Abstract
Introduction:
Osteoporosis has a significant role in the etiology of thoracolumbal spinal fractures in older patients. It is the segment where the relatively immobile thoracic segment transfers into a mobile lumbar spine. The clinical picture is always with the back pain after minimal trauma or sometimes even without injury. Diagnosis always includes X-ray and then CAT scan. Treatment depends on the stability of the fracture, neurological findings, and the size of the deformity. Consequences include pain in the legs, back, spinal deformity, reduced lung function, walking disturbances, etc.
Goal:
In this paper we will present the patients who were treated by conservative approach for osteoporotic fractures in thoracolumbal spine.
Material and methods:
They were treated at the Clinic for Orthopedics and Traumatology of Clinical Center university of Sarajevo from December 1st until December 31st 2010. Patients were divided into two groups: group I consisted of patients who were treated with orthoses, and group II patients treated with plaster corset. Both treatments have their use.
Results and discussion:
Plaster corset gives stability; patients with orthoses are more mobile without skin changes. Orthosis is recommended for most disciplined patients and the best is that all the patients have plaster corset for six weeks, followed until the recovery by three points orthoses.
Key words: osteoporotic fracture of the spine, cast immobilization, three points orthoses.
1. INTRODUCTION
Osteoporotic fractures of the spine are nowadays common clinical problem. This phenomenon becomes more significant as the average age of the population is increasing. Osteoporosis is a skeletal change characterized by reduction in bone strength due to loss of bone mass. With the loss of bone mass increases the incidence of fractures. In women, menopausal bone loss is ten times faster. Most of the compression load tolerates vertebral trabeculas (1).
These fractures occur typically in older women without significant trauma. Fractures of the vertebra body are more often in the thoracic than in the lumbar part of the spine. In case of these fractures we should pay attention to the occurrence of early menopause, early resection of the stomach and lack of vitamin D.
Thoracolumbal spine is prone to trauma. This is explained by fact that thoracic relatively immobile part transfers into a movable lumbar which affects the position of small articulations. Small articulations are placed in the second lumbar sagittal plane (2).
The primary task of treating these fractures is the prevention of neurological failure with preservation of stability, however, given that surgical and non surgical results are good, the choice of treatment must be though trough and individually made for each patient.
In the standard X-ray images it is difficult to determine whether it is the case of fresh or older fracture, so the diagnosis must be expanded by CAT scan. Spine X-ray profile provides the best information (2, 3).
Pectoral spine extends from first to twelfth thoracic vertebrae and in conjunction with the first ten ribs forming a solid anatomical structure – the chest. The remaining two ribs and breastbone last two vertebrae together with the first and second lumbar vertebrae, forming a thoracolumbal junction where is possible greater mobility, but by that also greater vulnerability.
Osteoporotic vertebral compression fractures typically involve the middle and lower thoracic spine and thoracolumbal transition. The clinical picture which is seen in the acute situation is in the form of sudden back pain after minimal injury, and often without any injury. For the diagnosis it is essential to take a good medical history and conduct a clinical examination of the patient. The basis of the radiological diagnosis is the standard X-ray. If clinically indicated (the differential diagnosis of tumor or spondylitis, neurological weakness) also used are the CAT and/or MRI. Computerized axial tomography (CAT) is the recognized as the best method to visualize bone compression of the vertebral canal. When CAT analysis of particular importance is in software that is used for analysis, it can present scan of the vertebrae with the different “windows” of density. Specifically, this process better reflects certain tissue density, or it can be separated with a certain range of absorption coefficient in intensity of reconstructed images shown in Hounsfield units (HU). Unlike the native X-ray where the difference in the absorption of less than 5% can not be recorded, the CAT scan differentiates absorption of less than 1%. The sensitivity of CT is also up to 100 times higher than conventional X-ray (1, 3, 4).
Approach to treating osteoporotic fractures of the spine is individual and based on medical history, symptoms, localization and correlation of clinical examination and radiological findings. Fractures often causing longterm pain, loss of height and spinal deformity, which is significantly correlated with gait and mobility disturbances, decreased lung function, loss of appetite and ultimately increased mortality. Open reposition, decompression and fixation is indicated in patients with posttraumatic stenosis and neurological weakness. Modern surgical treatment techniques are vertebroplasty and kyphoplasty, which significantly reduces the pain and improves mobility of patients, and thus the quality of life.
