Abstract
Background
Despite a well-described association of age and injury with mortality and decreased functional status, inpatient mortality studies have traditionally not included analysis of DNR status. We hypothesized that the increased likelihood of DNR status in older patients alters age-adjusted mortality rates in trauma.
Methods
The trauma registry was queried for adult patients admitted to our Level I trauma center (1/2005–12/2008) and divided into 8 age groups by decade. Ages 15–44 were collapsed due to lack of variation. We compared age, case fatality rate, and DNR status by univariate analysis and trends by Chi-square (p<0.05).
Results
15,227 adult patients were admitted, 13% were elderly (≥ 65), and 7% died. DNR status was known in 75% of deaths, and 42% of those had active DNR orders on the chart at time of death. DNR likelihood increased with age (p < 0.05), from 5 to 18%. With DNRs excluded, mortality variability across all ages was markedly diminished (4%–7%).
Conclusions
DNR status among trauma patients varies significantly, due to inconsistent implementation and meaning between hospitals, and successive decades are more likely to have an active DNR order at time of death. When DNR patients were excluded from mortality analysis, age was minimally associated with an increased risk of death. Inclusion of DNR patients within mortality studies likely skews those analyses, falsely indicating failed resuscitative efforts rather than humane decisions to limit care after injury.
Keywords: Elderly trauma, DNR, Withdrawal of care
BACKGROUND
As the US population ages, trauma centers have seen an increased proportion of elderly patients presenting with major injury. This change correlates with US Census figures projecting that the population over the age of 65 will nearly double in size over the next 20 years, from 46 million in 2010, to an estimated 81 million in 2030 [1]. Older trauma patients have significantly higher reported mortality rates than do younger patients with similar injury severity scores (ISS) [2,3]. The management of this particular cohort of patients poses several challenges in their management. Not only is their resuscitation greatly confounded by varied pre-existing co-morbidities, but ethical dilemmas of balancing post-injury recovery, quality of life, and the end of life decisions by family and care teams comes even more into play.
Despite a well-described association of age and injury severity with increased mortality and decreased functional status, inpatient mortality studies have traditionally not included analysis of the Do Not Resuscitate (DNR) order status. We hypothesized that the increased likelihood of active DNR orders in older patients alters age-adjusted mortality rates in trauma and thereby alters trauma center outcomes.
METHODS
The Texas Trauma Institute (TTI) at Memorial Hermann Hospital is the flagship hospital and trauma center for the University of Texas Health Science Center in Houston, Texas. TTI is one of only two level I trauma centers covering the city of Houston and Harris County, serving a population of over six million people. We queried the TTI registry to capture consecutive adult (> 14 years of age) patients admitted to our academic center between January 1, 2005 and December 31, 2008. We divided the patients into eight age groups by decade, to correlate with categories of data analysis in the National Trauma Data Bank (NTDB) [4]: 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥ 85 years of age. We collapsed ages 15–44 into a single group due to a lack of variability between these decades. We analyzed the relationship between age and Injury Severity Score (ISS), mechanism of injury, and DNR status at time of death. Mortality is presented as a case-fatality rate, the ratio of deaths to the total number of patients within each age group. While there is no consensus in the literature for this definition, for the purposes of this study we chose to define ‘elderly’ as individuals ≥ 65 years of age.
Our database is prospectively collected by concurrent chart review, and undergoes a regular quality assurance by health care professionals. Trained, dedicated data abstractors collect and enter variables into our trauma registry on a continuous basis. A less than ten percent error rate was accepted.
Continuous data are presented as medians (with 25th and 75th inter-quartile ranges, IQR) with comparisons between groups performed using the Wilcoxon rank sum (Mann-Whitney U test). Categorical data are reported as proportions and, where appropriate, tested for significance using χ2 or Fisher exact tests. Each decade group was compared to the immediately preceding decade group, and analysis was made by univariate as well as non-parametric trend analysis. A p-value of 0.05 was considered significant. Statistical analysis was conducted in Stata® 11.1 IC (2009 StatCorp, College Station, TX).
