Abstract
Objectives: to investigate whether psychosocial pathways mediate the association between neighbourhood socioeconomic disadvantage and stroke.
Methods: prospective cohort study with a follow-up of 11.5 years.
Setting: the Cardiovascular Health Study, a longitudinal population-based cohort study of older adults ≥65 years.
Measurements: the primary outcome was adjudicated incident ischaemic stroke. Neighbourhood socioeconomic status (NSES) was measured using a composite of six census-tract variables. Psychosocial factors were assessed with standard measures for depression, social support and social networks.
Results: of the 3,834 white participants with no prior stroke, 548 had an incident ischaemic stroke over the 11.5-year follow-up. Among whites, the incident stroke hazard ratio (HR) associated with living in the lowest relative to highest NSES quartile was 1.32 (95% CI = 1.01–1.73), in models adjusted for individual SES. Additional adjustment for psychosocial factors had a minimal effect on hazard of incident stroke (HR = 1.31, CI = 1.00–1.71). Associations between NSES and stroke incidence were not found among African-Americans (n = 785) in either partially or fully adjusted models.
Conclusions: psychosocial factors played a minimal role in mediating the effect of NSES on stroke incidence among white older adults.
Keywords: neighbourhood, psychosocial factors, stroke, older adults
Introduction
Several studies have found associations between neighbourhood characteristics and stroke incidence, [1–6] but limited research has addressed the causal mechanisms through which neighbourhoods may influence stroke incidence, specifically among older adults.
Psychosocial factors, such as depression, social support and social networks, have been hypothesised as pathways connecting neighbourhood and cardiovascular disease (CVD) including stroke [7–8]. Living in a disadvantaged neighbourhood has been shown to be associated with higher levels of depressive symptoms among older adults [9]. The presence of depressive symptoms, in turn, has been associated with a high risk of ischaemic stroke [10].
Disadvantaged neighbourhoods may lack amenities, such as community centres and churches, which may result in fewer social ties that promote social interaction and support [11]. Residing in less affluent areas is associated with lower levels of social activity among older adults [12]. Low social support is associated with a higher risk of CVD mortality [13] and stroke mortality in men [14]. Although empirical evidence about the effects of neighbourhoods on social networks among older adults is sparse, neighbourhood disadvantage appears to be associated positively with social isolation [15]. Pre-stroke social isolation has been associated with a post-stroke composite outcome of MI, stroke recurrence or death [16]. Although several studies have examined the association between the psychosocial features of neighbourhoods and self-reported CVD [17], none has investigated possible psychosocial pathways [7]. This study explores whether the relationship between neighbourhood exposures and incident stroke among older adults is mediated by psychosocial factors, using standardised measures of depressive symptoms, social support and social networks.
Methods
Study population and data sources
Study data are from the Cardiovascular Health Study (CHS), a longitudinal, population-based study of adults aged 65 years and older, from four US counties: Forsyth County, NC; Washington County, MD; Sacramento County, CA and Pittsburgh (Allegheny County), PA. A total of 5,888 whites and African-Americans were recruited between 1992 and 1993. Survey and clinical data were collected at regular intervals until 1999 and surveillance for cardiovascular events and mortality continued through 30 June 2006.
Outcome measure
The outcome variable was adjudicated incident ischaemic stroke. Incident strokes were ascertained through reviews at annual visits, interim telephone contacts, notification of events by participants and review of Medicare hospitalisation data [18].
Measures of neighbourhood characteristics
NSES was measured with a composite variable derived from 1990 US Census data used in other studies of the CHS population [19]. Participants were linked to their neighbourhood of residence using their baseline home address. Four dummy NSES variables were created based on a quartile analysis. Quartile 1 represented the highest residential NSES, and Quartile 4 the lowest. Less than 25% of African-Americans in the highest race-specific quartile overlapped with whites in the cohort, with even less overlap between the race-specific second and third quartiles of NSES for whites and African-Americans. Because of these large racial differences in the distribution of NSES, race-stratified analyses were conducted.
Measures of psychosocial factors
Psychosocial factors included depressive symptoms [Center for Epidemiologic Studies Depression Scale (CES-D)] [20], social support (Interpersonal Support Evaluation List) [21] and social networks [Lubben Social Network Scale (LSNS)] [22] were measured at baseline and annually. For more information about these measures, please see Supplementary data are available in Age and Ageing online, Appendix 1.
