Abstract
Goal:
To measure change in a quality of life after treatment with removable dentures and to describe differences in quality of life in patients with new and worn out dentures.
Materials and methods:
Measuring instrument was OHIP-49, translated from English into one of the languages in Bosnia-Herzegovina. Sample consisted of patients who wanted to make/replace mobile dentures or came to repair a broken dentures. Comprehensibility of the OHIP-BH49 was tested on a sub-sample of patients. Three measurements were made: before and after the insertion of dentu res and when patients came to repair their mobile dentures.
Results:
Sample consisted of 67 patients: 32 patients who sought prosthetic treatment, and 35 who came to repair their broken dentures. We received 89.7% correctly filled questionnaires. Minor changes were made in four (4) questions. Statistical analysis performed with the T-test revealed the significant differences, before and after the treatment with mobile dentures (t=39.5, p<0.001). There was a significant difference in OHIP scores in patients with a new dentures, compared to the patients who had worn out dentures (t=44.30, p<0.001). Substantial differences, between OHIP scores, regarding the time of wearing dentures or patients’ age were not observed.
Discussion:
Patients who wore dentures longer than 5 years, showed better quality of life, because they became accustomed to the dentures.
Conclusions:
Self-reported life quality improved considerably after insertion of a new dentures. Patients with a new dentures showed significantly better quality of life than patients with worn out dentures. One part of OHIP validation in Bosnia-Herzegovina has been done.
Key words: quality of life, prostheses, validation studies, OHIP-49.
1. INTRODUCTION
Dental problems have high prevalence and, like many other diseases, they are affecting various aspects of life: economical, social, physical and psychological. Social implications of oral diseases were often in the shadow of social implications some other medical conditions.
Susan Reisine was the first researcher in the field of social dimensions of dental problems. Reisine compared the work day’s loss as a consequence of various acute conditions and concluded that implications of dental problems can be as serious as social impacts of some other diseases (1). Later, during late eighties and nineties, a large number of indices were developed for assessing social dimensions of dental illness (2). OHIP (Oral Health Impact Profile) is a commonly used questionnaire for assessing Oral Health Related Quality of Life (OHRQoL).
OHIP consists of 49 questions, divided into seven constitutive domains: functional limitations (nine questions), physical pain/discomfort (nine questions), psychological discomfort (five questions), physical disability (nine questions), psychological disability (six questions), social disability (five questions) and handicap (six questions).
1.1. Development of OHIP
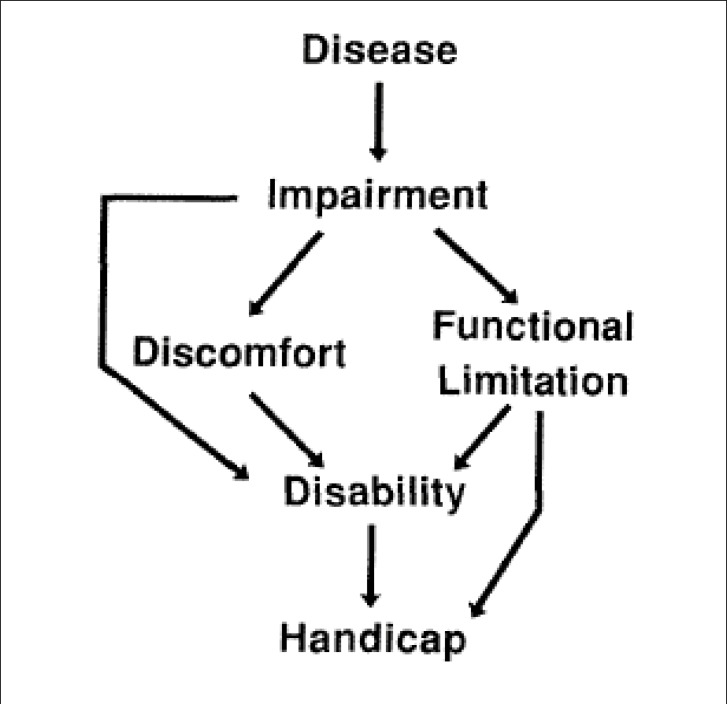
English-language version of OHIP was developed in Australia by Gary D. Slade and A. John Spencer. OHIP was presented in 1994 (3). The conceptual framework used for development of OHIP was Locker’s model of oral health based on the International classification of impairments, disabilities and handicaps, Figure 1.
Figure 1.
Locker´s model of oral health.
The OHIP questionnaire was translated into many languages (4-9). OHIP must be adapted if used in cultural unique region. For example, there are two OHIP versions in same language that are used in two different countries (10, 11).
OHIP is an important instrument in defining social impacts of oral disorders, in oral health promotion and in evaluation of dental treatment.
OHIP can be a part of the medical documentation; it can be used to estimate results of health services, to evaluate benefits of dental treatment, and to analyze relationship between patient’s benefits of the therapy and its financial cost.
