Abstract
Introduction:
Today’s lifestyle is characterized by increased intake of calories with reduced physical activity, which benefits a real epidemic of obesity in the population. The increase in the prevalence of hypertension in the population follows a significant increase in the prevalence of obesity. Parallel to the trend of increasing the number of older population with increased cardiovascular disease.
The aim:
The aim of our study was to determine the value of body mass index and determine the correlation of obesity and arterial hypertension.
Material and methods:
The study was conducted in family medicine Clinic of the Primary Health Care Center Zenica. Out of 600 patients of both sexes aged over 18 years, randomly are formed groups of 188 patients with hypertension and 189 patients without hypertension of the same gender and same age. The study included patients with primary or essential hypertension, and excluded patients with secondary hypertension, hypertension due to renal disease, pheochromocytoma, coarctation of the aorta, as a result of taking oral contraceptives, corticosteroids, and cocaine. We used the method of anthropometric measurements (body weight, body height from which is calculated the body mass index) measurement of blood pressure with the statistical data processing at the significance level of p <0.05.
Results and discussion:
The increased value of BMI in the sample with hypertension are present in much higher percentage (87.23%), compared to the tested sample without hypertension (60.10%). In patients with hypertension, the highest percentage (51.06%) of the respondents has the BMI in range between 25 and 30, then BMI in the range between 30 and 35 (25%). BMI of 35-40 have 6.38% of patients, and 3.72 patients BMI over 40. In patients without hypertension was significantly smaller percentage of respondents in the previous group (39.15%) with a BMI in the range 25-30, then BMI in the range between 30 and 35 (18.51%). BMI of 35-40 had 3.17% of respondents, and 1.05% of patients had BMI over 40. Correlation between groups of patients with and without hypertension compared to the value of BMI indicate the presence of strong positive correlation (Rho = 0.737). Correlation between groups of subjects with hypertension and without hypertension compared to triglycerides was statistically significant (Rho = 0.123).
Keywords: nutrition, obesity, body mass index, hypertension.
1. INTRODUCTION
In overweight people there is an increased relative risk of hypertension, hypercholesterolemia and diabetes mellitus (1). The Framingham study estimates that obesity may be responsible for 26% of cases of hypertension in men and 28% in women (2). Persistent obesity directly raises blood pressure and makes its control more difficult by interfering with the effectiveness of antihypertensive drugs (3). In contrast to this, loss of body weight leads to lower blood pressure (4, 5), which is important in the prevention and treatment of hypertension (4). For every kilogram lost, systolic and diastolic blood pressure decreases by about 0.5 to 2 mmHg (5).
Obesity is a major health problem in developed countries, and because of its high frequency we are talking about the epidemic of obesity (6). Obesity is no longer just a problem of developed countries, but it has become an increasing problem in developing countries. It is estimated that worldwide there are 1.1 billion adults and 10% of children who are overweight (7). Recent epidemiological studies suggest that according to the number of lost days of healthy life, obesity is among the top ten risks among mass non-communicable diseases (8, 9, 10, 11, 12). Research conducted in the Republic of Serbia (13) showed a significant association between systolic and diastolic blood pressure values and the body mass index, especially in patients over 60 years of age, increasing value of systolic decreases diastolic blood pressure and increases the value of glucose and lipids in the blood.
Studies in Africa suggest that the prevalence of hypertension in urban population is 21.3% and it is associated with body mass index (14). Research conducted in France in 2003 indicates that the prevalence of obesity is 29%; prevalence of hypertension was 24.7% in men, and 22.1% in women, while obesity is cited as a key factor for hypertension (15).
Arterial hypertension, by definition, means the measured value of pressure above normal, at least three times in two different time periods. Normal values are considered to be up to 140/90 mmHg, while optimal values are up to 120/80 mmHg. Timely and proper treatment of hypertension undoubtedly can extend life expectancy and significantly contribute to the success of primary and secondary prevention of cardiovascular disease, and contribute to a better quality of life (16, 17). Arterial hypertension is more than high blood pressure. It is not just a cardiovascular risk factor and highly prevalent chronic disease. Arterial hypertension is, as said by Hymann and Pavlik (18) barometer of efficient education of the population as general indicator of successful health care in the country. Arterial hypertension is a major independent factor of morbidity and mortality, and this was confirmed by the results of Murray and Lopez (19), where it is in the former socialist economies listed as the third risk factor for the lost years of life, just after smoking and alcohol.