Adjustment for potential confounders
We further adjusted for individual sociodemographic, behavioural and biological factors known to affect stroke. Individual socio-demographic factors included: age, gender, total combined family annual income, education and marital status. Behavioural risk factors included smoking, physical activity and alcohol consumption. Biological risk factors included atrial fibrillation, subclinical CVD, hypertension, diabetes and hyperlipidaemia.
Statistical analysis
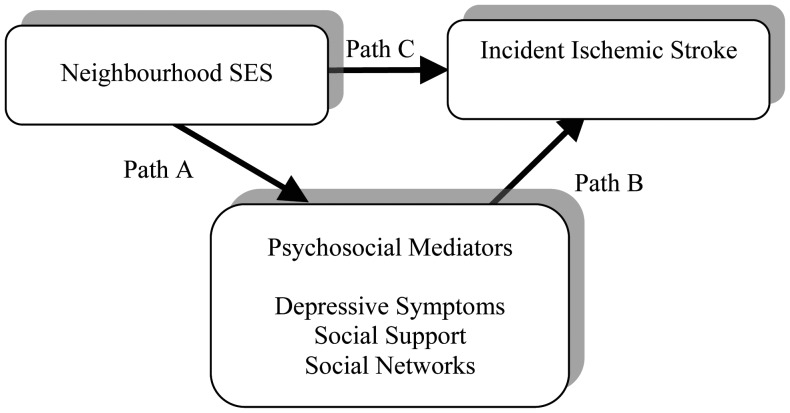
To test the mediating effects of psychosocial factors (Figure 1), we conducted a three-step analysis. First, to examine the relationships between NSES and each psychosocial factors (path A), we conducted a logistic or linear regression analyses to test the associations between NSES and depression, social support and social networks with and without adjusting for individual sociodemographic factors. Secondly, we constructed Cox proportional hazard models to test the associations between each psychosocial factors and time to first ischaemic stroke (path B) with and without adjustment for individual sociodemographic factors. Finally, to determine the extent to which psychosocial factors mediate the association between NSES and incident stroke (path C), we constructed Cox proportional hazard models with sandwich estimates to account for clustering within neighbourhoods. Psychosocial factors were added separately, and then simultaneously, to assess their mediating role in the relationship between NSES and incident stroke. Finally, we added behavioural and biological risk factors to compare the results.
Figure 1.
The mediating effects of psychosocial factors between NSES and incident ischaemic stroke. Age, gender, marital status, individual education and income were adjusted in these pathways.
We conducted two sensitivity analyses. The first used the last available observation for each psychosocial factor prior to incident stroke or censoring. The second used linear slopes of longitudinally measured psychosocial factors over the surveillance period up to incident stroke or censoring.
Results
A total of 4,619 participants with 652 incident strokes were included in the study sample (Table 1). No statistically significant associations were observed between NSES and each of the psychosocial factors (path A; Supplementary data are available in Age and Ageing online Table S1), after adjusting for individual sociodemographic characteristics. Depression, social support and social networks were not associated with stroke after adjusting for individual sociodemographic characteristics (path B; Supplementary data are available in Age and Ageing online Table S2).
Table 1.