OHIP is not suitable for people with limited cognitive or language skills, for children, and it can not be used in situations when there is no enough time or other conditions to fill out the questionnaire (12).
Some authors concluded that OHIP-49 can not be used for evaluation of dental appearance and aesthetics (13).
Period of time covered by this questionnaire has not been determined by the Australian authors of the OHIP. It can be any period that best suits the researcher.
2. GOAL
The OHIP-49 has never been used in Bosnia and Herzegovina before. The aim of this study was to translate the original English-language version into the one of the languages in Bosnia and Herzegovina, following the guidelines for cross-cultural adaptation and to examine responsiveness of this questionnaire.
Another intention of the present study was to compare quality of life (QoL) in patients who received new dentures, with life quality in patients before therapy. The goal of the study was to compare QoL in patients who received new dentures with QoL in patients who have worn out dentures. The aim of the study was also to find association between:
time of wearing dentures,
age of the patient
and QoL measured by OHIP.
3. MATERIALS AND METHODS
3.1. Instrument
Oral Health Impact Profile is a questionnaire that quantitatively determines impact of oral diseases on oral health related quality of life (3). OHIP has 49 items.
Answers to questions are given in the form of Likert scale with a maximum of 4 points per item (never=0, almost never = 1, sometimes=2, fairly often=3, very often = 4). OHIP-49 is a simple sum of codes.
Total OHIP-49 and sum for each domain indicate the subjective experience of OHRQoL (13). The larger is the sum, the poorer is the quality of life. OHIP can vary from 0 to 169.
3.2. Translation of OHIP-E49
OHIP-BH49, Appendix 1, has been developed translating OHIP-E49 into the Bosnian language by a forwardbackward translation method, with assistance of several translators. A specialist in prosthetic dentistry and a certified translator translated the English version of the questionnaire independently. Another translator, laic, translated the German version (OHIP-G53). All three translators were native Bosnian speakers. Translated questionnaires were compared and discussed. After debate, resulting version has been back translated into English by second certified translator and compared to the original. Substantial differences were not observed.
At the end of this phase we had the preliminary version of OHIP-BH49.
This version was applied to the subsample of patients in a form of an interview, to check the comprehensibility of the language used in the questionnaire.
3.3. Study sample and procedures
Sample consisted of patients who visited The Department of Prosthetic Dentistry at the Health Center “Dom zdravlja Stari Grad” (Public Institution Health Center of Sarajevo Canton), for a period of about 6 months. The aim of their visit was to make a new denture or to repair broken one. General information (year of birth), and denture data (type and time of wearing) were taken after the clinical examination.
Methods of administration were: printed questionnaire and face-to face interview.
Three measurements were made:
Before getting new dentures,
7-14 days after insertion of dentures,
When a patient brought worn out (broken) dentures.
Exclusion criteria were:
Broken dentures less than two years old, and
Missed answers in 5 or more items per questionnaire or two (and more) in a domain.
For each of 49 questions, study participants were asked to declare how much often they experienced described problem in the past few weeks (first and third measurement), and in the last 2-4 days (second measurement).
T-test, ANOVA test and Chi-square test were used for data analyses.
The significance level was p=0.05 for all tests.
4. RESULTS
First group of participants (N=32, 47% females) consisted of patients who wanted to replace old dentures or to make a new one. Second group of patients (N=35, 54% females) came in order to repair their broken dentures. In the first group of patients, seven of 32 wore dentures 2-5 years, 20 wore dentures longer than 5 years and 5 patients previously had no dentures. 14 of them were older than 50 years. In the second group of patients, 9 of 35 wore dentures shorter than 5 years. 25 of them were older than 50 years.
4.1. Missing data and percentage of correctly completed questionnaires
Seven patients were excluded due to missing data. Two of them wanted new prostheses and five came to repair their dentures. In total, we had 89.6% correctly completed questionnaires. Face-to-face interview resulted with 100% completely filled questionnaires.
4.2. Linguistic and cross-cultural adaptation
During the face-to-face interview on a subsample of patients (N=25), subjects had minor difficulties in understanding of some items. To make questionnaire more comprehensive, we made adjustments in four questions:
Q4: „osjećaj da su utjecali na vaš izgled“replaced with „negativno utjecali na vaš izgled“,
Q14: „bolovi u zubu“replaced with „imali zubobolju“,
Q17: “bolna mjesta“replaced with „bolna mjesta (tačke) “, because the item reffers to aphtae,
Q27: “ne možete dobro čistiti zube“; new item is „očetkati zube“,
Q41: „teže komunicirali sa drugim ljudima“replaced with „teže izlazili na kraj sa drugim ljudima“.
The final OHIP-BH49 version was completed after those adjustments, Appendix 1.
