Abstract
Hedgehog signaling pathway plays a critical role in the initiation and development of pancreatic ductal adenocarcinoma (PDA) and represents an attractive target for PDA treatment. Lithium, a clinical mood stabilizer for mental disorders, potently inhibits the activity of glycogen synthase kinase 3β (GSK3β) that promotes the ubiquitin-dependent proteasome degradation of GLI1, an important downstream component of hedgehog signaling. Herein, we report that lithium inhibits cell proliferation, blocks G1/S cell-cycle progression, induces cell apoptosis and suppresses tumorigenic potential of PDA cells through down-regulation of the expression and activity of GLI1. Moreover, lithium synergistically enhances the anti-cancer effect of gemcitabine. These findings further our knowledge of mechanisms of action for lithium and provide a potentially new therapeutic strategy for PDA through targeting GLI1.
Introduction
Pancreatic ductal adenocarcinoma (PDA), characterized by extreme aggressiveness, poor prognosis and high lethality, stands as the fourth leading cause of cancer-related death in the United States and shows little improvement in survival over the past 30 years [1]. PDA is reflective to current chemotherapeutic treatments as agents effective for other cancer types offer very limited survival benefit for PDA patients [2], [3], [4], [5], [6]. Surgical resection and gemcitabine chemotherapy are the main clinical treatment options for PDA patients based on the stage of diagnosis. Five-year relative survival rate for ∼20% of the PDA patients feasible for surgical resection is less than 20%, while the five-year relative survival rate of all stages patients is less than 6% [1], [7]. Therefore, a better understanding of PDA pathophysiology and the development of novel therapeutic options are urgently needed.
Hedgehog signaling pathway (Hh pathway), initially discovered in Drosophila to be important for the development of fruit fly body fragmentation, is a key regulator of animal development [8], [9]. This pathway in human starts with an intercellular ligand, hedgehog (HH) molecule, from autocrine and paracrine secretion. In the absence of HH ligand, a membrane receptor protein called patched (PTCH) represses the activity of another transmembrane receptor smoothened (SMO). Binding of HH ligand to PTCH releases the repression of SMO by the PTCH, and transduces the extracellular signal by activating downstream GLI zinc finger transcription factors 1 (GLI1), a hallmark of the activation of Hh pathway [10], [11].
Abnormal activation of the Hh pathway promotes the growth, proliferation, migration, invasion, angiogenesis and tumorigenic potential of cancer cells, and has been implicated in many human cancers [12], [13]. In pancreatic cancer patients, dysregulation of Hh pathway is not only present in PDA, but also in its precursor, pancreatic intraepithelial neoplasia (PanIN), suggesting that this pathway is an important early and late mediator of pancreatic cancer tumorigenesis [14]. Moreover, abnormal activation of the Hh pathway can be enhanced and sustained by mutations in key components of the canonical Hh pathway or by abnormal HH ligand in tumor microenvironment, as well as from noncanonical “cross talking” between Hh pathway and other pathways, such as the RAS/RAF/MEK/ERK pathway [15], [16]. Aberrant Hh pathway plays critical roles in the occurrence and development of epithelial mesenchymal transition (EMT) [17], oncogenic transformation and angiogenesis [18] in PDA. While suppression of Hh pathway by SMO inhibitors such as cyclopamine has been used as a therapeutic strategy for cancer, a significant fraction of GLI1 activation in PDA is driven by a SMO-independent mechanism [19], suggesting that direct inhibition of GLI1 protein may be a more effective route to suppress Hh pathway activation [20], [21] in PDA.
Lithium ions, a classical mood stabilizer, have been used in the clinical treatment of bipolar disorder and other mental disorders for more than half a century [22]. Lithium acts on a panel of molecular targets, majority of which are metal-dependent enzymes, such as glycogen synthase kinase 3 (GSK3α and GSK3β) [23], [24], [25], protein kinase B (PKB) [25], inositol monophosphatase (IMPase) [26], phosphoglucomutase [26] and bisphosphate 3′-nucleotidase (BPNT1) [27], presumably via direct competition with Mg2+ [28]. Although lithium is mainly used to treat mental disorders, it targets not only the nerve cells. Several reports have shown that lithium salts are effective for inhibiting glioma cell [29], colorectal cancer cell [30], medulloblastoma cell [31], hepatocellular carcinoma cell [32] and other cancer cells [33]. In fact, it has been suggested that lower cancer prevalence observed in mental patients is likely due to benefit from protection of lithium treatment [34]. At the molecular level, lithium has been shown to inhibit the growth and/or tumorigenicity of cancer cells by modulating the biologic activities of many cancer related genes, for example, STAT3 [35], β-catenin/WNT [30], [31], TNF [33] and FASL [36], and P53 [37].
In this study, we report that lithium inhibits cell proliferation and tumorigenic potential of PDA cells in vitro through suppressing the stability of GLI1 protein. Moreover, lithium synergizes the efficacy of gemcitabine on PDA. These novel findings expand our knowledge of lithium’s biological functions and provide a new therapeutic potential of lithium for the treatment of PDA.