Osteoporotic fractures of the spine are mostly still treated conservatively by: rest, analgesics and application of three points type of Jewett orthoses or similar.
Rest in bed accelerates the development of osteoporosis, and in most patients these therapeutic measures does not reduce pain (4, 5).
Generally accepted is classification according to Denis. Denis is the 1983 proposed a new concept, now widely accepted, in which the spine (thoracic and lumbar) is divided into three pillars or columns: anterior, middle and rear. Knowing this division is of importance in evaluation of injuries, or proclaiming spinal injuries as stable or unstable. About this estimate depend the choice of the patient treatment, and extent of preventive measures – also indication for the type of surgical treatment (2, 5, 6).
The front pillar or column includes the anterior two thirds of the vertebra body, lig. longitudinale anterius, the front part of the anulus and anterior 2/3 of intervertebral disc. The middle pillar or column covers the remaining third of the vertebral body, intervertebral disc and anulus, and the rear longitudinal ligament.
The rear pillar or column contains all the other structures belonging to the vertebra: the lamina, articular extensions (pedincle), the articular surface, transverse and pointed extensions and associated ligaments.
For the preservation of the integrity of the anterior and middle columns are the most responsible anterior and posterior longitudinal ligaments, and the preservation of the integrity of the rear column back nuchal ligament complex, flava ligaments, joint capsule and their supporting ligaments. We need to know: if only one column is damaged, and the remaining two have preserved the integrity the injury of the spine can be considered stable and there is no danger, in most cases, for the additional injury to the medulla. If two (or all three) columns are injured, spine injury should be considered and treated as unstable. The two split and separate column in the injured segment move independently and there is great risk of injury (or additional injury) to medulla spinalis and nerve roots (4, 5).
There are still disagreements over the determination of the threshold level of reduction which allows the unambiguous distinction between vertebral fracture, deformity, and normal forms. This has led to different morphometric algorithms for defining vertebral fractures. Melton et al. 1989 have developed adaptive algorithm that is based on an analysis of relations between the vertebral height adjustable corrected factors. Vertebral body is fractured when one of three height relations exist – front to back height (Hm/Hp) biconcave fractures and back towards the rear of the height of adjacent vertebrae (RHP compression fracture) – has been reduced for more than 15% compared with the normal ratio for that level. Depending on the deviation amount of the fracture can be mild, medium and severe, and are marked with degree from 1 to 3 (1, 3, 7).
Previously, the fractures were treated with the use of a longer rest with use of plaster corset or orthosis.
Three points orthoses are indicated in stable compressive fracture of the lower thoracic and lumbar vertebrae. The effect of spinal hyperextension ensures stability in the sagittal plane. The stability of the rotation is limited to extensional plate below the collarbone, stable frame design limits lateral flexion. Features: a conveyor belt at the hips for a comfortable seat is manufactured in 4 sizes. Size bar is adjustable (2, 8).
Plaster corset: It is used for the immobilization of the thoracolumbal spine.
Base points of this cast are manubrium sternum, symphysis and spinal extensions spine. These three points provide maintenance of spine reclination. Indications are fractures of thoracic-lumbal spine without neurological complications (8, 9).
2. GOAL
Indicate the effects of the use three points orthotics and plaster immobilization in conservative treatment of fractures thoracolumbal spine.
We have monitored the following parameters: patient gender, age, type of fracture, the duration of immobilization, presence of pain, skin changes, and other complications.
3. MATERIAL AND METHODS
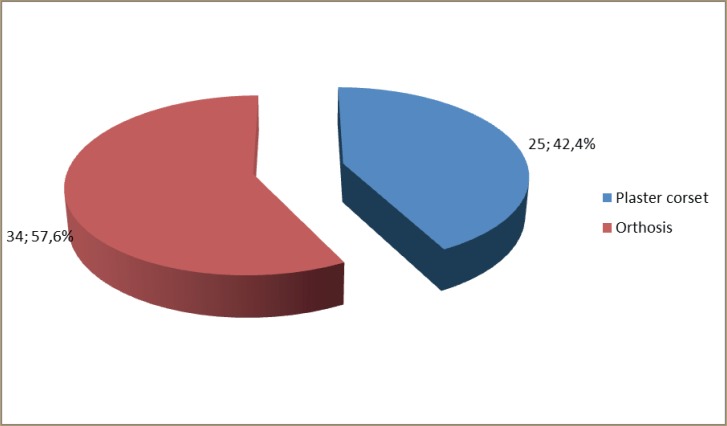
At the Clinic of Orthopedics and Traumatology of Clinical Center of Sarajevo we take into consideration 59 patients who were treated for osteoporotic fractures in the thoracolumbal segment of the spine during the 2010 year.