4.3. Statistical analysis performed with the T-test for patients with new dentures
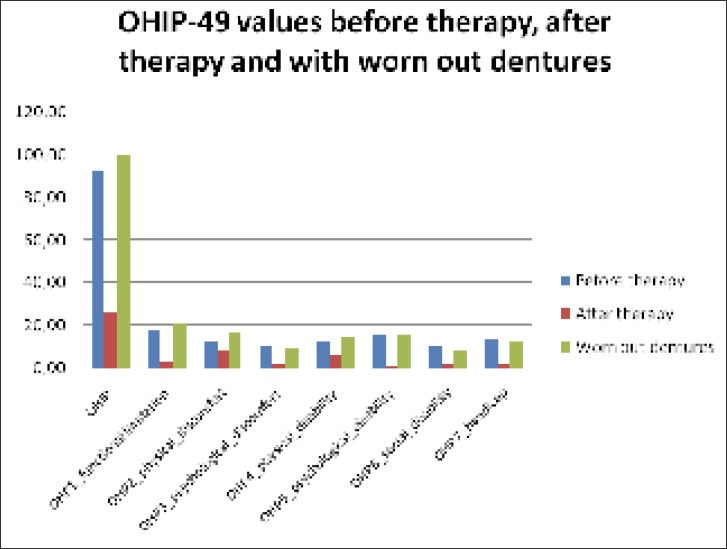
QoL in patients was much better after receiving new dentures. Patients with new dentures showed much better QoL than patients with worn out dentures, Chart 1.
Chart 1.
OHIP-49 values in patients before therapy with mobile dentures, after the therapy with new dentures and with worn out dentures.
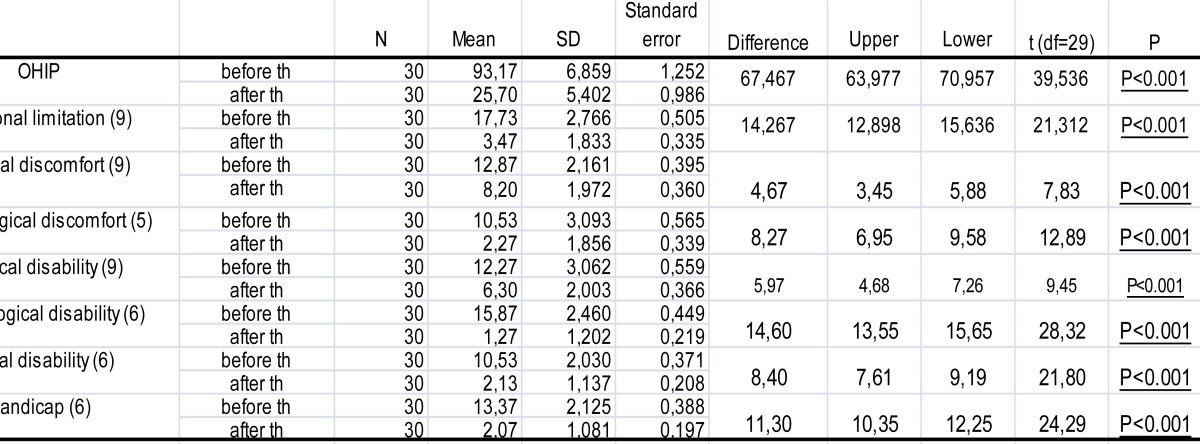
Statistical analyses performed with the T-test revealed significant differences for total OHIP and for each of the seven domains (p<0.001), Table 1 and 2.
Table 1.
T-test of differences in OHIP-BH49 scores between patients with new and worn out dentures (HC“DZ Stari Grad”, Sarajevo, 2010)
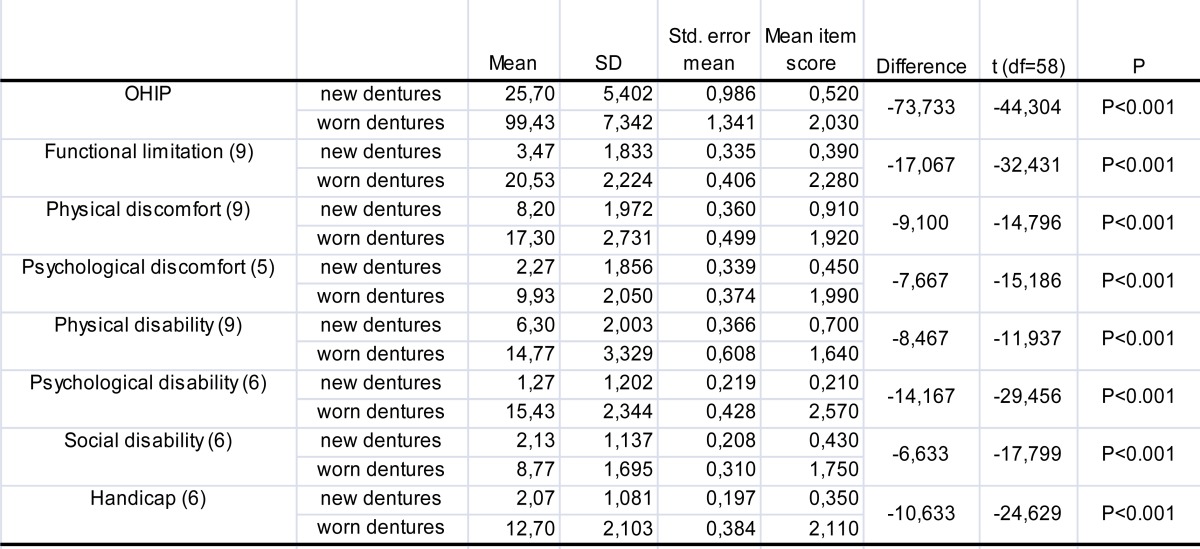 |
Table 2.
