Abstract
Aims
Problem solving is deemed a core skill for patient diabetes self-management education. The purpose of this systematic review is to examine the published literature on the effect of problem-solving interventions on diabetes self-management and disease control.
Data Sources
We searched PubMed and PsychINFO electronic databases for English language articles published between November 2006 and September 2012. Reference lists from included studies were reviewed to capture additional studies.
Study Selection
Studies reporting problem-solving intervention or problem solving as an intervention component for diabetes self-management training and disease control were included. Twenty-four studies met inclusion criteria.
Data Extraction
Study design, sample characteristics, measures, and results were reviewed.
Data Synthesis
Sixteen intervention studies (11 adult, 5 children/adolescents) were randomized controlled trials, and 8 intervention studies (6 adult, 2 children/adolescents) were quasi-experimental designs.
Conclusions
Studies varied greatly in their approaches to problem-solving use in patient education. To date, 36% of adult problem-solving interventions and 42% of children/adolescent problem-solving interventions have demonstrated significant improvement in HbA1c, while psychosocial outcomes have been more promising. The next phase of problem-solving intervention research should employ intervention characteristics found to have sufficient potency and intensity to reach therapeutic levels needed to demonstrate change.
Day-to-day management of diabetes is primarily in the hands of the patient [1]; therefore, patients require education and skills training to perform diabetes self-management. The American Association of Diabetes Educators (AADE) named seven self-management behaviors that each individual with diabetes must learn and master: 1) blood glucose self-monitoring; 2) taking medications; 3) healthy eating; 4) being active; 5) reducing risks; 6) healthy coping; and 7) problem solving [2]. Problem solving is a cognitive-behavioral process by which a person attempts to identify effective and adaptive solutions for specific problems encountered in everyday living [3]. In the AADE 7 framework, problem solving is defined as “a learned behavior that includes generating a set of potential strategies for problem resolution, selecting the most appropriate strategy, applying the strategy, and evaluating the effectiveness of the strategy [2].” Problem-solving facilitates enactment of each of the other self-management behaviors [2,4]. In behavioral science, problem solving has been a long-standing, effective, therapeutic intervention approach for behavior change [3]; however, its application to diabetes self-management is more recent [5].
In 2007, the AADE solicited systematic reviews on each of the seven self-management behaviors. An initial systematic review of problem solving in diabetes self-management and control was published, which addressed definitions and frameworks for problem solving in diabetes self-management, and evidence for problem solving as (1) an outcome that can be measured, (2) a behavior associated with self-management behaviors and clinical outcomes, (3) an effective intervention for improving self-management and/or disease control, and (4) a tool used by health care professionals [6]. The systematic review concluded that 50% of adult problem-solving studies and 25% of studies with children/adolescents reported improvement in HbA1c, and effect on behavioral and psychosocial outcomes was varied. Methodological limitations in the design and reporting of the research, however, hindered recommendations regarding intervention content delivery for effectiveness. The purpose of this current review is to examine the published literature during the period since the previous review on problem solving interventions for diabetes self-management and disease control.
METHODS
Search
Searches were conducted in PubMed (National Library of Medicine and National Institutes of Health) and PsycINFO (a database of psychological literature). The following medical subject heading (MeSH) terms were used to search each database: diabetes mellitus, problem solving, problem focused, decision making, self-management, and self-care. In order to capture all articles not presented in the previous review, searches spanned the dates November 2006 to September 2012. Searches were limited to peer-reviewed, English-language articles and human subjects. Dissertations were excluded from the searches.
Selection
Results from the searches of the identified databases were compared and duplicate findings were removed. Abstracts for each unique finding were reviewed (by K.P.S. and F.H.B.) for relevance to the topic. Exclusion criteria were as follows: (1) not an investigation of problem solving (e.g., unrelated to the topic or only a report of problems/barriers without investigation of problem solving), (2) investigation of clinical problem solving or clinical decision making (e.g., medical diagnostics) by professionals, (3) did not report on persons with diabetes (e.g., mixed disease samples that excluded or included very few persons diagnosed with diabetes), or (4) cross-sectional, non-intervention studies. Selected studies were reviewed in full, and their reference lists were scanned for additional studies not captured in the initial search. Inclusion criteria for full review were author description of problem-solving as a main intervention, description of problem solving as a component of an intervention, or report of use of problem-solving steps [3]. Selected studies were examined (by K.P.S. and S.L.F.) to determine if they were appropriate for the current review based on exclusion and inclusion criteria listed above. Any discrepancies were resolved through discussion for 100% consensus.
Data Abstraction
Data abstraction was performed by two investigators independently (K.P.S. and S.L.F.). The abstractions were reviewed by a third investigator (F.H.B.). In the data abstraction process, two studies were identified as not meeting previously stated inclusion criteria and were therefore excluded.
Study Characteristics examined in abstraction:
! ! Sample characteristics: sample size, type 1 or type 2 diabetes, age, gender, race/ethnicity, education, SES.
! ! Study design: randomized controlled trial or quasi-experimental design.
! ! Methods: measurement tools, procedures.
! ! Results: problem solving, self-management behaviors, and physiological, psychosocial, and process outcomes.
Missing data are denoted in the summary tables as not reported.
RESULTS
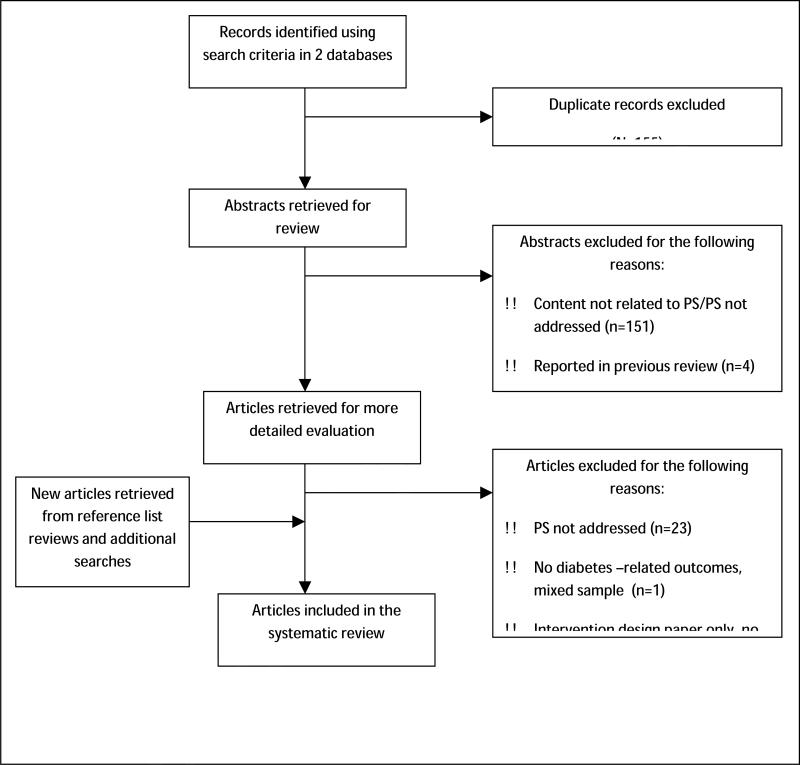
The number of studies identified and excluded at each stage of the search, selection, and data abstraction are presented in Figure 1. Twenty-four unique studies were included in the review.
Figure 1.
Flow diagram of record identification and selection for study inclusion in systematic review for 2006-2012.
Study Characteristics
The 24 intervention studies applied the following research designs: randomized controlled trial (n = 17) [7-23] and quasi-experimental or preintervention/postintervention design (n = 8) [24-32].
Of the intervention studies, 17 (71%) were conducted with adults and 7 (29%) examined children and/or adolescents. Three (13%) studies [9,16,17] examined only females and 2 (8%) studies did not report gender [21,30], but the rest of the studies included both genders. Race/ethnicity of study participants was not reported in 3 (13%) studies [18,22,31]. One study examined Caucasians [32], 12 (50%) studies included multiple ethnicities (generally Caucasian, African American, and Latino)[7,11,12,14-16,19,21,23,25,26,30], 5 (21%) studies were African American only [8,9,20,27,28], 2 study samples were Latino[13,17], and 1 study sample was South Korean [24].
