Abstract
Objective
To examine the efficacy of a 12-week manualized Meta-Cognitive Therapy (MCT) group designed to enhance time-management, organization, and planning in adults with AD/HD.
Method
Eighty-eight clinically referred adults who met DSM-IV criteria for ADHD based on clinical and structured diagnostic interviews and standardized questionnaires were stratified vis-à-vis ADHD medication use and otherwise randomly assigned to receive MCT or supportive psychotherapy in a group modality. MCT employs cognitive-behavioral principles and methods to impart skills and strategies in time-management, organization, and planning, and target depressogenic and anxiogenic cognitions that undermine effective self-management. The Support group controlled for non-specific aspects of treatment by providing support while avoiding discussion of cognitive-behavioral strategies. MCT and Support groups were comparable in gender (29% and 39% male, respectively) and age (41±11.59 yr and 42 ± 12.09 years, respectively). Therapeutic response was assessed by an independent (blind) evaluator via structured interview pre- and post-treatment, as well as by self-report and collateral informant behavioral ratings.
Results
General linear models, comparing change from baseline between treatments, revealed statistically significant effects for independent evaluator, self-report, and collateral ratings of DSM-IV inattentive symptoms. Employing dichotomous indices of therapeutic response, a significantly greater proportion of MCT vs. Support group members demonstrated improvement. Logistic regression examining group differences in operationally defined response (controlling for baseline ADHD severity) revealed a robust effect of Treatment Group (odds ratio=5.41; 95%CI=1.77,16.55).
Conclusion
MCT (vs. Support) yielded significantly greater improvements in dimensional and categorical estimates of ADHD severity, supporting its efficacy as a viable psychosocial intervention.
Once thought to be exclusively a childhood disorder, it is now recognized that ADHD frequently persists into adulthood, afflicting approximately 4% of the adult population (1) and generating significant impairment in academic, occupational, social and emotional functioning (2, 3). This impairment includes completion of fewer years of education and elevated rates of unemployment, antisocial behavior, interpersonal conflict, marital separation, and divorce. In addition, adults with ADHD are at significantly greater risk for substance and alcohol abuse disorders (4) as well as other comorbid disorders such as anxiety and depression (1).
Paralleling results with children, stimulant (5) and non-stimulant (6) drugs have been shown to be effective in adults in reducing the core symptoms of ADHD. However, there are limitations associated with drug treatment. First, little is known concerning the impact of pharmacotherapy on functional impairment typically associated with ADHD (7) - particularly in time-management and organization. Given the likely under-development of meta-cognitive skills in these areas in youth with ADHD (8), drug treatment alone may not be sufficient to remediate these deficits, and explicit skills training in adulthood may be necessary. Secondly, 20–50% of adults are non-responders or adverse responders to drug treatment (9), which highlights the need for additional interventions. Further, since “responder” typically refers to an individual who demonstrates at least a 30% reduction in symptoms, many considered “responders” do not achieve full remission, leaving room for improvement through other modalities. Thus, there is clearly a need for psychosocial interventions to help adults with ADHD develop essential self-management skills.
A recent review revealed limited research concerning psychosocial treatments for adults with ADHD (10). A case series (11), and several open studies of group (12, 13) and individual (14) cognitive-behavioral treatments yielded promising results. However, controlled studies are limited to trials of group-administered (15) and individually-administered (16) cognitive-behavioral interventions, each compared to a wait-list control condition. Both found significantly greater improvement in core ADHD symptoms in the treated group. Yet, while these studies yielded large effect sizes in the treated group and controlled for the passage of time, they enrolled small samples (n = 15–22 per condition) and did not control for non-specific effects of treatment (e.g., therapist support), which may exert powerful effects on treatment response (17, 18).
Over the past decade our group has been developing, studying, and refining a group-administered intervention, termed “Meta-Cognitive Therapy” (MCT), which incorporates cognitive-behavioral principles and was designed to foster development of executive self-management skills. We chose to focus on time-management and organization because difficulties in the attentional domain are more prevalent than those in the hyperactive-impulsive domain among adults with ADHD and most consistently related to clinician ratings of both severity of illness and impairment (19). Our clinical experience also indicates that problems with impulsivity, social behavior, and mood control are only common to a subset of patients and require a different intervention format. The group format was selected because: (i) the skills and strategies to be imparted lend themselves to semi-structured presentation; (ii) the group format provides opportunities for positive modeling, social reinforcement and social support; and (iii) the group is a cost-effective treatment delivery mode.
Our first study of MCT (20) found that adults who completed our manualized group MCT program showed robust change from pre- to post-treatment on standardized self-report measures of ADHD symptoms and executive skills. Given these positive results, we undertook the present study to rigorously examine the efficacy of MCT by comparing self-report, observer report, and ratings by an independent evaluator for those who received MCT compared to those of patients randomly assigned to a supportive therapy control group. We postulated greater positive change in the MCT group than in the Support group. We further hypothesized that patients concurrently receiving medications to treat ADHD would show an enhanced positive response to MCT because the medication would allow them to focus better, process and retain more during the therapy sessions, and facilitate the practice of strategies between sessions. Finally, we hypothesized that by improving functioning, MCT would enhance feelings of efficacy and competence, thereby yielding secondary improvements in co-morbid symptoms of anxiety and depression.
Method
The study received the approval of the Institutional Review Board at the Mount Sinai School of Medicine and all participants provided informed written consent to participate.
Design
Eighty-eight adults rigorously diagnosed with ADHD were stratified with respect to use of ADHD medications (stimulants or atomoxetine) and otherwise randomly assigned to receive either MCT or a Support group; the latter was intended to control for non-specific therapeutic effects of a group intervention. Response was assessed via a structured interview completed by an independent (blind) evaluator, and by questionnaires completed by the patient and a significant other, immediately pre- and post-treatment. Each group consisted of 6–8 participants. One MCT and one Support group intervention were run concurrently in a “cohort” to ensure that the groups were matched on the percentage receiving ADHD medications and were equivalent with respect environmental changes (e.g., seasonal and holiday periods).
Participants
Prospective participants were referred from New York area medical and psychiatric clinics, ADHD advocacy/self-help groups, community psychiatrists and internists, university health services, and postings on clinical trials websites.