Patients were divided into two groups:
The group of 34 patients who were treated for osteoporotic thoracolumbal fracture of the spine by orthosis.
Second group of 25 patients who were treated for osteoporotic thoracolumbal fracture of the spine by plaster corset.
All patients had confirmed diagnosis by X-ray and CAT scan.
The fractures were classified according to Denis and all belonged to the group of stable fractures.
4. RESULTS
Results are presented graphically and in tabular form.
More commonly orthoses were used.
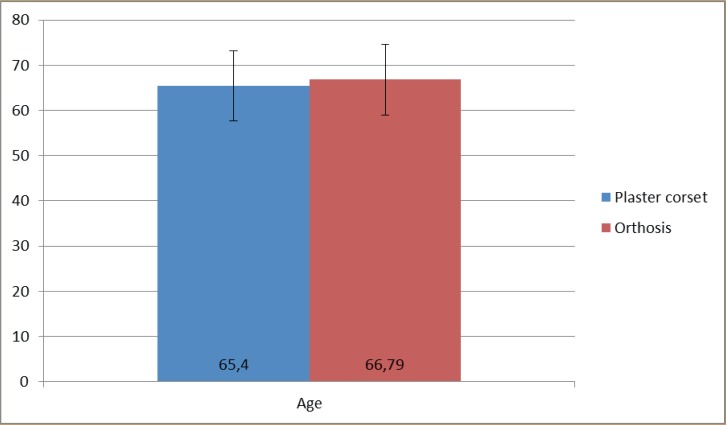
The average age was 66 years and according to the results patients in both groups was of similar age. 67% of the patients had orthoses for about 3 months.
The pain was present both in those with orthoses and plaster corset. After removal of immobilization in both groups there was occasional pain.
In four female patients we removed plaster after four weeks because of pressure sores on the skin.
Among the fractures most common were compressive fracture of Th12, L1 vertebrae in the first group, and L1, L2 fractures in the second group.
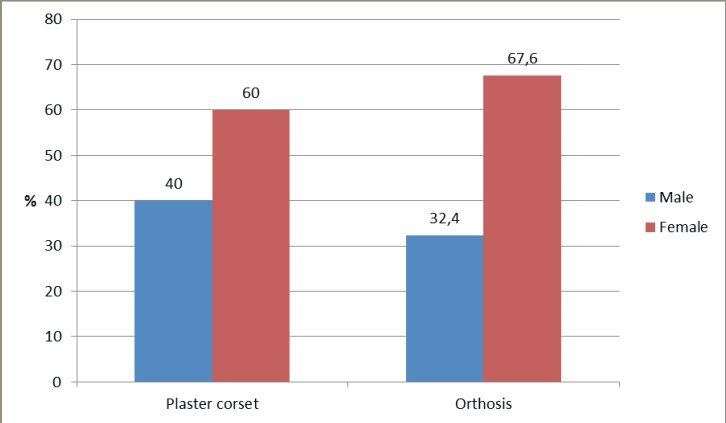
From the results it is evident that there were more female patients in both groups, so the groups do not differ by sex, age and localization of fractures, but differ according to the duration of recovery in terms of shorter duration in a cohort of plaster corset.
Wedge deformity for more than half of the front of the fractured vertebrae body had 9 patients with orthoses and 4 patients with a plaster corset.
5. DISCUSSION
Treatment of thoracolumbal spine osteoporotic fractures remains controversy despite technological progress, increased knowledge and advances in surgical techniques.
Osteoporotic fractures of the spine are more common in women (16%) than men (5%) and occur with minor trauma (7). These fractures are still treated conservatively by rest, analgesics and application of orthoses or plaster corset. Bed rest accelerates bone mass loss, while wearing immobilization for a long time leads to muscle hypotrophy (2, 5, 11).
Before the age of 40 years substantia spongiosa of the vertebra carries more than 50% of the load, and after this period of life substantia corticalis carries more than 50% of the load, as reported in their research by Kirkaldy-Willis 1990.