Data Synthesis
Studies were divided by age group (i.e., adult studies, n=17; and child/adolescent studies, n=7) for reporting of results.
Adult Intervention Studies of the Effect of Problem Solving on Diabetes Outcomes
Of the 17 studies of adults, 11 were randomized controlled trials, and six were quasi-experimental designs (Table 1). The extent and manner in which problem-solving was included in the intervention varied greatly. One study reported an intervention that was solely problem-solving-based [8]. In five (29%) of the studies, problem-solving was one component of a larger intervention that utilized other treatment approaches [9,12,16,24]. In seven (41%) of the studies, only certain steps of problem-solving were included in the intervention (e.g., goal setting or action planning) [13-15,18,19,25,26]. In the remaining three studies (18%), the intervention did not consist of problem-solving skills training, but rather a problem-solving based support group [17,27,28] or was included as one of multiple components of an intervention package [20,30]. Interventions were delivered in varying formats, including individual face-to-face [9,12,16,18,20,24,25], group face-to-face [8,13,14,17,18,20,25-28,30], phone-based [12,13,16,25], DVD-based [30], internet-based [15], and video-conferencing [19]. Four sets of outcomes were reviewed for each intervention study: physiological outcomes, self-management behaviors, problem solving, and psychosocial outcomes.
Table 1.
Adult Problem-Solving Intervention Studies from 2006-2012
| Study | Design | Sample | Intervention (I) and Control (C) Groups | Resultsa |
|---|---|---|---|---|
| Amoako et al. (2007, 2008)[9, 10] | RCT | N = 68; mean age = 61 y; type 2; 100% female; 100% African American; recruited from physician clinics | C – Usual care I – DM-UMI: 4 weekly sessions (10-60 minutes each) delivered via phone by a nurse |
Between-group differences at 6-week follow-upb ! ! Physio: NR ! ! SMB: Exercise (+); Diet (-); SMBG (-); Foot Care (-); Med Adherence (-) ! ! PS: NR ! ! Psych: DM knowledge (+); Patient-provider communication (+); Uncertainty in illness (+); Cognitive reframing (+) ! ! TS: NR |
| Simon et al. (2007)[12] | RCT | N = 329; mean age = 57-58 y; 96% type 2; 34% female; 75% Caucasian; recruited from primary care clinics | C – Usual care: pharmacotherapy, structured problem-solving psychotherapy, or both. I – Stepped care: step one – antidepressant pharmacotherapy or structured problem-solving psychotherapy; step two – combining meds and therapy or adjusting meds; step three – in- person consult with psychiatrist or referral for specialty mental health treatment; initial 60 minutes with depressionnurse specialist followed by twice monthly in-personor phone contact (30 min); in-person or phone follow-ups after the initial session for 12 months |
6-month, 12-month, 24-month follow-upb ! ! Physio: HbAlc (-) ! !SMB: NR ! ! PS: NR ! ! Psych: Depression (+) ! !TS: NR |
| Lorig et al. (2008)[13] | RCT | N = 417 (C) n = 198; mean age = 52.8 y; 67.2% female; 100% Latino/Spanish Speaking; (I) n = 219; mean age = 52.9 y; 57.1% female; 100% Latino/Spanish Speaking; recruited from community | Study 1: C – Usual care wait list I – SDSMP: 6 sessions (2.5 hours each) with peer leaders, no reinforcement Study 2: C2 – No reinforcement of SDSMP from study one I2 – Monthly automated telephone reinforcement of SDSMP from study 1 |
Study 1: Between-group differences at 6-month follow-upb ! ! Physio: HbAlc (+); Symptoms of hypoglycemia (+); Symptoms of hyperglycemia(-) ! ! SMB: Aerobic exercise (-); stretching/strength exercise (-); SMBG (-) ! ! PS: NR ! ! Psych: Health distress (+); self-efficacy (+); communication with physician (-) ! ! TS: NR Study 2: 18-month follow-upb ! ! Physio: HbAlc, between-group differences (-), C2 group (+); Symptoms of hypoglycemia, between-group differences (-), C2 group (+); Symptoms of hyperglycemia, between-group differences (-), C2 group (+) ! !SMB: Aerobic exercise, between-group differences (-), C2 group (-); stretching/strength exercise, between-group differences (-), C2 group (-); SMBG, between group differences (+), C2 group (-) ! !PS: NR ! !Psych: Self-efficacy, between-group differences (-), C2 group (+); Communication with physician, between-group differences (-) ! !TS: NR |
| Utz et al. (2008)[20] | RCT | N = 21; type 2; 100% African American; recruited from rural community (11)n = 8; mean age = 56.6 y; 75% female (12)n = 13; mean age = 62.4 y; 76.9% female | I1– Individual DSME (based on AADE 7): 3 sessions after baseline (week 1, week 4, week 8) I2– Group DSME (based on AADE 7): 8 weekly 2hr sessions |
Between-group differences at Post-intervention follow-upc ! ! Physio: HbAlc (-) ! !SMB: General diet (-); Specific diet (-); Carb Spacing (-); Exercise (-); SMBG (-); Foot care (-); Comprehensive foot care (-); Med Adherence (-); Smoking (-) ! !PS: NR ! !Psych: Self-efficacy (-) ! !TS: NR |
| Lorig et al. (2009)[14] | RCT | N = 352; type 2; recruited from community (C) n = 159; mean age = 65.4 y; 66.2% female; 70.6% Caucasian (I) n = 186; mean age = 67.7 y; 62.4% female; 64% Caucasian | C – Usual care I – DSMP: 6-weeks, 2.5 hour group workshops,content = AADE 7 plus additional self-management topics, peer-led |
Between-group differences at 6 month follow-upb ! ! Physio: HbA1c (-); Weight (-); Symptoms hypoglycemia(+); Symptoms hyperglycemia (-) ! ! SMB: Aerobic exercise (+); SMBG (+); Healthy eating (+); Reading food labels (+); Communication with physician (+) ! ! PS: NR ! ! Psych: Depression (+); Self-efficacy (+); Patient activation (+) ! !TS: NR |
| Lorig et al. (2010)[15] | RCT | N = 76; mean age = 54.3 y; type 2; 73% female; 76% Caucasian, 14% American Indian/Alaska Native; recruited from community and healthcare providers | C – Usual care I – IDSMP: Internet delivery with peer facilitators of online forums, online content plus interactive activities |
6-month follow-upb ! ! Physio: HbA1c, I group (-), between-group differences (+) ! ! SMB: Aerobic exercise, I group (-), between-group differences (-) ! !PS: NR ! !Psych: Depression, I group (-), between-group differences (-); patient activation , I group (-), between-group differences (+); self-efficacy, I group (+) and between-group differences (+) ! !TS: NR 18-month follow-upb ! !Physio: HbA1c (NR) ! !SMB: Aerobic exercise, between-group differences (-) ! !PS: NR ! !Psych: Depression (-); patient activation, between-group differences (+); self-efficacy, between-group differences (+) ! !TS: NR |
| Allen et al. (2011)[16] | RCT | N = 29; type 2; 100% female; recruited from large health system in Massachusetts (C) n = 15; mean age = 51.7 y; 66.7% Caucasian, 20% African American, 13.3% Latina (I) n = 14; mean age = 52.2 y; 64.3% Caucasian, 14.3% African American, 21.4% Latina | C – 90-minute counseling session with certified diabetes educator on continuous glucose monitoring and impact on physical activity; 90-minute diabetes education session provided by certified diabetes educator; and follow-up phone call 4 weeks later I – 90-minute counseling session on continuous glucose monitoring; 90- minute problemsolving skills counseling provided by nurse interventionist with focus on barriers to physical activity; and follow-up phone call 4 weeks later |