Participants were required to be between the ages of 18 and 65 with a DSM-IV diagnosis of ADHD (Predominantly Inattentive or Combined subtype). Exclusion criteria included: active substance abuse or dependence; suicidality; overtly hostile or aggressive behavior likely to alienate group members; “asocial” (e.g., PDD) characteristics; cognitive disability (estimated IQ < 80); psychosis; borderline personality disorder; Alzheimer’s or other dementia; overt neurological disorder; and/or childhood history of abuse or trauma or other severe psychiatric condition that confounded ascertainment of childhood ADHD symptoms. Patients with other Axis I psychiatric disturbances were eligible for participation. Individuals receiving psychotropic medication had to be stabilized on a given drug for at least two months, and on a given dose for at least one month, in order to be eligible for group assignment. Patients were instructed to defer non-essential changes in their therapeutic regimen (either medication or psychotherapy) until the end of treatment.
Assessments
Diagnostic Assessments
The diagnosis of ADHD was based on the Conners Adult ADHD Diagnostic Interview for DSM-IV (CAADID) (21). Also required was a T-score of at least 65 (93rd percentile) on the DSM-IV Inattentive subscale and a T-score of 63 (90th percentile) on the Inattention/Memory subscale of the Conners Adult ADD Rating Scale–Self-Report: Long Version (Conners-Self-Inattention) (22, 23). The latter subscale largely consists of items that gauge the severity of the difficulties in time-management and organizational functions that constitute the focus of MCT. The presence of childhood symptoms was confirmed by at least one of the following: self-report of ≥ 4 childhood symptoms in one domain (inattentive or hyperactive-impulsive) on the CAADID; report of ≥ 4 symptoms in a given domain on the Childhood Symptom Scale–Other Report (24) by the parent or other adult who knew the patient in childhood; or report of symptoms of ADHD on school report cards or a childhood psychological evaluation. Comorbid conditions were assessed using the Structured Diagnostic Interview for DSM-IV Axis-I disorders (SCID-I) (25) and the SCID-II (26) module for Borderline Personality Disorder. IQ was estimated using four subtests from the WAIS-III (Vocabulary, Similarities, Block Design, and Matrix Reasoning), as described by Tellegen (27).
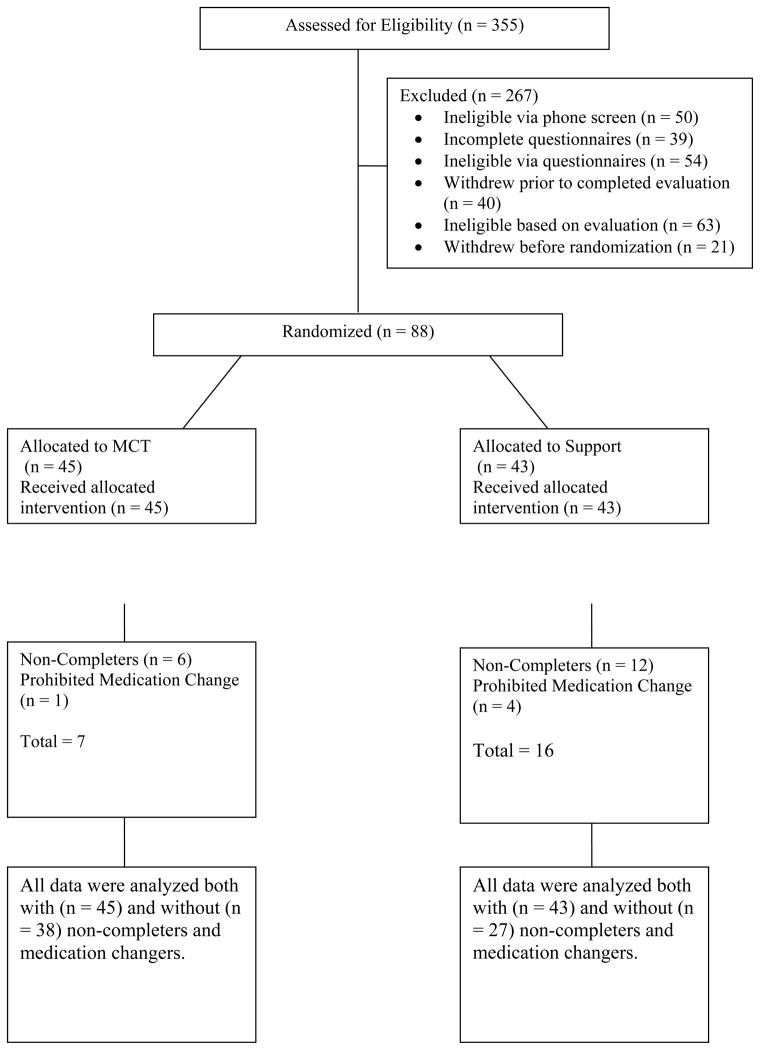
Candidates meeting criteria at each stage of screening are shown in Figure 1.
Figure 1.
Flow chart of participant progress through the phases of the trial.
Assessments of Response to Treatment
Patients were assessed by the independent evaluator pre-and post-treatment using the Adult ADHD Investigator Symptom Rating Scale (AISRS), a structured interview developed to assess the 18 DSM-IV symptoms of ADHD (28). Clinicians were licensed psychologists or Board-eligible psychiatrists who had been trained on the AISRS to a reliability criterion of .90. To reduce rater variance, the same evaluator administered the interview to a given participant pre- and post-treatment. The symptom score (0–3) summed across the nine Inattention items (AISRS-IN) served as one of two primary outcome scores for the study. The independent evaluator also administered the Structured Interview Guide for the Hamilton Anxiety Rating Scale (Hamilton Anxiety) (29). The Conners-Self-Inattention questionnaire served as the other primary outcome measure. In addition, the: following self-report questionnaires were completed pre- and post-treatment; Brown ADD Scales (30); Behavior Rating Inventory of Executive Function–Adult Version (BRIEF-A) (31); Beck Depression Inventory-II (32); Rosenberg Self-Esteem Inventory (33); and the On Time Management Organization and Planning (ON-TOP), which was developed and previously used in our program to assess those skills (20). The Conners-Observer Report: Long Version (Conners-Observer) was also completed pre- and post-treatment by a spouse, partner, family member or close friend of the participant, with the participant’s consent.
Meta-Cognitive Therapy
Principles of Meta-Cognitive Therapy
In MCT cognitive-behavioral principles are employed to: (i) provide contingent self-reward (e.g., for completing an aversive task); (ii) dismantle complex tasks into manageable parts; and (iii) sustain motivation toward distant goals by visualizing long-term rewards. Traditional cognitive-behavioral methods that challenge anxiolytic and depressogenic cognitions are also incorporated. Support from, modeling of, and reinforcement by other group members and the therapist are important components of the treatment that serve to stimulate, enhance and maintain positive gains.