2. RESEARCH GOALS
To determine the value of body mass index of respondents.
To correlate obesity and arterial hypertension.
3. MATERIAL AND METHODOLOGY
3.1. Material
The study was conducted in the outpatient Clinic of family medicine at the Primary Health Care Center Zenica. Out of 600 patients of both sexes aged over 18 years we formed randomized groups from 188 patients with hypertension and 189 patients without hypertension of same gender and age. The study involved patients with primary or essential hypertension, and excluded patients with secondary hypertension, hypertension due to renal disease, pheochromocytoma, coarctacio aorta, hypertension as a result of oral contraceptives use, corticosteroids, and cocaine.
3.2. Methods
Anthropometric measurements
Body mass index was calculated based on the relationship between body weight and body height: body weight (kg)/body height (m2). Body height (cm) is measured with anthropometer three times and the mean value was calculated. Weight (kg) is measured at the decimal scale (100 grams of tolerance), which is calibrated before the measurement. Measurement is done with as few clothes as possible three times and then is calculated the mean value.
General physical examination
We performed a general physical examination with measurement of blood pressure (three consecutive measurements taken and mean value calculated). The measured values were categorized according to the instructions of the World Health Organization, with hypertension marked as blood pressure that was ≥ 140/90 mmHg, and then categorized (8):
The first stage–mild hypertension: systolic BP of 140-159 mmHg and diastolic BP 90-99 mmHg;
Second stage–moderate hypertension: systolic 160-179 mmHg, and 100-109 mmHg diastolic BP;
The third stage–severe hypertension: systolic 180-209 mmHg and 110-119 mmHg diastolic BP, and
Fourth stage–very severe hypertension: systolic > 210 mmHg and diastolic BP > 120 mmHg).
Statistical analysis
Data were entered into for this purpose created form for data entry made in MS Access and then imported into the statistical software package SPSS 15.0 and MS Excel 2003, where after the definition of variables statistical data processing is done. The results are presented in the appropriate number of tables and figures, statistically analyzed by descriptive statistics. In order to test statistical significance among the surveyed groups we used the Student t-test, Chi square test at significance level p<0.05.
4. RESULTS
In a prospective study performed in the outpatient Clinic of family medicine at the Primary Health Care Center Zenica out of 600 examined patients of both sexes aged 18 years and older we randomly formed groups of 188 patients with hypertension and 189 patients without hypertension.
The multiple structure of the sample
Gender structure of the sample with hypertension and without hypertension is presented in Table 1.
Table 1.
Gender structure of the sample with hypertension and without hypertension
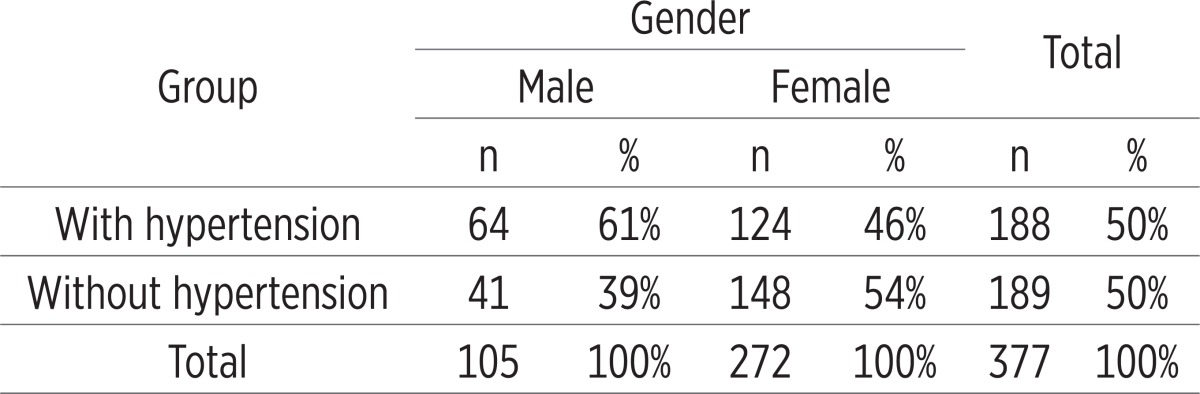 |
From the total number of respondents (377) 105 of them or 27.9% were male, and 272 or 72.1% females.