Between-group differences at 3-month follow-upb ! ! Physio: HbA1c (-); Systolic BP (-); Diastolic BP (-); Weight (-) ! !SMB: Personal Eating Plan (+); Healthful Eating Plan (-); Fruit and Vegetable consumption (-); High Fat Food consumption (-); Exercise (-); Minutes in Sedentary Activity (-); Minutes in Light Activity (-); Minutes in Moderate Activity (-) ! !PS: DPSI (+) ! !Psych: Depression (-); Self-efficacy for Physical Activity (-) ! !TS: NR |
| Hill-Briggs et al. (2011)[8] | RCT | N = 56 adults; type 2; 100% African American; recruited from diabetes registry from urban community practice sites (I1) n = 27; mean age = 61.5 y; 66.7% female (I2) n = 29; mean age = 61.1 y; 51.7% female | I1– DECIDE Condensed: 1 group self-management education session (90 min) followed by 1 condensed group PST session (60 min), based on D'Zurilla and Nezu's problem-solving therapy I2– DECIDE Intensive: 1 group self-management education session (90 min) followed by 8 group PST sessions (60 min), based on D'Zurilla and Nezu's problem-solving therapy |
1-week post-intervention follow-upc ! ! Physio: NR ! ! SMB: NR ! ! PS: Health Problem Solving Scale (-) ! ! Psych: DM and CVD knowledge, I group (+), C group (+); Barriers to DM Self-Management, I group (+), C group (-) ! ! TS: Patient workbooks: >4.71 (scale 1-5) on helpfulness, ease of understanding, ease of visual presentation; Group sessions: >4.75 (scale 1-5) on helpfulness, ease of understanding, and overall satisfaction 3-month post-intervention follow-upc ! !Physio: HbA1c, I group (+), C group (-), between group difference (+) ! !SMB: SDSCA, I group (+), C group (-) ! !PS: Health Problem Solving Scale, I group (+), C group(-) ! !Psych: DM and CVD knowledge, I group (+), C group (-); Barriers to DM Self-Management, I group (-), C group (-) ! !TS: NR |
| Toobert et al. (2011)[17] | RCT | N = 280; type 2; 100% Latina females; recruited from Kaiser Permanente Colorado Clinics and 1 large community health center (C) n = 138; mean age 58.7 y; 14.7% prefer Spanish (I) n = 142; mean age = 55.6 y; 17% prefer Spanish | C – Usual Care I – Usual care plus 2.5 day retreat followed by 1-hour meetings encouraging participants to: a) follow the Mediterranean diet adapted for Latin American culture; b)practice stress management techniques daily; c)engage in physical activitydaily for 30 minutes; d) stop smoking; and e) take part in problem solving-based support groups. Meetings were held weekly for first 6 months and twice monthly for next 6 months. |
Between group differences at 6-month follow-upb ! ! Physio: HbA1c (+); 10-year heart disease risk score (+) ! ! SMB: Diet (+); Exercise (+); Smoking (-) ! ! PS: DPSI (+) ! ! Psych: Self-efficacy (+); Perceived Support (+); Stress Management practice (+); Use of social and environmental resources (+); Physical HQOL (-); Mental HQOL (-); Change in PS and change in diet (+); Change in PS and change in stress management (-); Change in PS and change in exercise (-); Change in PS and change in use of social and environmental resources (+); Change in PS and change in HbA1c, 10-year CHD risk score, physical HQOL, and mental HQOL (-) ! !TS: NR Between group differences at 12-month follow-upb ! !Physio: HbA1c (-); 10-year heart disease risk score (?) ! !SMB: Diet (-); Exercise (-); Smoking (-) ! !PS: DPSI (+) ! !Psych: Selfefficacy (+); Perceived Support (+); Stress Management practice (+); Use of social and environmental resources (?); Physical HQOL (-); Mental HQOL (-); Change in PS and change in diet (-); Change in PS and change in stress management (-); Change in PS and change in exercise (+); Change in PS and change in use of social and environmental resources (-); Change in PS and change in HbA1c, 10-year CHD risk score, physical HQOL, and mental HQOL (-) ! !TS: NR |
| Trief et al. (2011)[18] | RCT | N = 44; mean age = 59.9 y; 64% female; ethnicity NR; recruited through letters and advertisements | C – Enhanced usual care I1– Individual intervention, 11 sessions I2– Couples intervention, 11 sessions |
6-month follow-upb ! ! Physio: HbAlc (-); Total Cholesterol, Il group (+), I2 group (+); Systolic BP (-); BMI (-); LDL (-); Waist circumference (-) ! !SMB: Diet (-); SMBG (-) ! ! PS: NR ! ! Psych: NR ! ! TS: NR |
| Trief et al. (2012)[19] | RCT | N = 1665; mean age = 70.8 y; 62.8% female; 49.4% Caucasian, 14.9% African American, 35.2% Hispanic, .5% Other; mean education = 9.8 y; recruited through primary care providers (C) n = 821; mean age = 70.9 y; 62.1% female; mean education = 9.9 y (I) n = 844; mean age = 70.8 y; 63.5% female; mean education = 9.7 y |
C – Usual care I – IDEATel Intervention: Televisits every 4-6 weeks over 5 years (study duration) with nurse case manager and dietitian via a home telemedicine unit. At each visit the educator and participant set a behavioral goal, address barriers to achieving goal and develop action plan. At the following visit behavioral goals are reviewed and action plans are revised if goal has not been met. |
5-year follow-upb ! ! Physio: HbA1c (NR) ! ! SMB: SDSCA, between group differences (+) ! ! PS: NR ! ! Psych: NR ! ! TS: NR |
| Klug et al. (2008)[26] | Quasi-experimental (pre-post design with no control group) | N = 179; mean age = 69.2 y; type 2; 78.2% female; 72% Caucasian, 1% African American, 11% American Indian, 8% Asian American, 1% Multiracial, 7% other; recruited from community | C – No control or comparison group I – Healthy Changes™: Weekly group sessions lasting 1.5 hours, 26 topics covered, # of sessions attended ranged from 0-46, peer leaders in community setting |
4-month follow-upb ! !Physio: BMI (-) ! !SMB: Diet (+); Physical Activity (+); number of days following a healthful diet (-); number of days engaged in physical activity (-) ! !PS: NR ! !Psych: Self-rated health (-); Use of supportive resources (+) ! !TS: 68-76% of participants rated the intervention as helpful in reaching program goals |
| DeWalt et al. (2009)[25] | Quasi-experimental (pre-post design with no control group) | N = 250; mean age = 56 y; type 2; 65% female; 22% Caucasian, 45% African American, 33% Latino/Hispanic, 31% Spanish; recruited from internal medicine practices | C – No control or comparison group I – 15 min brief counseling (FTF) followed by two brief counseling sessions at 2 and 4 weeks over the phone; intervention focused on setting an action plan |
2, 4, and 12 week follow-upb ! ! Physio: NR ! ! SMB: NR ! ! PS: 13% demonstrated problem-solving around goals, at 4 weeks post-baseline – 16%, at 12 weeks post-baseline – 20% ! ! Psych: NR ! ! TS: 75% Very/Extremely likely to keep using DM guide; 81% Very/Extremely likely to recommend DM guide |
| Glasgow et al. (2009)[30] | Quasi-experimental (Preference/Randomized Design) | N = 155; type 2; gender NR; recruited from Kaiser Permanente Colorado Health Plan DM Registry (I1) mean age = 63.5 y; 16.1% Latino/Hispanic (I2) mean age = 63.4 y; 15.3% Latino/Hispanic | I1 – DSME Class (based on AADE 7): 2 (2.5-3 hr) classes I2 – DVD (based on AADE 7): 7 segments recommended to be done in 2-3 sessions |