Results
Lithium Inhibited Cell Proliferation and Impaired Tumorigenic Potential of PDA Cells
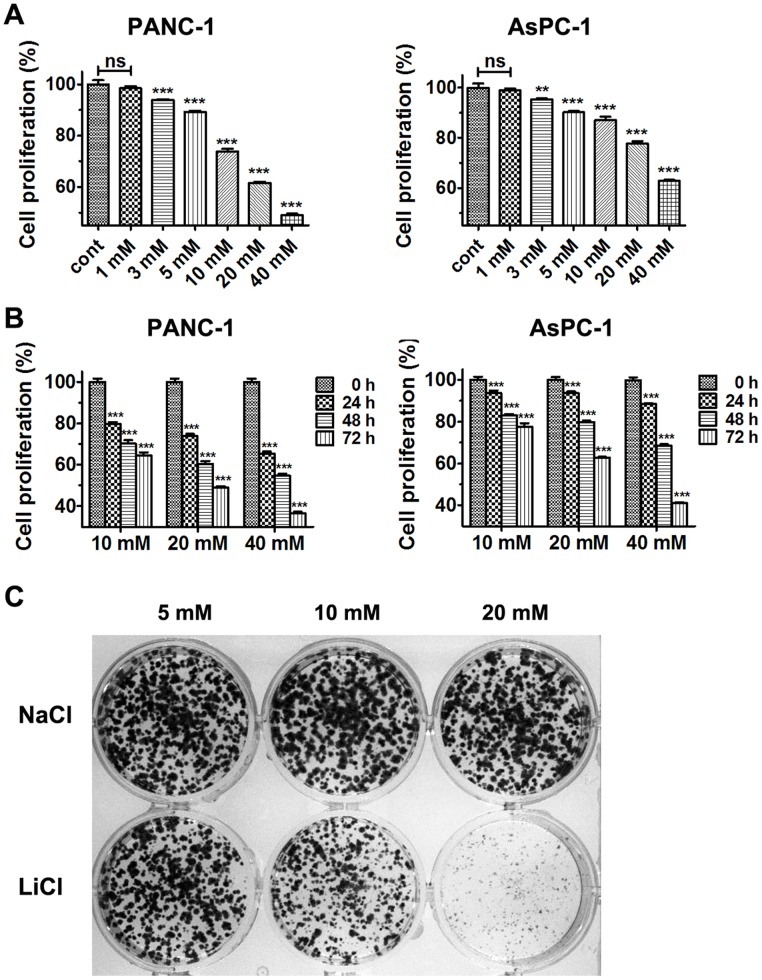
To investigate the effect of lithium on PDA cell proliferation, PANC-1 and AsPC-1 cells were treated with different doses of lithium chloride for one to three days and cells viabilities were determined. As shown in Figure 1A & B , treatment with lithium chloride, but not sodium chloride, markedly inhibited the proliferation of PANC-1 and AsPC-1 cells in a dose- and time-dependent manner. To further test if lithium treatment inhibits the tumorigenic potential of PDA cells, we performed colony formation assay, which is a test for oncogenic transformation in vitro. We observed that cell colonies were fewer and smaller for PANC-1 treated with lithium chloride than those from the control group with identical sodium chloride concentration in a doses-dependent manner ( Fig. 1C ).
Figure 1. Lithium chloride suppresses the proliferation of PDA cells and impairs tumorigenic potential of PANC-1 cell.
(A) Cell proliferation of PANC-1 cells and AsPC-1 cells after treatment with various concentrations of LiCl for 48 h. (B) Cell proliferation of PANC-1 cells and AsPC-1 cells after treatment with various concentrations of LiCl for indicated times. Data (Mean ± SEM) were representative of three independent experiments in triplicate. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001. (C) Tumorigenic potential of PANC-1 cells as monitored by colony formation after treatment with various concentrations of LiCl.
Lithium Induced Apoptosis and Cell Cycle Arrest of PDA Cells
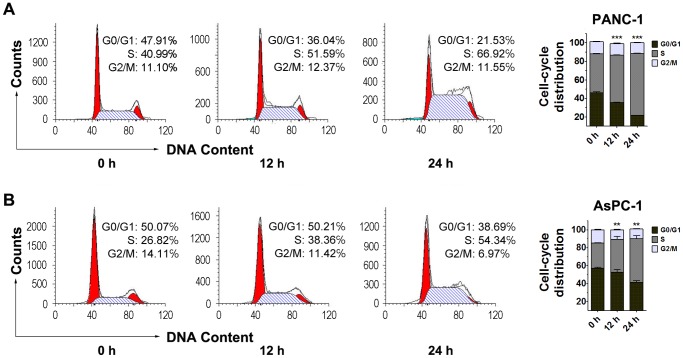
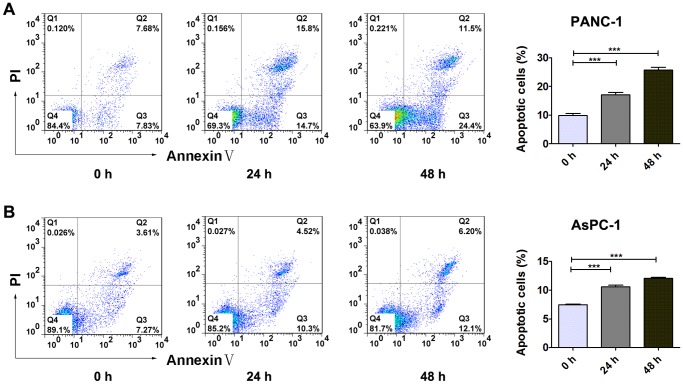
To test the effects of lithium on cell cycle progression and survival of PDA cells, we performed flow cytometric analyses of PANC-1 and AsPC-1 cells after 12 hours and 24 hours treatment with 20 mM lithium chloride. As shown in Figure 2 , lithium chloride treatment led to a significant increase in S-phase cell population and a decrease in population of G0/G1 phase in a time-dependent manner. Similarly, the percentage of apoptotic PDA cells was increased by lithium chloride treatment in a time-dependent manner ( Fig. 3 ). These data suggested that growth inhibition of PDA cells by lithium was at least partly due to S-phase cell cycle arrest and apoptosis.
Figure 2. Lithium chloride induces cell cycle arrest in PANC-1 cells and AsPC-1 cells.
PANC-1 cells (A) and AsPC-1 cells (B) were treated with 20 mM LiCl and analyzed by flow cytometry with PI staining. Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001.
Figure 3. Lithium chloride induces apoptosis of PANC-1 cells and AsPC-1 cells.
PANC-1 cells (A) and AsPC-1 cells (B) were treated with 20 mM LiCl and analyzed by flow cytometry with Annexin V-FITC/PI staining. Viable cells are Annexin V-FITC and PI negative (quadrant Q4), while apoptotic cells are Annexin V-FITC positive and PI negative (quadrant Q3); necrotic cells are Annexin V-FITC and PI positive (quadrant Q2), and damaged cells are Annexin V-FITC negative and PI positive (quadrant Q1). Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001.