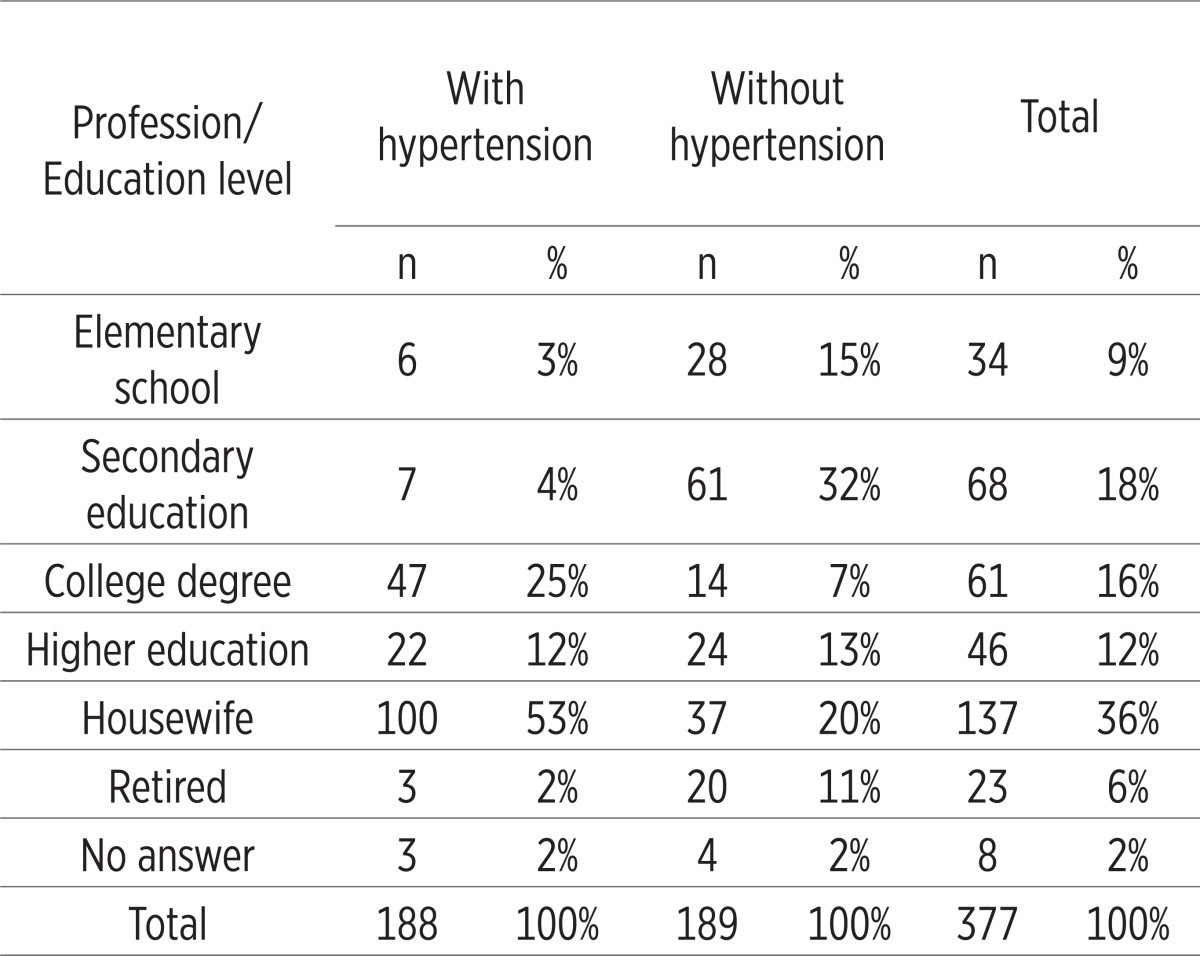
Out of the total number of patients the largest number (36%) were housewives, then with secondary education (18%), college degree (16%), 12% with higher education, elementary school 9% (Table 2).