Comparison of OHIP-BH49 values before and after therapy using T-test on a study sample of 30 patients who received removable dentures (HC“DZ Stari Grad”, Sarajevo, 2010)
 |
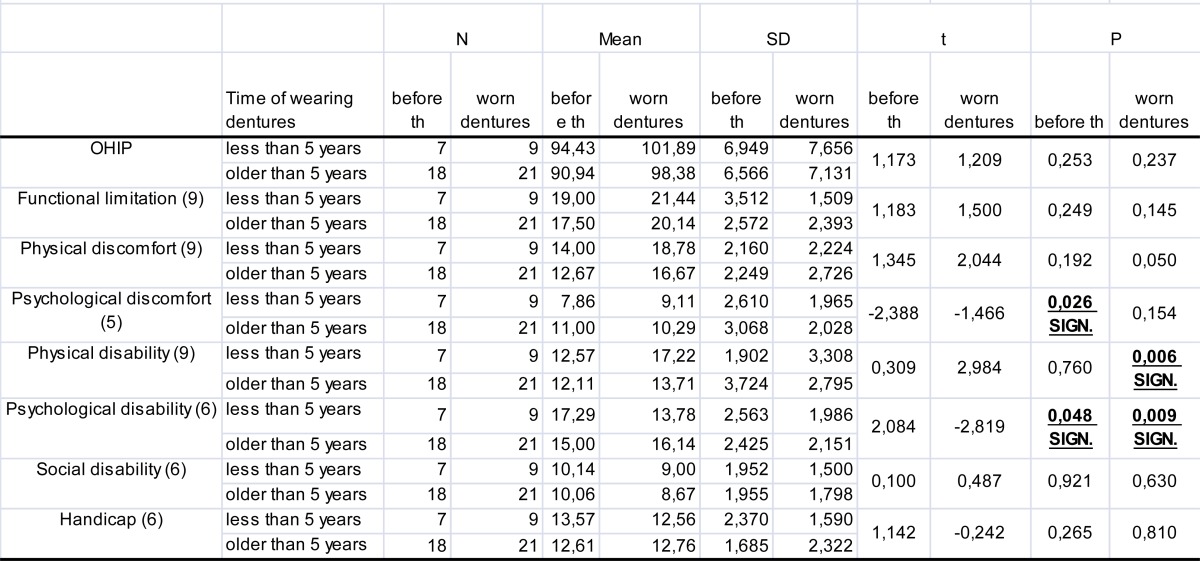
Statistical analysis performed with the T-test for time of wearing dentures.
We compared QoL of patients with dentures less than 5 years old to the QoL with dentures older than 5 years.
Patients who wore dentures longer than five years had better QoL.
Statistical analysis performed with the T-test revealed significant differences for two domains in our first measurement and for the same number of domains in third measurement. In every measurement, older dentures showed significantly better QoL in one domain, and newer dentures showed significantly better QoL in another. For total OHIP, no significant differences were found, Table 3.
Table 3.
Multiple comparison of OHIP-49 for time of wearing dentures using T-test.