6-month follow-upb ! !Physio: HbA1c (-); LDL (-); Systolic BP (-) ! !SMB: Diet (-); Exercise (-); Med Adhere (-); SMBG (-) ! !PS: DM Problem Solving Scale (-) ! !Psych: Self-Efficacy (-); Patient Activation (-); DM Distress (-) ! !TS: 54% DVD was fairly or extremely helpful; 46% class was extremely helpful |
| Tang et al. (2010)[27] | Quasi-experimental (Time-Series Design) | N = 77; mean age = 61 y; type 2; 69% female; 100% African American; recruited from community | C – Participants serve as their own controls (time-series design) I–LM: Empowerment Approach (Anderson and Funnell): 24 sessions |
6 month follow-upb ! ! Physio: HbAlc (-);Total cholesterol (+); Diastolic BP (+); Weight (-); BMI (-); Systolic BP (-); HDL (-); LDL (-) ! !SMB: Diet (+); SMBG (+); Carb spacing (-); Exercise (-); Foot care (-); Med Adherence (-); Insulin Adherence (-) ! ! PS: NR ! ! Psych: DM empowerment (-); DM QOL (-) ! ! TS: NR 6 months post-intervention follow-upc ! ! Physio: HbA1c (+); Weight (+); BMI (+); LDL (+); HDL (x); Systolic BP (-); Diastolic BP (-); Total Cholesterol (-) ! !SMB: Diet (-); SMBG (-); Carb spacing (-); Exercise (-); Foot care (-); Med Adherence (-); Insulin Adherence (-) ! !PS: NR ! !Psych: DM empowerment (-); DM QOL (-) ! !TS: NR |
| Lee et al. (2011)[24] | Quasi-experimental (pre-post design with comparison group) | N = 57; type 2; 100% South Koreans; recruited from 3 endocrinology or internal medicine clinics in an urban city of South Korea (I1) n = 28; mean age 63.2 y; 64.3% female (I2) n = 29; mean age 61.1 y; 44.8% female | I1– Problem-solving counseling based on the PS model of chronic disease self-management along with a recommendation to walk at moderate intensity (i.e., 40-60% of maximum heart rate) 5 times per week for > 30 minutes and self-monitor walking with diaries. 12-week intervention. I2– Same problem-solving counseling and walking recommendation provided in I1, but walking monitored by ambulatory heart rate monitor with instantaneous feedback. 12-week intervention. |
3-month post-intervention follow-upc ! ! Physio: HbA1c, I1 group (+) I2 group (+); Glycemic control (glucose), I1group (+) I2 group (+); BMI, I1 group (+) I2 group (-); Total cholesterol, I1 group (-) I2 group (-); HDL, I1 group (-) I2 group (-); LDL, I1 group (-) 12group (-); Triglycerides, I1 group (-) I2 group (-); CRP, I1 group (-) I2 group (-); Tissue plasminogen activator, I1 group (-) I2 group (+); Plasminogen activator inhibitor 1, I1 group (+) I2 group (-); Parma Cardiovascular Risk Index, I1 group (-) I2 group (-) ! !SMB: NR ! !PS: NR ! !Psych: Affective-oriented coping, I1 group (-) I2 group (-); Problem-oriented coping, I1 group (-) I2 group (-) ! !TS: NR 6-month post-intervention follow-upc ! !Physio: HbA1c, I1 group (-) I2 group (x); Glycemic control (glucose), I1 group (-) I2 group (-); BMI, I1 group (-) I2 group (x); Total cholesterol, I1 group (-) I2 group (-); HDL, I1 group (-) I2 group (-); LDL, I1 group (-) I2 group (-); Triglycerides, I1 group (-) I2 group (-); CRP, I1 group (+) I2 group (-); Tissue plasminogen activator, I1 group (-) I2 group (-); Plasminogen activator inhibitor 1, I1 group (-) I2 group (+); Parma Cardiovascular Risk Index, I1 group (-) I2 group (+) ! !PS: NR ! !Psych: Affective-oriented coping, I1 group (-) I2 group (-); Problem-oriented coping, I1 group (-) I2 group (-) ! !TS: NR |
| Tang et al. (2011, 2012)[28,29] | Quasi-experimental, prospective (participants had received DSME prior to enrolling in the study and received DSME enhancement or DSMS during the course of the study) | N = 60; mean age = 62.4 y; type 2; 70% female; 100% African American; recruited from community | I1– DSME Enhancement: 6 months of mailed DSME to reinforce DSME received in the past I2– DSMS: 88 weekly sessions (75 min each) over 24 months using Anderson and Funnell's empowerment approach in addition to DSME received in the past |
6-month follow-up, DSME Enhancementb ! ! Physio: HbAlc (-); Total Cholesterol (+); Diastolic BP (+); Weight (-); BMI (-); Systolic BP (-); HDL (-); LDL (-) ! !SMB: Diet (+); SMBG (+); Foot care (+); Carb spacing (-); Exercise (-); Med Adherence (-); Insulin Adherence (-) ! ! PS: NR ! ! Psych: DM empowerment (-); DM QOL (-) ! ! TS: NR 24-month follow-up, DSMSb ! ! Physio: HbA1c (-); Total Cholesterol (-); Diastolic BP (-);Weight (-); BMI (-); Systolic BP (-); HDL (-); LDL (-) ! !SMB: Diet (+); Carb spacing (+); Insulin Adherence (+); Exercise (-); Foot care (-); Med Adherence (-); SMBG (-) ! !PS: NR ! !Psych: DM QOL (+); DM empowerment (-) ! !TS: NR 1-year post-intervention follow-up, DSMSc ! !Physio: HbA1c (+); Total Cholesterol (+); LDL (+); Diastolic BP (x); HDL (x); Weight (-); BMI (-); Systolic BP (-) ! !SMB: Diet (-); Carb spacing (-); Insulin Adherence (-); Exercise (-); Foot care (-); Med Adherence (-); SMBG (-) ! !PS: NR ! !Psych: DM QOL (-); DM empowerment (-) ! !TS: NR |
AADE, American Association of Diabetes Educators; BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; DECIDE, Decision-Making Education for Choices in Diabetes Everyday; DM, diabetes; DM-UMI, Diabetes Uncertainty Management Intervention; DPSI, Diabetes Problem-Solving Inventory; DSME, diabetes self-management education; DSMP, Diabetes Self-Management Program; DSMS, Diabetes Self-Management Support; FTF, face-to-face; HDL, high-density lipoprotein; IDSMP, Internet Diabetes Self-Management Program; LDL, low-density lipoprotein; LM, Lifelong Management; NR, not reported; Physio, physiological outcomes; PS, problem solving; PST, problem-solving training; Psych, psychosocial outcomes; SDSCA, Summary of Diabetes Self-care Activities; SDSMP, Spanish Diabetes Self-management Program; SMB, self-management behaviors; SMBG, self-monitoring of blood glucose; TS, treatment satisfaction.
Results are categorized as problem solving, self-management behaviors, physiological outcomes, psychosocial outcomes, and treatment satisfaction. The symbol (-) indicates that the specified intervention outcome was not statistically significant; (+) indicates that the specified intervention outcome was statistically significant in the hypothesized direction; (x) indicates that the specified intervention outcome was statistically significant but not in the hypothesized direction; (?) indicates that the specified intervention outcome was not clearly stated in the article.
Follow-up time frame is number of weeks or months from baseline. Intervention duration within that time frame is indicated in the Intervention and Control Groups column.
Follow-up time frame is reported at post-intervention, i.e., number of weeks or months from conclusion of the intervention.
Physiological Outcomes
Physiological outcomes were reported in 15 (88%) of the studies, with 14 (93%) of those reporting HbA1c. With regard to outcomes, 7 (50%) studies reported significant improvements in HbA1c following intervention [8,13,15,17,24,27,29], ranging from -0.09 to -0.93. These improvements in HbA1c were seen over 3 to 12 months of follow-up. In three studies, however, the improvement in HbA1c was not maintained at 6-month follow-up [24], 12-month follow-up [17], or 18-month follow-up [13]. One study reported that an increase in adherence (assessed by the Summary of Diabetes Self-Care Activities [33]) was a significant mediator of improved glycemic control over five years [19].
