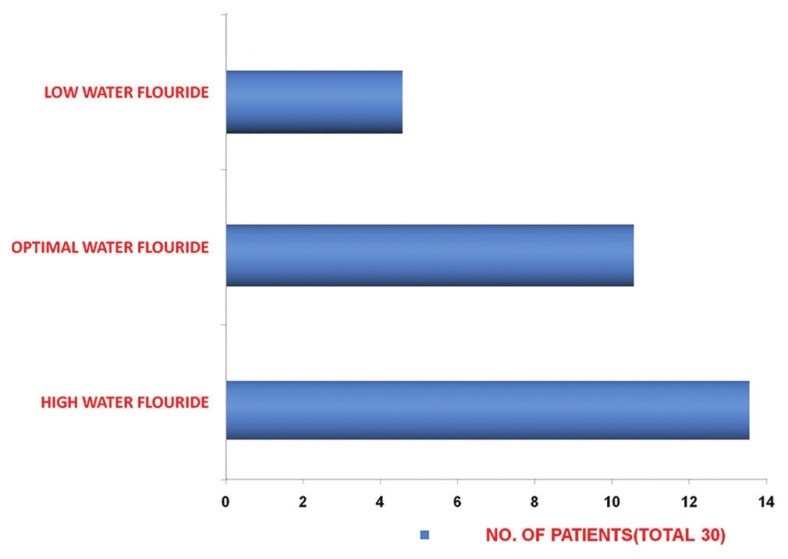
Fluoride level in drinking water of patients
Table 2.
Distribution of patients according to affected teeth
A noticeable reduction in serum fluoride level was found in group A and group B after three months of treatment [Figure 3]. It was more noticeable in group A than group B; mean difference of serum fluoride level was 0.79 ppm and 0.52 ppm, respectively [Table 3]. A noticeable reduction in urine fluoride level was found in group A and group B after three months of treatment [Figure 4]. It was more noticeable in group A than group B; mean difference of urine fluoride level was 1.24 ppm and 0.75 ppm, respectively [Table 3]. This shows the change in biochemical parameters after three months of treatment. No significant reduction in serum and urine fluoride level was noted in patients of group C, the control group.
Figure 3.
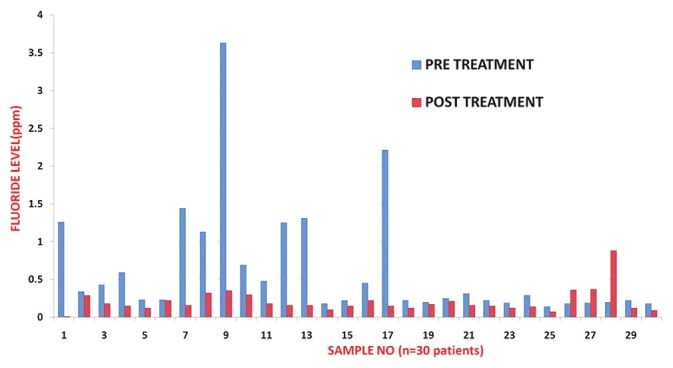
Correlative analysis of pretreatment and post-treatment serum fluoride level in patients of different treatment groups
Table 3.