Lithium Repressed Hedgehog Signaling Activity
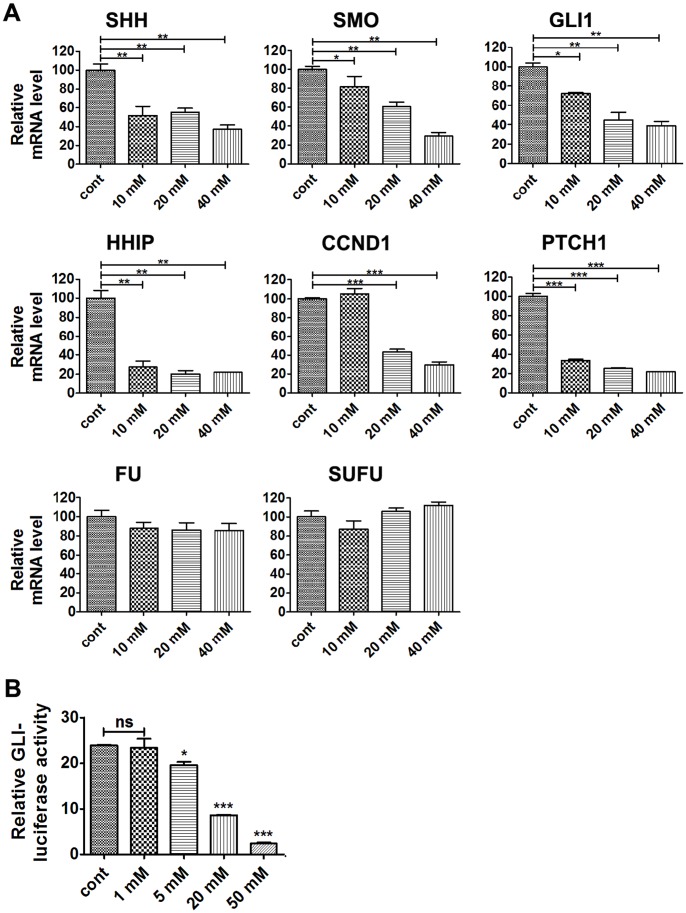
Abnormal Hh pathway plays an important role in PDA initiation and development. To determine whether lithium suppresses PDA cell proliferation through modulating the activity of Hh pathway, PANC-1 cells were treated with different concentrations of lithium chloride (10 mM, 20 mM, 40 mM) for 24 hours, and real-time PCR was carried out to monitor the expression levels of SHH, PTCH1, SMO, FU, SUFU, GLI1 and Hh pathway target gene HHIP and CCND1. As shown in Figure 4A , the mRNA levels of HHIP, CCND1 and PTCH1 were markedly decreased, suggesting that the activity of Hh pathway was downregulated. This is consistent with the fact that the expression of SHH, SMO and GLI1, the positive regulators of Hh pathway, were also significantly reduced. On the other hand, the expression of FU and SUFU were not significantly influenced by lithium treatment. To determine if lithium was capable of repressing Hh pathway directly, GLI-mediated luciferase activity was monitored, and the results showed that GLI-luciferase activities decreased in response to lithium treatment in a doses-dependent manner in AsPC-1 cells ( Fig. 4B ).
Figure 4. Lithium chloride represses Hh signaling activity.
(A) Real-time PCR analysis of mRNA expression levels of components of the Hh signaling pathway in PANC-1 cells treated with different concentrations of LiCl for 24 h. Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001. (B) GLI-luciferase activities in AsPC-1 cells transfected with GLI-luciferase reporter and treated with different concentrations of LiCl for 18 h. Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001.
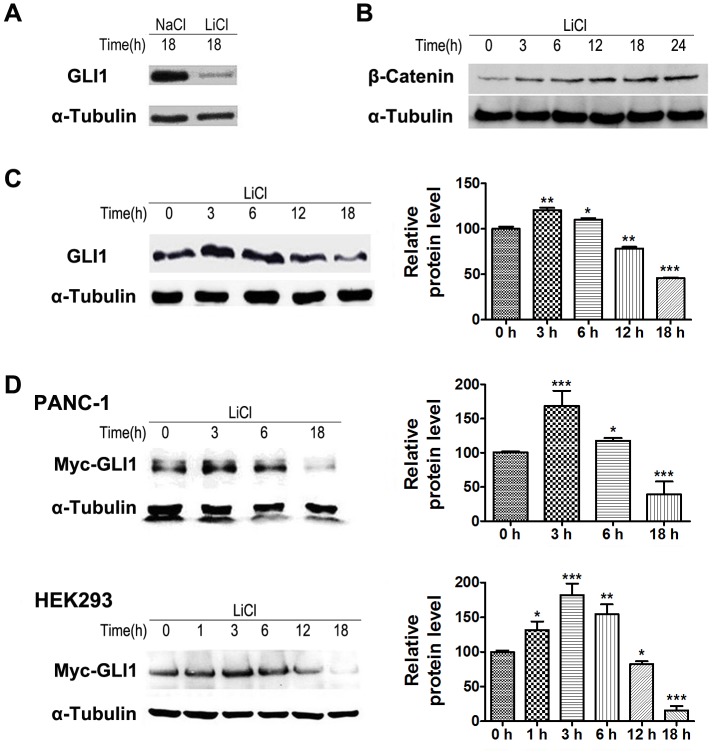
Lithium Modulated the Cellular Protein Levels of GLI1
To determine if lithium suppressed Hh pathway through modulating the cellular expression of GLI1, endogenous GLI1 proteins in PANC-1 cell were monitored using anti-GLI1 antibody. Immunoblotting analysis showed that endogenous GLI1 level was decreased in PANC-1 cell after 18 hours of treatment with 20 mM lithium chloride ( Figure 5A ). Since lithium is an inhibitor of glycogen synthase kinase 3 beta (GSK3β) that is known to suppressed Hh pathway by promoting ubiquitin/proteasome-dependent degradation of GLI1, our results were quite unexpected as logically lithium should up-regulate GLI1 expression by inhibiting GSK3β. Hence, we followed the time-dependent dynamic expression of GLI1 and β-catenin in response to lithium treatment. While the level of β-catenin was increased persistently as expected ( Fig. 5B ), the endogenous GLI1 protein levels showed a biphasic expression pattern. They were up-regulated initially at 3 and 6 hours but down-regulated subsequently in PANC-1 cell ( Fig. 5C ). To further confirm the dynamic effects of lithium on modulating cellular levels of GLI1, we ectopically expressed the full-length GLI1 tagged with a C-terminal Myc epitope in PANC-1 and HEK293 cells. These cells were incubated with 20 mM lithium chloride 48 hours post-transfection, and the expression level of GLI1-Myc was monitored using anti-Myc-Tag antibody. As shown in Figure 5D , the expression of GLI1-Myc protein in both of PANC-1 and HEK293 cells followed a similar biphasic pattern as the endogenous GLI1. Taken together, our results suggest that lithium treatment promotes the degradation of GLI1 protein, consequently leads to the inactivation of Hh pathway in PDA cells.