Table 2.
Profession/education level of the sample with and without hypertension
 |
Anthropometric characteristics of patients-BMI
Based on measured height and body weight was calculated body mass index BMI, in patients with and without hypertension (Table 3).
Table 3.
BMI values in patients with and without hypertension
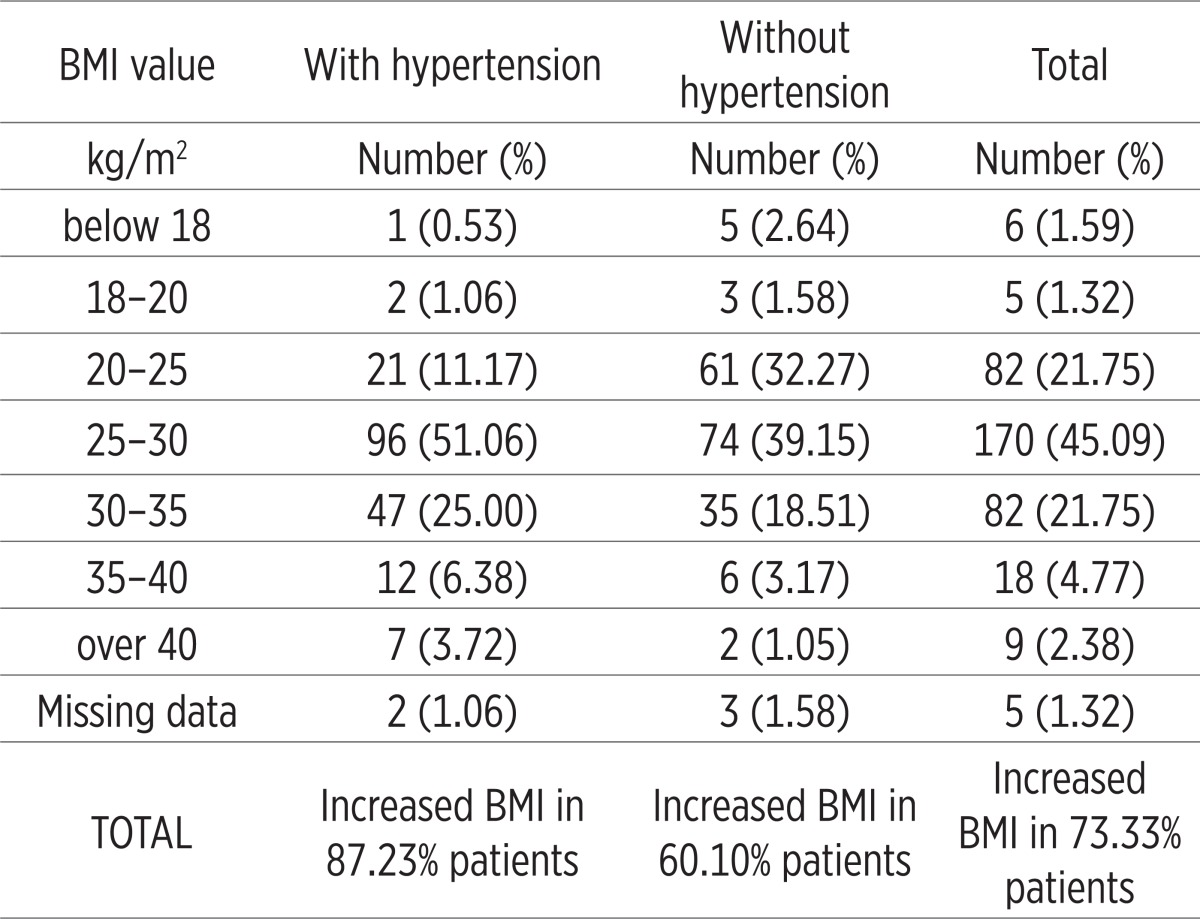 |
Increased value of BMI in the sample with hypertension are present in much higher percentage (87.23%), compared to the tested sample without hypertension (60.10%). In patients with hypertension, BMI was in the range >40 kg/m2 (3.72%) and 25-30 kg/m2 (51.06%), while in 25% the BMI was 30-35 kg/m2. In subjects without hypertension was significantly smaller percentage of respondents in the previous group (39.15%) with a BMI in the range of 25-30, then in the range of BMI between 30 and 35 (18.51%). BMI of 35-40 had 3.17% of respondents, and 1.05% of patients has a BMI over 40.