The latest data from the USA show that at least 700,000 patients a year have osteoporotic fracture of the spine which represents one of the leading health problems. Osteoporotic fractures of the spine are two to three times more frequent than hip fractures, particularly in women (7).
Assessment of morbidity and mortality of osteoporotic fractures of the spine is difficult because of the large number of undiagnosed fractures. Doctors contact only one third of the total number of patients with osteoporotic fractures of the spine (6), so probably only one third of all fractures of the spine is diagnosed (10, 11). The incidence of clinically diagnosed osteoporotic spine fractures was 117 per 100,000 people per year or 438,000 clinically diagnosed osteoporotic spine fractures per year in the European Union.
Among women aged over 60 years, 25% to 30% of them have at one point in life osteoporotic fracture of the spine and the resulting deformation (12). Fractures of the spine are two to three times more frequent than hip fractures, particularly in women. The latest data in the United States show that at least 700,000 patients a year have osteoporotic spine fracture, which is one of the leading health problems of the elderly population (13, 14). The cause for fact that a small fraction of osteoporotic fractures of the spine is diagnosed is because they are often asymptomatic or develop with fewer symptoms (15). In women, 90% of osteoporotic fracture occurs with minimal injury, and in men in approximately 60% of fractures of the spine (7, 14).
Three points orthoses are used more often because they are more comfortable for the patient because of the increased mobility. Orthoses have lower weight and are aesthetically more acceptable to the patient.
Most frequently injured spine segments of examined patients in both were segments (Th-L) of thoracolumbal transition area, or Thll-L2, which is, logically, given that this part is most mobile in thoracolumbal spine and as such is prone to injury. These results correspond to data of other authors and representation of injuries of this region by 50% to 70%. Cantor and colleagues reported on the satisfactory results of conservative treatment in patients without neurological deficits (12, 13).
Multi-level fractures are usually localized at levels Th5-6 and II-2. According to recent studies, compression fractures are more frequently represented at the level of thoracolumbal transition – about 85% of cases (14, 15).
Less pain according to Load Sharing Scale has patients who were treated by three points orthoses. Three points orthosis is suitable for patients with cardiopulmonary disease and the elderly population.
Plaster immobilization has the advantage of maintaining the stability of the fracture, repositioning and reducing the possibility of kyphosis occurrence (16).
Rest in bed accelerates the development of osteoporosis in most patients, these therapeutic measures do not reduce pain (17). In regard the difficulty of wearing orthotics, and poor results of conservative treatment, the development of surgical techniques and technology have created new opportunities for treatment of compressive fractures of the spine. Clinical signs may worsen later, accompanied by radiographically visible reduction in height of the corpus vertebrae, posttraumatic stenosis and associated deformity of the spine. Opposite of surgically treated patients in the group of conventionally treated there is increasing average angle of kyphosis over time. In the referral articles authors point to increase in the average value of kyphosis in conservatively treated thoracolumbal fractures (18, 19).
6. CONCLUSIONS
Immobilization by plaster corset or orthosis is the manner of conservative treatment for osteoporotic thoracolumbal spine fractures.
Immobilization by plaster corset is more stable because it has fewer complications in terms of spinal deformity after osteoporotic fracture.
Immobilization by three points orthosis is comfortable for patients, more mobile and causes less pain.
For the successful treatment of osteoporotic fractures of the thoracolumbal spine it is best to place at first the plaster corset for six weeks, followed by orthoses until complete rehabilitation.
Figure 1.
Distribution of patients according to the type of immobilization
Figure 2.
Distribution of patients by gender and type of immobilization
Figure 3.
Distribution of patients by age and type of immobilization
Figure 4.