Figure 5. Lithium chloride regulates cellular levels of GLI1.
(A) Levels of GLI1 protein in PANC-1 cell treated with 20 mM LiCl or 20 mM NaCl for 18 h. (B) Time-dependent accumulation of β-Catenin protein level in PANC-1 cell treated with 20 mM LiCl. (C) Time-dependent change of GLI1 protein level in PANC-1 cell treated with 20 mM LiCl. (D) Time-dependent change of Myc-GLI1 expression in PANC-1 cells and HEK293 cells treated with 20 mM LiCl. These cells were treated with LiCl for indicated time. Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001.
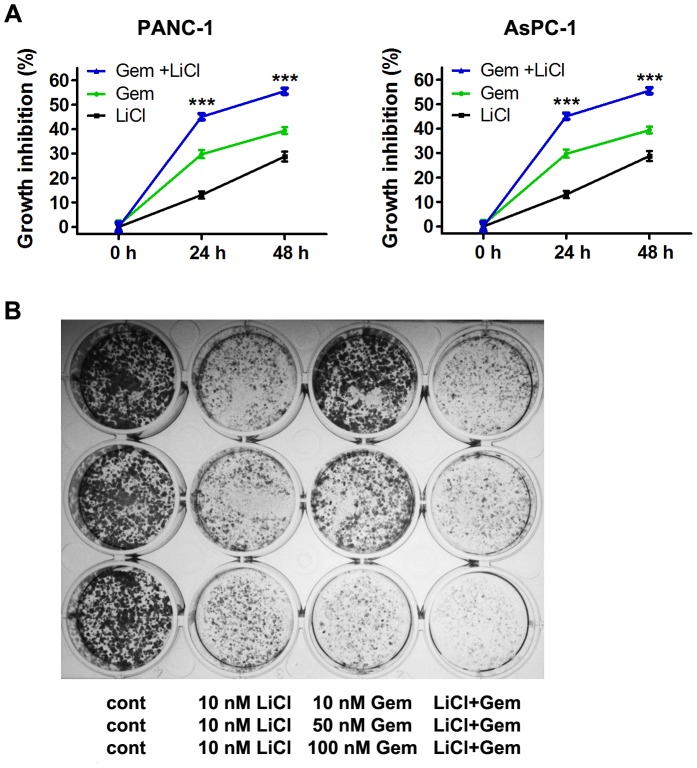
Lithium Synergized with Gemcitabine’s Suppressive Effects on Cell Viability and Tumorigenic Potential of PDA Cells
To determine if lithium-mediated Hh pathway suppression can synergize with gemcitabine to inhibit PDA cell proliferation, we followed cell viabilities of PANC-1 and AsPC-1 cells after treatment with lithium chloride (20 mM), gemcitabine (200 nM) or lithium chloride plus gemcitabine. The cell viabilities of both cell lines were significantly reduced by the combination treatment as compared to those of single agent treatment ( Fig. 6A ). Furthermore, the effect of lithium and gemcitabine combination on the tumorigenic potential of PANC-1 cell was investigated by colony formation assay. While gemcitabine dose-dependently suppressed the number and size of PANC-1 colonies, lithium significantly enhanced inhibitory effect of gemcitabine ( Fig. 6B ). These data suggest that lithium synergizes with gemcitabine’s suppressive effects on cell viability and tumorigenic potential of PDA cells.
Figure 6. Lithium chloride synergizes with gemcitabine in reducing cell viability and tumorigenic potential of PDA cells.
(A) Growth inhibition of PANC-1 and AsPC-1 cells after treatment with 20 mM LiCl, 200 nM gemcitabine and combination of LiCl and gemcitabine. Data (Mean ± SEM) were representative of three independent experiments. P values are indicated by asterisks (relative to control): *P<0.05, **P<0.01, ***P<0.001. (B) Tumorigenic potential of PANC-1 cells as monitored by colony formation after treatment with LiCl, gemcitabine and combination of LiCl and gemcitabine.
