Abstract
Background
According to willingness of the Ministry of Health, Iran and presence of appropriate conditions for disease elimination, national malaria control program decided to conduct a research to clarify malaria status in 2007 and to provide required information to perform the elimination program. This review is comprised of the basis of national malaria elimination program in vision of 2025, which was started in 2010.
Methods:
In this descriptive study, data were analyzed by applications of different variables at district level. All districts in the three south eastern provinces, in which malaria has local transmission, were considered. Malaria cases has been determined and studied based on the national malaria surveillance system.
Results:
Since vivax malaria is predominant in Sistan & Baluchestan Province, number of vivax cases is equal to malaria positive cases approximately. The important point is that Nikshahr contains the maximum number of local vivax cases in this province and the maximum number of falciparum cases is reported from Sarbaz district. Among all districts of Hormozgan Province, no case of autochthonous falciparum was detected except in Bandar Jask and one case in Minab. There was no case of autochthonous falciparum in Kerman Province, except in Kahnoj and Ghale Ganj that each of them had one case in 2007.
Conclusion:
It appears that the report of locally transmitted cases in Iran is increasing over the past few years, before starting malaria elimination plan. Since the Afghan refugees started to return to their own country so the main source of reporting of imported malaria cases reduced and local cases would be demonstrated more clearly.
Keywords: Malaria, Autochthonous case, Epidemiology, Iran
Introduction
Malaria is one of the most serious hygienic concerns around the world. Annually, 0.6 to 1 million people of 196 to 297 million malaria infected population lose their lives, mostly children under five and pregnant women (1). In Eastern Mediterranean regions, over 10 million clinical malaria cases occur each year, of which 50 thousand lead to death. Totally, 287 million which is about 60% of Eastern Mediterranean population is at risk of malaria infection. Fifteen percent of this population lives in areas with P. vivax parasite transmission and 45% of lives in areas with simultaneous transmission of both P. vivax and P. falciparum parasites (2).
Iran with population of more than 72 million people is located in West Asia. It has approximately 1.648 million square km area of which mountainous regions and arid deserts comprise 50% and 25%, respectively.
The Malaria Control Program started extensively in 1951. By 1953, the program covered 5 million of the total population (18 million). The main duty of the program was DDT Indoor Residual Spraying and with massive use of DDT considerably decreased malaria infection rate in most endemic areas (3, 4). Based on Iranian’s estimations before the starting of the program, there was an infection rate of 4 million people per year. The involved areas were mainly of southern areas beside Persian Gulf, Azerbaijan and coastal areas of Caspian Sea. Subsequent malaria metric studies of Institute of Malariology demonstrated that the disease has dispersed in many villages all over the country (3,5).
The Health Cooperation Organization was established based on a contract that was signed on December 31, 1952 between Iranian Ministry of Health and Technical Cooperation of United States of America (USA). In early 1949, the health section of Budget and Planning Organization integrated malaria control program to the other development programs. In 1948 and 1949, following request of Iranian government, three officials of public health service attended in Iran for a period of two months for evaluating status of Malaria and proposing programs for controlling it. These programs included insecticide spraying, entomology survey and environment management. Malaria control program had the highest priority among all programs of Health Cooperation Organization (6, 7).
Initially, cooperation between Iran and USA in technical and public health fields was called the “June the Forth” Principle; afterwards, this name changed into Technical Cooperation with USA. The health section of the program was extracted from collaborative programs between USA and Latin American countries, known as Service Organization. The Health Cooperation Organization was active until 1964; from that time on, the name of the organization changed into Central Health Department and the American technical experts supported the program as consultant.
The Institute of Malariology was established by Faculty of Medicine, Tehran University and Iranian Ministry of Health with technical support of WHO and USA. Scientific data of malaria was constantly collected by the institute and employed in control programs. Furthermore, the institute was responsible for teaching malaria courses to executive managers involved on the control program. Nevertheless, years later, the institute started to work independently (8).
Subsequent to starting and actively performing malaria control programs, which in the first years was named “Malaria Eradication”, the disease was eliminated in most parts of the country. In such a way that, after 1972 the disease was under control in most parts of the country and local transmission were limited to some endemic parts. These areas were located mainly in Sistan & Baluchestan, Hormozgan and Kerman Provinces (9).
National program for malaria control in Ministry of Health and Medical Education has divided areas of infected regions into two categories. Category No.1: areas with malaria transmission at the moment and category No.2: areas in which malaria transmission existed in the past but now it does not exist due to prevention measures or socio-economic development.