 |
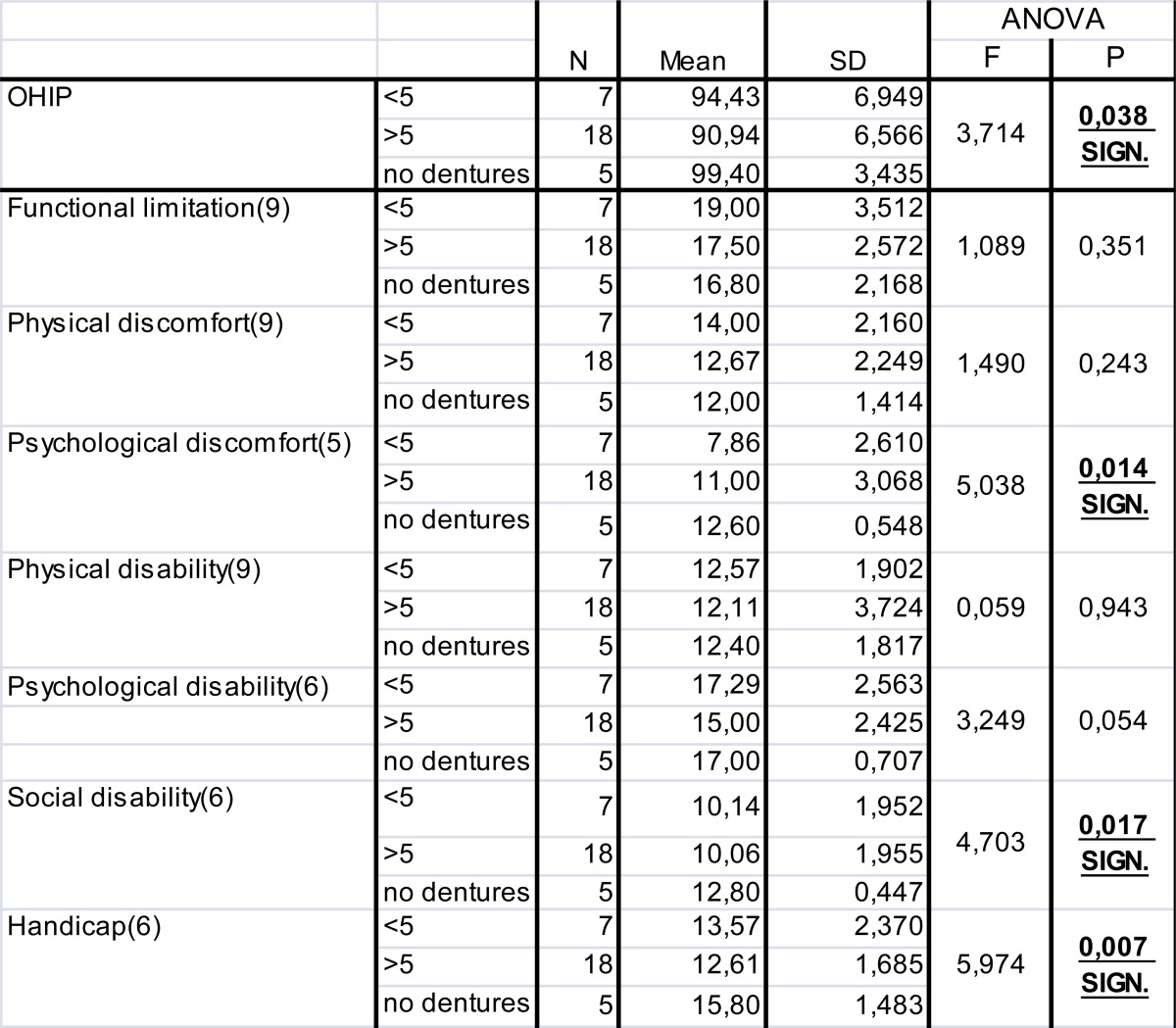
Statistical analysis performed with the ANOVA-test for time of wearing dentures Statistical analysis with ANOVA in our first measurement revealed significant differences in OHIP values between patients without dentures, with dentures less than 5 years old and with dentures older than 5 years for total OHIP and for three domains (p<0.05), Table 4. ANOVA test of differences in OHIP values among patients who wore dentures less than 5 years, longer than 5 years and who had no dentures before receiving one.
Table 4.
ANOVA test of differences in OHIP values among patients who wore dentures less than 5 years, longer than 5 years and who had no dentures before receiving one.
 |
Statistical analysis performed with the Chi-square test for time of wearing dentures. Chi-square tests for time of wearing dentures in a sample of 55 patients who had dentures before therapy or had worn out dentures find no significant differences (Pearson’s chi square = 5:48, p = 0065: p> 0.05).
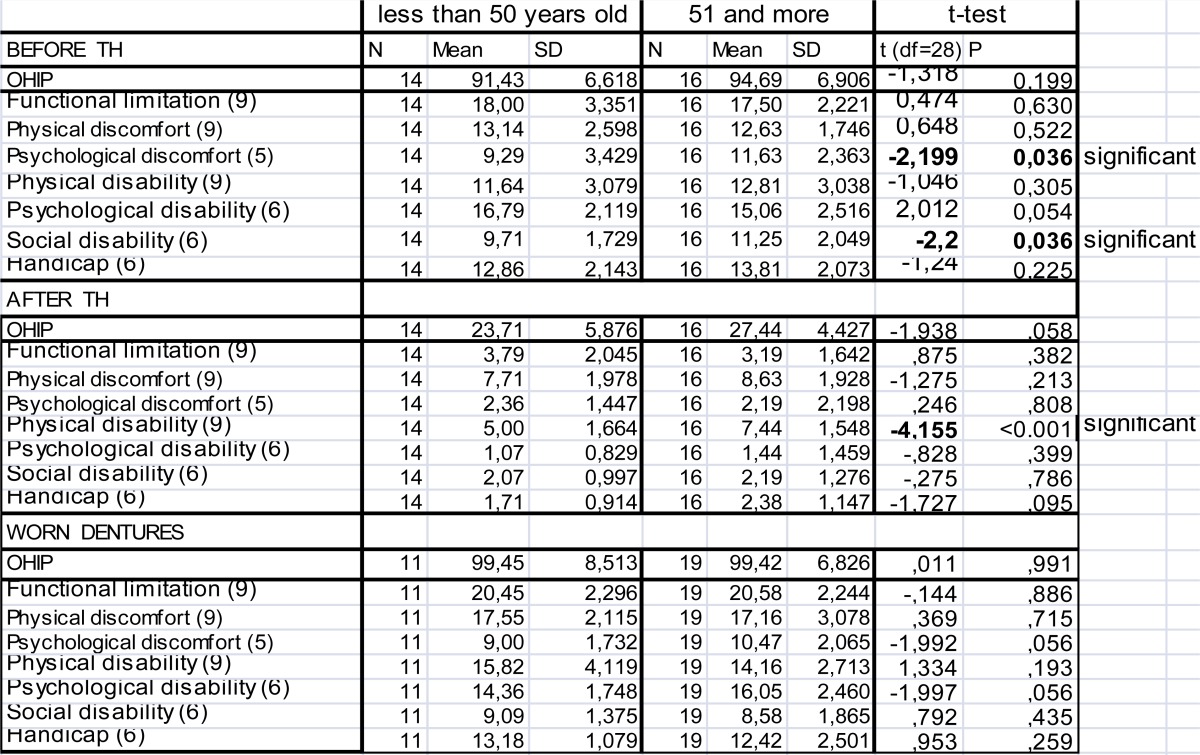
4.4. Statistical analysis performed with the T-test for patients’ age
Before and after receiving new dentures, patients older than 50 years had higher total OHIP and higher values in majority of domains. In our third measurement, patients younger than 50 had higher total OHIP and higher values in four domains.
T-test revealed significant differences in OHIP values in two domains in our first measurement and in one domain in our second measurement. In third measurement there were no significant differences. Older patients had poorer QoL in all domains with significant differences.
We had no significant differences for total OHIP, Table 5.
Table 5.
Multiple comparison of differences in OHIP values between patients younger/older than 50 years using T-test
 |
5. DISCUSSION
In our study, patients with new dentures showed significantly better QoL compared to pre-treatment period and compared with patients with worn out dentures. Patients’ age and time of wearing dentures had no significant impact on QoL with dentures. Correlation between oral health conditions and life quality is scientifically more and more interesting. Various instruments have been developed in order to identify the way dental problems (problems with teeth, oral cavity, jaws and dentures) interfere with people’s daily lives (3). Most questionnaires have been produced in English-speaking countries, although interest in developing their own instruments has arisen in other countries. The aim of this study was to make conditions for use of OHIP-49 in Bosnia and Herzegovina. In the present study, the original English-language Oral Health Impact Profile was translated into the Bosnian language, mostly following the international guidelines for linguistic and cross-cultural adaptation of self-reported measures (14, 15).