Cues to promote generalization and maintenance
The program also makes use of self-instruction using phrases that link a problematic situation (cue) with a cognitive response that provides a solution to that problem. Examples include, “If I am having trouble getting started (cue), then the first step is too big (solution is to break task down into parts).” Another example, designed to cue individuals to minimize distracters in their organizational space is, “Out of sight, out of mind.” Such phrases are repeated strategically throughout the program so that they become part of the individual’s problem-solving repertoire, thereby enhancing generalization and maintenance of gains.
Content of MCT
The sequence of treatment sessions, displayed in Table 1, is hierarchical in nature, beginning with training in specific skills (e.g., mechanics of planner use) and progressing to higher-order skills that encompass both time-management and organization (i.e., planning).
Table 1.
MCT Program Sequence
Session 1. Participants are oriented to:
|
Sessions 2–6. Each session addresses one or more time- and task-management topics, including:
|
Sessions 7–9.
|
Sessions 10–11.
|
Session 12.
|
Session Format
The first hour of each 2-hour session is devoted to a round-table review of each participant’s experience with the home exercise to: ascertain and address cognitive, situational, and emotional obstacles to implementation; suggest additional or alternative strategies; and address counter-productive emotional responses. The second half of each session begins with a presentation of the new topic and corresponding strategies, followed by an in-session exercise to illustrate/model each technique. Sessions conclude with an explanation of the next home exercise and anticipatory trouble-shooting,.
Supportive Therapy
The Support condition was designed to control for non-specific elements of the MCT program, including session and treatment duration (two hours per week for twelve weeks), group support/validation, therapist attention, and psychoeducation, yet lacked didactic strategies and exercises contained within the MCT program. A Manual delineated the techniques and strategies that were prohibited and permitted to the therapist during Support sessions.
Program Structure
Each Support treatment series commenced with a brief discussion regarding the program orientation and the role of the therapist as an educator and facilitator. The group was characterized as a mechanism for providing information (e.g., addressing and dispelling myths), uniting around shared experiences, and fostering a network of support.
During the initial session, group members were asked to identify a specific goal to address during the program. Each subsequent session was subdivided into two segments, with the initial half devoted to a review of events that transpired during the preceding week, including challenges and/or positive accomplishments; the second portion, when time permitted, involved a therapist-led discussion of a specific psychoeducational theme, elicited from group members at the outset of the session. Although the specific topics varied somewhat across groups, the most typical areas covered included: primary symptoms of ADHD; everyday manifestations of ADHD symptoms; and psychopharmacological treatment. Throughout the various sessions, each therapist responded by: providing psychoeducation; offering support and encouragement (e.g., highlighting positive changes and effort); and/or referring the problem to the group for alternative solutions.
Therapists and Training
Two psychologists who were already highly experienced in the diagnosis and treatment of ADHD in adults (DM, JW) were thoroughly trained in MCT and Support interventions and served as therapists. Each therapist led half of the MCT groups and half of the Support groups in randomized sequence.
Fidelity Ratings
Therapist competence and adherence to the treatment protocols were rated on a checklist (available upon request) developed following recommendations of Waltz et al. (34). All treatment sessions were taped and four sessions from each 12-session series were randomly selected for rating by a therapist experienced in cognitive-behavioral therapy (48 tapes in all). Comparison of ratings yielded no differences between groups in mean rated therapist competence and also indicated that there were no instances of contamination of the Support condition by use of behavioral or cognitive-behavioral interventions.
Data Analyses
The treatment groups were compared on baseline characteristics using t-tests for continuous variables and chi-square tests for categorical variables. Because the treatments were conducted in groups, we investigated the intra-cluster correlation due to group, as well as cohort, and group leader in the outcome change (pre minus post) measures, controlling for the pre-treatment measure. These were done using mixed models that specified group, cohort, and group leader as random effects. General linear Modeling was used to compare the degree of change in the two treatment groups, controlling for the pre-treatment measure. Models that included the interaction of treatment with the pre-treatment measure were also run to assess whether any effects of treatment differed by the severity prior to treatment. Additional models also incorporated interactions of treatment with potential moderators of treatment response, including demographic characteristics, comorbid diagnoses, and medication status.
Results
Sample Characteristics
Eighty-eight participants meeting full eligibility criteria were randomized to treatments (45 to MCT and 43 to Support). MCT and Support conditions did not differ on any socio-demographic or clinical variable with the exception of marital status (Table 2). Although this was a largely well-educated sample, only half were employed full time, and household income in both groups evenly spanned 10 intervals between <$9,999 and ≥$150,000.
Table 2.
Demographic and Clinical Characteristics
| MCT n = 45 | Support n = 43 | Statistic | p (2-tailed) | |||
|---|---|---|---|---|---|---|
| Gender | n | % | n | % | ||
| Males | 13 | 29 | 17 | 39 | χ = 1.11 | .292 |
| Females | 32 | 71 | 26 | 61 | ||
|
| ||||||
| M | (SD) | M | (SD) | |||
|
| ||||||
| Age (years) | 41.04 | (11.59) | 42.37 | (12.09) | t = −.526 | .600 |
| Years of Education | 16.40 | (1.74) | 15.98 | (2.23) | t = .996 | .322 |
|
| ||||||
| n | % | n | % | |||
|
| ||||||
| Highest Degree Achieved | χ = 10.70 | .152 | ||||
| High School/GED | 3 | 7 | 6 | 14 | ||
| Technical/Associates | 4 | 9 | 8 | 19 | ||
| Bachelors | 23 | 51 | 12 | 28 | ||
| Graduate | 15 | 33 | 17 | 39 | ||
| Ethnicity1 | χ = 4.31 | .506 | ||||
| Asian | 1 | 2 | 2 | 5 | ||
| Black | 2 | 4 | 1 | 2 | ||
| Caucasian | 40 | 89 | 34 | 79 | ||
| Hispanic | 2 | 4 | 3 | 7 | ||
| Mixed Race | 0 | 0 | 3 | 8 | ||
| Marital Status | χ = 10.75 | .013 | ||||
| Married | 20 | 44 | 10 | 23 | ||
| Divorced | 2 | 4 | 6 | 14 | ||
| Never Married | 17 | 38 | 26 | 61 | ||
| Cohabiting | 6 | 13 | 1 | 2 | ||
| Employed (Any) | 33 | 73 | 31 | 72 | χ = .017 | .896 |
| Employed Full Time | 22 | 49 | 23 | 54 | χ = .186 | .666 |
| Household Income | χ = 12.35 | .194 | ||||
| $0–$9,999 | 3 | 7 | 6 | 14 | ||
| $10,000–$19,999 | 3 | 7 | 4 | 10 | ||
| $20,000–$29,999 | 4 | 9 | 4 | 10 | ||
| $30,000–$39,999 | 7 | 16 | 3 | 7 | ||
| $40,000–$49,999 | 2 | 4 | 7 | 17 | ||
| $50,000–$59,999 | 2 | 4 | 6 | 14 | ||
| $60,000–$74,999 | 7 | 16 | 3 | 7 | ||
| $75,000–$99,999 | 4 | 9 | 3 | 7 | ||
| $100,000–$149,999 | 6 | 13 | 4 | 10 | ||
| $150,000 or more | 7 | 16 | 2 | 5 | ||
|
| ||||||
| M | (SD) | M | (SD) | |||
|
| ||||||
| WAIS-III Abbreviated IQ | 119.23 | (11.47) | 114.07 | (14.10) | t = 1.89 | .062 |
| CAARS-Self Scales | ||||||
| Inattention/Memory | 79.62 | (7.25) | 79.67 | (6.56) | t = −.035 | .972 |
| DSM-IV Inattentive | 82.82 | (11.77) | 84.93 | (6.30) | t = −1.04 | .301 |
| DSM-IV Hyperactive-Impulsive | 64.87 | (13.43) | 65.88 | (14.11) | t = −1.02 | .730 |
|
| ||||||
| n | % | n | % | |||
|
| ||||||
| ADHD Subtype2 | χ = .142 | .707 | ||||
| Combined | 14 | 31 | 15 | 35 | ||
| Inattentive | 31 | 69 | 28 | 65 | ||
| Any Current Anxiety Disorder | 25 | 56 | 23 | 54 | χ = .038 | .846 |
| Any Current Mood Disorder | 13 | 29 | 15 | 35 | χ = .364 | .546 |
|
| ||||||
| M | (SD) | M | (SD) | |||
|
| ||||||
| Beck Depression Inventory-II | 10.89 | (9.44) | 11.60 | (8.56) | t = −.372 | .711 |
| Rosenberg Self-Esteem Inventory | 17.20 | (5.07) | 18.55 | (5.42) | t = −1.20 | .234 |
Note. CAARS=Conners Adult ADHD Rating Scales – Self-Report.