Correlation between groups of patients with hypertension and without hypertension compared to the value of BMI indicate the presence of strong positive correlation (Rho = 0.737). The mean value of BMI was presented in the following table (Table 4).
Table 4.
The mean value of BMI in patients with and without hypertension
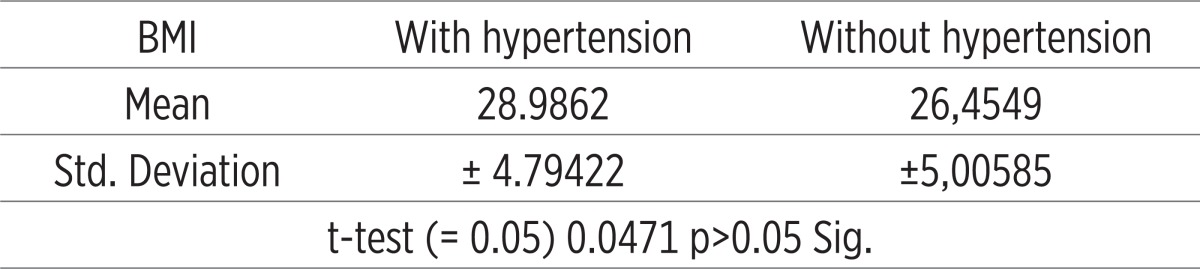 |
Mean BMI values were different between the two groups (with and without hypertension). In both groups of patients, values are elevated, and somewhat higher in the group of patients without hypertension.
5. DISCUSSION
Excess body weight and obesity are the first consequences of nutritional transition and the etiologic agent of mass non-communicable diseases (Anonymous 2002, 2003; 2005). Around 690 million people worldwide suffer from hypertension. At least three million people a year die directly from the consequences of hypertension, while hypertension contributes to many other fatal cases (20). These and similar studies in this area are few, and this research will contribute to clarify the need for prevention activities in terms of lifestyle changes in the field of nutrition and obesity prevention.
The study was conducted in family medicine Clinic of the Primary Health Care Center Zenica. Out of 600 patients of both sexes aged 18 years and older we randomly formed group of 188 patients with hypertension and 189 patients without hypertension of the same gender and age. The study included patients with primary or essential hypertension, and excluded patients with secondary hypertension, hypertension due to renal disease, pheochromocytoma, and coarctation of the aorta, as a result of taking oral contraceptives, corticosteroids, and cocaine. Conducted are anthropometric measurements and general physical examination with measurement of blood pressure. Body mass index is computed based on the relationship between body weight and body height: body weight kg / body height m2. Performed are three consecutive measurements of blood pressure and mean value is calculated. The measured values were categorized according to the WHO instructions, whereby the hypertension is marked as blood pressure equal to or greater than 140/90 mmHg. (16, 17).
The increased value of BMI in the sample with hypertension are present in much higher percentage (87.23%), compared to the tested sample without hypertension (60.10). This is much more than in research conducted in Croatia by Heim and colleagues (18, 21). Their study showed that in the adult population are a little bit more than a fifth of obese ones.
In patients with hypertension, the highest percentage (51.06%) of patients has the BMI in range between 25 and 30, then BMI in the range between 30 and 35 (25%). BMI of 35-40 have 6.38% of patients, and 3.72 patients over 40.
In the group of patients without hypertension there was a significantly smaller percentage of respondents compared to the previous group (39.15%) with a BMI in the range of 25-30, then BMI in the range between 30 and 35 (18.51%). BMI of 35-40 had 3.17% of patients, and 1.05 patients has a BMI over 40.