Where the international guidelines suggest a small-scale field test to be performed prior to the implementation of a new instrument, comprehensibility testing of the preliminary version of OHIP-BH49 was done during the application of the questionnaire to the subsample (part of the main study group, N=25). No pilot-study was performed before the main study. During the interview, however, we used to ask subjects about difficulties in understanding items or frequencies. Despite this minor departure from the recommended procedure, we have confidence in the quality of the translation process, because items that showed signs of misunderstanding were changed right away (item was applied to the next interviewed person). We had to make minor changes in only four questions.
The patients’ compliance was good. Even though the OHIP-BH49 consists of many questions, most patients seemed willing to make a statement about the perceived negative effects of their dental condition. The questionnaire’s length seems not to be a factor that will interfere with the collection of the OHIP-BH data.
In some previous studies, code from every answer was multiplied by the importance coefficient, in order to get the OHIP final score (16, 17). In present study, question coefficients were not determined or used, because they did not result in improvements of measurement properties (17).
Our study demonstrated that new dentures are associated with better OHRQoL. Many authors have concluded that getting new dentures would improve QoL. Significant differences were found in all of seven domains or in a majority of domains (10, 13). In the present study, patients completed OHIP questionnaire 7-14 days after the placement of new dentures.
According to the available literature, OHIP is changing immediately after obtaining prosthesis. These changes, as the time goes by, seem to be much slower (18, 19).
Higher values of total OHIP, but not significantly, were recorded in patients older than 50 years. Older patients had worse QoL in all domains with statistical significance. In one study, with increasing age of subjects for 10 years, mean OHIP score increased by 1.7 units (20). Many researchers concluded that time of wearing dentures and the age of the patient have no impact on the quality of life (4, 5, 9, 19, 20).
6. CONCLUSIONS
Patients with new dentures had significantly better QoL compared with the QoL in subjects with worn dentures.
QoL in patients 7-14 days after insertion of new prosthesis was significantly better compared with QoL before therapy.
Patients who needed dentures, and previously had no dentures, showed significantly worse QoL compared with patients who had old dentures before receiving the new one.
Time of wearing dentures had no significant impact on QoL. Patients who wore dentures longer than five years had better QoL but the difference was not significant.
Patients’ age did not have significant effect on the QoL. Older patients had slightly poorer QoL.