Characteristics of the study participants by race
| Whites (n = 3,834) |
African-Americans (n = 785) |
|||
|---|---|---|---|---|
| Incident ischaemic stroke (n = 548) | No incident ischaemic stroke (n = 3286) | Incident ischaemic stroke (n = 102) | No incident ischaemic stroke (n = 683) | |
| NSESa, mean (SD), range, −12.06 to 11.80 | 0.67 (4.67) | 1.17 (4.70)* | −4.43 (4.97) | −5.23 (4.65) |
| Sociodemographic factors, % | ||||
| Age, mean (SD), Range, 64–100 | 73.67 (5.62) | 72.54 (5.56)*** | 73.2 (5.6) | 73.2 (5.2) |
| Female | 59.12 | 57.79 | 73.5 | 62.7* |
| Marital status | ||||
| Married | 68.98 | 69.84 | 38.24 | 47.80* |
| Widowed | 24.45 | 22.36 | 47.06 | 34.60 |
| Divorced or separated | 3.83 | 3.69 | 14.71 | 13.20 |
| Never married | 2.74 | 4.11 | 0.00 | 4.40 |
| Education | ||||
| Less than high school | 30.4 | 25.2** | 47.5 | 43.5 |
| High school or GED | 31.9 | 29.7 | 17.8 | 22.4 |
| Some college | 23.8 | 24.1 | 14.9 | 18.7 |
| College graduate | 8.2 | 10.9 | 9.9 | 5.5 |
| Graduate/professional school | 5.7 | 10.1 | 9.9 | 10.0 |
| Income | ||||
| Less than $12,000 | 23.91 | 19.45 | 46.08 | 48.02 |
| $12,000 to less than $25,000 | 35.22 | 34.78 | 34.31 | 25.18 |
| $25,000 to less than $35,000 | 15.15 | 16.07 | 7.84 | 10.69 |
| At least $35,000 | 20.07 | 23.19 | 5.88 | 9.22 |
| Missing income | 5.66 | 6.51 | 5.88 | 6.88 |
| Psychosocial factors, % | ||||
| Depression | 21.18 | 18.95 | 33.33 | 29.18 |
| Social support, mean (SD), range, 8–24 | 21.85 (2.58) | 21.72 (2.63) | 21.55 (2.70) | 21.49 (2.93) |
| Social networks, mean (SD), range, 0–50 | 32.67 (7.54) | 32.61 (7.13) | 29.94 (8.08) | 31.22 (8.31) |
| Behavioural factors, % | ||||
| Smoking status | ||||
| Never smoked | 48.54 | 46.58 | 56.86 | 47.94 |
| Former smoker | 40.88 | 41.89 | 33.33 | 35.00 |
| Current smoker | 10.58 | 11.54 | 9.80 | 17.06 |
| Alcohol use | ||||
| 0 drinks per week | 50.64 | 45.84 | 76.24 | 64.70* |
| One to seven drinks per week | 37.29 | 40.43 | 15.84 | 28.66 |
| >7 drinks per week | 12.07 | 13.72 | 7.92 | 6.65 |
| Physical activity (kcal in the past 2 weeks) | ||||
| Less than 395 | 26.69 | 21.01* | 39.22 | 40.68 |
| 395 to <1080 | 21.02 | 25.98 | 29.41 | 27.02 |
| 1080 to <2355 | 24.68 | 25.31 | 18.63 | 19.82 |
| 2355–14805 | 27.61 | 27.69 | 12.75 | 12.48 |
| Biologic factors, % | ||||
| Atrial fibrillation | 5.29 | 2.04*** | 1.03 | 1.00 |
| Subclinical cardiovascular disease | 77.37 | 62.99*** | 75.49 | 69.55 |
| Hypertension | ||||
| Normal | 30.90 | 47.27*** | 16.67 | 27.46 |
| Borderline | 15.90 | 15.05 | 12.75 | 13.80 |
| Hypertensive | 53.20 | 37.68 | 70.59 | 58.74 |
| Systolic BP, mean (SD), range, 77–236 | 141.5 (22.8) | 134.5 (21.0)*** | 148.4 (26.0) | 142 (22.5)* |
| Diastolic BP, mean (SD), range, 0–116 | 71.7 (11.9) | 69.8 (11.4)*** | 76.8 (12.2) | 75.9 (12.0) |
| Diabetic status | ||||
| Normal | 66.42 | 74.16*** | 60.42 | 61.67 |
| Impaired fasting glucose | 15.05 | 12.71 | 15.63 | 12.73 |
| Diabetes | 18.53 | 13.14 | 23.96 | 25.61 |
| TC/HDL-C, mean (SD), range, 1.31–10.99 | 4.34 (1.24) | 4.17 (1.26)** | 3.98 (1.11) | 3.78 (1.03) |
aThe quartiles of NSES score for the white participants are: (i) −11.90 to −2.37; (ii) −2.37 to 0.77;
(iii) 0.77 to 4.77 and (iv) 4.77 to 11.80. The quartiles of NSES score for the African-American participants are: (i) −12.06 to −9.25; (ii) −9.25 to −6.06; (iii) −6.06 to −2.63 and (iv) −2.63 to 11.80.
*Significant between incident and no incident ischaemic stroke at P < 0.05.