Discussion
The development of PDA is associated with the accumulation of genetic mutations and abnormal signaling pathways, including the KRAS, JAK/STAT, EGF, TGF-β/SMAD and Hh pathway [38], [39], [40]. Hh pathway inhibition has been proven to be an effective anti-cancer therapeutic strategy, and several antagonists targeting SMO have been developed and show efficacy in preclinical studies and clinical trials in humans [41], [42], [43], [44]. Recent studies demonstrate that it is sufficient to inhibit the growth of PDA through blocking GLI1 activity with RNAi technology or medicinal compounds [19], [45]. GLI1, can be phosphorylated by cAMP-dependent protein kinase (PKA), casein kinase I (CKI) and GSK3β, which in turn results in β-TRCP-mediated protein degradation by the ubiquitin-proteasome system [46], [47], which provides us a direction by targeting GLI1 on PDA therapy. GSK3β is a proline-directed serine-threonine kinase, involved in many cellular processes, such as metabolism, neuronal development, and body pattern formation [48], and GSK3β signaling has also been implicated in mental illness and tumor formation. Lithium, an effective GSK3β inhibitor, has been used in treating depression and bipolar disorder for many years [22]. Recently, it has been shown that inhibition of GSK3β promotes apoptosis in glioma cells and PDA cells [49], [50], and sensitizes PANC-1 cells to gemcitabine [51]. In addition, lithium induces apoptosis of a variety of cancer cells [36], [52]. At present, the mechanism of lithium-mediated anti-cancer activity is not clear.
In this study, we investigated the effect of lithium on Hh pathway in PDA cells. To our surprise, our results showed that the expression and activity of GLI1 in PDA cells were significantly down-regulated after treatment with lithium for 18 hours. Since GSK3β is known to promote ubiquitin-proteasome mediated GLI degradation, one would expect that inhibition of GSK3β by lithium should up-regulate cellular GLI levels. A more careful analysis revealed a biphasic regulation in which GLI1 protein levels were indeed increased initially following lithium treatment up to 6 hours. On the basis of these observations, coupled with the fact that in addition to directly phosphorylate GLI1, GSK3β is also known to control protein translation through direct suppression of EIF2β [53] and indirect suppression of MTOR [54], we deduce that the inhibition of GSK3β by lithium increases GLI1 cellular levels initially via blocking ubiquitin-proteasome mediated GLI degradation and releasing the inhibition of protein synthesis. At present, the long-term inhibitory effect of lithium on GLI1 is not clear. While we could not completely rule out the possibility that lithium-induced reduction of GLI1 over longer time course may be an indirect consequence of SHH and SMO downregulation ( Fig. 4A ). However, this scenario is most unlikely based on existing literature. Nolan-Stevaux and colleagues report that multistage development of PDA tumors is not affected by the deletion of Smo in the pancreas, suggesting a Smo-independent mechanism in which autocrine Shh–Ptch–Smo signaling is not required in pancreatic ductal cells for PDA progression [19]. This finding, coupled with the fact that more than 50% of PDA cells lines with sustained Hh signaling activity are resistant to SMO antagonist cyclopamine [14], implicates alternative means of GLI regulation by KRAS and TGF-β in PDA [15], [19]. Nevertheless, parallel observation of dual regulation involving GSK3β inhibition has been reported. Sun et al. show that 24-hour lithium treatment blocks prostate cancer cells at the S phase while lithium treatment for 6 hours promotes cells to pass through S phase [55]. Since GSK3β also promotes the degradation of E2F target gene cyclin E (CCNE) [56], it is most likely that CCNE may be also transiently increased at the beginning of lithium treatment, which facilitates the G1/S transition. On the other hand, it has been shown that long-term GSK3β inhibition by GSK3β specific inhibitor TDZD-8, lithium, or GSK3β siRNA disrupts the E2F-DNA interaction and suppresses the expression of E2F target genes CDC6, cyclin A (CCNA), CCNE and CDC25C [55]. Down-regulation of these DNA-replication related gene leads to G1/S arrest as reported and also shown in our study. Since E2F is a known target gene of GLI [57], the reported effects of lithium on E2F suppression and the cell cycle may depend on down-regulation of GLI1. We are currently actively testing this hypothesis.
In summary, we show for the first time that lithium inhibits Hh pathway through down-regulation of cellular GLI1 such that it blocks cell proliferation, induces cell-cycle arrest, promotes apoptosis and reduces tumorigenic potential of PDA cells. Moreover, lithium synergistically enhances the anti-cancer effect of gemcitabine. These novel findings extend our knowledge of mechanisms of action for lithium and provide a potentially new therapeutic strategy for PDA.
Materials and Methods
Cell Culture and Transfection
PDA cell lines PANC-1 and AsPC-1, and HEK293 were obtained from the Cell Bank of Type Culture Collection of Chinese Academy of Science (Shanghai, China). PANC-1 and HEK293 cell lines were cultured in DMEM and AsPC-1 cell line was in RPMI-1640 medium (Gibco/BRL) supplemented with 10% fetal calf serum (PAA, Austria) at 37°C under 5% humidified CO2. Transfection was performed using Lipofectamine 2000 reagent (Invitrogen) according to the manufacturer’s instructions.
Cell Viability Analysis
Growth-phase PDA cells were seeded in 96-well plates at a density of 4×103 cells/well (PANC-1) or 1×104 cells/well (AsPC-1), respectively. The cells were treated with various concentration of LiCl (Calbiochem) and gemcitabine (Tocris) the next day for 0–3 days and six replications were performed for each treatment. Ten microliters of Cell Counting Kit-8 (CCK-8) solution (Dojindo Laboratories) were added to each well and incubated at 37°C for 2–6 hours. The absorbance of each well at 450 nm was determined using a plate reader and the growth curves were then plotted accordingly. Each experiment was performed independently three times.
Colony Formation Assay
Single cell suspension of growth-phase PANC-1 cell was seeded in 6-well plates (1×103 cells/well) or 12-well plates (5×102 cells/well). After 24 hours incubation, cells were treated with various concentrations of LiCl and gemcitabine. Fresh medium with corresponding concentration of LiCl and gemcitabine were added every 5 days to replace the old medium. Two weeks later, the medium was aspirated off and the cells colonies were washed with PBS twice, then fixed for 15 minutes with methanol and stained with crystal violet (0.1% crystal violet in 20% methanol), and visualized using a microscope.