A part of the validation process of OHIP-49 for Bosnia and Herzegovina has been done.
The initial steps towards validation of OHIP-49 in B&H setting, conducted in present research, were: Translation of OHIP into Bosnian language using the forward-backward translation technique. Product was the preliminary Bosnia-Herzegovina version of the OHIP-49.
Evaluation of language and cross-cultural adaptation: OHIP was applied in a form of the interview to a subsample of patients (N=25). Some items were adjusted to clarify the questions. Testing responsiveness of the OHIP-BH49. Responsiveness was tested on 32 patients in a treatment demand (new dentures). Patients completed the OHIP questionnaire twice, before and after treatment. Mean score difference was significant. Before considering OHIP-BH49 as a suitable instrument for assessment of oral health quality of life in Bosnia and Herzegovina, we must evaluate the properties of OHIP-BH49 as a measuring instrument in a separate research.
Acknowledgements
Author is thankful to Ms. Selma Hadžipašić for translation of the German version of OHIP.
Appendix 1
OHIP-BH49 (The Bosnia and Herzegovina version of The Oral Health Impact Profile)*
Ponuđeni odgovori su: 0=nikad, 1=skoro nikad, 2=ponekad, 3=prilično često, 4=veoma često Molim zaokružite broj pored odgovora s obzirom na to koliko ste često iskusili opisanu poteškoću u vremenskom periodu od ....
Ograničenje funkcije
Da li ste
imali poteškoće prilikom žvakanja hrane zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima?
imali poteškoće prilikom izgovaranja riječi zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima?
primijetili da neki Vaš zub ne izgleda kako treba ?
imali osjećaj da su problemi sa zubima, usnom šupljinom ili protetskim nadomjescima negativno utjecali na Vaš izgled ?
imali utisak neuobičajenog, ustajalog mirisa iz usta koji je bio uzrokovan problemima sa zubima, usnom šupljinom ili protetskim nadomjescima?
imali osjećaj da Vam se osjet okusa izmijenio zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
primjetili da se hrana zadržavala tokom jela na zubima ili protetskim nadomjescima ?
imali osjećaj da Vam se probava pogoršala zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
imali osjećaj da Vam protetski nadomjesci loše naliježu?
Tjelesna nelagodnost
Da li
10. ste imali osjećaj dugotrajne boli u ustima?
11. ste imali osjećaj bolne čeljusti ?
12. ste imali glavobolju zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima?
13. ste imali osjećaj osjetljivih zuba, npr . pri uzimanju hladne ili vruće hrane ili pića?
14. ste imali zubobolju?
15. ste imali bolove u zubnom mesu?
16. ste imali nelagodnosti pri konzumiranju neke hrane zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
17. ste imali bolna mjesta (tačke) u ustima ?
18. su Vas žuljale proteze?
Psihološka nelagodnost
Da li
19. ste bili zabrinuti zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
20. Vas je brinulo šta drugi ljudi misle o Vama zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
21. Vam je bilo teško zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
22. Vam je bilo nelagodno zbog izgleda Vaših zuba ili protetskog nadomjeska?
23. ste bili napeti zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Tjelesna onesposobljenost
Da li
24. ste nerazgovjetno govorili zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima?
25. su drugi ljudi pogrešno razumjeli neke Vaše riječi zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima?
26. ste imali utisak da je hrana lošijeg ukusa zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
27. Vam se desilo da ne možete dobro očetkati svoje zube zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
28. ste morali izbjegavati neku vrstu hrane zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
29. Vam je ishrana postala nedovoljna zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
30. Vam se desilo da niste mogli jesti svojim protezama zbog problema sa njima ?
31. Vam se desilo da ste izbjegavali nasmijati se zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
32. Vam se desilo da ste morali prekinuti obrok zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Psihološka onesposobljenost
Da li Vam se desilo da
33. Da li Vam se desilo daVam je prekinut san zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
34. Da li Vam se desilo da ste bili uznemireni zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
35. Da li Vam se desilo da ste imali poteškoću opustiti se zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
36. Da li Vam se desilo ste bili potišteni ili depresivni zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
37. Da li Vam se desilo da ste se teško koncentrirali zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
38. Da li Vam se desilo da ste se osjećali postiđeno zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Socijalna onesposobljenost
Da li
39. Vam se desilo da ste izbjegavali izaći zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
40. ste bili manje tolerantni u odnosima sa bračnim partnerom ili članovima porodice zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
41. ste uopšte teže izlazili na kraj sa drugim ljudima zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
42. Vam se desilo da ste bili razdražljivi prema drugim ljudima zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
43. ste imali poteškoće u obavljanju uobičajenih poslova zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Hendikep
Da li ste
44. imali utisak da Vam se cjelokupno zdravlje pogoršalo zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
45. pretrpjeli neki finansijski gubitak koji je bio u vezi sa problemom sa zubima, usnom šupljinom ili protetskim nadomjescima?