Other physiological outcomes reported included: total cholesterol (n=4), LDL (n=6), HDL (n=3), systolic blood pressure (n=6), diastolic blood pressure (n=4), weight (n=3), BMI (n=5), waist circumference (n=1), and symptoms of hypo/hyperglycemia (n=2). Two studies [18,27] demonstrated significant improvement in total cholesterol immediately following the intervention, while one study did not [24,27,28]. The immediate improvement in total cholesterol reported by Tang et al. [27] was not maintained at six months post-intervention. However, a study that did not see immediate improvements in total cholesterol found significant improvement at one-year post-intervention [28]. Two of six studies found significant improvement in LDL following intervention, the first [27] noted a decrease of 8.47 mg/dL following intervention and the second [8] reported a median decrease of 25.0 mg/dL among the subset of persons with suboptimal LDL at baseline, but without an overall group-level effect. One study [24,28] reported no significant change in HDL while two studies [27,28] found that HDL significantly worsened following intervention. A majority of studies [16,18,27,30] reported no effect of the intervention on either systolic BP or on diastolic BP [16,27,28]. Two studies reported significant effect on diastolic BP immediately following the intervention [27,28], while one study reported clinically significant reductions in systolic blood pressure (median reduction of 7.17 mm/Hg) and diastolic (median reduction of 14.67 mm/Hg) blood pressure in those patients with suboptimal BP at baseline but found no overall group effect [8]. Overall, studies reported no improvement in BMI [18,24,26,28], weight [16,28], or waist circumference [18] following the intervention. A set of studies by Lorig and colleagues reported symptoms of hyper- and hypoglycemia as an outcome. Two studies [13,14] reported no effect of the intervention on symptoms of hyperglycemia. One study [13] reported a significant effect of the intervention on symptoms of hypoglycemia, which did not persist to the 18-month follow-up, while the other study [14] found no effect of the intervention on symptoms of hypoglycemia.
Self-management behaviors
Fifteen (88%) studies with adults reported self-management behaviors as intervention outcomes. Most frequently reported were diet (n=10), exercise (n=11), self-monitoring of blood glucose (n=8), and medication adherence (n=5). Of the 10 studies reporting dietary outcomes, six (60%) [14,16,17,26-28] reported a significant effect of the intervention on one or more aspects of following a healthy diet, while 4 studies [10,18,20,30] reported no effect of the intervention on any aspect of following a healthy diet. Of the 11 studies reporting physical activity outcomes, three (27%) reported a significant effect of the intervention on one or more aspects of physical activity, while 8 studies [13-16,20,27,28,30] reported no effect of the intervention on physical activity. All 8 studies assessing self-monitoring of blood glucose [10,13,14,18,20,27,28,30] reported no effect of the intervention. Similarly, none of the 5 studies assessing medication adherence [10,20,27,28,30] reported a significant effect of the intervention. Both studies [8,19] reporting global diabetes adherence (Summary of Diabetes Self-Care Activities scale) found significant improvement in self-management behaviors overall following intervention.
Problem solving
Problem-solving skill or process was reported in 5 (29%) of the studies with adults. Each study used a different problem-solving measure and examined a different intervention approach. One study reported increased problem solving following brief in-person counseling plus two telephone counseling sessions at 2 and 4 weeks [25]. A second study demonstrated that problem solving significantly improved over 3-months post-intervention following group-delivered intensive (8 session), but not brief (1 session) problem-solving training [8]. Another study did not find a significant change in problem solving following AADE-based education presented on a DVD [30]. Problem solving increased and there was significant between group differences in problem-solving at 3-month follow-up for participants who received a 90-minute problem-solving skills counseling session with a nurse versus those who only received a 90-minute diabetes education session with a diabetes educator [16]. A culturally adapted diabetes self-management intervention for Latinas also resulted in an increase in problem-solving at 3-months and significantly higher problem solving at 3- and 6-month follow-ups compared to usual care [17].
Psychosocial outcomes
Fifteen (88%) studies reported psychosocial outcomes. Most commonly assessed were self-efficacy (n=7), patient activation (n=3), depression (n=4), and patient-provider communication (n=3). Four of 7 studies (57%) [13-15,17] reported a significant, positive effect of the intervention on self-efficacy, while 3 studies [16,20,30] reported no effect of the intervention on self-efficacy. Patient activation did not significantly improve in any of the three studies assessing this outcome [13-15]. Two of 4 studies [12,14] reported a significant effect of the intervention on depression, while the remaining two studies [15,16] reported no effect of the intervention on depression. Two of 3 studies [9,14] demonstrated a significant effect of the intervention on patient-provider communication, while the third study [13] reported no significant effect of the intervention on patient-provider communication. One study found no effect of the intervention on affective-oriented or problem-solving oriented coping [24]. Another study reported a significant, positive effect on perceived social support, practice of stress management techniques, and use of social-environmental resources, but no effect on physical or mental health quality of life [17].
Child and Adolescent Intervention Studies of the Effect of Problem Solving on Diabetes Outcomes
Of the seven studies of children and adolescents, five (71%) [7,11,21-23] were randomized controlled trials and the remaining two were quasi-experimental designs [31,32] (Table 2). In five (71%) of the intervention studies problem-solving was the main behavioral treatment approach, [7,11,21,22,31] and in two studies problem solving was combined with Behavioral Family Systems Therapy [23] or Cognitive Behavioral Therapy [23,32]. Interventions were delivered in varying formats, including individual face-to-face [32], single family face-to-face [7,11,21,23], group face-to-face [31], multifamily face-to-face [23], internet-based [22], and telephone follow-ups after face-to-face sessions [7,11,21,32]. Three of the studies delivered the intervention during routine clinic visits [7,11,21]. Effect of the intervention on problem-solving, self-management behaviors, physiological outcomes, and psychosocial outcomes are described.
Table 2.
Child and Adolescent Problem-Solving Intervention Studies from 2006-2012
| Study | Design | Sample | Intervention (I) and Control (C) Groups | Resultsa |
|---|---|---|---|---|
| Wysocki et al. (2008)[23] | RCT | N = 104 families with adolescents; aged 11-16;type 1; recruited from two pediatric centers (C) n = 32; 50% female; 53% Caucasian, 34% African American (11)n = 36; 44% female; 75% Caucasian, 25% African American (12)n = 36; 42% female; 61% Caucasian, 33% African American, 3% Latino, 3% other | C: Standard Care I1: Education sessions led by diabetes nurses and health care professionals; guided by ADA curriculum for teens; 12 multifamily sessions in 6 months I2: BFST-D led by psychologist, postdoc, or LCSW; PST is one component of BFST in addition to communication training, cognitive restructuring, functional and structural family therapy; 12 sessions in 6 months (single family) |
6, 12, and 18-month follow-upsb ! ! PS (Coded video-tape of family discussions around problems using Interaction Behavior Code): I2 > C at 12 and 18-months (+); I2 > ES at 18 months (+) ! ! Problem Resolution: I2 > C at all follow-ups (+); I2 > ES at 6 and 18-months (+) ! ! Psych: Adolescent negative communication, I2 < C at all follow-ups (+), I2 < ES at 6-months (+); Adolescent positive communication (-); Mother negative communication, I2 < C at all follow-ups (+), I2 < ES at 6 and 12- months (+); Mother positive communication, I2 > C at all follow-ups (+), I2 > ES at 6 and 12-months (+); Father negative communication (-); Father positive communication (-); Negative reciprocity, I2 < C at 6 and 12-months (+), I2 < ES at 6-months (+); Positive reciprocity, I2 > C at all follow-ups (+), I2 > ES at 6 and 12-months (+) ! ! TS: NR 6-month follow-upb (I2) ! ! Physio: PS and HbA1c (+); Problem Resolution and HbA1c (+) ! !SMB: PS and DSMP (+); Problem Resolution and DSMP (-) ! !Psych: PS and DRC (-); Problem Resolution and DRC (+) 12-month follow-upb (I2) ! !Physio: PS and HbA1c (-); Problem Resolution and HbA1c (-) ! !SMB: PS and DSMP (+); Problem Resolution and DSMP (+) ! !Psych: PS and DRC (-); Problem Resolution and DRC (+) 18-month follow-upb (I2) ! !Physio: PS, Problem Resolution & HbA1c (-) ! !SMB: PS, Problem Resolution and DSMP (-) ! !Psych: PS, Problem Resolution and DRC (-) |
