Abstract
We have reported a case of a 40-year-old male diabetic patient, resident of a rural area, who visited the outpatient clinic of the diabetic center in Alnoor Specialist Hospital, Makkah, Saudi Arabia. He came to seek medical advice for a single wound in the back of the shoulder since 1 month. After examination, a larva was eliminated and sent to laboratory for confirmation. It was confirmed as the third-stage larva of Sarcophaga species after macroscopic and microscopic examination. This is the first case of a patient having diabetic wound myiasis with the larva of Sarcophaga species reported in the Makkah region of Saudi Arabia.
Keywords: Diabetes mellitus, larva, myiasis, Sarcophagi
INTRODUCTION
Myiasis or infestation with fly larvae is common in domestic and wild mammals around the world, and is caused by different species of flies.[1] It broadly includes interaction between flies and warm-blooded hosts.[2] Advanced age, poor hygiene, bad housing conditions, vascular disease, and diabetes are the predisposing factors for myiasis. In humans, myiasis is seen more frequently in rural regions where people are in close contact with pets.[3] Infestation with fly larvae may occur when flies deposit eggs or first-stage larvae on the human body or body apertures. The portion of the body affected varies with the habits and preferences of the fly species and may also depend on other factors.[4]
Here, we report a case of a diabetic patient with myiasis in the back of the trunk. Moreover, morphological identification of these larvae, both macroscopically and microscopically, has been done.
CASE REPORT
A 40-year-old male diabetic patient visited the outpatient clinic of the diabetic center in Alnoor Specialist Hospital, Makkah, Saudi Arabia, seeking medical advice for a single wound in the back of the shoulder since 1 month. He resided in a rural area near Makkah and was working as a shepherd who was in close contact with goats and sheep. A moving worm was found in his wound. After complete general physical examination, which was normal with normal vital signs with no organomegaly or palpable masses, the worm was eliminated through pressure around the wound with forceps and sent to the parasitological department in the laboratory of Alnoor Specialist Hospital. The wound was cleaned and rinsed with antiseptic solution and covered with a sterile dressing of gauze and nylon mesh. The blood report results for thyroid function test (free thyroxin [FT4] and thyroid-stimulating hormone [TSH]) and lipid profile (cholesterol, triglycerides, high-density lipoprotein [HDL]) were found to be within the normal range. However, fasting blood glucose and HbA1c values were high. The patient was discharged on appropriate counseling and medication to control diabetes as well as wound care.
Subsequently, the larva was subjected to macroscopic and microscopic examination. Macroscopic examination was done by naked eyes, which revealed that it was the third-stage larva of Sarcophaga species, and was grayish in color, 18–19 mm long and 4 mm in width. The body of the larva was pointed anteriorly and was progressively widened posteriorly. For microscopic examination, the larva was cleared in a solution of 10% potassium hydroxide.[5]
The anterior and posterior parts of the larva were prepared for whole mount for identification of the anterior and the posterior spiracles. A preserved larva sample was prepared.[6]
The larva was first washed in distilled water and then cleared in 10% potassium hydroxide (KOH) solution for 26 h. The larva was washed again in distilled water, transferred to 10% acetic acid for 30 min and washed again in distilled water. At this stage, all the internal organs of the maggot were removed and the posterior spiracles were cut transversely. The specimens were then dehydrated in ascending series of ethanol (30%, 50%, 70% and 90%) for 30 min each. The larva was then soaked in absolute alcohol for at least 1 h and then transferred into clove oil. The specimens were mounted onto a glass slide using Canada balsam and left in an incubator for 1–2 days. The slide was examined under a light microscope for taxonomy studies and identification. Light microscopic findings revealed that the larva was sub-cylindrical in cross-sections with the flattened ventral surface and tapering toward the anterior extremity. The posterior end was narrowed with a pit-like depression where the posterior spiracles were located. Body segments were banded with transverse spinous swellings. In this third-stage larva of Sarcophaga species, the posterior spiracles were located near each other and each plat was formed of widely opened peritreme with a very indistinct button. Each plate contained of three elongated slits. The median one was straight, whereas the lateral ones were curved anteriorly [Figures 1 and 2].
Figure 1.

Larva extraction and size
Figure 2.
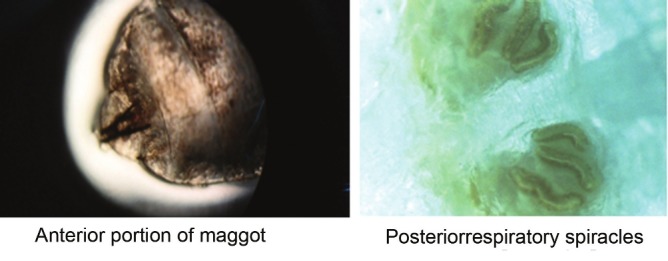
Microscopic features of larva
DISCUSSION
In our case report, the patient was residing in a rural area and had low standards of living. The 40-year-old male patient was working as a shepherd and was in close contact with goats and sheep. The larva collected was identified as the third stage of Sarcophaga species macroscopically and microscopically after identifying the respiratory spiracles .