Apoptosis and Cell Cycle Analyses
PANC-1 and AsPC-1 cells were distributed into 12-well plates at a density of 2×105 cells/well, incubated with 20 mM LiCl. At the indicated time, cells were trypsinized and harvested by centrifugation, washed once with a buffer containing 10 mM Hepes, 140 mM NaCl, 2.5 mM CaCl2 and stained with Annexin V-FITC and propidium iodide (PI) in the dark at room temperature for 15 minutes, then analyzed using by flow cytometry (FACScan; Becton-Dickinson). Data were analyzed using the FlowJo software. For cell cycle analysis, the DNA contents of cells stained with PI and determined by flow cytometry. Data were analyzed using the ModFit software package. Each experiment was performed independently at least three times.
Immunoblotting Analysis
Cells were seeded in 6-well plates (5×105 cells/well) and treated with LiCl the next day. At the indicated time, lysis buffer containing 62.5 mM Tris pH 6.8, 2% sodium dodecylsulfate, 10% Glycerol, 0.01% bromophenol blue (300 µl/well) was used to harvest cellular proteins. The protein samples from lysates with 2% β-mercaptoethanol added were separated using 8% sodium dodecylsulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore). After being blocked with 5% non-fat dry milk in TBST (Tris buffered saline buffer containing 0.1% Tween-20) at room temperature for 1 hour, the PVDF membranes were incubated with individual primary antibodies (anti-Myc-Tag, anti-GLI1, Cell Signaling Technology; anti-α-Tubulin, Sigma; anti-β-catenin, Santa Cruz) at 4°C overnight, followed by corresponding HRP-conjugated secondary antibody at room temperature for 45 minutes. Protein bands were detected by ECL Western Blotting Detection System (Millipore). Each experiment was performed independently at least three times.
Real-time PCR Assay
Total RNA was extracted from PANC-1 cell treated with LiCl at different concentrations using TRIzol reagent (Invitrogen). cDNA was synthesized using the TaKaRa RNAiso Reagent (TaKaRa) according to the manufacturer’s instructions. Real-time PCR for GAPDH, GLI1, SHH, HHIP, PTCH1, SMO, FU, SUFU and CCND1 was performed on an Applied Biosystems stepone plus Sequence Detection System (Applied Biosystems) using SYBR green dye and primers as described in Table 1. For quantification, the relative mRNA level of specific gene expression was calculated using the 2−ΔΔCt method with GAPDH level as the control. Each experiment was performed independently at least three times.
Table 1. Primers for Real-time PCR.
| Genes | Forword primer (5′-3′) | Reverse primer (5′-3′) |
| GLI1 | CTCCCGAAGGACAGGTATGTAAC | CCCTACTCTTTAGGCACTAGAGTTG |
| PTCH1 | TCGAGACCAACGTGGAGGAG | CCGAGTCCAGGTGTTGTAGG |
| HHIP | TTCCATACCAAGGAGCAACC | TCTTGCCACTGCTTTGTCAC |
| SHH | CGGGAAGAGGAGGCACCCCA | GTACTTGCTGCGGTCGCGGT |
| CCND1 | AGAAGGAGGTCCTGCCGTCC | GGTCCAGGTAGTTCATGGCC |
| FU | ACTCTGAGCAGACTTTGCGGAG | CCATCCAAGACAACCTGCTGTG |
| SUFU | AGAGTGCCGCCGCCTTTACC | ACGGGCTGCATCTGTGGGTC |
| SMO | CAGGAGGAAGCGCACGGCAA | TGCAGCGCAGGAAGTCAGGC |
| GAPDH | TGTGGGCATCAATGGATTTGG | ACACCATGTATTCCGGGTCAAT |
Luciferase Reporter Gene Assay
GLI luciferase reporter construct (8×3′ GLI BSwt-luc) was kindly provided by Dr. Hisato Kondoh [58]. AsPC-1 cells were transiently transfected with the GLI-luc plasmid and the SV40-Renilla control plasmid using Lipofectamine 2000 (Invitrogen) according to the manufacturer’s instructions. Twenty-four hours post-transfection, cells were treated with various concentration of LiCl for 18 hours. Luciferase activity was determined with the dual luciferase reporter assay system (Promega Corporation, WI) according to the manufacturer’s instruction, and normalized to renilla luciferase activity as a control for transfection efficiency. Each experiment was repeated at least three times with similar results.
Statistical Analysis
Results were presented as mean±S.E.M. Statistical significance between groups was analyzed by one-way ANOVA followed with the Student–Newman–Keuls multiple comparisons tests. A P-value of <0.05 was considered significant.