| Wysocki et al. (2008)[7] | RCT | 114 youth and 109 parents; type 1; aged 9-14.5; 51% female; 71% Caucasian, 12% African American, 10% Latino, 7% other; parents - 35% some college; 40% $50,000-100,000; recruited from 4 pediatric diabetes centers across US | C: Usual care I: 3 sessions of a family-focused, low-intensity behavioral intervention applying basic problem-solving strategy to daily problems in management of diabetes delivered during quarterly routine diabetes clinic visits over 6-months; clinic encounters followed by telephone calls to evaluate and refine intervention plan |
Post-intervention follow-upb ! ! Physio: HbA1c between group differences (-) ! ! SMB: DSMP between group differences (-) ! ! PS: DPSI between group differences (-) ! ! Psych: DFRQ between group differences (-) ! ! TS: NR |
| Nansel et al. (2009)[21] | RCT | 122 adolescents (30-32 families); aged 9-14.5; type 1; gender NR; 71.1% Caucasian, 11.6% African American, 9.9% Latino, 7.4% other; 45.4% of parents had a college degree; 77.4% of families reported annual income of $50,000 or greater; recruited from four major medical centers (C) n = 62 (I) n = 60 |
C: Usual care I: WE*CAN intervention (W for work together to set goals; E for explore possible barriers and solutions; C for choose the best solutions; A for act on your plan; and N for note the results) delivered by specially trained graduate students at 3 routine clinic visits over a maximum of 12 months with telephone follow-up at weeks 2 and 6. Specific objectives were to improve disease management problem solving, improve parent-child cooperation and communication and reduce conflict regarding disease management, and facilitate appropriate sharing of disease management responsibility. |
Post-intervention follow-upb ! ! Physio: HbA1c, I group (-), C group (-), between-group differences (-) ! ! SMB: DSMP, I group (-); DSMP, C group (-); DSMP between-group differences (-) ! ! PS: NR ! ! Psych: PedsQOL, I group (-), between-group differences (-); DQOL, I group (-), between-group differences (-); Parent-Child Conflict, I group (-), between-group differences (-); Responsibility Sharing, I group (-), between-group differences (-) ! ! TS: 97.7% of youth and 93.4% of parents liked intervention |
| Mulvaney et al. (2010)[22] | RCT | 52 adolescents; type 1; aged 13-17 years old; 49% female; ethnicity NR; recruited from pediatric diabetes clinics (C) n = 18 (I) n = 34 |
C: Usual care I: YourWay, an 11- week internet-based intervention with 6 multimedia stories depicting psychosocial barriers to self-management and problem solving and multimedia presentations on the steps of problem solving; included help from problem-solving expert |
Post-intervention follow-upb ! ! Physio: HbA1c, I group (-), between-group differences (-) ! ! SMB: DBRS, I group (?), between-group differences (+) ! ! PS: DPSB, I group (-), between-group differences (-) ! ! Psych: NR ! ! TS: 63% gave intervention an ‘A’, 37% gave it a ‘B’ |
| Nansel et al. (2012)[11] | RCT | 390 adolescents; aged 9-14.9; type 1; recruited from four major medical (C) n = 189; mean age = 12.4y; 50.8% female; 74.4% Caucasian, 10.8% African American, 9.1% Hispanic, 5.7% Other (I) n = 201; mean age = 12.5 y; 50.7% female; 75.5% Caucasian, 7.8% African American, 10.9% Hispanic, 5.7% Other | C: Usual care I: WE*CAN intervention (W for work together to set goals; E for explore possible barriers and solutions; C for choose the best solutions; A for act on your plan; and N for note the results) delivered by trained health advisors at each routine clinic visits over a maximum of 21 months with telephone follow-up at weeks 2 and 6. |
24-month follow-upb ! ! Physio: HbA1c between group differences (+) for ages 12-14 at both 18-month and 24-month follow-up; Change in HbA1c and change in parental DSMP (+), change in SMBG (-), change in adolescent DSMP (-) ! ! SMB: DSMP between-group differences (-); SMBG (x) ! ! PS: NR ! ! Psych: NR ! ! TS: NR |
| Loding et al. (2007)[31] | Quasi-experimental (pre-post design with no control group) | 19 adolescents and 17 mothers; type 1; aged 13-18; 52.6% female; ethnicity NR; recruited from two diabetes centers in Norway (I1)n = 5 (I2)n = 6 (I3)n = 6 |
C: No control or comparison group I: Education, support and problem solving sessions once a month for 1 hour; adolescent and parent groups separate; I1 and I2 received 10 group sessions and I3 received 6 group sessions |
12- and 24-month follow-upb ! ! Physio: HbA1c (-) for total sample, HbA1c (+) for girls only at 12 months ! ! SMB: NR ! ! PS: NR ! ! Psych: DQOL (-); ! ! TS: NR |
| Salamon et al. (2010)[32] | Quasi-experimental (pre-post design with no control group) | 10 adolescents; type 1; aged 11-18; 40% female; 100% Caucasian; recruited from outpatient diabetes clinic | C: No control or comparison group I: CBT program which aimed to train adolescents to develop cognitive restructuring and behavioral problem-solving skills. Initial session was 60-90 minutes delivered in patient's home by psychology doctoral students followed by 3 individual weekly phone contacts. |
1-month follow-upb ! ! Physio: NR ! ! SMB: SCF (-) ! ! PS: NR ! ! Psych: DSQ (-) ! ! TS: NR |
BFST-D, Behavioral Family Systems Therapy-Diabetes; CBT, Cognitive Behavioral Therapy; DBRS, Diabetes Behavior Rating Scale; DFRQ, Diabetes Family Responsibility Questionnaire; DPSB, Diabetes Problem-Solving Behavior Scale; DPSI, Diabetes Problem Solving Inventory; DSMP, Diabetes Self-Management Profile; DQOL, Diabetes Quality of Life Scale; DRC, Diabetes Responsibility & Conflict Scale; DSQ, Diabetes Stress Questionnaire; LCSW, licensed clinical social worker; NR, not reported; Physio, physiological outcomes; PS, problem-solving; PST, Problem Solving Therapy; Psych, psychosocial outcomes; RCT, randomized controlled trial; SCF, Self-care Around Friends Scale; SMB, self-management behaviors; SMBG, self-monitoring of blood glucose; TS, treatment satisfaction.
Results are categorized as problem solving, self-management behaviors, physiological outcomes, psychosocial outcomes, and treatment satisfaction. The symbol (-) indicates that the specified intervention outcome was not statistically significant; (+) indicates that the specified intervention outcome was statistically significant in the hypothesized direction; (x) indicates that the specified intervention outcome was statistically significant but not in the hypothesized direction; (?) indicates that the specified intervention outcome was not clearly stated in the article.
Follow-up time frame is number of weeks or months from baseline. Intervention duration within that time frame is indicated in the Intervention and Control Groups column.
cFollow-up time frame is number of weeks or months from conclusion of the intervention.
Physiological Outcomes
Six (86%) of the intervention studies examined HbA1c as an outcome. No other physiological outcomes were reported. Only two of the six studies (33%) reported significant improvement in HbA1c associated with the intervention. Loding et al, [31] found a significant decrease in HbA1c (from 9.4% to 8.4%) in girls, but not in boys, at the 12 month follow-up. Among adolescents who received BFST-D [23] problem-solving and poor problem resolution was significantly, positively correlated with HbA1c level at the six month follow-up assessment. In the feasibility test of the WE*CAN intervention [21] there was no significant effect on HbA1c at follow-up; however, there were significant between group differences for change in HbA1c in the larger trial at the 24-month follow-up among older adolescents (i.e., 12-14 years old) [11]. Furthermore, Nansel et al. [11] reported a significant relationship between change in parent-reported adherence and change in HbA1c, but no significant relationship between change in HbA1c and change in blood glucose monitoring or adolescent-reported adherence. There were no significant changes in HbA1c in the other two studies [7,22].
Self-management Behaviors
One study examined the relationship between problem-solving skills and self-management behaviors after intervention [23] and five studies assessed between-group differences in self-management behaviors following problem-solving intervention [7,11,21,22,32]. In Wysocki et al. [23] use of the problem-solving process was significantly correlated with higher scores on a general measure of diabetes self-management at 6-months and 12-months post-baseline and problem resolution was significantly correlated with an increase in self-management behaviors at 12-months post-baseline. There were no significant associations at 18-months post-baseline. Each of five studies that examined group differences in self-management behaviors at post-intervention utilized a global measure of diabetes behaviors [7,11,21,22,32]. Only one of the five studies found a significant effect of the intervention on self-management at the post-intervention follow-up [22].