According to willingness of Ministry of Health and presence of proper conditions for disease elimination, national malaria control program decided to conduct a research to clarify malaria status in 2007 and to provide required information to perform the elimination program. This review is comprised of the basics of national malaria elimination program in vision of 2025, which was started in 2010 (10).
Materials and Methods
A questionnaire was designed in seven titles in cooperation with peripheral staff and provincial authorities. The titles which set by national coordinator were: demographic information, diagnosis, the epidemiologic information, outbreak control, consistent with new definitions of WHO, information on the vectors. The questionnaire was completed with collaboration of peripheral levels in cooperation with malaria experts and technicians in 20 health centers of malarious provinces.
In this descriptive study, relying on raw data; data were analyzed by applications of different variables at district level. All districts in the three south eastern provinces, in which malaria has local transmission, were considered. Malaria cases has been determined and studied based on the national malaria surveillance system.
Malaria surveillance
It is noteworthy that all of diagnosis and treatment services are free of charge in Iran. District hospitals, urban/rural health centers and malaria passive laboratories posts are considered as malaria service providers. Malaria surveillance based on two main methods; passive and active case finding (Table 1).
Passive surveillance: In this method, the patient refers to the nearest health care center to take malaria blood slide. Main features of this method are full time coverage but its problem is deficient location coverage.
Active surveillance: This method of surveillance is divided into two subcategories; routine surveillance and case follow up.
Table 1:
Current malaria surveillance including passive and active case finding
| Passive surveillance | Active surveillance | ||
|---|---|---|---|
| Routine | Active foci (foci with positive report) | ||
| Target group (for detection of blood smear) | People with fever, recent Malaria cases (for follow up) | Suspected malaria cases, infected people in the interval between two case finding activities, foreign people (Afghani & Pakistani) | Persons who feel ill, infected in last month, persons with history of malaria, foreign people (Afghani & Pakistani) |
| Target regions | All over the country | Household in the villages, mobile villagers in local malaria region | Active foci, (in urban areas and villages have more than 50 households: around the reported cases. In villages less than 50 households: all the village |
| Service center | Malaria labs, Health House, hospitals | Health workers, Malaria mobile team | Health workers, Malaria mobile team |
| Remark | Active surveillance is usually done with interval of two weeks, unless during transmission season which will be done weekly. In areas with no malaria transmission it will be with monthly bases | First active case detection will be done within 24 hours of case detection and it will be continued for four consequent weeks | |
In this method, health staff (community health workers and malaria technicians) will screen villagers for malaria, case detection and treat them. The routine screening would be set at regular intervals contingent upon their distant and number. Active surveillance usually takes place on a semimonthly basis. It is expected to take place on a weekly basis during peak of transmission period and on a monthly basis during the rest of year. This method features full location coverage and deficient time coverage. The base of diagnosis and registering positive cases is microscopic diagnosis of parasite from suspected cases.
Results
Sistan & Baluchestan Province
Six southern districts, located in Sistan & Baluchestan, were studied. The demographics, epidemiological and important vectors information in these districts are provided briefly in the (Table 2).