**Significant at P < 0.01.
***Significant at P < 0.001.
The results of the mediating analyses (path C) are presented in the Table 2. Although a significant association between NSES and stroke was found among whites after adjusting for sociodemographic factors, none of the psychosocial factors mediated this relationship. The hazard ratio for the lowest NSES quartile compared with the highest NSES quartile was reduced only from 1.32 [95% confidence interval (CI) = 1.01–1.73] in Model 1 to 1.31 (CI = 1.00–1.71) in Model 4 and remained non-significant.
Table 2.
Race-stratified multivariate associations between neighbourhood SES and time to incident ischaemic stroke (path C, see Figure 1)
| Model 0: unadjusted | Model 1: adjusted for age, gender, marital status, income and education | Model 2: Model 1 + depression | Model 3: Model 1 + social support and social networks | Model 4: Model 1 + psychosocial factors | Model 5: Model 1 + psychosocial, behavioural and biological factors | |
|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Whites (n = 3,834) | ||||||
| NSES | ||||||
| Q1(highest) (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Q2 | 1.33* (1.05–1.69) | 1.25 (0.98–1.60) | 1.26 (0.98–1.61) | 1.22 (0.96–1.54) | 1.22 (0.96–1.56) | 1.16 (0.90–1.50) |
| Q3 | 1.43** (1.12–1.82) | 1.27 (0.97–1.66) | 1.28 (0.97–1.67) | 1.24 (0.96–1.61) | 1.25 (0.96–1.63) | 1.14 (0.86–1.51) |
| Q4 (lowest) | 1.56*** (1.24–1.97) | 1.32* (1.01–1.73) | 1.34* (1.02–1.76) | 1.29 (0.99–1.68) | 1.31 (1.00–1.71) | 1.14 (0.86–1.52) |
| Depression | — | — | 1.21 (0.97–1.49) | — | 1.24 (0.98–1.56) | 1.18 (0.93–1.49) |
| Social support | — | — | — | 1.01 (0.97–1.05) | 1.02 (0.98–1.06) | 1.02 (0.98–1.07) |
| Social network | — | — | — | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | 1.00 (0.98–1.01) |
| Hazard reductiona | — | Reference | −1.52% | 2.2% | 0.8% | 13.6% |
| African-American (n = 785) | ||||||
| NSES | ||||||
| Q1(highest) (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Q2 | 0.74 (0.44–1.22) | 0.66 (0.39–1.11) | 0.66 (0.39–1.12) | 0.65 (0.38–1.11) | 0.65 (0.38–1.11) | 0.71 (0.40–1.24) |
| Q3 | 0.84 (0.50–1.42) | 0.68 (0.41–1.13) | 0.68 (0.41–1.14) | 0.67 (0.40–1.10) | 0.67 (0.40–1.11) | 0.66 (0.37–1.20) |
| Q4 (lowest) | 0.71 (0.43–1.17) | 0.60 (0.35–1.05) | 0.61 (0.35–1.05) | 0.57 (0.31–1.04) | 0.57 (0.32–1.04) | 0.70 (0.39–1.28) |
| Depression | — | — | 1.20 (0.75–1.92) | — | 1.15 (0.71–1.87) | 1.32 (0.80–2.19) |
| Social support | — | — | — | 1.02 (0.93–1.11) | 1.02 (0.93–1.12) | 1.02 (0.93–1.12) |
| Social network | — | — | — | 0.98 (0.95–1.01) | 0.98 (0.95–1.01) | 0.98 (0.95–1.02) |
| Hazard reductiona | — | Reference | −1.7% | 5% | 5% | −16.7% |
aTaken as the percentage of excess hazard reduction for the model compared with a reference model.
*P < 0.05
**P < 0.01
***P < 0.001.
When behavioural and biological factors were added in Model 5, the reduction in the incident stroke hazard was more substantial—with a proportionate decline of 13.6% in magnitude. Biological risk factors were the primary mediators of the association between NSES and incident stroke [6].
For the African-American cohort, significant associations were lacking in the unadjusted or adjusted models between NSES and incident ischaemic stroke (Table 2).