46. osjetili da Vam društvo drugih ljudi nije tako ugodno kao ranije zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
47. imali utisak da je Vaš život sve skupa manje zadovoljavajući zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
48. bili potpuno nesposobni funkcionirati zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
49. iskusili da ne radite nešto svojim uobičajenim, punim kapacitetom zbog problema sa zubima, usnom šupljinom ili protetskim nadomjescima ?
Footnotes
The English version of OHIP-49 is available elsewhere (3).
REFERENCES
- 1.Reisine ST. Dental Health and Public Policy: The Social Impact of Dental Disease. American Journal of Public Health. 1995;75(1) doi: 10.2105/ajph.75.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen PF. Assessment of oral health related quality of life. Health and Quality of Life Outcomes. 2003;1:40. doi: 10.1186/1477-7525-1-40. doi:10.1186/1477-7525-1-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 4.John MT, Patrick DL, Slade GD. The German version of the Oral Health Impact Profile - Translation and psychometric properties. Eur J Oral Sci. 2002;110:425–433. doi: 10.1034/j.1600-0722.2002.21363.x. [DOI] [PubMed] [Google Scholar]
- 5.Larsson P, List T, Lundstroem I, Marcusson A, Ohrbach R. Reliability and validity of a Swedish version of the Oral Health Impact Profile. J Dent Res. 2003;82:245. doi: 10.1080/00016350410001496. [DOI] [PubMed] [Google Scholar]
- 6.Ide R, Yamamoto R, Mizoue T. The Japanese version of the Oral Health Impact Profile (OHIP) - validation among young and middle-aged adults. Community Dent Health. 2006 Sep;23(3):158–63. [PubMed] [Google Scholar]
- 7.Saub R, Locker D, Allison P, Disman M. Cross-cultural adaptation of the Oral Health Impact Profile (OHIP) for the Malaysian adult population. Community Dent Health. 2007 Sep;24(3):166–75. [PubMed] [Google Scholar]
- 8.Al-Jundi MA, Szentpétery A, John MT. An Arabic version of the Oral Health Impact Profile: translation and psychometric properties. Int Dent J. 2007 Apr;57(2):84–92. doi: 10.1111/j.1875-595x.2007.tb00443.x. [DOI] [PubMed] [Google Scholar]
- 9.Van der Meulen MJ, John MT, Naeijew M, Lobbezoo F. The Dutch version of the Oral Health Impact Profile (OHIP-NL): Translation, reliability and construct validity. BMC Oral Health. 2008 Apr 11;8:11. doi: 10.1186/1472-6831-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez R, Baelum V. Spanish version of the Oral Health Impact Profile (OHIP-Sp) BMC Oral Health. 2006 Jul 7;6:11. doi: 10.1186/1472-6831-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castrejón-Pérez RC, Borges-Yáñez SA, Irigoyen-Camacho ME. Validation of an instrument for measuring the effects of oral health on the quality of life of older adults in Mexico. Rev Panam Salud Publica. 2010 May;27(5):321–9. doi: 10.1590/s1020-49892010000500001. (Article in Spanish) [DOI] [PubMed] [Google Scholar]
- 12.Lesaffre E, Feie J, Leroux B. Statistical and Methodological Aspects of Oral Health Research. Publ.John Wiley and Sons; 2009. p. 136. [Google Scholar]
- 13.Mehl C, Kern M, Freitag-Wolf S, Wolfart M, Brunzel S, Wolfart S. Does the Oral Health Impact Profile questionnaire measure dental appearance? Int J Prosthodont. 2009 Jan-Feb;22(1):87–93. [PubMed] [Google Scholar]
- 14.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 15.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 16.Cushing AM, Sheiman A, Maizels J. Developing socio-dental indicators-the social impact of dental disease. Community Dent Health. 1986;4:3–17. [PubMed] [Google Scholar]
- 17.John MT, Patrick DL, Slade PDL. The German version of the Oral Health Impact Profile - translation and psychometric properties. Eur J Oral Sci. 2002;110:425–433. doi: 10.1034/j.1600-0722.2002.21363.x. [DOI] [PubMed] [Google Scholar]
- 18.John TM, Szentpetery A, Steele GJ. Association between factors related to the time of wearing complete dentures and oral health-relatted quality of life in patients who maintained a recall. Int Jour Prost. 2007;20(1):31–36. [PubMed] [Google Scholar]
- 19.John MT, Reissmann DR, Schierz O, Allen F. No significant retest effects in oral health-related quality of life assessment using the Oral Health Impact Profile. Acta Odontol Scand. 2008 Jun;66(3):135–8. doi: 10.1080/00016350802077835. [DOI] [PubMed] [Google Scholar]
- 20.John MT, Koepsell TD, Hujoel P, Miglioretti DL, LeResche L, Micheelis W. Demographic factors, denture status and oral health-related quality of life. Community Dent Oral Epidemiol. 2004 Apr;32(2):125–32. doi: 10.1111/j.0301-5661.2004.00144.x. [DOI] [PubMed] [Google Scholar]