Ascertained on the basis of self-report.
Ascertained on the basis of CAADID structured interview for ADHD
Attrition
Five participants in each Group dropped out of treatment, thereby missing more than three sessions. “Non-completers” additionally included one MCT participant and seven Support participants, who missed more than three sessions during the program. “Missing” was defined as missing at least half of a session. An additional five participants (1 MCT, 4 Support) made proscribed medication changes during the 12-week program. Post-treatment outcome data were obtained from all randomized participants except 7 drop-outs (4 MCT, 3 Support).
Non-completers plus medication changers constituted 16% of the MCT and 37% of the Support Group (χ2 = 5.34, df=1, p=.02). Completers (n=65) were more likely than non-completers (including medication changers) to be female (72% vs. 48%, respectively, χ2 = 4.53, df=1, p =.03) and to be of the Predominantly Inattentive subtype (74% vs. 48%, χ2 = 5.21, df=1, p =.02). Completers and non-completers did not differ with respect to any other demographic or clinical characteristics.
Analyses of ADHD-Related Measures
The primary outcome measures were the blind structured interview (AISRS) and the Conners-Self-Inattention scale. We examined effects on the full AISRS, as well as on a subscale of the AISRS-IN consisting of five items that most directly reflect the skills of time-management, organization and planning (TMOP) that are targeted by MCT: failure to complete tasks, disorganization; avoidance of effortful tasks, losing things, and forgetting things (AISRS-TMOP). Due to lower rates of return of the Conners Observer scales (in part, attributable to limited availability of a collateral), effects on the Conners-Self and Observer reports were examined in separate univariate analyses.
The results of General Linear Modeling comparing change from baseline between treatment groups, adjusting for the baseline value of the change outcome measure are shown in Table 3, along with the unadjusted pre- and post- means and change scores adjusted for baseline by treatment group.
Table 3.
Response on Dimensional Measures
| Measure | MCT Group (n = 41) | Support Group (n = 40) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Pre | Post | Pre | Post | Difference between Least Square Mean Change scores (95%CI) |
||||||||||
|
| ||||||||||||||
| Mean | (SD) | Mean | (SD) | Least Squares Mean Change1 |
(95% CI) | Mean | (SD) | Mean | (SD) | Least Squares Mean Change1 |
(95% CI) | |||
| AISRS-IN | 18.88 | (3.75) | 13.71 | (4.27) | 5.0 | (3.7,6.3)* | 18.33 | (3.55) | 16.18 | (4.71) | 2.3 | (1.0, 3.6)* | 2.7 | (0.9, 4.6)*** |
| AISRS-TMOP | 10.98 | (2.30) | 7.66 | (2.83) | 3.2 | (2.3, 4.1)* | 10.58 | (2.59) | 9.70 | (3.16) | 1.0 | (0.1, 1.9)* | 2.2 | (0.9,3.5)*** |
| Conners-Observer-IN2,3 | 72.47 | (10.56) | 66.94 | (11.64) | 5.7 | (3.1, 8.3)* | 74.33 | (9.67) | 73.19 | (10.33) | 0.9 | (−2.0, 3.9) | 4.8 | (0.8, 8.7)* |
| Brown-Total T-Score | 84.73 | (8.82) | 75.80 | (12.63) | 9.1 | (6.0, 12.2)* | 85.72 | (9.53) | 76.80 | (11.00) | 8.8 | (5.6, 12.0)* | 0.3 | (−4.2, 4.7) |
| BRIEF-A Metacog Index3 | 78.37 | (8.69) | 73.83 | (9.01) | 5.39 | (2.2, 8.6)* | 80.71 | (9.24) | 78.64 | (11.52) | 1.26 | (−2.0, 4.6) | 4.13 | (−0.5, 8.7)+ |
| ON-TOP | −40.56 | (23.87) | −22.10 | (20.64) | −17.9 | (−23.7, −2.1)* | −37.87 | (22.57) | −28.98 | (24.67) | −9.5 | (−15.5,−3.4)* | −8.4 | (−16.8, 0.0)+ |
| Beck Depression (BDI-II) | 11.48 | (9.59) | 9.66 | (8.31) | 1.8 | (−0.1, 3.7) | 11.34 | (8.12) | 9.08 | (7.16) | 2.3 | (0.3, 4.3)* | −0.5 | (−3.2, 2.2) |
| Hamilton - Total Anxiety | 9.56 | (5.37) | 8.07 | (5.38) | 1.2 | (−0.2, 2.7) | 8.45 | (5.20) | 8.88 | (5.63) | −0.2 | (−1.7, 1.3) | 1.4 | (−0.7, 3.5) |
| Hamilton - Observed Anxiety4 | 0.65 | (0.74) | 0.50 | (0.64) | 0.2 | (−0.0, 0.3) | 0.50 | (0.64) | 0.65 | (0.70) | −0.1 | (−0.3, 0.1) | 0.3 | (−0.0, 0.5) |
| Rosenberg Self-Esteem | 16.93 | (5.14) | 18.39 | (6.02) | −1.3 | (−2.6, 0.0) | 18.37 | (5.62) | 19.50 | (5.86) | −1.3 | (−2.7, 0.1) | −0.0 | (−1.9, 1.9) |
p <.10,
p<.05;
p<.01;
p<.005,
p<.001 Scores for CAARS, Brown, and BRIEF are T-scores.