Similar results were observed in our sensitivity analyses (tables not shown). Although we found stronger effects between NSES and social support and social network when we used the last measured observation for each psychosocial factor prior to either incident ischaemic stroke or censoring, our main findings remain the same. Trajectories of these psychosocial factors did not change the association between NSES and stroke dramatically. However, there was a significant association between the longitudinal increasing depression over time and time to incident ischaemic stroke among whites after adjusting for confounders.
Discussion
This population-based study is to our knowledge, the first to explore the psychosocial pathways between neighbourhood characteristics and incident ischaemic stroke in a large population-based sample of community-dwelling older adults. Our findings suggest that although living in a socioeconomically disadvantaged neighbourhood is associated with an increased risk of ischaemic stroke in white older adults, contrary to our hypotheses, depression, social support and social networks did not act as important mediators in the relationship between NSES and incident ischaemic stroke. Results from our sensitivity analysis show that changes in depression over time were significantly associated with time to incident ischaemic stroke among whites, underscoring the importance of recognising and treating depression in older adults.
The lack of an association between NSES and stroke for older African-Americans may be due to several factors. The sample included a relatively small number of African-Americans who resided in neighbourhoods that were much more disadvantaged than those of the white participants, which may have results in a ceiling effect among the African-Americans and limited our ability to detect a neighbourhood effect. Another important consideration is that older African-American adults may have experienced substantial disadvantage over their life course [23]. Compared with whites, African-Americans have higher stroke incidence rates at a younger age and a lower proportion of them survive to older ages [24]. It is possible that neighbourhood influences on stroke are stronger at a younger age among African-Americans.
The study has limitations that deserve discussion. First, although CHS is a rich data set, it includes participants from only four counties and these findings may not be generalisable to other regions of the USA. Secondly, the sample size of African-Americans was small. Thirdly, the summary neighbourhood score may be an inadequate proxy for neighbourhood features [19]. Additionally, neighbourhood conditions encountered in childhood may have long-term effects on adult health [25]. We did not have the data to investigate the role of NSES over the life course on stroke risks or incorporate information on whether participants changed their neighbourhood among the study period.
Our study suggests that depression, social support and social networks played minimal roles in mediating the association between NSES and incident ischaemic stroke among older adults. Further study is needed to assess the role of other psychosocial pathways. Additionally, future research should also investigate whether psychosocial factors play a role in mediating the effect of NSES on stroke incidence among middle-aged patients.
Key points.
Living in a socioeconomically disadvantaged neighbourhood is associated with an increased risk of ischaemic stroke in white older adults.
Depression, social support and social networks did not act as important mediators in the relationship between NSES and incident ischaemic stroke among white older adults.
The significant association between increasing depression over time and time to incident ischaemic stroke underscores the importance of recognising and treating depression in older adults.
Conflicts of interest
None declared.
Funding
This work was supported by the American Heart Association Pharmaceutical Roundtable -Spina Outcomes Research Center #0875135N and #0875133N as well as by contract numbers N01-HC-85239, N01-HC-85079 through N01-HC-85086, N01-HC-35129, N01 HC-15103, N01 HC-55222, N01-HC-75150, N01-HC-45133, grant number U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. A full list of principal CHS investigators and institutions can be found at http://www.chs-nhlbi.org/pi.htm. A.F.B. was also supported by the NIH/National Center for Advancing Clinical and Translational Science (NCATS)/UCLA Clinical and Translational Science Institute, grant # UL1TR000124.
