Dear Sir,
I am Dr. Zhi-Qing Li from Tianjin Medical University Eye Hospital, Tianjin City, China. I write to present a case with hiding iris neovascularization (INV) following central retinal vein occlusion (CRVO) can be detected early by iris angiography (IA) and neovascular glaucoma (NVG) was avoided with prompt ocular treatments after long-term follow-up.
NVG following CRVO is a serious complication and its management is difficult [1]. Although details for the mechanism of intraocular pressure (IOP) elevation are still unclear, the clinic consensus of early diagnosis and early treatment of anterior segment (iris or angle) neovascularization is crucial to prevent NVG. The management of retinal vein occlusion–consensus document (edition 2011) contains recommendations for the detection of anterior segment neovascularization which includes gonioscopy, slitlamp exam, visual acuity (VA) and determining the area of nonperfused retina using ocular fundus fluorescein angiography [2]. However, in darkly pigmented eyes, the stromal pigment blocks observation of iris vascular patterns and INV may be difficult to see by slitlamp observation, even if the degree of INV has progressed, making NVG inevitable. As for ectropion uveae at the pupillary margin, it is just an indirect index for progression to INV and NVG, and a real correlation between ectropion uveae and INV has not clear actually. A recent study in Japanese patients, reported that fluorescein angiography and indocyanine green angiography of the anterior ocular segment were useful for evaluating the effect of bevacizumab injection on obvious iris and angle neovascularization[3]. It reminded us if early hiding INV could be visualized with angiography in the presence of negative slitlamp ? To our knowledge, such a case has not been previously reported in the literature.
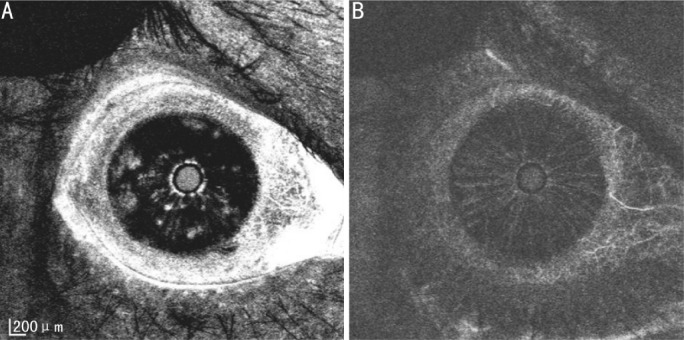
A 54-year-old Chinese man presented reporting, acute painless vision loss over a 20 day period. On presentation the findings included, total retinal venous engorgement, intensive intraretinal hemorrhages and OD intraretinal edema with best-corrected visual acuity (BCVA) of 1/20, and IOP of 14mmHg. In addition, a uveal ectropion at the pupil margin, there was no observation of anterior segment (iris or angle) neovascularization by gonioscopy and slitlamp examination (Figure 1). The patient had received 3 Fufangxueshuantong Capsules (a kind of Chinese patent medicine), orally tid for 20 days; however, he complained his eyesight did not improve.
Figure 1. Slit lamp observation.
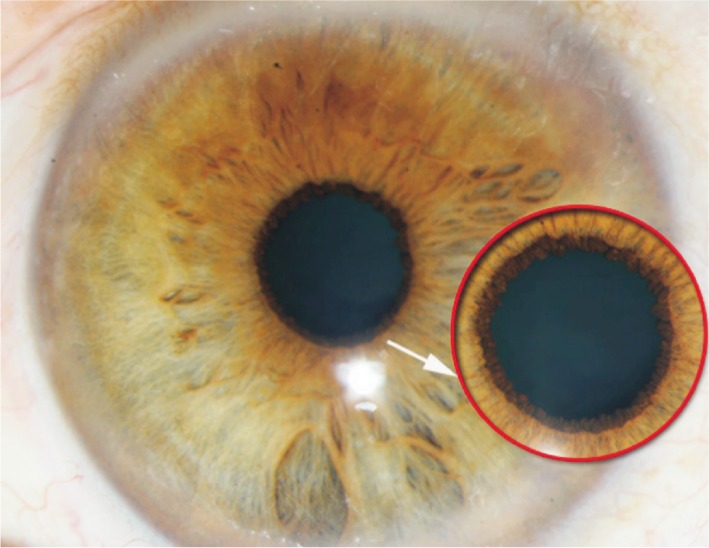
Arrow shows an ectropion uveae at pupillary margin but no any newly formed vessels are found at the pupillary margin and the surface of the iris.