Table 2:
The demographics, epidemiological and important vectors information in Sistan & Baluchestan Province
| Province name | District name | Total Population | Afghani & Pakistani Pop. (%) | City | village | Falciparum Foci | Vivax Foci | Villages having more than 5 cases of Vivax | Health house | Annual blood smear | Autochthones Case | Imported Case | Total Case | Primary Vectors* | Secondary Vectors* | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Urban | Rural | Active | Passive | Vivax | Fal + Mix | |||||||||||||
| Sistan & Baluchistan | Iranshahr | 275467 | 5 | 8 | 887 | 12 | 132 | 15 | 8 | 8 | 43438 | 5913 | 365 | 12 | 172 | 549 | 1 | 3,4 |
| Sarbaz | 607015 | 0.03 | 1 | 136 | 87 | 157 | 42 | 2 | 4 | 27580 | 3003 | 477 | 2 | 596 | 1075 | 2 | 4,5 | |
| Nikshahr | 190194 | 0.05 | 5 | 741 | 17 | 349 | 134 | 6 | 11 | 1E+05 | 14865 | 2499 | 10 | 188 | 2697 | 2 | 4,5 | |
| Konarak | 607015 | 0.03 | 1 | 136 | 10 | 32 | 28 | 2 | 4 | 27580 | 3003 | 477 | 2 | 137 | 616 | 1 | 2,4 | |
| Saravan | 252296 | 3.63 | 6 | 871 | 114 | 207 | 48 | 8 | 15 | 32865 | 11890 | 379 | 126 | 408 | 913 | 1 | 2,4 | |
| Chabahar | 198192 | 0.8 | 2 | 468 | 76 | 227 | 92 | 6 | 10 | 61035 | 10393 | 1074 | 119 | 699 | 1892 | 1 | 2,4 | |
1. Anopheles culicifacies; 2. An.stephensi; 3. An.pulcherrimu; 4. An.fluviatilis; 5. An.culicifacies
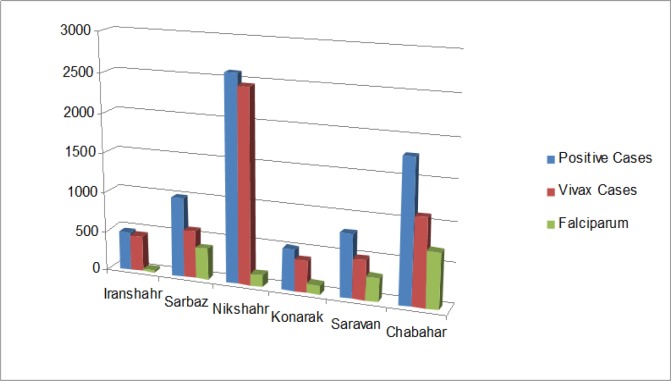
Since vivax malaria is predominant in Sistan & Baluchestan Province number of vivax cases is equal to malaria positive cases approximately. The important point is that Nikshahr contains the maximum number of local vivax cases in this province and the maximum number of falciparum cases reported from Sarbaz District which can be the result of common border with Pakistan and continuous cross border movement (Fig. 1).
Fig. 1:
The number of local malaria cases by parasite and district in Sistan & Baluchestan Province, 2007
Active surveillance has a large proportion of total surveillance in this province, in such way that 90% of malaria cases in Konarak, 88% in Nikshahr and Iranshahr, 85% in Chabahar and as the minimum 73% of malaria cases were detected through active surveillance in Sarbaz and Saravan Districts.
It appears that the prepared blood smears per population is very high in Nikshahr in compare to other districts. Since the rate of detected cases is not different to other districts it seems that the taken slides are not targeted precisely in Nikshahr. This district has higher incidence in Sistan-Baluchestan.
Hormozgan Province
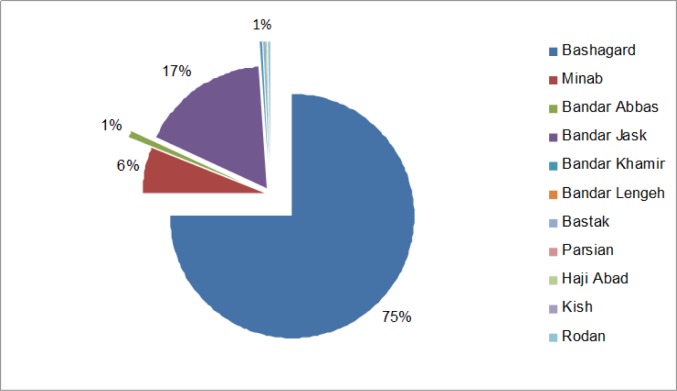
Eleven districts were studied in Hormozgan Province. The demographics, epidemiological information and information of important vectors in these districts are provided briefly in (Table 3). Among all districts of this province, no case of autochthonous falciparum was detected except in Bandar Jask and one case in Minab. There was no case of local transmission in Kish or Parsian districts. In this province, the maximum number of registered positive cases was respectively in Bashargad, Bandar Jask and Minab. Bashagard’s role in local transmission of malaria is 74%. Notably, there is no falciparum transmission report in Bashagard (Fig. 2). Active surveillance, in this province plays a more prominent role than passive surveillance, similar to Sistan & Baluchestan Province.