Funding Statement
This work is supported by the “111 Project” from the Ministry of Education of China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62: 10–29. [DOI] [PubMed] [Google Scholar]
- 2. Kim R (2011) FOLFIRINOX: a new standard treatment for advanced pancreatic cancer? Lancet Oncol 12: 8–9. [DOI] [PubMed] [Google Scholar]
- 3. Philip PA (2008) Improving treatment of pancreatic cancer. Lancet Oncol 9: 7–8. [DOI] [PubMed] [Google Scholar]
- 4. Van Cutsem E, Vervenne WL, Bennouna J, Humblet Y, Gill S, et al. (2009) Phase III trial of bevacizumab in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. J Clin Oncol 27: 2231–2237. [DOI] [PubMed] [Google Scholar]
- 5. Van Cutsem E, Verslype C, Grusenmeyer PA (2007) Lessons learned in the management of advanced pancreatic cancer. J Clin Oncol 25: 1949–1952. [DOI] [PubMed] [Google Scholar]
- 6. Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, et al. (2007) Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 25: 1960–1966. [DOI] [PubMed] [Google Scholar]
- 7. Hidalgo M (2010) Pancreatic cancer. N Engl J Med 362: 1605–1617. [DOI] [PubMed] [Google Scholar]
- 8. McMahon AP, Ingham PW, Tabin CJ (2003) Developmental roles and clinical significance of hedgehog signaling. Curr Top Dev Biol 53: 1–114. [DOI] [PubMed] [Google Scholar]
- 9. Lewis EB (1978) A gene complex controlling segmentation in Drosophila. Nature 276: 565–570. [DOI] [PubMed] [Google Scholar]
- 10. Zhao Q, Beck A, Fraidenraich D (2010) A direct, non-canonical pathway for Hedgehog proteins in the endothelium. Cell Cycle 9: 647–648. [PubMed] [Google Scholar]
- 11. Blotta S, Jakubikova J, Calimeri T, Roccaro AM, Amodio N, et al. (2012) Canonical and non canonical Hedgehog pathway in the pathogenesis of multiple myeloma. Blood 120: 5002–5013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berman DM, Karhadkar SS, Maitra A, Montes De Oca R, Gerstenblith MR, et al. (2003) Widespread requirement for Hedgehog ligand stimulation in growth of digestive tract tumours. Nature 425: 846–851. [DOI] [PubMed] [Google Scholar]
- 13. Xie J, Murone M, Luoh SM, Ryan A, Gu Q, et al. (1998) Activating Smoothened mutations in sporadic basal-cell carcinoma. Nature 391: 90–92. [DOI] [PubMed] [Google Scholar]
- 14. Thayer SP, di Magliano MP, Heiser PW, Nielsen CM, Roberts DJ, et al. (2003) Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature 425: 851–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ji Z, Mei FC, Xie J, Cheng X (2007) Oncogenic KRAS activates hedgehog signaling pathway in pancreatic cancer cells. J Biol Chem 282: 14048–14055. [DOI] [PubMed] [Google Scholar]
- 16. Wang Y, Ding Q, Yen CJ, Xia W, Izzo JG, et al. (2012) The crosstalk of mTOR/S6K1 and Hedgehog pathways. Cancer Cell 21: 374–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xu X, Zhou Y, Xie C, Wei SM, Gan H, et al. (2012) Genome-Wide Screening Reveals an EMT Molecular Network Mediated by Sonic Hedgehog-Gli1 Signaling in Pancreatic Cancer Cells. PLoS One 7: e43119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Soleti R, Benameur T, Porro C, Panaro MA, Andriantsitohaina R, et al. (2009) Microparticles harboring Sonic Hedgehog promote angiogenesis through the upregulation of adhesion proteins and proangiogenic factors. Carcinogenesis 30: 580–588. [DOI] [PubMed] [Google Scholar]
- 19. Nolan-Stevaux O, Lau J, Truitt ML, Chu GC, Hebrok M, et al. (2009) GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation. Genes Dev 23: 24–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mazumdar T (2011) The GLI genes as the molecular switch in disrupting Hedgehog signaling in colon cancer. oncotarget 2: 638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lauth M, Bergstrom A, Shimokawa T, Toftgard R (2007) Inhibition of GLI-mediated transcription and tumor cell growth by small-molecule antagonists. Proc Natl Acad Sci U S A 104: 8455–8460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Johnson G, Gershon S (1999) Early North American research on lithium. Aust N Z J Psychiatry 33 Suppl: S48–53 [DOI] [PubMed] [Google Scholar]
- 23. Cohen P, Goedert M (2004) GSK3 inhibitors: development and therapeutic potential. Nat Rev Drug Discov 3: 479–487. [DOI] [PubMed] [Google Scholar]
- 24. Klein PS, Melton DA (1996) A molecular mechanism for the effect of lithium on development. Proc Natl Acad Sci U S A 93: 8455–8459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mora A, Sabio G, Risco AM, Cuenda A, Alonso JC, et al. (2002) Lithium blocks the PKB and GSK3 dephosphorylation induced by ceramide through protein phosphatase-2A. Cell Signal 14: 557–562. [DOI] [PubMed] [Google Scholar]
- 26. Quiroz JA, Gould TD, Manji HK (2004) Molecular effects of lithium. Mol Interv 4: 259–272. [DOI] [PubMed] [Google Scholar]
- 27. Spiegelberg BD (2005) Alteration of Lithium Pharmacology through Manipulation of Phosphoadenosine Phosphate Metabolism. J Biol Chem 280: 5400–5405. [DOI] [PubMed] [Google Scholar]
- 28. Freland L, Beaulieu JM (2012) Inhibition of GSK3 by lithium, from single molecules to signaling networks. Front Mol Neurosci 5: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nowicki MO, Dmitrieva N, Stein AM, Cutter JL, Godlewski J, et al. (2008) Lithium inhibits invasion of glioma cells; possible involvement of glycogen synthase kinase-3. Neuro Oncol 10: 690–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vidal F, de Araujo WM, Cruz AL, Tanaka MN, Viola JP, et al. (2011) Lithium reduces tumorigenic potential in response to EGF signaling in human colorectal cancer cells. Int J Oncol 38: 1365–1373. [DOI] [PubMed] [Google Scholar]
- 31. Ronchi A, Salaroli R, Rivetti S, Della Bella E, Di Tomaso T, et al. (2011) Lithium induces mortality in medulloblastoma cell lines. Int J Oncol 37: 745–752. [DOI] [PubMed] [Google Scholar]
- 32. Erdal E, Ozturk N, Cagatay T, Eksioglu-Demiralp E, Ozturk M (2005) Lithium-mediated downregulation of PKB/Akt and cyclin E with growth inhibition in hepatocellular carcinoma cells. Int J Cancer 115: 903–910. [DOI] [PubMed] [Google Scholar]