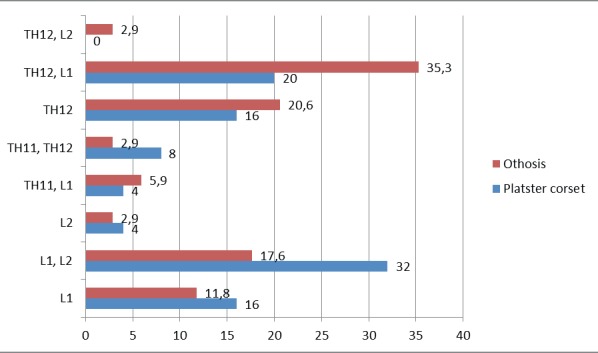
Distribution of patients according to the localization of the fracture and the type of immobilization
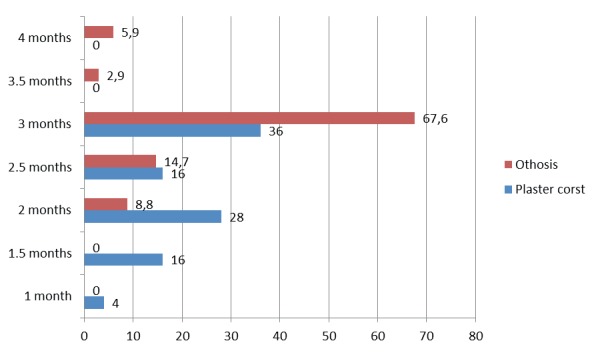
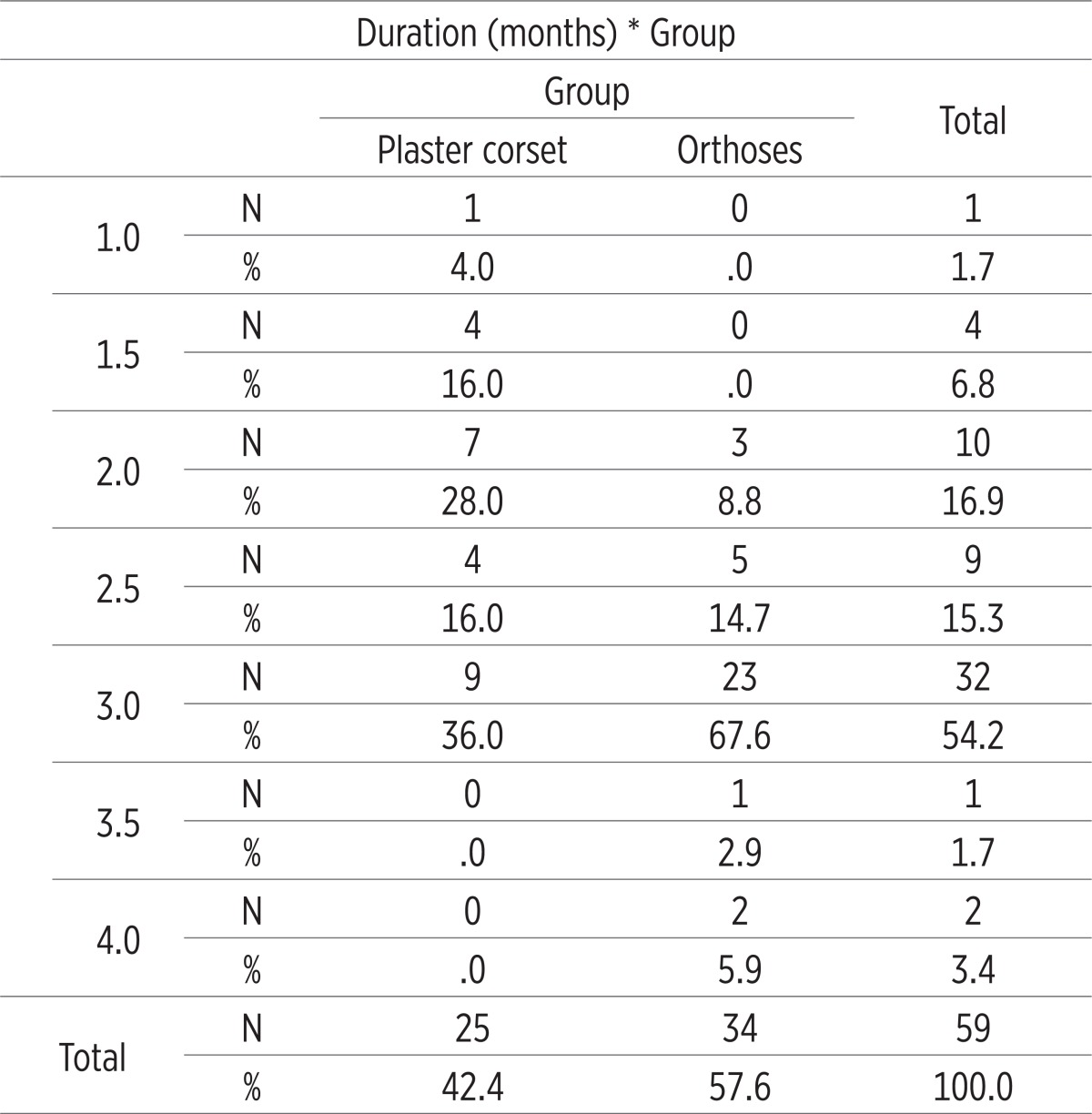
Figure 5.