Table 3:
The demographics, epidemiological and important vectors information in Hormozgan Province
| Province name | District name | Total Population | Afghani & Pakistani Pop. (%) | City | village | Falciparum Foci | Vivax Foci | Villages having more than 5 cases of Vivax | Health house | Annual blood smear | Autochthones Case | Imported Case | Total Case | Primary Vectors* | Secondary Vectors* | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Urban | Rural | Active | Passive | Vivax | Fal + Mix | |||||||||||||
| Hormozgan | Bandar Abbas | 511445 | 2 | 2 | 284 | 1 | 2 | 4 | 8 | 17 | 13913 | 1536 | 38 | 26 | 54 | 118 | 1,2 | 3,4 |
| Bandar Jask | 47307 | 6 | 1 | 147 | 1 | 2 | 41 | 1 | 5 | 24351 | 2724 | 1062 | 46 | 37 | 1145 | 1,2 | 3,4 | |
| Bandar Khamir | 51519 | 2 | 1 | 45 | 0 | 2 | 0 | 1 | 4 | 72 | 1 | 1 | 0 | 0 | 1 | 7 | 7 | |
| Bandar Lengeh | 93590 | 2 | 5 | 129 | 1 | 2 | 0 | 4 | 9 | 3153 | 475 | 3 | 0 | 21 | 27 | 2 | 4 | |
| Bastak | 66211 | 7 | 1 | 92 | 0 | 4 | 0 | 1 | 15 | 920 | 1754 | 4 | 0 | 4 | 4 | 7 | 7 | |
| Parsian | 33789 | 5 | 1 | 48 | 0 | 0 | 0 | 1 | 4 | 3472 | 1428 | 2 | 0 | 11 | 13 | 7 | 7 | |
| Haji Abad | 68416 | 2 | 2 | 234 | 0 | 4 | 1 | 1 | 8 | 4595 | 396 | 85 | 0 | 4 | 89 | 2 | 4 | |
| Kish | 21000 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 10703 | 153 | 3 | 0 | 35 | 38 | 2 | 5 | ||
| Rudan | 112935 | 1 | 1 | 244 | 0 | 3 | 0 | 1 | 12 | 10860 | 532 | 6 | 0 | 3 | 9 | 2 | 6 | |
| Minab | 270581 | 6 | 2 | 360 | 0 | 180 | 10 | 3 | 13 | 33012 | 3898 | 322 | 1 | 43 | 366 | 2 | 6 | |
| Bashagard | 29917 | 1 | 0 | 196 | 131 | 0 | 2 | 1E+05 | 3600 | 4398 | 0 | 0 | 4398 | 2 | 6 | |||
1. An.culicifacies; 2. An.stephensi; 3. An. superpictus; 4. An. dthali; 5. An.sacharovi; 6. An.fluviatilis; 7. Not available
Fig. 2:
The number of local malaria cases by district in Hormozgan Province, 2007
In fact, the average share of active surveillance exceeds to 85%; even in some districts, it exceeds to 98%. However, an exception can be found such as Bastak, that its passive surveillance share is 65%. The important point is that the per capita rate of slide preparation is three-eighth in Bashagard. It means that, approximately, each resident of Bashagard suspect of malaria infection four times a year and the blood slide provides four times a year. Furthermore, there is one suspected case of malaria in any two people in Bandar Jask. The important point is SPR which is 3.87 in Bashagard, in other words among each 25 prepared slides one was showed a positive case.
The incidence in Bashagard is the highest among these districts, which has a meaningful difference with others; in fact, 147 people were malaria infected among one thousand at risk population. As Fig. 2 indicates, the incidence in Bandar Jask is 21.41 and in other districts the incidence is negligible, where in Kish and Parsian the incidence of locally transmitted case is zero.
Kerman Province
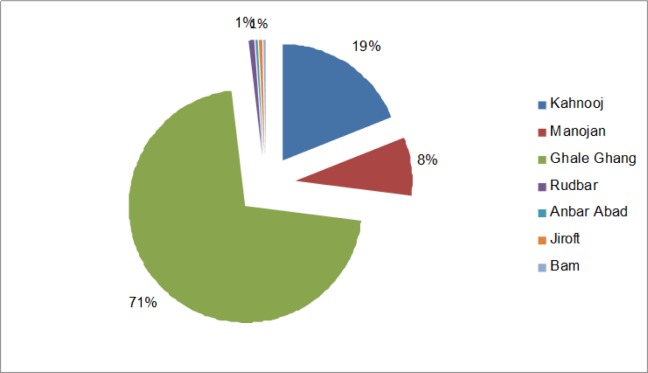
Six southern districts of Kerman Province were assessed in this study. The demographics, epidemiological information and information of important vectors are provided briefly in the (Table 4). There was no case of autochthonous falciparum in this province, except in Kahnoj and Ghale Ganj that each of them had one case in 2007. The highest number of locally transmitted vivax cases in Ghale Ganj, Kahnoj and Manojan were 108, 405 and 48 respectively; other districts rarely had cases of malaria. In Jiroft the locally transmitted cases of both parasite strains were nonexistent. Seventy percent of malaria cases took place in Ghale Ganj (Fig. 3).
