Abstract
Jugular venous aneurysm is an extremely rare condition. The patients presented with a painless swelling in the neck that appears while coughing, straining, bending, or breath holding. Detection of a soft and compressible swelling in the course of an external jugular vein (EJV) superficial to the sternomastoid muscle, non-filling on compression of the EJV during Valsalva maneuver clinches the diagnosis of EJV aneurysm. Color Doppler ultrasound allows precise delineation of the lesion and is considered the gold standard for confirming the diagnosis. Surgical excision is indicated mostly for cosmetic reasons and symptomatic aneurysms. We, herein, report a patient with saccular external jugular venous aneurysm to highlight the typical clinical presentation and diagnosis of this rare entity.
Keywords: Aneurysm, external jugular vein, ultrasound
INTRODUCTION
Cervical swelling is a commonly encountered problem in pediatric population. The neck swellings can be solid, cystic and pulsatile on clinical examination. The differential diagnosis of a cystic neck mass that becomes prominent on coughing, straining, breath holding, or Valsalva maneuver includes superior mediastinal tumors or cysts, external laryngeal diverticula and laryngocele, inflation of the cupola of the lung, and jugular venous aneurysms.[1] Isolated venous aneurysm involving the low pressure superior vena caval reservoir system is uncommon, particularly in the absence of an underlying cardiovascular disease or trauma. We report a case of a 12-year-old boy who was diagnosed to have saccular external jugular venous aneurysm, and discuss the clinical presentation and management of this rare entity.
CASE REPORT
We report a case of a 12-year-old boy presented with a painless swelling on the right side of the neck for 6 months. The swelling became more prominent on breath holding [Figure 1] and decreased in size on resuming normal breathing. There was no prior history of trauma or any chronic illness. Upon examination, a 4.0 × 4.0 cm swelling appeared on the right supraclavicular area lateral to the clavicular head of the sternomastoid muscle on breath holding. The swelling was non-tender, soft and compressible, and had ill-defined margins. Visible pulsation or cough impulse was absent. However, the swelling did not become prominent on Valsalva maneuver when pressure was applied to an external jugular vein (EJV) above the swelling. No bruit was audible on auscultation. Chest X-ray was normal. Ultrasound revealed an anechoic lesion measuring 3.4 × 3.3 × 3.0 cm adjacent to and communicating with EJV, approximately 1.3 cm proximal to its merger with the subclavian vein [Figure 2]. Color Doppler examination demonstrated slow flow within this lesion. On computerized tomogram (CT) angiography, a 3.4 × 3.3 × 3.0 cm enhancing lesion was seen superior to the right subclavian vein causing splaying of EJV and internal jugular vein [Figure 3]. Intra-operatively, the vascular lesion was found to be originating from the right EJV. The aneurysm was excised after ligation of various tributaries. Recovery was uneventful and the child was discharged on the fourth postoperative day.
Figure 1.

Neck swelling lateral to the right sternomastoid muscle made prominent on breath holding
Figure 2.
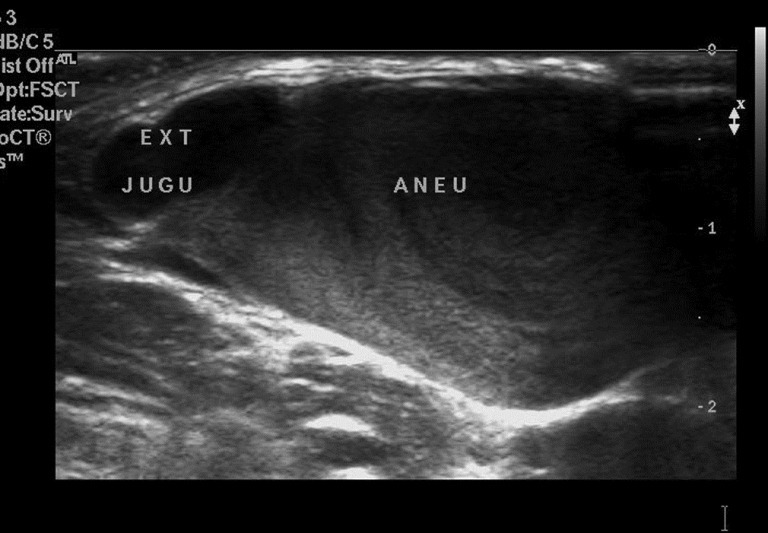
Ultrasonogram demonstrating the origin of aneurysm from the external jugular vein
Figure 3.