RESULTS
There were 15,227 adult trauma patients admitted during the four year study period (Table 1), of which 13% were ≥ 65 years of age. Overall, our study population was 71% male, however when divided to young versus elderly, with elderly defined as ≥ 65 years of age, males were 75% of the younger patients, and 50% of the elder patients. The mechanism of injury experienced by our patients was 86% blunt in the overall population, but varied with the highest percentage of penetrating trauma in 20–35 year old groups (19%) and an age-associated trend down to three to five percent in the ≥ 65 year old groups (p<0.001). The mechanism of blunt injury experienced by the elderly patients was motor vehicle crash in 42% (832), motorcycle crash in 8% (158), falls in 37% (733), auto versus pedestrian in 5% (97), and assault in 3% (59), with the remaining 5% (102) injured by penetrating trauma. Overall, there was a high severity of injury (as measured by ISS) treated at our facility with 40% of our patients being admitted with ISS scores >15. NTDB reports an average of 21% of patients admitted with ISS >15 [4]. As seen in Table 2, the majority of our patients were young, but the distribution of ISS was the same across age groups.
Table 1.
Demographics
| Patients | 15,227 | |
| ≥ 65 years | 1,981 | 13% |
| Males | 10,811 | 71% |
| Females | 4,416 | 29% |
| Blunt Mechanism | 13,095 | 86% |
| MVC | 7,309 | 48% |
| MCC | 2,284 | 15% |
| Falls | 2,132 | 14% |
| Auto vs Pedestrian | 761 | 5% |
| Assault | 609 | 4% |
| Penetrating | 2,132 | 14% |
| ISS | ||
| 0–8 | 3,966 (26%) | |
| 9–15 | 5,483 (35%) | |
| 16–24 | 3,064 (20%) | |
| ≥ 25 | 2,949 (19%) | |
| Case Fatality Rate | 6.8 % |
Description of demographics of all trauma patients within study. ISS : Injury Severity Score
Table 2.
Distribution of patients by ISS
| ISS 0–15 % of group | ISS 16–24 % of group | ISS ≥ 25 % of group | % of total population | |
|---|---|---|---|---|
| 15–44y (n=9408) | 62.9% | 18.2% | 18.9% | 61.8 |
| 45–54y (n=2425) | 59.2% | 21.2% | 19.6% | 15.9 |
| 55–64(n=1472 | 59.2% | 21.7% | 19.1% | 9.7 |
| 65–74y (n=845) | 57.7% | 23.0% | 19.3% | 5.6 |
| 75–84y (n=692) | 51.6% | 25.9% | 22.5% | 4.5 |
| ≥85 (n=385) | 58.4% | 26.3% | 15.3% | 2.5 |
| TOTAL (n=15227) | 61.0 % of total | 19.8 % of total | 19.2 % of total | 100 |
Distribution of all study patients by Injury Severity Score (ISS) score, divided into age groups used for analysis.
Our overall mortality was 6.8% (1,030 deaths) during the four-year study period. In 75% (775) of the deaths, the patients’ DNR status was known, with 42% (328) of these having active DNR orders on the chart at time of death. When evaluated by age group, older patients were more likely to be DNR at time of death than were their younger counterparts. Only 25% of patients age 15–44 were DNR at time of death, compared to 73% of individuals over the age of 65. There were significant increases with each subsequent decade (Figure 1). Of the 1,030 deaths, 43% of patients died more than 24 hours from arrival to the hospital, with median time to death of 129 hours. In contrast, 63% of the 276 elderly deaths occurred more than 24 hours after arrival, with a median time to death of 117 hours. 83% (144) of the late elderly deaths had a known DNR status, and of those, 89% (129) had an active DNR status at time of death, compared to 44% (32) of the 72 elderly deaths with known DNR status that occurred within 24 hours of arrival.
Figure 1.