Table 4:
The demographics, epidemiological and important vectors information in Kerman Province
| Province name | District name | Total Population | Afghani & Pakistani Pop. (%) | City | village | Falciparum Foci | Vivax Foci | Villages having more than 5 cases of Vivax | Health house | Annual blood smear | Autochthones Case | Imported Case | Total Case | Primary Vectors* | Secondary Vectors* | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Urban | Rural | Active | Passive | Vivax | Fal + Mix | |||||||||||||
| Kerman | Kahnoj | 94262 | 4 | 2 | 182 | 0 | 1 | 0 | 2 | 8 | 5423 | 1070 | 122 | 4 | 10 | 136 | 1,2 | 4,5,6 |
| Manojan | 65116 | 1.6 | 2 | 134 | 0 | 1 | 5 | 1 | 7 | 10581 | 1018 | 42 | 0 | 6 | 48 | 3 | 6 | |
| Ghale Ganj | 64818 | 3 | 1 | 193 | 0 | 5 | 16 | 2 | 5 | 23449 | 2476 | 362 | 1 | 24 | 387 | 3 | 1,6 | |
| Rudbar | 83579 | 1 | 1 | 250 | 0 | 1 | 0 | 1 | 7 | 2637 | 76 | 2 | 0 | 9 | 11 | 3 | 4,6 | |
| Anbar Abad | 86846 | 1.1 | 2 | 428 | 0 | 1 | 2 | 2 | 8 | 1230 | 360 | 8 | 0 | 18 | 26 | 3,4 | 6 | |
| Jiroft | 168815 | 1.7 | 3 | 123 | 0 | 1 | 1 | 5 | 11 | 923 | 505 | 24 | 0 | 15 | 39 | 3,4 | 5,6 | |
| Bam | 243555 | 1 | 4 | 894 | 0 | 0 | 0 | 10 | 19 | 14625 | 586 | 8 | 0 | 19 | 27 | 3 | 6 | |
1. An.culicifacies; 2. An.fluviatilis; 3. An.stephensi; 4. An. dthali; 5. An. Superpictus; 6. An.fluviatilis
Fig. 3:
The number of local malaria cases by district in Kerman Province, 2007
Active surveillance has a more prominent role than passive surveillance in this province. In fact, the average share of active surveillance exceeds 90%. Additionally, in some districts it reaches over 96%. Certainly, Bam has less malaria cases in compare to other districts, having 96% active surveillance and considering its high sensitive active surveillance system. In Ghale Ganj, slides have been prepared among 40% of the total malaria suspected population, which its SPR was 1.56. In Manoujan slides have been prepared among 18% of the total malaria suspected population, with SPR of 0.41. In Kahnoj slides have been prepared among 6.89% of the total malaria suspected population, with SPR of 1.66. On the other hand, in Kahnoj ABER is less in comparison with two previous districts but its SPR is higher. It shows that the case finding is more targeted in Kahnoj.
The incidence in Ghale Ganj was the highest and it has a meaningful difference with other districts. In each 1000 thousand population, 6.25 were infected by malaria. The incidence of Jiroft, Anbar Abad and Bam is approximately zero.
Discussion
Bashagard took the first place in all three provinces, having the highest ABER of 380%. In other words; any person is a malaria suspect three-eight times in a year. This can indicate either high sensitivity in surveillance system. The second one can raise hope for discovering and reporting all malaria cases. Nikshahr, Konarak and Jask took the next places having a meaningful difference with Bashagard. It can be inferred that there is a direct relationship between their SPR and their difference with Bashagard. The SPR in Bandar Jask does not have a meaningful difference to Bashagard, although its ABER is one seventh of Bashagard.
Bashagard with SPR of 3.87% and Bandar Jask with SPR of 3.74% were the highest infected districts in 2007, and the two of them have a significant difference with other districts in south-east of the country. The next place of SPR belongs to Nikshahr with SPR of 1.92%. The other districts like Sarbaz, Chabahar, Haji Abad, Kahnoj, Ghale Ganj and Konarak have close range of SPR. Kish, Parsian and Jiroft have the SPR of close to the 0%, which means they do not have any reported or registered locally made cases. The SPR of other districts are approximately1%.