Computerized tomogram angiography showing aneurysmal mass superior to the right subclavian vein with splaying of an external jugular vein and an internal jugular vein
DISCUSSION
Jugular venous aneurysm or jugular phlebectasia is the most commonly encountered venous malformation involving the neck veins. Venous dilatation in the neck involves the internal, external and anterior jugular vein, in descending order of frequency.[2] Macroscopic fusiform dilatation or phlebectasia in the neck veins is considered to be congenital in origin. However, saccular dilatation or aneurysm involving the jugular venous system can appear either spontaneously, in the absence of any known etiologic cause or secondary to tumors, inflammation and trauma.[3] In children, jugular phlebectasia is commonly encountered on the right side. In adults, the venous aneurysms are mostly acquired and are more common on the left side. Increased occurrence of the left-sided lesions in elderly hypertensive patients have been attributed to compression of the left innominate vein by a high atherosclerotic aorta.[4]
Clinically, by a careful process of elimination, the preoperative diagnosis can often be accurately established. Saccular aneurysm of the jugular vein mostly presents as a painless swelling. Thrombosis within the aneurysm can produce pain in the swelling and symptoms secondary to pressure effect on surrounding structures. The presence of a unilateral, non-tender, soft, and non-pulsatile swelling that enlarges with straining, crying, sneezing, or Valsalva maneuver is the characteristic of venous aneurysm. Finding of a soft and compressible swelling superficial to the right sternomastoid muscle in the course of EJV that became prominent with breath holding but no refilling on Valsalva while EJV was kept compressed above the swelling clinched the diagnosis in favor of venous aneurysm in our case.
The radiological investigations for diagnosis; ranges from simple ultrasonogram to sophisticated tools such as venography, CT angiography, and magnetic resonance angiography. However, ultrasound with Doppler imaging has replaced other costly invasive diagnostic tools as the investigation of choice for EJV aneurysm.[5] Ultrasound with Doppler allows differentiation between cystic and solid lesions, differentiation of vascular from non-vascular lesions, identification of site of origin of the lesion, and its relationship with the surrounding structures in the neck.
Asymptomatic aneurysms can be managed expectantly with reassurance and regular follow-up. Surgical excision is offered for either cosmetic reasons or a painful aneurysm secondary to thrombosis or phlebitis of the jugular venous system.[6] Surgical resection also eliminates the theoretical risk of aneurismal rupture, pulmonary embolism and allows for histopathological diagnosis. A symptomatic saccular jugular venous aneurysm can be safely managed by excision and ligation, while exclusion and bypass is indicated in fusiform dilatation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Zohar Y, Ben-Tovim R, Talmi YP. Phlebectasia of the jugular system. J Craniomaxillofac Surg. 1989;17:96–8. doi: 10.1016/s1010-5182(89)80053-8. [DOI] [PubMed] [Google Scholar]
- 2.LaMonte SJ, Walker EA, Moran WB. Internal jugular phlebectasis.A clinicoroentgenographic diagnosis. Arch Otolaryngol. 1976;102:706–8. [PubMed] [Google Scholar]
- 3.Schatz IJ, Fine G. Venous aneurysms. N Engl J Med. 1962;266:1310–2. doi: 10.1056/NEJM196206212662505. [DOI] [PubMed] [Google Scholar]
- 4.Nwako FA, Agugua NE, Udeh CA, Osuorji RI. Jugular phlebectasia. J Pediatr Surg. 1989;24:303–5. doi: 10.1016/s0022-3468(89)80019-3. [DOI] [PubMed] [Google Scholar]
- 5.Lee HY, Yoo SM, Song IS, Yu H, Lee JB. Sonographic diagnosis of a saccular aneurysm of the internal jugular vein. J Clin Ultrasound. 2007;35:94–6. doi: 10.1002/jcu.20263. [DOI] [PubMed] [Google Scholar]
- 6.Ascher E, Salles-Cunha S, Hingorani A. Morbidity and mortality associated with internal jugular vein thromboses. Vasc Endovascular Surg. 2005;39:335–9. doi: 10.1177/153857440503900405. [DOI] [PubMed] [Google Scholar]