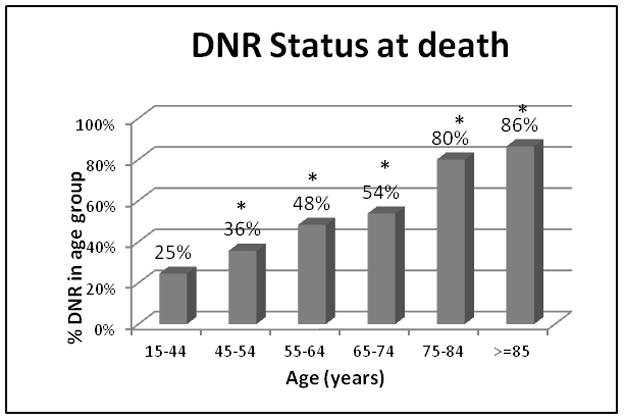
The percentage of patients within each age group with active DNR orders on the chart at time of death. * p<0.05
In our study, increasing age correlated with increased fatality, with a 5% fatality rate of patients aged 15–44 years compared to 14.4% fatality rate in those aged 65 years or older. More importantly, however, when the subset of patients with active DNR orders (775) were removed, and only non-DNR deaths evaluated, the increase in case-fatality rate by age group was attenuated. So while this noted similar case-fatalities in the younger age groups, the case-fatality rate for those patients aged 65 years or older was dramatically reduced from 14.4% to only 6.7% (Figure 2).
Figure 2.
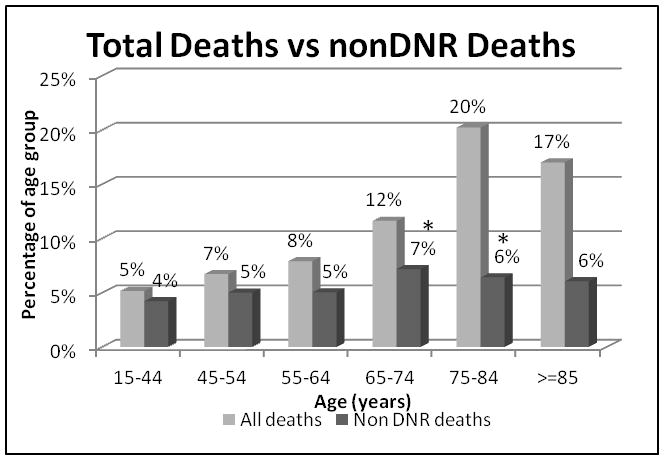
The percentage of deaths within each age group, comparing all deaths to deaths with no active DNR orders. *p<0.05
DISCUSSION
As the population ages and the demographics of injured patients correspondingly change, trauma surgeons and critical care physicians will more frequently face discussions and decisions regarding prognosis and end-of-life care. We found that exclusion of patients with an active “do not resuscitate” order in place at time of death significantly reduced the age-related mortality in our trauma population. These findings differ greatly from the well established mortality pattern in our previous study and in the literature [2, 3, 5]. The reduced mortality rate seen in this study could represent a successful response to resuscitation (successful “rescue”) in elderly patients, which would support the findings of Jacobs and McKinley that an initial aggressive approach is warranted despite advanced age [6, 7]. The increased mortality traditionally observed in the elderly trauma patient (when DNR patients are included) could represent a decision not to pursue aggressive resuscitation in addition to a failed resuscitative effort (“failure to rescue”) in these patients. Our database did not include information on the timing of the DNR order in relation to death during the study period, however the marked discrepancy in the trends of mortality raises an important question, particularly in light of recent trends to create benchmarks of care in the trauma population.
The Trauma Quality Improvement Program (TQIP) was created by the American College of Surgeons Committee on Trauma with a mandate to design, test and implement a quality improvement program for trauma that is validated, risk-adjusted and outcomes-based, to measure, and continually improve the quality of trauma care [8]. The main advantage of TQIP is to disseminate clinical “best practices”, derived from evidence-based guidelines, for external comparison between institutions [9]. The primary outcome of interest in the TQIP analysis was death during hospitalization, and a method of calculating an expected mortality rate was developed based on potential predictors of mortality. This expected mortality can then be compared to a trauma center’s observed mortality rate, and an observed-to-expected (O/E) mortality ratio calculated. These O/E ratios can be ranked against the performance of other trauma centers nationwide [8]. Patients with pre-existing DNR orders or advanced directives to withhold life sustaining interventions are excluded as well as those with a GSW to the head with brain injury and those recorded as dead on arrival [8]. Individuals in whom a DNR directive was created during the hospitalization are included in the mortality data for the TQIP registry. However, the quality of external benchmarks created from the NTDB is highly dependent on not only the quality of the data but also the comparability of data registries [10].