In studied districts, the incidence trend also follows SPR and ABER. Bashagard has the highest local case, having the incidence of 147 per 1000. Bandar Jask took second place with a significant difference to Bashagard, having 21 per 1000 incidence. Nikshahr, Konarak and Manojan took the next places.
Bashagard, Nikshahr, Bandar Jask, Ghale Ganj and Minab have the maximum number of locally made vivax among all the districts. Sarbaz, Saravan and Chabahar in Sistan & Baluchestan and Bandar Jask in Hormozgan had locally transmitted cases of falciparum. In all other districts locally made cases of falciparum was nonexistent except for Minab, Kahnoj and Ghale Ganj, which only had one cases of locally transmitted falciparum in 2007. Notably, in districts, which ranked among the highest places of vivax cases (such as Bashagard, Nikshahr and Bandar Jask) there is no reports of local falciparum case.
It appears that the report of locally transmitted cases in Iran is increasing over the past few years. Since the Afghan refugees started to return to their own country so the main source of reporting of imported malaria cases reduced and local cases would be demonstrated more clearly (11).
The new approach to combat malaria in Iran is elimination which simply aimed to reduce local cases with final goal of zero local case of malaria. National strategic plan for malaria elimination includes three main technical and four supportive strategies as follows (10):
Main strategies:
○ Promoting access to malaria treatment and diagnosis
○ Promoting access to preventive services by improving IVM
○ Strengthening Malaria Surveillance System
Supportive strategies:
○ Developing and strengthening the monitoring and evaluation system of malaria elimination interventions system
○ Strengthening malaria applied researches
○ Using all stakeholders potentials for eliminating malaria
○ Capacity building of human resources and using all resources for eliminating malaria
Reaching a complete elimination is a difficult task to achieve, due to existence of favorable conditions for disease transmission and dysfunctional status of eastern neighboring countries. There is a demand for controlling measures in cooperation with Afghanistan and Pakistan and conducting joint research. Knowing the fact that malaria is associated with poverty, malaria control demands determination of health system officials and special attention from other organizations involved in reconstructions such as improving electricity supply, constructing and improving roads and special concentration on general aspects of socio-economic development in deprived southeastern provinces.
Conclusion
According to this study it seems that the surveillance of malaria control program is strong enough at all levels and malaria elimination is possible in the country. This will be more feasible especially in the context of plasmodium falciparum.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
While conducting this program and collecting information from the peripheral, many of our colleagues including urban and rural health care personnel, malaria experts of district health care centers in malarious provinces in three provinces went through so many troubles along with their precision and honesty, thankfully appreciate each one of them. The authors declare that there is no conflict of interest.
References
- 1.World Health Organization. World Malaria Report. 1st ed. World Health Organization; Switzerland: 2009. Chapter 3. [Google Scholar]
- 2.World Health Organization. Strategic plan for malaria control and elimination in the WHO Eastern Mediterranean Region 2006–2010. 1st ed. World Health Organization; 2007. Regional Office for the Eastern Mediterranean, Cairo, Chapter 2. [Google Scholar]
- 3.Palmquist EE, Aldridge FF. Malaria in Iran. Public Health Rep. 1954;69(10):976–81. [PMC free article] [PubMed] [Google Scholar]
- 4.Palmquist EE, Aldridge FF. Iran’s public health cooperative organization. Public Health Rep. 1954;69(10):970–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Edrisian GHH. Malaria in Iran: Past and Present Situation. Iranian J Parasitol. 2006;1(1):1–14. [Google Scholar]
- 6.Faghih MA. Malarialogy and Malaria Eradication. Tehran University press; 1969. [Google Scholar]
- 7.Ministry of Health and Medical Education. 1961. Annual report of CDC, I.R. Iran.
- 8.Moulding T, Rosa F. The doctor in international health-United States sponsored program in Iran. A J Public Health Nations Health. 1960;50(5):696–708. doi: 10.2105/ajph.50.5.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edrisian GHH. Malaria history and status in Iran. Journal of School of Public Health and Institute of Public Health Research. 2002;1(1):50–61. [Google Scholar]
- 10.Ministry of Health and Medical Education. Malaria elimination plan in I.R. Iran (2026 vision) 2009 Islamic Republic of Iran. [Google Scholar]
- 11.Raeisi A, Nikpoor F, Ranjbar Kahkha M, Faraji L. The trend of Malaria in I.R. Iran from 2002 to 2007. Hakim. 2009;12(1):35–41. [Google Scholar]