A case of oral myiasis in an 8-year-old child caused by the flies of the Sarcophagidae in Abqaiq in the Eastern Province of Saudi Arabia was reported in 2002.[7] Omar and Abdalla reported seven cases of human cutaneous myiasis caused by maggots of the tumbu fly, Cordylobia anthropophaga, from the Asir region, which is a southwestern region of Saudi Arabia, and confirmed that this calliphorine species is not restricted to tropical Africa.[8]
A case of cutaneous myiasis identified as Sarcophaga cruentata was reported in a hospitalized patient with serious multiple traumas in 2008 in Italy. The presence of cutaneous myiasis in such a patient is sometimes due to poor general hospital hygiene; however, nosocomial myiasis can be considered as sarcasm of the infectious and parasitic risks faced by sensitive patients with large suppurative, necrotic wounds.[9] Another 25-year-old male patient from a rural area in India presented with intestinal myiasis caused by larvae of Sarcophaga, which was reported in 2009. It was presumed that myiasis was due to improper cooked food from outside vendors, which again showed bad hygiene as the causative organism.[10]
Ahmad et al. reported four cases of intestinal myiasis (two of them were living in a village/suburban region of Minia Governorate, Egypt) that were caused by larvae of Sarcophaga species. This finding is similar to that of our findings.[3]
It has been suggested that greater awareness on the part of physicians about clinical symptoms and relevant exposure histories would improve the expediency and efficacy of treatment for patients with myiasis.[11] Particular attention should be given to the wound dressings and plaster casts of elderly or infirmed patients because these can actually conceal infestations to which these patients are unable to respond.[12] Furthermore, it is likely that many cases of myiasis remain unreported for various cultural, social and medico–political reasons.[13]
To the best of our knowledge, this is the first report of wound myiasis in Makkah region. There is a paucity of such information from this country, probably because specimens tend to be discarded without study due to lack of expertise in identifying fly larvae.
CONCLUSION
We conclude that the myiasis, in this case, was a complication of an open, neglected wound mainly due to uncontrolled diabetes. The most important procedure in the treatment of diabetic wounds is a thorough rinsing procedure with antiseptic and/or antibiotic solutions before consistent dressing changes on a daily basis. Here, a complete covering of the wound is indispensable, especially during the summer.
Footnotes
Source of Support: Alnoor Specialist Hospital, Makkah, Saudi Arabia
Conflict of Interest: None declared
REFERENCES
- 1.Yilmaz H, Kotan C, Akdeniz H, Buzğan T. Gastric myiasis due to Oestrus species in a patient with gastric adenocarcinoma : A case report. East J Med. 1999;4:80–1. [Google Scholar]
- 2.Mohammadzadeh T, Esfandiari1 F, Sadjjadi SM. A case of gingival myiasis caused by Wohlfahrtia magnifica. Iran J Arthropod Borne Dis. 2008;2:53–6. [Google Scholar]
- 3.Ahmad AK, Abdel-Hafeez EH, Makhloof M, Abdel-Raheem EM. Gastrointestinal myiasis by larvae of Sarcophaga sp. and Oestrus sp. in Egypt: Report of cases, and endoscopical and morphological studies. Korean J Parasitol. 2011;49:51–7. doi: 10.3347/kjp.2011.49.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shazia MT, Anjum S, Yousuf MJ. Systematics and population of sarcophagid flies in Faisalabad (Pakistan) Int J Agric Biol. 2006;8:809–11. [Google Scholar]
- 5.Khalifa RM, Mowafy NM. Light and scanning electron microscopical identification of sarcophagid larva causing intestinal myiasis. Egypt J Med Sci. 1997;18:235–43. [Google Scholar]
- 6.Lee HL, Abdullah AA, Cheong WH. The use of fly larvae from human corpses in determining the time of death: A review and some technical considerations. J Med Health Lab Tech Malays. 1984;9:15–7. [Google Scholar]
- 7.Khayat RM. A case report on oral myiasis in Saudi Arabia. Saudi Dent J. 2002;14:140–2. [Google Scholar]
- 8.Omar MS, Abdalla RE. Cutaneous myiasis caused by tumbu fly larvae, Cordylobia anthropophaga in southwestern Saudi Arabia. Trop Med Parasitol. 1992;43:128–9. [PubMed] [Google Scholar]
- 9.Dutto M, Bertero M. Traumatic myiasis from Sarcophaga (Bercaeal cruentata Meigen, 1826 (Diptera, Sarcophagidae) in a hospital environment: Reporting of a clinical case following polytrauma. J Prev Med Hyg. 2010;51:50–2. [PubMed] [Google Scholar]
- 10.Das A, Pandey A, Madan M, Asthana AK, Gautam A. Accidental intestinal myiasis caused by genus Sarcophaga. Indian J Med Microbiol. 2010;28:176–8. doi: 10.4103/0255-0857.62503. [DOI] [PubMed] [Google Scholar]
- 11.Zygutiene M, Narkeviciute I, Mudeniene V, Ziliukiene J. A case of myiasis due to Hypoderma bovis, Lithuania, 2004. Euro Surveill. 2006;11:E1–2. [PubMed] [Google Scholar]
- 12.Abram LJ, Froimson AI. Myiasis (maggot infection) as a complication of fracture management.Case report and review of the literature. Orthopedics. 1987;10:625–7. doi: 10.3928/0147-7447-19870401-14. [DOI] [PubMed] [Google Scholar]
- 13.Lukin LG. Human cutaneous myiasis in Brisbane: A prospective study. Med J Aust. 1989;150:237–40. doi: 10.5694/j.1326-5377.1989.tb136454.x. [DOI] [PubMed] [Google Scholar]