Factors other than quality of care can influence the risk-adjusted mortality rates created from the TQIP analysis [8]. There is a great variability in the implementation and interpretation of DNR directives between institutions across the country. Nathens et al found an average of 7% of trauma patients in their large ICU cohort study had a DNR directive placed, with a wide variation in the proportion of patients with DNR status (0–57%) between centers. They noted an extremely high mortality rate associated with a DNR order (88%) compared to the 3% mortality rate of those without a DNR. While not absolute, this suggests that a DNR order, rather than specifically a decision to not perform CPR after loss of vital signs, indicates a change in focus away from full supportive measures to a less aggressive care plan overall, and possibly even withdrawal of further supportive measures [11, 12]. The timing of a DNR order late in an ICU course may represent failed aggressive ICU therapy compared to an early-enacted DNR based on pre-existing disease or overall injury burden [13]. There are also well-established cultural and racial differences in DNR implementation, as well as institutional characteristics associated with variations in use of DNR orders and how aggressively these orders are pursued [11].
Factors that alter the institutional mortality rate will significantly affect the institutions’ national ranking against external benchmarks. Gomez et al reported that the decision of whether or not to include isolated hip fractures in mortality studies from the NTDB changed the ranking of 78% of participating centers, over a third of which changed by at least three rankings [10]. Similarly, an aggressive placement of patients into long term acute care facilities by Kelly et al, and the resultant decrease of their reported in-hospital mortality (3.3 to 2.4%), was sufficient to move their institution to a lower quartile on the NTDB benchmark report [14].
There are a several limitations in this study that should be mentioned. This was a retrospective review of a clinical database, not a prospective analysis of data specifically related to the geriatric population or DNR status. During the four years of this study, we did not record the DNR status of those patients that survived, and did not record the timing of enactment of the DNR directive in relation to time of death, so are unable to assess causality between DNR status and death. We did separately examine the DNR status of deaths that occurred more than 24 hours after arrival, however this did not change our results. It is possible that the DNR order was placed during an acute clinical decline, as a pre-terminal decision, rather than it being a deliberate decision to withhold resuscitation due to a combined assessment of injury severity, baseline functional status, and expected quality of life if resuscitation were successful. Additionally, we have no data on pre-existing living wills or DNR status prior to admission. We have since expanded our data collection to include DNR status regardless of outcome, as well as the timing of the DNR decision in relation to time of death, to provide insight in the future to end-of-life decisions in our patients.
CONCLUSIONS
The increasing age of the trauma population and the increased morbidity and mortality experienced by these patients is an issue of real and growing concern to all trauma care providers. As further efforts are made to create benchmarks of trauma care nationwide, a factor that alters the assessment of trauma outcomes will determine whether or not these benchmarks are attainable. With the considerable variation between centers for DNR use and implementation, can we depend on outcomes in the geriatric patient population to be accurate? We noted near abolishment of the age-related increase in mortality once DNR patients were removed, as more than 50% patients over 65 had a DNR at the time of death. Inclusion of these patients skews our outcome analysis of the relationship of age to mortality.
Footnotes
Presented at the 70th Annual Meeting of the American Association for the Surgery of Trauma, September 14, 2011.
No Conflicts of Interest to declare.
AUTHORSHIP:
S.A., B.C. and J.H. designed this study. S.A. and C.W. performed the literature search. J.P. and E.D. acquired the data; S.A., B.C., J.H. and R.K. analyzed the data. All authors contributed to the interpretation of the data. S.A. and B.C. prepared the manuscript, which all authors critically revised and approved.
DISCLOSURE:
The authors declare no conflicts of interest.
Financial disclosure: This research was supported by the University of Texas Medical School-Houston and NIGMS funding (T-32 GM008792 and P-50 GM38529)
Contributor Information
Sasha D Adams, Email: sasha_adams@med.unc.edu.
Bryan A Cotton, Email: bryan.a.cotton@uth.tmc.edu.
Charles E Wade, Email: charles.e.wade@uth.tmc.edu.
Rosemary A Kozar, Email: rosemary.a.kozar@uth.tmc.edu.
Edmundo Dipasupil, Email: edmundo.dipasupil@memorialhermann.org.
Jeanette M Podbielski, Email: jeanette.m.podbielski@uth.tmc.edu.