AISRS = Adult ADHD Investigator Symptom Rating Scale (blind structured interview; IN=inattentive symptoms, TMOP=symptoms relating to time-management, organization, and planning). Conners-Observer-IN=Conners Adult ADHD Rating Scales-Observer: Long Version, Inattention/Memory subscale. BRIEF-A = Behavior Rating Inventory of Executive Function – Adult Version. ON-TOP=self-report questionnaire On Time-Management, Organization, and Planning; range of scores for ON-TOP is −102 to +102.
Least Squares Mean Change is change from baseline (pre minus post) adjusted for baseline value.
MCT n=34, Support n=27.
The difference between Groups was no longer significant (Conners-Observer-IN) or no longer approached significance (BRIEF-A) after excluding non-completers and medication changers.
This refers to anxiety observed and rated by the interviewer during the structured interview.
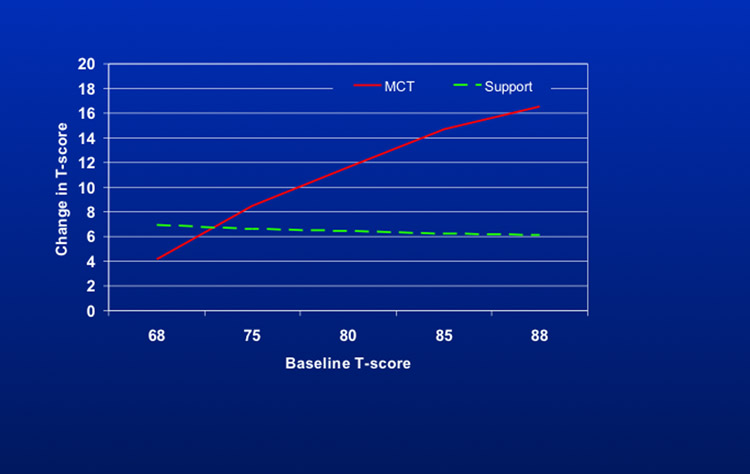
Only one statistically significant interaction between baseline score, Conners-Self-Inattention, and response to treatment was observed. The results of the analysis of change in Conners-Self-Inattention are thus presented separately in Table 4 and Figure 2 since there can be no single contrast between treatment groups given the presence of the interaction. The pattern of treatment contrasts indicated that the larger (more severe) the score at baseline, the greater the differential improvement with MCT; this occurred whether the data were analyzed with or without non-completers and medication changers (interaction coefficients 0.66 and 0.72, respectively). Change in the Support group, by contrast, was stable across the entire range of baseline Conners-Self-Inattention scores. Baseline AISRS-IN did not interact with treatment in the analysis comparing change in AISRS following MCT versus Support. With respect to the change in score on the AISRS-IN from pre- to post-treatment, controlling for baseline AISRS-IN, Table 3 indicates that the MCT group improved by 5.0 points, whereas Support improved by 2.3 points, a difference between groups of 2.7 (95% CI = 0.9, 4.6; p<0.005) or 56% of the overall standard deviation of the change score (4.8). The same pattern (i.e., greater change in MCT vs. Support), was evident on the AISRS-TMOP and the CAARS-Observer-Inattention. On all of the foregoing measures, examination of confidence limits revealed significant change from pre- to post-treatment for Support as well as MCT. On the Brown and the ON-TOP, there was significant change from pre- to post-treatment for Support as well as MCT. However, the change score difference between groups was not significant (Brown) or only marginally significant (ON-TOP). The BRIEF-A Metacognitive Index yielded marginally significant greater improvement in MCT compared to Support; change in MCT but not Support was significant.
Table 4.
CAARS-IN Self-Report as a function of Baseline CAARS-IN Self-Report Values
| Baseline Conners Self–IN Value |
%ile in sample | Least Squares (LS) Mean Change scores
|
Difference between LS Mean Change scores |
(95%CI) | |||
|---|---|---|---|---|---|---|---|
| MCT Group (n=41) | (95%CI) | Support Group (n=38) | (95%CI) | ||||
| 68 | 5th | 4.16 | (−0.53, 8.85) | 6.91 | (2.04, 11.77) | −2.74 | (−9.51, 4.02) |
| 75 | 25th | 8.50 | (5.58, 11.42) | 6.62 | (3.68, 9.56) | 1.88 | (−2.27, 6.02) |
| 80 | 50th | 11.60 | (9.23, 13.97) | 6.42 | (3.95, 8.89) | 5.18 | (1.75, 8.60) |
| 85 | 75th | 14.70 | (11.82, 17.58) | 6.22 | (2.99, 9.45) | 8.48 | (4.15, 12.81) |
| 88 | 95th | 16.56 | (13.00, 20.11) | 6.10 | (2.06, 10.14) | 10.46 | (5.08, 15.84) |
Note. Conners-Self-IN=Conners Adult ADHD Rating Scales-Self-Report - Inattention/Memory subscale.
Figure 2.
Change in Conners-Self-Inattention as a function of baseline score.
Analyses of Measures of Comorbidity
No differences were observed between treatment groups in pre- to post-change scores for depression (Beck), self-esteem (Rosenberg) or anxiety (Hamilton). With the exception of a small but significant improvement on the Beck in the Support condition, examination of confidence intervals for change scores for each treatment group separately showed no significant effects for any of these outcome variables. Given that the sample as a whole scored within normal limits on the Beck, we re-examined the data to ascertain whether there was a significant decrease in Beck scores for those individuals with a concurrent Axis I mood disorder. Results of ANOVA showed that for these participants mean Beck scores decreased from 17 to 13, yielding a significant main effect of Time (pre- to post-treatment), F (1,24) =4.998, p=.035, but no interaction with treatment condition. The same analysis was done for those with a current anxiety disorder vis-à-vis scores on the Hamilton with no significant results.
Intra-Cluster Correlation
Mixed model analyses of variance were run to adjust for intra-cluster correlation using Group, Therapist, and Cohort as clusters. Therapist consistently did not account for any intra-cluster correlation. Adjusting for Group and Cohort simultaneously as random variables did not affect the significance of the treatment effects noted in Table 3.