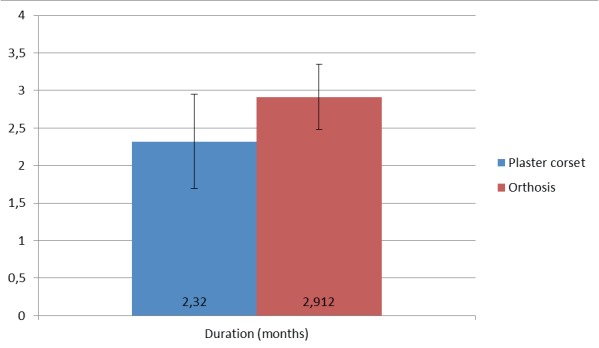
Distribution of patients by duration and type of immobilization
Figure 6.
Immobilization duration
Table 1.
Gender structure χ2 = 0.367 p = 0.369
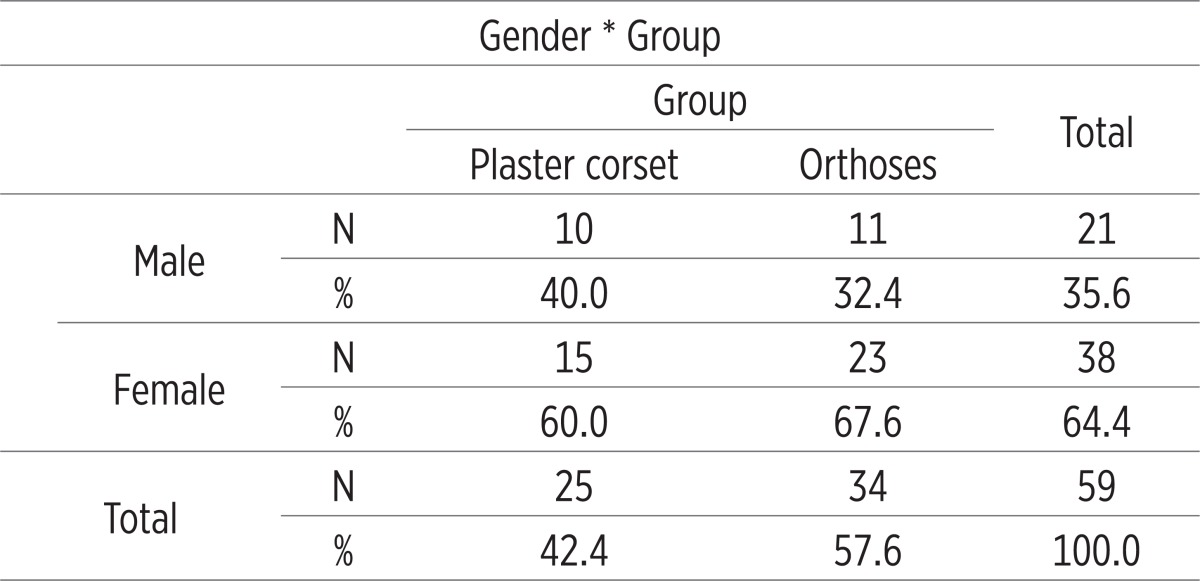 |
Table 2.
Patients age T = 0.457 p = 0.502
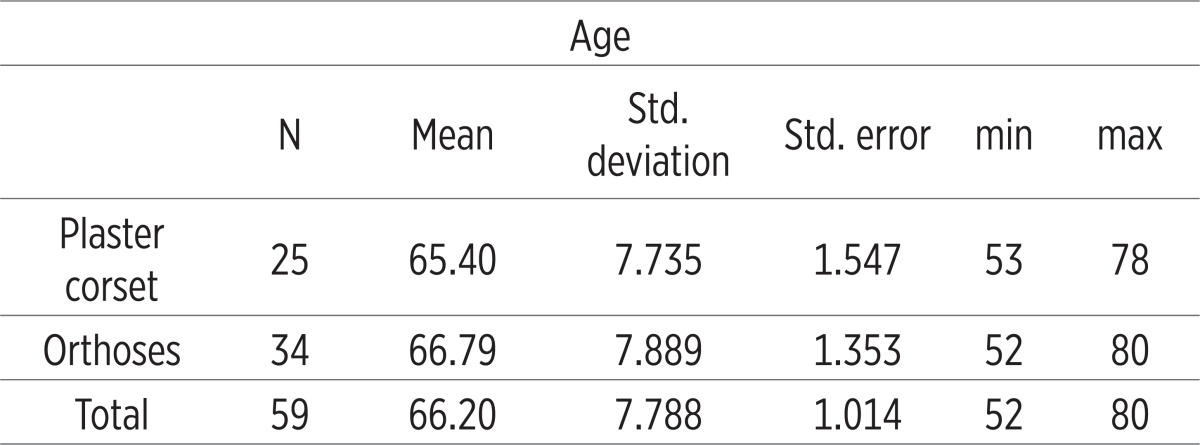 |
Table 3.