Correlative analysis of pretreatment and post-treatment serum and urine fluoride levels in patients of different treatment groups
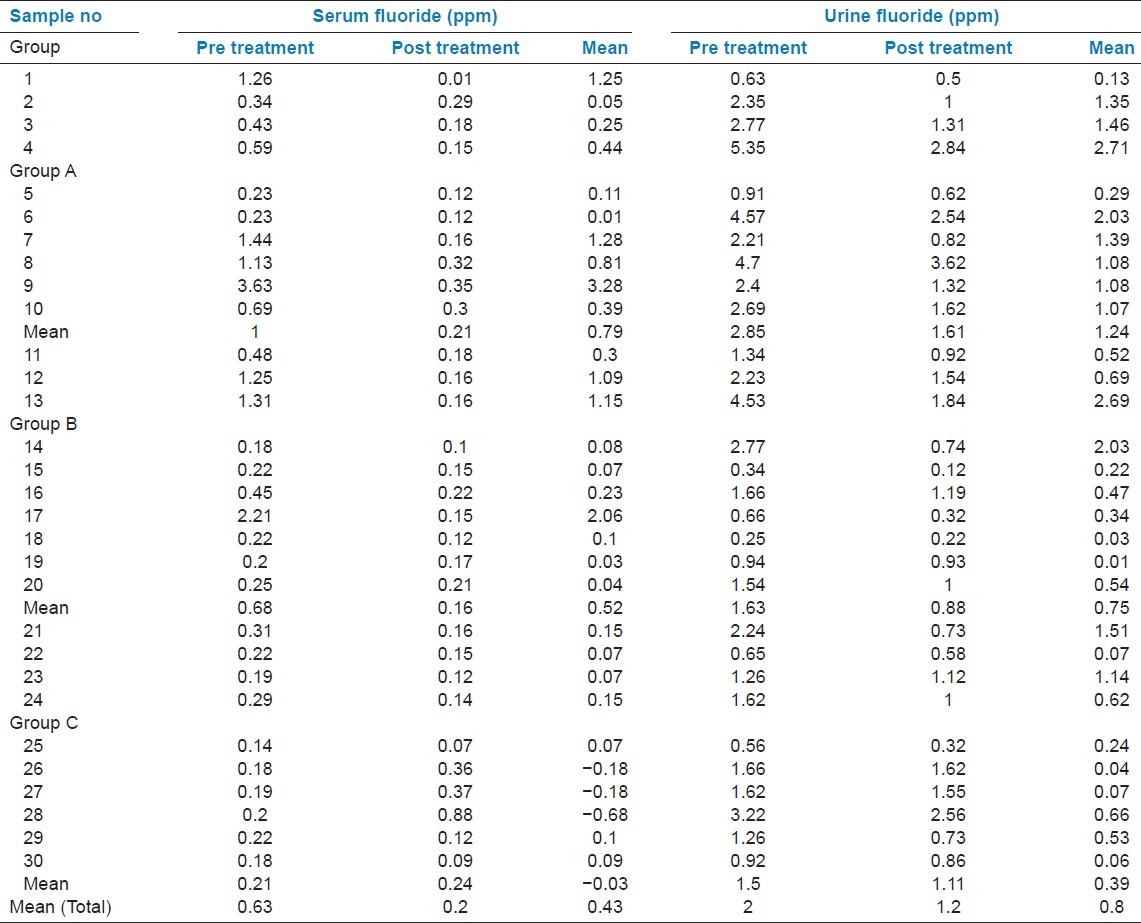
Figure 4.
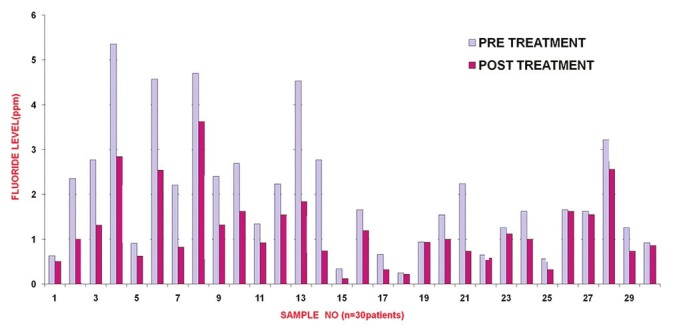
Correlative analysis of pretreatment and post treatment urine fluoride level in patients of different treatment groups
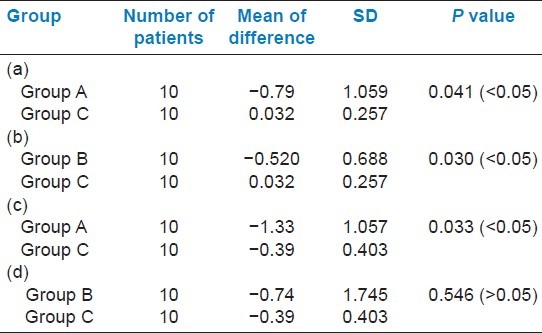
Table 4 shows the change in serum and urine fluoride level after three months of treatment in various groups as compared to baseline values. Tables 4a and b show a significant reduction in serum fluoride level after three months of treatment from the baseline values recorded before treatment. The P value is 0.041 which is <0.05 suggestive of a significant reduction in serum fluoride level after three months of treatment from baseline values in treatment group A as compared to group C [Table 4a]. The P value is 0.030, which is <0.05 suggestive of a significant reduction in serum fluoride level after three months of treatment from baseline values in treatment group B as compared to group C [Table 4b]. Tables Table 4c and d show a decrease in urine fluoride level from the baseline values after three months of treatment. The P value is 0.033, which is <0.05 suggestive of a significant decrease in urine fluoride level after three months of treatment in group A as compared to group C Table 4c. The P value is 0.546 which is >0.05. This means the decrease in urine fluoride level after three months of treatment is not significant in group B as compared to group C [Table 4d].