- 33. Beyaert R, Vanhaesebroeck B, Suffys P, Van Roy F, Fiers W (1989) Lithium chloride potentiates tumor necrosis factor-mediated cytotoxicity in vitro and in vivo. Proc Natl Acad Sci U S A 86: 9494–9498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cohen Y, Chetrit A, Cohen Y, Sirota P, Modan B (1998) Cancer morbidity in psychiatric patients: influence of lithium carbonate treatment. Med Oncol 15: 32–36. [DOI] [PubMed] [Google Scholar]
- 35. Zhu Z, Kremer P, Tadmori I, Ren Y, Sun D, et al. (2011) Lithium suppresses astrogliogenesis by neural stem and progenitor cells by inhibiting STAT3 pathway independently of glycogen synthase kinase 3 beta. PLoS One 6: e23341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kaufmann L, Marinescu G, Nazarenko I, Thiele W, Oberle C, et al. (2011) LiCl induces TNF-alpha and FasL production, thereby stimulating apoptosis in cancer cells. Cell Commun Signal 9: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mao CD, Hoang P, DiCorleto PE (2001) Lithium inhibits cell cycle progression and induces stabilization of p53 in bovine aortic endothelial cells. J Biol Chem 276: 26180–26188. [DOI] [PubMed] [Google Scholar]
- 38. Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, et al. (1988) Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell 53: 549–554. [DOI] [PubMed] [Google Scholar]
- 39. Levy L, Hill CS (2005) Smad4 dependency defines two classes of transforming growth factor {beta} (TGF-{beta}) target genes and distinguishes TGF-{beta}-induced epithelial-mesenchymal transition from its antiproliferative and migratory responses. Mol Cell Biol 25: 8108–8125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kayed H, Kleeff J, Osman T, Keleg S, Buchler MW, et al. (2006) Hedgehog signaling in the normal and diseased pancreas. Pancreas 32: 119–129. [DOI] [PubMed] [Google Scholar]
- 41. Chen JK (2002) Inhibition of Hedgehog signaling by direct binding of cyclopamine to Smoothened. Genes & Development 16: 2743–2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Daniel D. Von Hoff MD, Patricia M LoRusso, D.O., et al (2009) Inhibition of the Hedgehog Pathway in Advanced Basal-Cell Carcinoma. N Engl J Med 361: 1164–1172. [DOI] [PubMed] [Google Scholar]
- 43. Merchant AA, Matsui W (2010) Targeting Hedgehog – a Cancer Stem Cell Pathway. Clinical Cancer Research 16: 3130–3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Low JA, de Sauvage FJ (2010) Clinical experience with Hedgehog pathway inhibitors. J Clin Oncol 28: 5321–5326. [DOI] [PubMed] [Google Scholar]
- 45. Fu J, Rodova M, Roy SK, Sharma J, Singh KP, et al. (2013) GANT-61 inhibits pancreatic cancer stem cell growth in vitro and in NOD/SCID/IL2R gamma null mice xenograft. Cancer Lett 330: 22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Huntzicker EG, Estay IS, Zhen H, Lokteva LA, Jackson PK, et al. (2006) Dual degradation signals control Gli protein stability and tumor formation. Genes Dev 20: 276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jiang J (2006) Regulation of Hh/Gli signaling by dual ubiquitin pathways. Cell Cycle 5: 2457–2463. [DOI] [PubMed] [Google Scholar]
- 48. Plyte SE, Hughes K, Nikolakaki E, Pulverer BJ, Woodgett JR (1992) Glycogen synthase kinase-3: functions in oncogenesis and development. Biochim Biophys Acta 1114: 147–162. [DOI] [PubMed] [Google Scholar]
- 49. Kotliarova S, Pastorino S, Kovell LC, Kotliarov Y, Song H, et al. (2008) Glycogen synthase kinase-3 inhibition induces glioma cell death through c-MYC, nuclear factor-kappaB, and glucose regulation. Cancer Res 68: 6643–6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Marchand B, Tremblay I, Cagnol S, Boucher MJ (2012) Inhibition of glycogen synthase kinase-3 activity triggers an apoptotic response in pancreatic cancer cells through JNK-dependent mechanisms. Carcinogenesis 33: 529–537. [DOI] [PubMed] [Google Scholar]
- 51. Shimasaki T, Ishigaki Y, Nakamura Y, Takata T, Nakaya N, et al. (2012) Glycogen synthase kinase 3beta inhibition sensitizes pancreatic cancer cells to gemcitabine. J Gastroenterol 47: 321–333. [DOI] [PubMed] [Google Scholar]
- 52. Schotte P, Van Loo G, Carpentier I, Vandenabeele P, Beyaert R (2001) Lithium sensitizes tumor cells in an NF-kappa B-independent way to caspase activation and apoptosis induced by tumor necrosis factor (TNF). Evidence for a role of the TNF receptor-associated death domain protein. J Biol Chem 276: 25939–25945. [DOI] [PubMed] [Google Scholar]
- 53. Welsh GI, Miller CM, Loughlin AJ, Price NT, Proud CG (1998) Regulation of eukaryotic initiation factor eIF2B: glycogen synthase kinase-3 phosphorylates a conserved serine which undergoes dephosphorylation in response to insulin. FEBS Lett 421: 125–130. [DOI] [PubMed] [Google Scholar]
- 54. Inoki K, Ouyang H, Zhu T, Lindvall C, Wang Y, et al. (2006) TSC2 integrates Wnt and energy signals via a coordinated phosphorylation by AMPK and GSK3 to regulate cell growth. Cell 126: 955–968. [DOI] [PubMed] [Google Scholar]
- 55. Sun A, Shanmugam I, Song J, Terranova PF, Thrasher JB, et al. (2007) Lithium suppresses cell proliferation by interrupting E2F-DNA interaction and subsequently reducing S-phase gene expression in prostate cancer. Prostate 67: 976–988. [DOI] [PubMed] [Google Scholar]
- 56. Welcker M, Singer J, Loeb KR, Grim J, Bloecher A, et al. (2003) Multisite phosphorylation by Cdk2 and GSK3 controls cyclin E degradation. Mol Cell 12: 381–392. [DOI] [PubMed] [Google Scholar]
- 57. Regl G, Kasper M, Schnidar H, Eichberger T, Neill GW, et al. (2004) The zinc-finger transcription factor GLI2 antagonizes contact inhibition and differentiation of human epidermal cells. Oncogene 23: 1263–1274. [DOI] [PubMed] [Google Scholar]
- 58. Sasaki H, Hui C, Nakafuku M, Kondoh H (1997) A binding site for Gli proteins is essential for HNF-3beta floor plate enhancer activity in transgenics and can respond to Shh in vitro. Development 124: 1313–1322. [DOI] [PubMed] [Google Scholar]