Contribution of obesity that we obtained in our study is considerably higher than the values that were recorded in the European Union (www.iotf.org). Between 36% and 53% of men is overweight in the European Union. The highest percentage was recorded in Germany (52.9; 2002), Greece (51.1%; 1994-1998), Slovakia (49.7%; 1992-1999) Czech Republic (48.5%; 1997/98), etc. The lowest percentage was in Estonia (35.5; 1994-1998) and France (37.4, 2003). The percentage of women who are overweight is lower, ranging from 24% (France, 2003) up to 37% (Greece, 1994-1998) (18, 19, 20, 21).
According to WHO data in Europe is obese one third of adults (130 millions). The average BMI was 26.5 kg/m2, while the index in Croatia in 2003 amounted to 29.93 kg/m2 (18) and in our study the mean BMI in patients with hypertension was 28.98 kg/m2, while in patients without hypertension was 26.45 kg/m2.
Mean values of body mass index in both groups of patients were increased, while the group of patients with hypertension significantly higher than the group without hypertension. Tests of significance show that there is a statistically significant difference observed between groups.
There was a negative correlation between groups of patients with hypertension and without hypertension in relation to the BMI value (Rho = 0.22). Correlation between groups of patients with hypertension and without hypertension according to the value of BMI is determined the presence of strong positive correlation (Rho = 0.737). Noting that the study of BMI in elementary school Jusupovic (2001) found obesity in 15.2% of children without implementation of any preventive action this large percentage of obesity in this population group could be expected. All this is consistent with the results of ATTICA study conducted in Greece, which confirmed the results of previous studies that obesity is associated with various cardiovascular risk factors such as diabetes, hypertension, and hypercholesterolemia, as is the case in our research. Panagiotakos et al. (22) noted that obese people were less educated, often with sedentary lifestyle, higher consumption of alcoholic beverages, they were prone to unhealthy diet and had the classic cardiovascular risks. Our studies agree with recently published results of the TROPHI (Trial of Preventing Hypertension) study, which showed that 84% of patients with hypertension have excess body weight. According to data of Framingham Heart Study 78% of hypertension in men and 65% of women can be attributed to obesity. There is a linear correlation with BMI, systolic and diastolic blood pressure.
The fact that the 3% of patients with hypertension and 5% without hypertension stated that obesity has no effect on the health speaks among other things, about the need for preventive work in order to increase level of health culture. Total cholesterol values in patients with hypertension for 57.97% of the cases were increased, which is much higher than in patients without hypertension, 2.32%. Correlation between groups of patients with hypertension and without hypertension compared to HDL indicate the presence of strong negative correlation (Rho = 0.152), while compared to LDL was not statistically significant (Rho = 0.018). Correlation between groups of patients with hypertension and without hypertension compared to triglycerides was statistically significant (pc = 0.123).
6. CONCLUSION
The increased value of BMI in the tested sample with hypertension are present in much higher percentage (87.23%), compared to the tested sample without hypertension (60.10%) with the existence of strong positive correlation (Rho = 0.737).
The mean value of the BMI in patients with hypertension was 28.98 kg/m2, while in those without hypertension 26.45 kg/m2.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Must A, Spadano J, Coakley EH, Field AE, Coldit G, Dietz WH. The disease burden associated with over weight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 2.Wilson PW, D“Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risc: the Framingham experience. Arch Intern Med. 2002;162:1867–1872. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- 3.Modan M, Almos S, Fuchs Z, Chetrit A, Lusky A, Halkin H. Obesity, glucose intolerance, hyperinsulinemia, and response to antihypertensive drugs. Hypertension. 1991;17:565–573. doi: 10.1161/01.hyp.17.4.565. [DOI] [PubMed] [Google Scholar]
- 4.Neter JE, Stam BE, Kok FJ, Grobbee DE, Gelijanse JM. Influence of weight reduction on blood pressure: a meta –analysis of randomized controlled trials. Hypertension. 2003;42:878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 5.Bray A.G, Chobanian AV. Predicting obesity in adults from childhood and adolescent weight. Am J Clin Nutr. 2002;76:497–498. doi: 10.1093/ajcn/76.3.497. [DOI] [PubMed] [Google Scholar]
- 6.Haslam DW, James WP. Obesity. Lancet. 2005;366:1197–1209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- 7.Anonymous. Evaluation and Treatment of High Blood Pressure. The fifth report of the The Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNCV) Arch. Intern. Med. 1993;153:154–183. [PubMed] [Google Scholar]
- 8.Anonymous. Reducing Risks, Promoting Healthy Life. Geneva: World Health Organisation; 2002. [Google Scholar]
- 9.Anonymous. Diet, nutricion and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation, Geneva. 2003. pp. 4–132.