Table 4.
Change in serum fluoride level after three months of treatment in various groups as compared to baseline values
DISCUSSION
Dental fluorosis is a fluoride-induced disturbance in tooth formation, which results in hypomineralized enamel with increased porosity caused by excessive intake of fluoride.[1]
In the present study, the age group of 11-17 years was found to be the most commonly affected with dental fluorosis, as during this period parents as well as children become conscious about dental health, particularly cosmetic appearance. Moreover, dental fluorosis is more common in permanent teeth compared to deciduous teeth.[26–28] Hence, this group remains the most commonly affected for dental fluorosis.
The present study showed that approximately 46% of the patients were living in various areas of Ahmedabad city with normal fluoride level of water. Dental fluorosis was found in approximately 33% of the patients coming from the area with higher fluoride level of water and only 20% cases were from the area with low level of fluoride in the drinking water. The prime reason for dental fluorosis is high fluoride level in drinking water. Other than this, three major risk factors were identified. They are fluoridated supplements, fluoridated dentifrices, and infant formulas before the age of seven years.[4–14,29] Fluoridated toothpastes contribute to the risk of enamel fluorosis because the swallowing reflex is not well developed in children below six years, particularly below three years. The significantly lower prevalence and severity of dental fluorosis among the vegetarian group compared to the nonvegetarians would seem to be related to diet.[30] The present study showed that 92% of the cases fall in the age group of 11-17 years; so, fluoridated toothpaste cannot be considered as a causative factor of dental fluorosis in our study.
The maximum number of patients in the present study showed prevalence of dental fluorosis in permanent teeth rather than deciduous teeth. The literature also showed that the prevalence in permanent teeth is more than that in deciduous dentition.[26–28] This is because excess fluoride arrests the late phases of enamel formation. The maturative stage of enamel formation is the lengthiest phase, lasting from one to two years for primary teeth and four to five years for permanent posterior teeth. As the maturative stage is much shorter in primary teeth, less fluoride is found in the primary teeth than in permanent teeth developed under the same exposure to fluoride. Studies also showed that prevalence in deciduous teeth is low due to limited permeability of the human placenta by fluoride.[26]
In the present study, maxillary teeth were found to be more commonly affected than homologous mandibular teeth. The literature also showed that dental fluorosis is more severe in maxillary teeth than in homologous mandibular teeth.[4] In the present study, in permanent teeth, maxillary central incisors were found most commonly affected by dental fluorosis followed by premolars and second molars. Various studies established that maxillary central incisors are most commonly affected by dental fluorosis.[31] The prevalence of dental fluorosis is low in mandibular incisors and first molars in contrast to maxillary central incisors. From Haavikko's 1970 tooth development data it is evident that first molars and lower incisors are at or have passed the ‘crown completed’ stage around the age of three, that is, the time when the fluoride regimen is initiated in most children. However, upper central incisors are at an earlier stage of tooth development at this age.[32] Various other studies showed that premolars and second molars which mineralize later than anterior teeth may be more severely affected due to the cumulative effect of fluoride.[4] Various studies showed that the intraoral distribution of the severity of dental fluorosis within permanent dentition in decreasing order depends on the duration of enamel formation, age at completion of enamel formation, age of tooth eruption, and the age at the start of enamel formation.[2]
In this study, no change in clinical grades was noted, but changes were noted in biochemical parameters, that is, serum fluoride and urine fluoride levels. As seen in the results, a significant decrease in serum fluoride levels of the patients was noted in patients of group A and group B after three months of treatment and was more significant in group A treated with calcium and vitamin D3 supplements than group B treated with ascorbic acid and vitamin D3 supplements. A significant decrease in urine fluoride level of patients was also noted after three months of treatment in both group A and group B. This is suggestive of a decrease in the level of biochemical parameters in patients of dental fluorosis. No significant changes in either serum fluoride or urine fluoride were noted in patients of the control group C. Thus, the therapy reduced the fluoride levels markedly in body fluids, serum and urine. Fluoride level in urine has been used to estimate the absorbed amount of fluoride.[25] Thus, the present study showed reduced fluoride absorption.