Brijesh S Gill, Email: brijesh.s.gill@uth.tmc.edu.
James R Duke, Email: james.h.duke@uth.tmc.edu.
Philip R Adams, Email: pradamsmd@yahoo.com.
John B Holcomb, Email: john.holcomb@uth.tmc.edu.
References
- 1.U.S. Census Bureau. Population estimates. 2000 Available at http://www.census.gov/popest/estimates.html. Census.
- 2.Tornetta P, 3rd, Mostafavi H, Riina J, Turen C, Reimer B, Levine R, Behrens F, Geller J, Ritter C, Homel P. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;46:702–706. doi: 10.1097/00005373-199904000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Adams SD, Cotton BA, McGuire MF, Dipasupil E, Podbielski JM, Zaharia A, Ware DN, Gill BS, Albarado R, Kozar RA, et al. Unique pattern of complications in elderly trauma patients at a Level 1 trauma center. J Trauma. 2012;72:112–118. doi: 10.1097/TA.0b013e318241f073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Surgeons National Trauma Data Bank. Report 2009. Available at http://www.facs.org/trauma/ntdb/docpub.html.
- 5.Jacobs DG. Special considerations in geriatric injury. Curr Opin Crit Care. 2003;9:535–9. doi: 10.1097/00075198-200312000-00012. [DOI] [PubMed] [Google Scholar]
- 6.McKinley BA, Marvin RG, Cocanour CS, Marquez A, Ware DN, Moore FA. Blunt trauma resuscitation: the old can respond. Arch Surg. 2000;135(6):688–93. doi: 10.1001/archsurg.135.6.688. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma; the EAST practice management guidelines work group. J Trauma. 2003;54:391–416. doi: 10.1097/01.TA.0000042015.54022.BE. [DOI] [PubMed] [Google Scholar]
- 8.Hemmila MR, Nathens AB, Shafi S, Calland JF, Clark DE, Cryer HG, Goble S, Hoeft CJ, Meredith JW, Neal ML, et al. The Trauma Quality Improvement Program: pilot study and initial demonstration of feasibility. J Trauma. 2010;86:253–62. doi: 10.1097/TA.0b013e3181cfc8e6. [DOI] [PubMed] [Google Scholar]
- 9.Eastridge BJ, Wade CE, Spott MA, Costanzo G, Dunne J, Flaherty S, Holcomb JB, West S, Apodaca A, Blackbourne L, et al. Utilizing a trauma systems approach to benchmark and improve combat casualty care. J Trauma. 2010;69:S5–9. doi: 10.1097/TA.0b013e3181e421f3. [DOI] [PubMed] [Google Scholar]
- 10.Gomez D, Haas B, Hemmila M, Pasquale M, Goble S, Neal M, Mann NC, Meredith W, Cryer HG, Shafi S, et al. Hips can lie: impact of excluding isolated hip fractures on external benchmarking of trauma center performance. J Trauma. 2010;69(5):1037–41. doi: 10.1097/TA.0b013e3181f65387. [DOI] [PubMed] [Google Scholar]
- 11.Nathens AB, Rivara FP, Wang J, Mackenzie EJ, Jurkovich GJ. Variation in the rates of do not resuscitate orders after major trauma and the impact of intensive care unit environment. J Trauma. 2008;64(1):81–88. doi: 10.1097/TA.0b013e31815dd4d7. [DOI] [PubMed] [Google Scholar]
- 12.Kazaure H, Roman S, Sosa JA. High mortality in surgical patients with do-no-resuscitate orders: analysis of 8256 patients. Arch Surg. 2011;146(8):922–8. doi: 10.1001/archsurg.2011.69. [DOI] [PubMed] [Google Scholar]
- 13.Teres D. Trends from the United States with end of life decisions in the intensive care unit. Intensive Care Med. 1993;19(6):316–22. doi: 10.1007/BF01694704. [DOI] [PubMed] [Google Scholar]
- 14.Kelly KB, Koeppel ML, Como JJ, Carter JW, McCoy AM, Claridge JA. Continued rationale of why hospital mortality is not an appropriate measure of trauma outcomes. Am J Surg. 2012;203:366–369. doi: 10.1016/j.amjsurg.2011.10.004. [DOI] [PubMed] [Google Scholar]