The patient's left eye had no ocular disease and therefore served as a control eye. Both eyes underwent simultaneous IA with fluorescein and indocyanine green using a Heidelberg Retina Angiograph 2 (HRA-2). The patient had no reported drug allergies, and his blood pressure and pulse rate were all within normal reference ranges. Injection of metoclopramide hydrochloride, 10mg, through an intravenous catheter was followed by intravenous injection of a mixed solution of fluorescein (2.5mL) and indocyanine green (2.5mL) through the same route. The angiographic pictures were stored on a hard disc as digital images within the HRA-2.
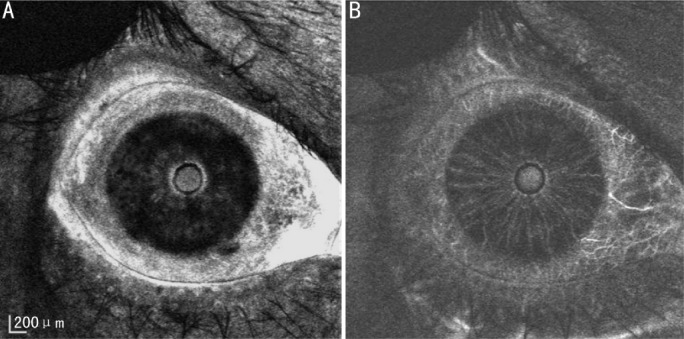
Iris vessels appeared with fluorescein and indocyanine green 20 seconds after the mixed dye injection. IA with indocyanine green showed clearer vessels and no dye leakage, whereas, IA with fluorescein showed fewer iris vessels which were mostly blocked with melanin pigment and intense vessel leakages at the pupillary margin and the surface of the right iris (Figure 2). There was no dye leakage from iris vessels in either FA or IA in the left control eye. IA findings supported the final diagnosis of ischemic CRVO combined with INV.
Figure 2. IA with fluorescein and indocyanine green at 29 seconds before PRP treatment.
IA with fluorescein shows remarkable leakage from the newly formed vessels at the pupillary margin and the surface of the iris (A), whereas IA with indocyanine green shows no any leakage from newly formed vessels and normal vessels (B).
The patient was started immediately on a treatment of panretinal photocoagulation (PRP) (n = 800 effects) and underwent a second iris angiography 8 weeks after treatment. Reexamination with IA showed that the dye leakage was dramatically decreased in the right iris (Figure 3). Coinstantaneous follow-up examination revealed BCVA improved to 5/20. IOP was 16mmHg. Finally, 12 months after the first visit BCVA of this patient was 6/20 in right eye and IOP was 14mmHg, which maintained at normal level all along; newly formed vessels in the iris never appeared on slit lamp examination.
Figure 3. IA with fluorescein and indocyanine green at 29 seconds after PRP treatment.
A: 6 weeks later, IA with fluorescein shows dye leakage from the NFVs decreased remarkably compared with the pre-treatment levels; B: IA with indocyanine green showed that there were no changes in the vascular structures on the iris.
Our results showed early INV could be seen with IA in the presence of negative slit lamp observations. Furthermore, simultaneous IA presented clear views of vessel shape in the black-brown iris of Chinese patients and the correlation between INV and ectropion uveae at the pupillary margin was established. PRP treatment markedly decreased fluorescein leakage and effectively reduced the INV, but the vascular structure with indocyanine green angiography did not change, which indicated PRP treatment reduced vascular permeability and the effect was proportional to the intravitreal injection of bevacizumab [3].
In conclusion, the use of angiography to detect anterior segment neovascularization should be considered as a routine diagnostic tool to avoid NVG and this technique may be recommended into the new therapy guideline for patients with CRVO.
REFERENCES
- 1.McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, Kowalski JW, Nguyen HP, Wong TY. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117(6):1094–1123e15. doi: 10.1016/j.ophtha.2010.01.060. [DOI] [PubMed] [Google Scholar]
- 2.Coscas G, Loewenstein A, Augustin A, Bandello F, Battaglia Parodi M, Lanzetta P, Monés J, de Smet M, Soubrane G, Staurenghi G. Management of retinal vein occlusion–consensus document. Ophthalmologica. 2011;226(1):4–28. doi: 10.1159/000327391. [DOI] [PubMed] [Google Scholar]
- 3.Ishibashi S, Tawara A, Sohma R, Kubota T, Toh N. Angiographic changes in iris and iridocorneal angle neovascularization after intravitreal bevacizumab injection. Arch Ophthalmol. 2010;128(12):1539–1545. doi: 10.1001/archophthalmol.2010.282. [DOI] [PubMed] [Google Scholar]