Various studies showed that dietary calcium protects the individual against fluoride toxicity by reducing its absorption.[25,33,34] Calcium interacts with the fluoride to form calcium fluoride which is an insoluble salt and being a larger molecule is not absorbed from the gastrointestinal tract and excreted through feces.[35] Vitamin D3 increases the absorption of calcium and thus directly affects the absorption of fluoride ions.[24] Vitamin C (ascorbic acid) is an important entity to ameliorate the ill effects of fluoride. Vitamin C acts as a cofactor or coenzyme in the process of hydroxylation of proline, one of the most important amino acids of collagen, the base material for bone and tooth matrix.[35]
CONCLUSION
Increasing fluoride level in water is a major risk factor for dental fluorosis. Permanent dentition is involved more in dental fluorosis than primary dentition. Maxillary teeth are more commonly affected than homologous mandibular teeth and maxillary central incisors are found to be the most commonly affected teeth, whereas first molars are the least commonly affected. No change in clinical grading of dental fluorosis was noted in all three groups of treated patients. A significant reduction in serum fluoride and urine fluoride levels was noted in patients treated with calcium, vitamin D3, and ascorbic acid-vitamin D3. The study regarding reversal of dental fluorosis comprised only 30 patients with three months of regular follow-up. So, this sample of patients and duration of follow-up period are conclusive to observe changes in biochemical parameters but not sufficient to observe changes in clinical grading. Hence, more number of patients with long term follow-up is required for better clinical evaluation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Rabelo MA, Aparecido J, Milton G. Fluoride exposures and dental fluorosis: A literature review. Rev Fob. 2001;9:1–10. [Google Scholar]
- 2.Ekanayake L, van der Hoek W. Prevalence and distribution of enamel defects and dental caries in a region with different concentration of fluoride in drinking water in Sri Lanka. Int Dent J. 2003;53:243–8. doi: 10.1111/j.1875-595x.2003.tb00752.x. [DOI] [PubMed] [Google Scholar]
- 3.Hossny E, Reda S, Marzouk S, Diab D, Fahmy H. Serum fluoride levels in a group of Egyptian infants and children from Cairo city. Arch Environ Health. 2003;58:306–15. doi: 10.3200/aeoh.58.5.306-315. [DOI] [PubMed] [Google Scholar]
- 4.Alvarez JA, Rezende KM, Marocho SM, Alves FB, Celiberti P, Ciamponi AL. Dental fluorosis: Exposure, prevention and management. Med Oral Patol Oral Cir Bucal. 2009;14:E103–7. [PubMed] [Google Scholar]
- 5.Marshall T, Levy S, Warren J, Broffitt B, Eichenberger J, Stubo P. Associations between intakes of fluorides form beverages during infancy and dental fluorosis of primary teeth. J Am Coll Nutr. 2004;23:108–16. doi: 10.1080/07315724.2004.10719350. [DOI] [PubMed] [Google Scholar]
- 6.Warren JJ, Levy SM. Current and future role of fluoride in nutrition. Dent Clin North Am. 2003;47:225–43. doi: 10.1016/s0011-8532(02)00098-8. [DOI] [PubMed] [Google Scholar]