Supplementary data
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
References
- 1.Engström G, Jerntorp I, Pessah-Rasmussen H, et al. Geographic distribution of stroke incidence within an urban population: relations to socioeconomic circumstances and prevalence of cardiovascular risk factors. Stroke. 2001;32:1098–103. doi: 10.1161/01.str.32.5.1098. [DOI] [PubMed] [Google Scholar]
- 2.Brown P, Guy M, Broad J. Individual socio-economic status, community socio-economic status, and stroke in New Zealand: a case-control study. Soc Sci Med. 2005;61:1174–88. doi: 10.1016/j.socscimed.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Thrift AG, Dewey HM, Sturm JW, et al. Greater incidence of both fatal and nonfatal strokes in disadvantaged areas: the Northeast Melbourne Stroke Incidence Study. Stroke. 2006;37:877–82. doi: 10.1161/01.STR.0000202588.95876.a7. [DOI] [PubMed] [Google Scholar]
- 4.Lisabeth LD, Diez Roux AV, Escobar JD, et al. Neighbourhood environment and risk of ischemic stroke: the Brain Attack Surveillance in Corpus Christi (BASIC) Project. Am J Epidemiol. 2007;165:279–87. doi: 10.1093/aje/kwk005. [DOI] [PubMed] [Google Scholar]
- 5.Morgenstern LB, Escobar JD, Sanchez BN, et al. Fast food and neighbourhood stroke risk. Ann Neurol. 2009;66:165–70. doi: 10.1002/ana.21726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown AF, Liang LJ, Vassar SD, et al. Neighbourhood disadvantage and ischemic stroke: the Cardiovascular Health Study. Stroke. 2011;42:3363–8. doi: 10.1161/STROKEAHA.111.622134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez Roux AV. Residential environments and cardiovascular risk. Bull N Y Acad Med. 2003;80:569–89. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Ann N Y Acad Sci. 2010;1186:146–73. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- 9.Kubzansky LD, Subramanian SV, Kawachi I, et al. Neighbourhood contextual influences on depressive symptoms in the elderly. Am J Epidemiol. 2005;162:253–60. doi: 10.1093/aje/kwi185. [DOI] [PubMed] [Google Scholar]
- 10.Arbelaez JJ, Ariyo AA, Crum RM, et al. Depressive symptoms, inflammation, and ischemic stroke in older adults: a prospective analysis in the cardiovascular health study. J Am Geriatr Soc. 2007;55:1825–30. doi: 10.1111/j.1532-5415.2007.01393.x. [DOI] [PubMed] [Google Scholar]
- 11.Krause N. Neighbourhood deterioration and social isolation in later life. Int J Aging Hum Dev. 1993;36:9–38. doi: 10.2190/UBR2-JW3W-LJEL-J1Y5. [DOI] [PubMed] [Google Scholar]
- 12.Bowling A, Stafford M. How do objective and subjective assessments of neighbourhood influence social and physical functioning in older age? Findings from a British survey of ageing. Soc Sci Med. 2007;64:2533–49. doi: 10.1016/j.socscimed.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Uchino BN. Social support and health: A review of physiological processes potentially underlining links to disease outcomes. J Behav Med. 2006;29:377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 14.Ikeda A, Iso H, Kawachi I, et al. Social support and stroke and coronary heart disease: the JPHC study cohorts II. Stroke. 2008;39:768–75. doi: 10.1161/STROKEAHA.107.496695. [DOI] [PubMed] [Google Scholar]
- 15.Rankin BH, Quane JM. Neighbourhood Poverty and the Social Isolation of Inner-City African American Families. Soc Forces. 2000;79:139–64. [Google Scholar]
- 16.Boden-Albala B, Litwak E, Elkind MS, et al. Social isolation and outcomes post stroke. Neurology. 2005;64:1888–92. doi: 10.1212/01.WNL.0000163510.79351.AF. [DOI] [PubMed] [Google Scholar]
- 17.Augustin T, Glass TA, James BD, et al. Neighbourhood psychosocial hazards and cardiovascular disease: the Baltimore Memory Study. Am J Public Health. 2008;98:1664–70. doi: 10.2105/AJPH.2007.125138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events: the Cardiovascular Health Study. Am J Epidemiol. 1995;5:278–85. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 19.Diez-Roux AV, Kiefe CI, Jacobs DR, Jr, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Am J Epidemiol. 2001;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 21.Cohen S, Mermelstein R, Kamarck T, et al. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Applications. Dordrecht: Martinus Nijhoff Publishers; 1985. pp. 73–94. [Google Scholar]
- 22.Lubben J. Assessing social networks among elderly populations. Fam Community Health. 1988;11:42–52. [Google Scholar]
- 23.Gorelick PB. Cerebrovascular disease in African Americans. Stroke. 1998;29:2656–64. doi: 10.1161/01.str.29.12.2656. [DOI] [PubMed] [Google Scholar]
- 24.Kissela B, Schneider A, Kleindorfer D, et al. Stroke in a biracial population: the excess burden of stroke among Blacks. Stroke. 2004;35:426–31. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 25.Vartanian TP, Houser L. The effects of childhood neighbourhood conditions on self-reports of adult health. J Health Soc Behav. 2010;51:291–306. doi: 10.1177/0022146510378241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.