Responder Analyses
Results were also examined to determine whether participants exhibited clinically meaningful change in response to treatment. On the blind structured interview of DSM-IV inattention symptoms (AISRS-IN), a positive response was defined as a decrease of 30% (maximum score = 27), a criterion that has conventionally been used in pharmaceutical trials (9). Positive response on the Conners-Self-Inattention scale was defined as a decrease of 10 T-score points (1 SD). Seven participants who dropped out, and for whom post-treatment data were not available, were conservatively scored as non-responders on these variables.
On the AISRS-IN, 19 participants (42.2%) in the MCT group were responders, compared to only 5 (12%) in Support (χ2 = 10.38, df=1, p=.002). On the Conners-Self-Inattention, 24 (53%) in the MCT group and 12 (28%) in the Support group were responders (χ2 = 5.88, df=1.p=.018). Logistic regression, with AISRS-IN responder status as the dependent variable, was conducted to control for baseline AISRS-IN score. Results revealed a significant effect of Treatment Group on responder status (odds ratio of 5.41; 95% CI = 1.77,16.55) favoring MCT.
Analyses of Completers
The above analyses were repeated excluding all those who were non-completers or medication changers. The pattern of significance across dependent measures was identical to that of the entire sample except that the effect of treatment was no longer significant for the Conners Observer-Inattention report, F(1,50) = 2.59, p=.1141, a result most likely due to the reduction in sample size.
Expectancy for Change and Credibility of Treatments
Expectancy of change and treatment credibility were assessed using two questions (coded on a 4-point Likert Scale) derived from Borkovec (35) concerning the anticipated helpfulness of treatment and confidence in recommending the treatment to another. Group responses were compared prior to the start of treatment and again at the end of session 2, when participants had been exposed to the treatment group methods but before actual change due to treatment might have confounded measurement of expectancy. Results (Table 5) indicated no significant difference between groups at pre-treatment, nor significant change in either group after exposure to two treatment sessions.
Table 5.
Expectancy for Change and Treatment Credibility
| Meta-Cognitive Therapy | Support Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-Treatment | Session 2 | Pre-Treatment | Session 2 | |||||
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | |
| Helpfulness | 2.35 | (.734) | 2.33 | (.796) | 2.41 | (.609) | 2.30 | (.696) |
| Confidence | 1.83 | (.718) | 2.17 | (.718) | 2.42 | (.669) | 2.23 | (.725) |
Note. The first question was, “How helpful do you think this treatment will be for you?” The second question was, “How confident would you be in recommending this treatment to a friend who has ADHD?” Responses were recorded on a 4-point Likert scale: 0=“Not At All Helpful/Confident”, 1= “Slightly…,” 2= “Moderately…,” 3 = “Very Helpful/Confident.” There were no significant differences between groups.
Moderators of Response
The following covariates were added one-by-one to the General Linear Model to examine whether these potential moderators attenuated or interacted with the effects of treatment: Age, gender, ethnicity, education, household income, marital status, employment status, IQ, ADHD subtype, concurrent medication for ADHD, and comorbid depressive and/or anxiety disorder. In each analysis the effect of MCT vs. Support remained significant while controlling for the covariate, and in no case did the covariate interact significantly with the treatment effect.
In the total sample of 88, 49 (56%) were receiving FDA-approved medication for ADHD. Of these 36 patients (18/treatment group) were receiving a minimally adequate dose, defined as 20 mg daily of methylphenidate, 20 mg daily of amphetamine, or 40 mg daily of atomoxetine, as determined on the basis of the most recent dose-response studies in adults (36–38). Treatment groups did not differ significantly in the type, adequacy, or dose of medication treatment (Table 6). Unexpectedly, adequately medicated patients did not differ from other patients on any measure of baseline severity of ADHD symptoms. Chi-square analysis revealed no difference between these subsets of patients in response rate to treatments, as defined on either blind structured interview (AISRS) or by Conners Selfrating (p>.05); effect sizes (Eta) were .033 and .053, respectively. Similarly, ANOVA of dimensional scores on the Conners-Self-Inattention rating showed no impact of medication on response: The effect size (partial eta squared) corresponding to the three-way interaction among medication, time (pre-to post-treatment) and treatment group was <.001. The effect size corresponding to the medication × time interaction (collapsed across treatments) was .002. For subjects who completed the study (n=31 adequately medicated vs. 39 unmedicated or inadequately medicated), effect sizes for the double interaction were similar to those for the full sample (.001 for the two-way and three-way interactions).
Table 6.
Mean Daily Doses of ADHD Medications in Meta-Cognitive Therapy (MCT) and Support Groups
| Medication | n | Mean Daily Dose (mg)1 | (SD) | Minimum Daily Dose (mg) | Maximum Daily Dose (mg) |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| MCT | 8 | 51.38 | (29.5) | 20 | 90 |
| Support | 10 | 49.00 | (18.4) | 27 | 80 |
| Amphetamine | |||||
| MCT | 5 | 40.00 | (23.5) | 20 | 80 |
| Support | 7 | 32.14 | (19.1) | 20 | 70 |
| Atomoxetine | |||||
| MCT | 6 | 90.00 | (16.7) | 60 | 100 |
| Support | 3 | 73.33 | (30.6) | 40 | 100 |
Treatment groups did not differ significantly in mean dosages.
Note: For purposes of this analysis, doses of Focalin (n=2) and Vyvanse (n=2) were converted to equivalent doses of d,l methylphenidate or amphetamine (Adderall) respectively. Two other patients were taking two different stimulants (ie methylphenidate or amphetamine) or a stimulant plus atomoxetine (Strattera). In those instances, only the methylphenidate equivalent dose was entered. In two cases an adequate dose was discontinued before the midpoint of the Group. These patients were not included as “adequately dosed”. In cases (n=2) in which there was a dose change in the second half of the program; only the dose at the start of the program was recorded.
Mediators of Response
Session attendance and completion of the home exercise in the MCT group were examined as potential mediators of change in AISRS-IN score. Regression analysis indicated that attendance was not related to response and did not mediate the treatment effect. However, within the MCT group, completion of the home exercise was significantly related, F(1,38)=6.49, p = .015, to change in AISRS-IN score, with a 0.85 score increase from baseline for each home exercise completed.