Problem Solving
Change in problem-solving skill or process was examined in three (43%) of the intervention studies. In one study [23], participants in Behavioral Family Systems Therapy – Diabetes (BFST-D) had significantly better problem solving skills than standard care at 12 and 18 month post-baseline follow-ups and Education Session participants at 18 months post-baseline. Also, problem resolution was significantly higher for those in BFST-D compared to standard care at all time points and better than the education intervention at 6 and 18-months [23]. However, two studies found that there was no intervention effect or significant differences between the intervention and control groups on problem-solving [7,22].
Psychosocial Outcomes
All children/adolescent intervention studies except one examined psychosocial outcomes, including diabetes care responsibility, conflict, quality of life, and diabetes related stress, and studies generally reported improvement in one or more aspect of communication or conflict. Problem resolution, but not problem-solving process, was significantly associated with less diabetes conflict at the 6- and 12-month follow-ups among those who received the BFST-D [23]. Furthermore, adolescents and mothers who received BFST-D displayed significantly less negative communication and mothers in this group demonstrated significantly more positive communication than participants in the standard care group at each follow-up time point [23]. BFST-D was significantly better than the Education Session condition for reducing adolescent negative communication at the 6-month follow-up only and for reducing the mother's negative communication and increasing mother's positive communication at 6- and 12-month follow-ups. Participants in the BFST-D group displayed significantly less negative reciprocity than the standard condition at 6- and 12-months and the Education Session condition at 6-months only. The BFST-D group had significantly higher positive reciprocity than the standard condition at all follow-ups and significantly higher than the Education Session condition at 6- and 12-months. There were no significant between-group differences in adolescents’ use of positive communication or fathers’ communication style.
Studies reported no significant effect of intervention on diabetes stress [32], diabetes-specific or general pediatric quality of life [21,31], or parent-child conflict or responsibility sharing [21]. Finally, three (50%) of the studies provided qualitative data on patient satisfaction with the intervention. For the WE*CAN intervention (feasibility study) [21], 97.7% of children/adolescents and 93.4% of parents agreed or strongly agreed that overall they liked being in the intervention. In the study on an internet-based problem-solving intervention [22], 63% of the children/adolescents gave the intervention an ‘A.’ Children/adolescents participating in the Loding et al. study [31] reported feeling more able to discuss issues about diabetes more calmly with parents.
DISCUSSION AND CONCLUSIONS
This current review encompassing literature published during the period from November 2006 – September 2012, examined the evidence of problem-solving interventions on diabetes self-management and control since the previous systematic review [6] that included intervention research from 1990 – 2006. Conclusions regarding the problem-solving intervention literature are discussed in the context of intervention design, delivery, and populations and characteristics of effective interventions.
Problem-solving intervention design, delivery, and populations
The current review period demonstrated increased modalities for problem-solving intervention delivery, particularly new use of internet and DVD approaches. However, primary delivery modalities, across both review periods, remained group-based contacts in studies with adults [68,13,14,17,18,20,25-28,30,31], and in-person family contacts in studies with children/adolescents [6,7,11,21,23]. In this current review, there were three child/adolescent studies that demonstrated the feasibility of delivering a problem-solving intervention during routine clinic visits [7,11,21].
Studies examined in this current review were more likely to provide information on who delivered the intervention and in some cases how the interventionists were trained and supervised. Professional background, training, and discipline of the interventionists varied greatly and included college graduates, graduate student therapist/psychology doctoral students, diabetes nurses, diabetes educators, licensed social workers, geriatric nurse practitioners, clinical psychologists, psychiatrists, and depression nurse specialists. Additional evaluation needs to be conducted to determine experience and training requirements for personnel to be effective in delivering a problem-solving intervention as well as the feasibility of routinely implementing problem-solving interventions in clinical practice settings.
There is inconsistency in how problem-solving interventions have been conceptualized across the treatment studies included in both reviews. Some studies address problem-solving as an educational topic, among several other topics of education; others describe use of problem-solving as a process that is support-group based or as a therapeutic modality, either in an informal manner or as a more structured approach within a package of interventions; while others delivered structured patient problem-solving training largely as a stand-alone behavioral intervention. Consistent with the differences in how problem-solving intervention was conceptualized and designed, number of intervention sessions and duration varied widely, spanning a single session, three in-clinic sessions spread out over 6-months to a year, to 4 or more sessions delivered on a routine schedule.
Studies included in this current review suggests that more problem-solving interventions have been applied to more diverse patient populations since the previous review [6]. The majority of studies in this current review reported either multiethnic samples or racial/ethnic minorities as the sole participants in the study. One adult study conducted the intervention completely in Spanish [13] whereas two had bilingual interventionists [17,19]. In addition, some of the child/adolescent studies provided education and income background information on the parents, which mostly consisted of moderate to high socioeconomic status families. Based on this review, there is evidence that problem-solving training and support can feasibly be delivered to various patient populations.
Characteristics of effective problem-solving interventions
Overall, the current review yielded only minimal additional evidence of intervention effectiveness on key outcomes. Combining findings from the 2007 systematic review and the current review, with regard to HbA1c only 38% of the intervention studies reported significant improvement in HbA1c or between-group differences in HbA1c following the intervention (36% of adult studies and 42% of child/adolescent studies). Interestingly, among the adult studies that demonstrated significant improvement in HbA1c, six included samples of only racial/ethnic minorities, suggesting that a problem-solving intervention is an effective approach for diabetes control and self-management among ethnic minorities [8,13,15,17,24,27,28]. Overall, it appeared that both adult and child/adolescent studies that had multiple intervention sessions (~4 or more sessions) with problem-solving as one component of the intervention or patient's receiving training in the steps of problem-solving appeared to be most effective for diabetes self-management and control. However, only one study actually compared the effectiveness of a single problem-solving training session to multiple sessions (i.e., 8 sessions on problem-solving) [8], and demonstrated that the multiple session format of traditional problem-solving therapy [3] was more effective in improving behavioral and physiological outcomes than a single-topic/module approach to problem solving. Although evidence of the effectiveness of one delivery modality over the other is premature at this time, it appears that internet-based interventions may not be as effective for children/adolescents [22,34] as family and group-based approaches to date
In the 2007 review, with regard to behavioral outcomes, evidence appeared strongest for effectiveness of interventions on isolated self-management behaviors in children, adolescents, and adults and on depression in adults. The current review found evidence for intervention effectiveness on self-management behaviors to be inconsistent and weak. Between both reviews very few interventions assessed problem solving as an outcome. Among studies that did, 71% of adult studies and 50% of child/adolescent studies demonstrated a significant effect of problem-solving interventions on problem-solving ability. Interventions that were effective for improving problem solving generally consisted of four or more patient education or problem-solving training sessions [6,8,17]. In addition, it is clear from both reviews that problem-solving interventions consistently have a positive effect on several psychosocial outcomes among adults and children/adolescents.
In conclusion, this current systematic review reveals an increase in the research focusing on intervening on problem solving as a modifiable skill for diabetes self-management and disease control. An encouraging finding was the reporting of investigating different delivery modalities for this intervention approach, as well as expansion of the populations investigated to include more minority and underserved groups. However, this systematic review found persisting methodological limitations in the body of literature that contribute to overall patterns of inconsistency in outcomes of problem-solving interventions to date. The next phase of problem-solving intervention research will need to address whether interventions are designed and delivered with sufficient potency (with regard to problem-solving content and training of patients in problem-solving as a skill set) and sufficient intensity (with regard to treatment dose and duration) to reach therapeutic levels needed to demonstrate change. There is a need for greater consistency in the content of problem-solving interventions in order to compare outcomes across studies. Greater consistency would allow for more in-depth exploration of other factors influencing outcome (e.g., treatment dose, method of delivery, interventionist training, patient characteristics, etc.). In order to achieve greater consistency, researchers should clearly identify what constitutes problem-solving training and use this definition to guide study design. Observed characteristics of effective problem-solving interventions to date should be used to help standardize treatments and to test replication or generalization of effect across patient populations. Additional feasibility studies examining the implementation of behavioral interventions in clinical settings are needed.