- 10.Anonymus. WHO Tehnical Report Series No.916. DIET, NUTRITION AND THE PREVENTION OF CHRONIC DISEASES. Report of a Joint WHO/FAO Expert Consultation, Geneva. 2003.
- 11.Anonymus. WHO. The World Health Report. Shaping the Future. Geneva: World Health Organisation; 2003. [Google Scholar]
- 12.Smjernice za dijagnostiku i liječenje arterijske hipertenzije. Zagreb: Hrvatsko kardiološko društvo; 2004. Anonymus. Europsko društvo za hipertenziju, Europsko kardiološko društvo 2003. [Google Scholar]
- 13.Pantelinac P. Nutricija, tretman i kardiovaskularni faktori rizika sa međunarodno prihvaćenim preporukama za prevenciju ateroskleroze. Novi Sad: Društvo fiziologa Srbije; 2007. Ishrana i njen značaj u lečenju šećerne bolesti; pp. 121–131. [Google Scholar]
- 14.Longo-Mbenza B, Nkoy Belila J, Vangua Ngoma D, Mbungu S. Prevalence and risk factors of arterial hypertension among urban Africans in workplace: the obsolete role of body mass index. Niger J Med. 2007;16(1):42–49. doi: 10.4314/njm.v16i1.37280. [DOI] [PubMed] [Google Scholar]
- 15.Atallah A, Inamo J, Lang T, Larabi L, Chatelher G, Rozet JE, Machuron C, De Gaudemaris R. Prevalence of hypertension in a disadvantag ed population in Antilles: a major role for obesity. Arch Mal Coeur Vaiss. 2007;100(1):22–27. [PubMed] [Google Scholar]
- 16.Obesity and overweight. Geneva: World Health Organisation; 2004. Anonymous. Global strategy on diet, physical activity and health. [Google Scholar]
- 17.Anonymous. Preventinng chronic diseases: a vital investiment. Geneva: World Health Organisation; 2005. [Google Scholar]
- 18.Hyman D, Pavlik V. Self-reported hypertension treatment practices among primary care physicians. Arch Intern Med. 2000;160:2281–2286. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 19.Ðurić D, Jakovljević V. Nutricija, tretman i kardiovaskularni faktori rizika. Novi Sad: Društvo fiziologa Srbije; 2007. Međunarodno društvo za aterosklerozu: usklađene preporuke za sprečavanje ateroskleroze; pp. 207–233. [Google Scholar]
- 20.Huang Z, Willett WC, Manson JE. i sar. Body weight, weight change, and risc for hypertension in women. Ann Intern Med. 1998;128:81–88. doi: 10.7326/0003-4819-128-2-199801150-00001. [DOI] [PubMed] [Google Scholar]
- 21.Jovanovski Z, Vasiljević N, Damjanov V, Kašanin J, Knežević T. Nutricija, tretman i kardiovaskularni faktori rizika. Novi Sad: Društvo fiziologa Srbije; 2007. Stanje uhranjenosti starih osoba urbane i ruralne sredine kao faktor rizika za pojavu kardiovaskularnih bolesti; pp. 45–58. [Google Scholar]
- 22.Pantagiotakos DB, Pitsavos C, Chrysohoou C. i sur. Epidemiclogy of overweight and obesity in a Greek adult population: ATTICA Study. Obesity Research. 2004;12:1914–1920. doi: 10.1038/oby.2004.239. [DOI] [PubMed] [Google Scholar]