Discussion
The current study was designed to assess the efficacy of a cognitive-behavioral intervention (MCT) for treatment of adult ADHD. Those randomized to MCT showed greater improvement on standardized measures of inattentive symptoms, whether self-rated, observer-rated, or rated by a blind evaluator, than did those in a Supportive group condition. The finding on the AISRS structured interview favoring a clinically significant response for MCT over Support (odds ratio of 5.41) provides strong support for the efficacy of this intervention. The fact that groups were initially found to be equivalent with respect to expectancy for change suggests that positive expectancy cannot fully account for change. Furthermore, the finding that completion of the home exercise was significantly related to treatment response provides evidence that change was mediated by the active MCT treatment components. The same may be said of the finding that baseline severity was related to the outcome of MCT, whereas change in the Support condition was constant across all levels of severity. The significantly higher total rate of non-completion and medication change in Support compared to MCT may be interpreted as an indication that patients felt they were deriving less benefit from this intervention.
Although the magnitude of change on the primary outcome measures strongly favored the MCT group, it is noteworthy that individuals in the Support group also reported improvement. It may be that the support in the group reduced demoralization and improved hopefulness, which in turn motivated Support participants to tackle their own difficulties and/or discover solutions through reading, talking to others, or trial and error.
The lack of significant change on measures of comorbidity (Beck Depression, Rosenberg Self-Esteem, Hamilton Anxiety) in MCT may have been due to floor effects on these measures, as scores at baseline were, on average, not in the clinically significant range. Support for this possibility was generated by a post-hoc analysis of Beck scores for patients with a concurrent mood disorder, which revealed a significant decrease from pre- to post-treatment for the combined sample, but no differential effect of Group assignment. A parallel result was not obtained on the Hamilton Anxiety interview for those with concurrent anxiety disorders.
The failure of medication to act as a treatment moderator may be due to several possibilities. First, we had not expected that patients receiving adequate medication would not differ in baseline symptom severity from those not receiving medication. Given that participants were required to meet entry criteria for minimum levels of severity of symptoms, we may have been effectively selecting those who were non-responders or suboptimal responders to medication. Additionally, although we conducted moderator analyses on a subset of medicated participants who appeared to be receiving minimally adequate amounts of medication, doses for these individuals may not have been adequately titrated by community practitioners, and may have been suboptimal. A final possibility is that the program is sufficiently structured and effective that patients are able to benefit irrespective of whether they are receiving effective medication. A more rigorous examination of the effects of medication and MCT, separately and together, would require a 2 × 2 design in which medication treatment is optimally titrated for each individual within the study proper.
Although other demographic and clinical variables did not have significant effects on outcome, larger samples, with greater power, may be needed to fully ascertain the effects of these potential moderating and mediating variables. In particular, although IQ was not a moderator of response, it should be noted that the mean IQ in this sample was above average. A sample with greater range would be needed to fully assess the potential moderating effect of IQ and to gauge the generalizability of these treatment results to adults across a broader range of IQ.
Overall, the results of this study indicate that MCT provides significant benefit to patients with ADHD with respect to inattentive symptoms that reflect the specific functions of time-management, organization, and planning. It is the first published study to formally demonstrate the efficacy of a psychosocial treatment in adults with ADHD compared to a condition that controlled for the non-specific effects of therapy. It thereby represents a noteworthy contribution to a developing literature supporting the benefits of cognitive-behavioral treatment – whether delivered in groups or individually - for the treatment of ADHD in adults. It will be important in future studies to examine the maintenance of these benefits beyond the termination of treatment proper, as well as to determine the relative efficacy of pharmacotherapy and psychosocial treatments, separately and together, for the treatment of this condition.
Acknowledgments
The study was supported by NIMH Grant 1R34MH071721 to the first author.
We gratefully acknowledge the expert consultation concerning cognitive-behavioral therapy provided by Jacqueline Gollan, Ph.D. and Richard Heimberg, Ph.D. We also acknowledge the contributions of Megan Wilens, MD and Heather Goodman, Ph.D. who served as blind evaluators as well as the assistance of Lauren Knickerbocker, M.A. with manuscript preparation.
Footnotes
The results of this study were presented at the 14th Scientific Meeting of the International Society for Research in Child and Adolescent Psychopathology (ISRCAP) in Seattle, Washington in June, 2009.
Disclosures: Dr. Solanto is currently on the Medical Advisory Board for Shire Pharmaceuticals. She has previously served as a consultant and speaker for Ortho-McNeil-Janssen Pharmaceuticals, Inc. During the past five years, Dr. Abikoff has received research funding from the National Institute of Mental Health, the Hughes, Lemberg and Heckscher Foundations, Ortho-McNeil, Shire, and Eli Lilly; has consulted to Shire, Eli Lilly, Cephalon, and Novartis; and has a financial interest in the Children’s Organizational Skills Scale, published by Multi-Health Systems. Drs. Marks, Wasserstein, Mitchell, Alvir, and Kofman have no competing interests.
References
- 1.Kessler RC, Adler LA, Barkley RA, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. Am J Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life areas. J Am Acad Child Adolesc Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 3.Biederman J, Monuteaux MC, Mick F, Spencer T, Wilens TE, Silva JM, Snyder LE, Faraone SV. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med. 2006;36(2):167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 4.Wilens TE, Biederman J, Mick E, Faraone SV, Spencer T. Attention deficit hyperactivity disorder (ADHD) is associated with early onset substance use disorders. J Nerv Ment Disease. 1997;185:475–482. doi: 10.1097/00005053-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Spencer T, Biederman J, Wilens T, Doyle R, Surman C, Prince J, Mick E, Alcardi M, Herzig K, Faraone S. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(5):456–463. doi: 10.1016/j.biopsych.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 6.Michelson D, Adler L, Spencer T, Reimherr FW, West SA, Allen AJ, Kelsey D, Wernicke J, Dietrich A, Milton D. Atomoxetine in adults with ADHD: two randomized, placebo-controlled studies. Biol Psychiatry. 2003;15:112–120. doi: 10.1016/s0006-3223(02)01671-2. [DOI] [PubMed] [Google Scholar]