Acknowledgments
This research was supported by NHLBI grant R01 HL089751 and NIDDK Diabetes Research and Training Center grant P60 DK079637.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Fisher EB, Brownson CA, O'Toole ML, Anwuri VV, Shetty G. Perspectives on self-management from the diabetes initiative of the Robert Wood Johnson Foundation. Diabetes Educ. 2007;33(Suppl 6):216S–224S. doi: 10.1177/0145721707304124. [DOI] [PubMed] [Google Scholar]
- 2.Mulcahy K, Maryniuk M, Peeples M, et al. Diabetes self-management education core outcomes measures. Diabetes Educ. 2003;29(5):768–70. 773–84, 787–8. doi: 10.1177/014572170302900509. passim. [DOI] [PubMed] [Google Scholar]
- 3.D'Zurilla T, Nezu A. Problem-solving therapy: A positive approach to clinical intervention. 3rd ed. Springer Publishing Company; New York: 2007. [Google Scholar]
- 4.Peeples M, Mulcahy K, Tomky D, Weaver T. National Diabetes Education Outcomes System (NDEOS). The conceptual framework of the National Diabetes Education Outcomes System (NDEOS). Diabetes Educ. 2001;27(4):547–562. doi: 10.1177/014572170102700410. [DOI] [PubMed] [Google Scholar]
- 5.Schumann K, Sutherland JA, Majid HM, Hill-Briggs F. Evidence-based behavioral treatments for diabetes: Problem-solving therapy. Diabetes Spectr. 2011;24:64–69. [Google Scholar]
- 6.Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: A systematic review of the literature. Diabetes Educ. 2007;33(6):1032–50. doi: 10.1177/0145721707308412. discussion 1051-2. [DOI] [PubMed] [Google Scholar]
- 7.Wysocki T, Iannotti R, Weissberg-Benchell J, et al. Diabetes problem solving by youths with type 1 diabetes and their caregivers: Measurement, validation, and longitudinal associations with glycemic control. J Pediatr Psychol. 2008;33(8):875–884. doi: 10.1093/jpepsy/jsn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill-Briggs F, Lazo M, Peyrot M, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amoako E, Skelly AH. Managing uncertainty in diabetes: An intervention for older African American women. Ethn Dis. 2007;17(3):515–521. [PubMed] [Google Scholar]
- 10.Amoako E, Skelly AH, Rossen EK. Outcomes of an intervention to reduce uncertainty among African American women with diabetes. West J Nurs Res. 2008;30(8):928–942. doi: 10.1177/0193945908320465. [DOI] [PubMed] [Google Scholar]
- 11.Nansel TR, Iannotti RJ, Liu A. Clinic-integrated behavioral intervention for families of youth with type 1 diabetes: Randomized clinical trial. Pediatrics. 2012;129(4):e866–73. doi: 10.1542/peds.2011-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simon GE, Katon WJ, Lin EH, et al. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64(1):65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 13.Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self-management with and without automated telephone reinforcement: Two randomized trials. Diabetes Care. 2008;31(3):408–414. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 14.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: A randomized trial. Diabetes Educ. 2009;35(4):641–651. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 15.Lorig K, Ritter PL, Laurent DD, et al. Online diabetes self-management program: A randomized study. Diabetes Care. 2010;33(6):1275–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen N, Whittemore R, Melkus G. A continuous glucose monitoring and problem-solving intervention to change physical activity behavior in women with type 2 diabetes: A pilot study. Diabetes Technol Ther. 2011;13(11):1091–1099. doi: 10.1089/dia.2011.0088. [DOI] [PubMed] [Google Scholar]
- 17.Toobert DJ, Strycker LA, Barrera M, Jr, Osuna D, King DK, Glasgow RE. Outcomes from a multiple risk factor diabetes self-management trial for Latinas: Inverted exclamation markViva bien! Ann Behav Med. 2011;41(3):310–323. doi: 10.1007/s12160-010-9256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trief P, Sandberg JG, Ploutz-Snyder R, et al. Promoting couples collaboration in type 2 diabetes: The diabetes support project pilot data. Fam Syst Health. 2011;29(3):253–261. doi: 10.1037/a0024564. [DOI] [PubMed] [Google Scholar]
- 19.Trief PM, Izquierdo R, Eimicke JP, et al. Adherence to diabetes self care for White, African-American and Hispanic American telemedicine participants: 5 year results from the IDEATel project. Ethn Health. 2012 doi: 10.1080/13557858.2012.700915. [DOI] [PubMed] [Google Scholar]
- 20.Utz SW, Williams IC, Jones R, et al. Culturally tailored intervention for rural African Americans with type 2 diabetes. Diabetes Educ. 2008;34(5):854–865. doi: 10.1177/0145721708323642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nansel TR, Anderson BJ, Laffel LM, et al. A multisite trial of a clinic-integrated intervention for promoting family management of pediatric type 1 diabetes: Feasibility and design. Pediatr Diabetes. 2009;10(2):105–115. doi: 10.1111/j.1399-5448.2008.00448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mulvaney SA, Rothman RL, Wallston KA, Lybarger C, Dietrich MS. An internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes Care. 2010;33(3):602–604. doi: 10.2337/dc09-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wysocki T, Harris MA, Buckloh LM, et al. Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008;39(1):33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Lee H, Kim MS, Park KY, Park HS, Kim IJ. Effects of a problem-solving counseling program to facilitate intensified walking on Koreans with type 2 diabetes. Jpn J Nurs Sci. 2011;8(2):129–139. doi: 10.1111/j.1742-7924.2010.00163.x. [DOI] [PubMed] [Google Scholar]
- 25.DeWalt DA, Davis TC, Wallace AS, et al. Goal setting in diabetes self-management: Taking the baby steps to success. Patient Educ Couns. 2009;77(2):218–223. doi: 10.1016/j.pec.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klug C, Toobert DJ, Fogerty M. Healthy changes for living with diabetes: An evidence-based community diabetes self-management program. Diabetes Educ. 2008;34(6):1053–1061. doi: 10.1177/0145721708325886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang TS, Funnell MM, Brown MB, Kurlander JE. Self-management support in “real-world” settings: An empowerment-based intervention. Patient Educ Couns. 2010;79(2):178–184. doi: 10.1016/j.pec.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang TS, Funnell MM, Noorulla S, Oh M, Brown MB. Sustaining short-term improvements over the long-term: Results from a 2-year diabetes self-management support (DSMS) intervention. Diabetes Res Clin Pract. 2011 doi: 10.1016/j.diabres.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang TS, Funnell MM, Oh M. Lasting effects of a 2-year diabetes self-management support intervention: Outcomes at 1-year follow-up. Prev Chronic Dis. 2012;9:E109. doi: 10.5888/pcd9.110313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glasgow RE, Edwards LL, Whitesides H, Carroll N, Sanders TJ, McCray BL. Reach and effectiveness of DVD and in-person diabetes self-management education. Chronic Illn. 2009;5(4):243–249. doi: 10.1177/1742395309343978. [DOI] [PubMed] [Google Scholar]
- 31.Loding RN, Wold JE, Skavhaug A, Graue M. Evaluation of peer-group support and problem-solving training in the treatment of adolescents with type 1 diabetes. Eur Diabetes Nursing. 2007;4(1):28–33. [Google Scholar]
- 32.Salamon KS, Hains AA, Fleischman KM, Davies WH, Kichler J. Improving adherence in social situations for adolescents with type 1 diabetes mellitus (T1DM): A pilot study. Prim Care Diabetes. 2010;4(1):47–55. doi: 10.1016/j.pcd.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 34.Horan PP, Yarborough MC, Besigel G, Carlson DR. Computer-assisted self-control of diabetes by adolescents. Diabetes Educ. 1990;16(3):205–211. doi: 10.1177/014572179001600311. [DOI] [PubMed] [Google Scholar]