Distribution of the localization of fractures X2 = 4.382 p = 0.735
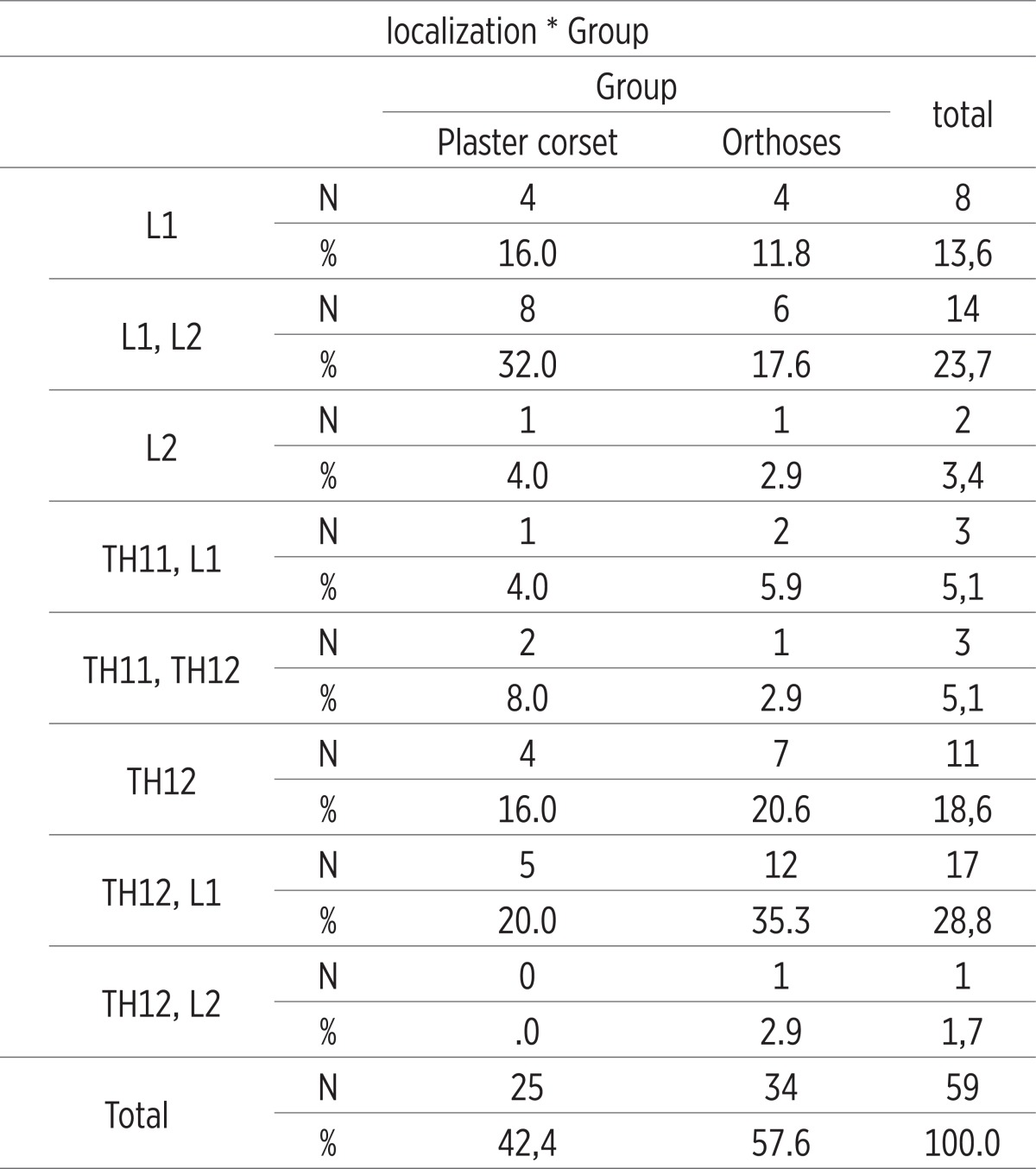 |
Table 4.