- 7.Wolf LE, Wasserstein J. Adult ADHD. Concluding thoughts. Ann N Y Acad Sci. 2001;931:396–408. [PubMed] [Google Scholar]
- 8.Douglas VI. Cognitive control processes in Attention-Deficit/Hyperactivity Disorder. In: Quay HC, Hogan AE, editors. Handbook of Disruptive Behavior Disorders. New York: Kluwer Academic/Plenum Publishers; 1999. pp. 105–138. [Google Scholar]
- 9.Wilens TE, Spencer TJ, Biederman J. A review of the pharmacotherapy of adults with attention-deficit/hyperactivity disorder. J Attent Disord. 2002;5:189–202. doi: 10.1177/108705470100500401. [DOI] [PubMed] [Google Scholar]
- 10.Weiss M, Safren SA, Solanto MV, Hechtman L, Rostain AL, Ramsay JR, Murray C. Research forum on psychological treatment of adults with ADHD. J Attent Disord. 2008;11(6):642–651. doi: 10.1177/1087054708315063. [DOI] [PubMed] [Google Scholar]
- 11.McDermott SP, Wilens TE. Cognitive therapy for adults with ADHD. In: Brown T, editor. Attention deficit disorders and comorbidities in children, adolescents, and adults. Washington, DC: American Psychiatric Press; 2000. pp. 569–606. [Google Scholar]
- 12.Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, Ebert I. Psychotherapy of attention deficit hyperactivity disorder in adults - a pilot study using a structured skills training program. Eur Arch Psychiatry Clin Neurosci. 2002;252:177–184. doi: 10.1007/s00406-002-0379-0. [DOI] [PubMed] [Google Scholar]
- 13.Virta M, Vedenpaa A, Gronroos N, Chydenius E, Partinen M, Vataja R, Kaski M, Iivanainen M. Adults with ADHD benefit from cognitive-behaviorally oriented group rehabilitation: A study of 29 participants. J Attent Disord. 2008;12(3):218–226. doi: 10.1177/1087054707311657. [DOI] [PubMed] [Google Scholar]
- 14.Rostain AL, Ramsay JR. A combined treatment approach for adults with ADHD - results of an open study of 43 patients. J Attent Disord. 2006;10(2):150–159. doi: 10.1177/1087054706288110. [DOI] [PubMed] [Google Scholar]
- 15.Stevenson CS, Whitmont S, Bornholt L, Livesey D, Stevenson RJ. A cognitive remediation programme for adults with Attention Deficit Hyperactivity Disorder. Aust N Z J Psychiatry. 2002;36:610. doi: 10.1046/j.1440-1614.2002.01052.x. [DOI] [PubMed] [Google Scholar]
- 16.Safren SA, Otto MW, Sprich S, Winett CL, Wilens TE, Biederman JJ. Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behav Res Ther. 2005;43(7):831–842. doi: 10.1016/j.brat.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Roberts AH, Kewman DG, Mercier L, Hovell M. The power of nonspecific effects in healing: implications for psychosocial and biological treatments. Clin Psychol Rev. 1993;13(5):375–391. [Google Scholar]
- 18.Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1(2):138–155. [Google Scholar]
- 19.Knouse LE, Sprich S, Cooper-Vince C, Safren SA. ADHD symptom profiles in medication-treated adults entering a psychosocial treatment program. Journal of ADHD and Related Disorders. 2009;1:34–47. [PMC free article] [PubMed] [Google Scholar]
- 20.Solanto MV, Marks DJ, Mitchell K, Wasserstein J, Kofman MD. Development of a new psychosocial treatment for adults with AD/HD. J Attent Disord. 2008;11(6):728–736. doi: 10.1177/1087054707305100. [DOI] [PubMed] [Google Scholar]
- 21.Epstein JN, Johnson DE, Conners CK. Conners’ Adult ADHD Diagnostic Interview for DSM-IV. North Tonawanda, NY: Multi-Health Systems; 2001. [Google Scholar]
- 22.Conners CK, Erhardt D, Epstein JN, Parker JDA, Sitarenios G, Sparrow E. Self-ratings of ADHD symptoms in adults I: Factor structure and normative data. J Attent Disord. 1999;3:141–151. [Google Scholar]
- 23.Erhardt D, Epstein JN, Conners CK, Parker JDA, Sitarenios G. Self-ratings of ADHD symptoms in adults II: Reliability, validity, and diagnostic sensitivity. J Attent Disord. 1999;3:153–158. [Google Scholar]
- 24.Barkley RA, Murphy KR. Attention-deficit hyperactivity disorder: A clinical workbook. New York, NY: The Guilford Press; 1998. [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders- Patient Edition (SCID-I/P, 11/2002 revision) New York, N.Y. 10032: Biometrics Research Department; New York State Psychiatric Institute; 1051 Riverside Drive - Unit 60: 2002. [Google Scholar]
- 26.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Persontlity Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 27.Tellegen A, Briggs PF. Old wine, new skins: Grouping Wechsler subtests into new scales. J Consult Clin Psychol. 1967;31(5):499–506. doi: 10.1037/h0024963. [DOI] [PubMed] [Google Scholar]
- 28.Adler LA, Spencer T, Biederman J. Adult ADHD Investigator Symptom Rating Scale -AISRS. Massachusetts General Hospital and New York University School of Medicine; 2003. [Google Scholar]
- 29.Shear MK, Vanderbilt J, Rucci P, Endicott J, Lydiard B, Otto MW, Pollack MH, Chandler L, Williams J, Ali A, Frank D. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001;13:166–178. [PubMed] [Google Scholar]
- 30.Brown TE. Attention-Deficit Disorder Scales: Manual. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 31.Roth RM, Isquith PK, Gioia GA. Behavior Rating Inventory of Executive Function -Adult Version (BRIEF-A) Lutz, FL: Psychological Assessment Resources, Inc; 2005. [Google Scholar]
- 32.Beck AT, Steer RA, Brown GK. Beck Depression Inventory - II (BDI-II) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 33.Rosenberg M. Society and the Adolescent Self-Image. Princeton, N.J: Princeton University Press; 1965. [Google Scholar]
- 34.Waltz J, Addis ME, Koerner K, Jacobson NS. Testing the integrity of a psychotherapy protocol: Assessment of adherence and competence. J Consult Clin Psychol. 1993;61:620–630. doi: 10.1037//0022-006x.61.4.620. [DOI] [PubMed] [Google Scholar]
- 35.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–260. [Google Scholar]
- 36.Spencer TJ, Adler LA, McGough JJ, Muniz R, Jiang H, Pestreich L Adult ADHD Research Group. Efficacy and safety of dexmethylphenidate extended-release capsules in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61(12):1380–1387. doi: 10.1016/j.biopsych.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 37.Medori R, Ramos-Quiroga A, Casas M, Kooij JJS, Niemela A, Trott G-E, Lee E, Buitelaar JK. A randomized, placebo-controlled trial of three fixed dosages of prolonged-release OROS methylphenidate in adults with Attention-Deficit/Hyperactivity Disorder. Biol Psychiatry. 2008;63:981–989. doi: 10.1016/j.biopsych.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Weisler RH, Biederman J, Spencer TJ, Wilens TE, Faraone SV, Chrisman AK, Read SC, Tulloch SJ. Mixed amphetamine salts extended-release in the treatment of adult ADHD: a randomized, controlled trial. CNS Spectr. 2006;11(8):625–639. doi: 10.1017/s1092852900013687. [DOI] [PubMed] [Google Scholar]