- 7.Jackson RD, Brizendine EJ, Kelly SA, Hinesley R, Stookey GK, Dunipace AJ. The fluoride content of foods and beverages from negligibly and optimally fluoridated communities. Community Dent Oral Epidemiol. 2002;30:382–91. doi: 10.1034/j.1600-0528.2002.00002.x. [DOI] [PubMed] [Google Scholar]
- 8.Brothwell DJ, Limeback H. Fluorosis risk in grade 2 students residing in a rural area with widely varying natural fluoride. Community Dent Oral Epidemiol. 1999;27:130–6. doi: 10.1111/j.1600-0528.1999.tb02002.x. [DOI] [PubMed] [Google Scholar]
- 9.Yoder KM, Mabelya L, Robison VA, Dunipace AJ, Brizendine EJ, Stookey GK. Severe dental fluorosis in a Tanzanianh population consuming water with 9. negligible fluoride concentration. Community Dent Oral Epidemiol. 1998;26:382–93. doi: 10.1111/j.1600-0528.1998.tb01976.x. [DOI] [PubMed] [Google Scholar]
- 10.Marino R, Villa A, Weitz A, Guerrero S. Prevalence of fluorosis in children aged 6-9 years old who participated in milk fluoridation programme in Codegua, Chile. Community Dent Health. 2004;21:143–8. [PubMed] [Google Scholar]
- 11.Levy SM. Review of fluoride exposures and ingestion. Community Dent Oral Epidemiol. 1994;22:173–80. doi: 10.1111/j.1600-0528.1994.tb01836.x. [DOI] [PubMed] [Google Scholar]
- 12.Clarkson JJ, O’Mullane DM. Prevalence of enamel defects/fluorosis in fluoridated and non-fluoridated areas in Ireland. Community Dent Oral Epidemiol. 1992;20:196–9. doi: 10.1111/j.1600-0528.1992.tb01715.x. [DOI] [PubMed] [Google Scholar]
- 13.Levy SM. An update of fluorides and fluorosis. J Can Dent Assoc. 2003;69:286–91. [PubMed] [Google Scholar]
- 14.Stookey GK. Review of fluorosis of self-applied topical fluorides: Dentifrices, mouthrinses and gels. Community Dent Oral Epidemiol. 1994;22:181–6. doi: 10.1111/j.1600-0528.1994.tb01837.x. [DOI] [PubMed] [Google Scholar]
- 15.DenBesten PK. Biological mechanisms of dental fluorosis relevant to the use of fluoride supplements. Community Dent Oral Epidemiol. 1999;27:41–7. doi: 10.1111/j.1600-0528.1999.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 16.Rozier RG. Epidemiologic indices for measuring the clinical manifestations of dental fluorosis: Overview and critique. Adv Dent Res. 1994;8:39–55. doi: 10.1177/08959374940080010901. [DOI] [PubMed] [Google Scholar]
- 17.Whyte MP, Totty WG, Lim VT, Whitford GM. Skeletal fluorosis from instant tea. J Bone Miner Res. 2008;23:759–69. doi: 10.1359/jbmr.080101. [DOI] [PubMed] [Google Scholar]
- 18.Yadav JP, Lata S. Urinary fluoride levels and prevalence of dental fluorosis in children of Jhajjar District, Haryana. Indian J Med Sci. 2003;57:394–9. [PubMed] [Google Scholar]
- 19.Majumdar KK. Health impact of supplying safe drinking water containing fluoride below permissible level on flourosis patients in a fluoride-endemic rural area of West Bengal. Indian J Public Health. 2011;55:303–8. doi: 10.4103/0019-557X.92411. [DOI] [PubMed] [Google Scholar]
- 20.Richards A, Likimani S, Baelum V, Fejerskov O. Fluoride concentrations in unerupted fluorotic human enamel. Caries Res. 1992;26:328–32. doi: 10.1159/000261463. [DOI] [PubMed] [Google Scholar]