Duration of immobilization t=5.045 p=0.001
 |
Table 5.
Immobilization duration X 2 = 14.808 p = 0.022
 |
Conflict of interest
none declared.
REFERENCES
- 1.Kučukalić–Selimović E. i sar., Osteoporoza dijagnostika, prevencija, liječenje. Institut za naučnoistraživački rad i razvoj KCUS. 2008.
- 2.Komadina R. in sod. Zlami zaradi osteoporoze. Drutvo traumatologa Slovenije, Celje. 1999.
- 3.Hadžiahmetovic Z, Hadžiahmetovic–Vavra N. Sarajevo: Avicena; 2005. Traumatologija. [Google Scholar]
- 4.Biščević M. Moderne tehnike liječenja osteoporotskih prijeloma kičme - vertebroplastika i kifoplastika. Univerziteti Tuzla i Sarajevo. 2011.
- 5.Buljat G, Perović D. Treatment of osteoporotic fractures of the spine. Arh Hig Rada Toksikol. 2007;58:49–54. doi: 10.2478/v10004-007-0008-4. [DOI] [PubMed] [Google Scholar]
- 6.Denis F. Spinal instability as defined by the three-column concept in acute spinal trauma. Clin Orthop. 1984;189:65–9. [PubMed] [Google Scholar]
- 7.Melton LJ, Kan SH, Frye MA, Wahner HW, O’Fallon WM, Riggs BL. Epidemiology of vertebral fractures in women. Am J Epidemiol. 1989 May;129(5):1000–1011. doi: 10.1093/oxfordjournals.aje.a115204. [DOI] [PubMed] [Google Scholar]
- 8.Lonstein JE. History of spinal bracing. Orthotics 703, course for physicians and surgeons, Northwestern University Medical School, Prosthetic-Orthotic Center, 1989-1992.
- 9.Hančević J, Antoljak T, Korač Ž. Zagreb: Medicinska naklada; 2001. Imobilizacija. [Google Scholar]
- 10.Axelsson P, Johnsson R, Stromqvist B. Effect of lumbar orthosis on intervertebral mobility. A roentgen stereophotogrammetric analysis. Spine. 1992;17:678–681. doi: 10.1097/00007632-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Anderson PA. Nonsurgical treatment of patients with thoracolumbar fractures. Instr Course Lect. 1995;44:57–65. [PubMed] [Google Scholar]
- 12.Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine. 1993;18:971–976. doi: 10.1097/00007632-199306150-00004. [DOI] [PubMed] [Google Scholar]
- 13.Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH. Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing andearly mobilization. Spine. 1996;21:2170–2175. doi: 10.1097/00007632-199609150-00022. [DOI] [PubMed] [Google Scholar]
- 14.Golubović Z, Stojiljković P, Bošnjaković P, Radovanović Z, Višnjić A, Ristić S, Golubović I, Najman S. Prelomi pršljenova kičmenog stuba kod bolesnika sa osteoporozom
- 15.Acta facultatis medicae Naissensis. 2008;25(2):69–74. [Google Scholar]
- 16.Grew ND, Deane G. The physical effect of lumbar spinal supports. Prosthet Orthot Int. 1982;6:79–87. doi: 10.3109/03093648209166772. [DOI] [PubMed] [Google Scholar]
- 17.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl1):S17–S24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Willen J, Lindahl S, Nordwall A. Unstable thoracolumbarfractures. A comparative clinical study of conservative treatment and Harrington instrumentation. Spine. 1985;10:111–22. doi: 10.1097/00007632-198503000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Tonbul M, Yilmaz MR, Ozbaydar MU, Adaş M, Altan E. Long-term results of conservative treatment for thoracolumbar compression fractures. Acta Orthop Traumatol Turc. 2008 Mar-Apr;42(2):80–3. doi: 10.3944/aott.2008.42.2.080. [DOI] [PubMed] [Google Scholar]