- 21.Villa AE, Salazar G, Anabalón M, Cabezas L. Estimation of the fraction of an ingested dose of fluoride excreted through urine in pre-school children. Community Dent Oral Epidemiol. 1999;27:305–12. doi: 10.1111/j.1600-0528.1998.tb02025.x. [DOI] [PubMed] [Google Scholar]
- 22.Heintze SD, Bastos JR, Bastos R. Urinary Fluoride levels and prevalence of dental fluorosis in three Brazilian cities with different fluoride concentrations in the drinking water. Community Dent Oral Epidemiol. 1998;26:316–23. doi: 10.1111/j.1600-0528.1998.tb01967.x. [DOI] [PubMed] [Google Scholar]
- 23.Levy FM, Bastos JR, Buzalaf MA. Nails as biomarkers of fluoride in children of fluoridated communities. J Dent Child. 2004;71:121–5. [PubMed] [Google Scholar]
- 24.Gupta SK, Gupta RC, Seth AK, Gupta A. Reversal of fluorosis in children. Acta Paediatr Jpn. 1996;38:513–9. doi: 10.1111/j.1442-200x.1996.tb03536.x. [DOI] [PubMed] [Google Scholar]
- 25.Sheth Gupta SK, Gupta RC, Seth AK. Reversal of clinical and dental fluorosis. Indian Pediatr. 1994;31:439–43. [PubMed] [Google Scholar]
- 26.Thylstrup A. Is there a biological rationale for prenatal fluoride administration? ASDC J Dent Child. 1981;48:103–8. [PubMed] [Google Scholar]
- 27.Warren JJ, Levy SM, Kanellis MJ. Prevalence of dental fluorosis in the primary dentition. J Public Health Dent. 2001;61:87–91. doi: 10.1111/j.1752-7325.2001.tb03371.x. [DOI] [PubMed] [Google Scholar]
- 28.Levy SM, Hillis SL, Warren JJ, Broffitt BA, Mahbubul Islam AK, Wefel JS, et al. Primary tooth fluorosis and fluoride intake during the first year of life. Community Dent Oral Epidemiol. 2002;30:286–95. doi: 10.1034/j.1600-0528.2002.00053.x. [DOI] [PubMed] [Google Scholar]
- 29.Akpata ES, Fakiha Z, Khan N. Dental fluorosis in 12-15 year children exposed to fluorides from well drinking water in the Hail region of Saudi Arabia. Community Dent Oral Epidemiol. 1997;25:324–7. doi: 10.1111/j.1600-0528.1997.tb00947.x. [DOI] [PubMed] [Google Scholar]
- 30.Awadia AK, Haugejorden O, Bjorvatn K, Birkeland JM. Vegetarianism and dental fluorosis among children in a high fluoride area of northern Tanzania. Int J Paediatr Dent. 1999;9:3–11. doi: 10.1046/j.1365-263x.1999.00104.x. [DOI] [PubMed] [Google Scholar]
- 31.Mascarenhas AK, Burt BA. Fluorosis risk form early exposure to fluoride toothpaste. Community Dent Oral Epidemiol. 1998;26:241–8. doi: 10.1111/j.1600-0528.1998.tb01957.x. [DOI] [PubMed] [Google Scholar]
- 32.Larsen MJ, Richards A, Fejerskov O. Development of dental fluorosis according to age at start of fluoride administration. Caries Res. 1985;19:519–27. doi: 10.1159/000260892. [DOI] [PubMed] [Google Scholar]
- 33.Wagner M, Muhler J. The effect of calcium and phosphorus on fluoride absorption. J Dent Res. 1960;39:49–52. [Google Scholar]
- 34.Gupta SK, Khan TI, Gupta RC, Gupta AB, Gupta KC, Jain P, et al. Compensatory hyperparathyroidism following high fluoride ingestion-a clinco-biochemical correlation. Indian Pediatr. 2001;38:139–46. [PubMed] [Google Scholar]
- 35.Choubisa SL, Choubisa L, Choubisa D. Reversibility of natural dental fluorosis. Int J Pharmacol Bio Sci. 2011;5:89–93. [Google Scholar]


